Abstract
Prospective nonrandomized control study.
The study aimed to investigate the implication of the HE's Lumbar LOcation (HELLO) system in improving the puncture accuracy and reducing fluoroscopy in percutaneous transforaminal endoscopic discectomy (PTED).
Percutaneous transforaminal endoscopic discectomy is one of the most popular minimally invasive spine surgeries that heavily depend on repeated fluoroscopy. Increased fluoroscopy will induce higher radiation exposure to surgeons and patients. Accurate puncture in PTED can be achieved by accurate preoperative location and definite trajectory.
The HELLO system mainly consists of self-made surface locator and puncture-assisted device. The surface locator was used to identify the exact puncture target and the puncture-assisted device was used to optimize the puncture trajectory. Patients who had single L4/5 or L5/S1 lumbar intervertebral disc herniation and underwent PTED were included the study. Patients receiving the HELLO system were assigned in Group A, and those taking conventional method were assigned in Group B. Study primary endpoint was puncture times and fluoroscopic time, and the secondary endpoint was location time and operation time.
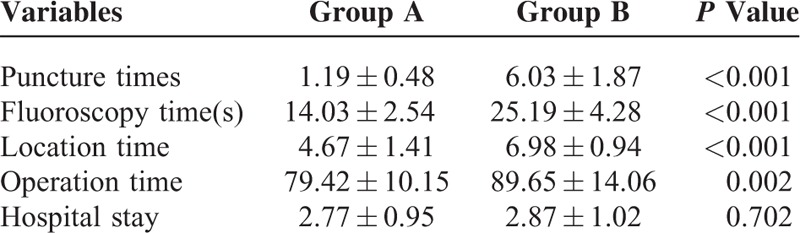
A total of 62 patients who received PTED were included in this study. The average age was 45.35 ± 8.70 years in Group A and 46.61 ± 7.84 years in Group B (P = 0.552). There were no significant differences in gender, body mass index, conservative time, and surgical segment between the 2 groups (P > 0.05). The puncture time(s) were 1.19 ± 0.48 in Group A and 6.03 ± 1.87 in Group B (P < 0.001). The fluoroscopic times were 14.03 ± 2.54 in Group A and 25.19 ± 4.28 in Group B (P < 0.001). The preoperative location time was 4.67 ± 1.41 minutes in Group A and 6.98 ± 0.94 minutes in Group B (P < 0.001). The operation time was 79.42 ± 10.15 minutes in Group A and 89.65 ± 14.06 minutes in Group B (P = 0.002). The hospital stay was 2.77 ± 0.95 days in Group A and 2.87 ± 1.02 days in Group B (P = 0.702). There were no significant differences in the complication rate between the 2 groups (P = 0.386).
The highlight of HELLO system is accurate preoperative location and definite trajectory. This preliminary report indicated that the HELLO system significantly improves the puncture accuracy of PTED and reduces the fluoroscopic time, preoperative location time, as well as operation time. (ChiCTR-ICR-15006730)
INTRODUCTION
Lumbar disc herniation (LDH) is considered to be one of the most common causes of low back pain,1 which often occurs in the L4/5 or L5/S1 level. Discectomy surgery was usually conducted if the conservative therapy was failed. Over the past decades, minimally invasive spine surgery (MISS) has been widely used around the world. Percutaneous transforaminal endoscopic discectomy (PTED) and microdiscectomy were 2 popular and effective MISS techniques for the management of LDH.2,3 However, microdiscectomy may require muscle retraction, bone resection of the lamina and facet joint, and dural sac and nerve retraction.4 In contrast, PTED has the advantages of small incision, local anesthesia, no nerve or muscular traction, rapid recovery, short operation time, low post-operation cost, and so on.5–7 The work channel of PTED is ∼7 mm and it was considered to be the true MISS technique.
Puncture is an essential procedure for PTED, and accurate puncture requires an accurate location of the target and accurate puncture trajectory. Similar with other MISS technique, PTED requires repeated fluoroscopy for the puncture.8,9 Once the puncture target was inaccurate, increased puncture would be inevitable and it might increase the risk of injuring normal tissues. Once the puncture was increased, increased fluoroscopy would be inevitable which might need extra operation time and increase the radiation exposure to doctors and patients. Radiation exposure was considered to be associated with increased risk of cancer, cataract, and cardiovascular disease.10 Therefore, we designed a surface locator to identify the surgical target and applied this self-made device in clinical practice.11–13 However, preoperative location with our self-made surface locator might not be sufficient to reduce the fluoroscopy during PTED. In order to optimize the lumbar location system, we also designed a puncture-assisted device to optimize the puncture trajectory of PTED. The present study aimed to investigate the efficacy of novel lumbar location system in improving puncture accuracy and reducing fluoroscopy during PTED.
MATERIALS AND METHODS
General Information
This prospective nonrandomized control study is approved by institutional review board of Shanghai Tenth People's Hospital (clinical registry: ChiCTR-ICR-15006730). Consent forms were obtained from all included patients prior to PTED. From July 13, 2015, patients who received PTED in Orthopedic Department of Shanghai Tenth People's Hospital were enrolled in the study. The inclusion criteria were: (1) L4/5 or L5/S1 lumbar intervertebral disc herniation combined with/without foraminal stenosis or lateral recess stenosis; (2) patients with an age >18 years old; (3) no severe mental illness or severe obesity. The exclusion criteria were: (1) combined with multilevel lumbar intervertebral disc herniation; (2) highly free intervertebral disc; (3) accompanied by lumbar spondylolisthesis, lumbar instability, lumbar malformation, vertebral fractures, active infection, or other severe spinal diseases.
The patients were evenly divided into 2 groups based on their inclusion number. Patients with odd number receiving HE's (designer) Lumbar LOcation (HELLO) system were assigned in Group A, and those with even number taking a conventional method were assigned in Group B. Study primary endpoint was puncture times and fluoroscopic time, and the secondary endpoint was location time and operation time. Basic information of the patients in 2 groups including age, gender, body mass index (BMI), surgical segment, conservative treatment duration, and fluoroscopy voltage and currents were also recorded.
HELLO System
The HELLO system mainly consists of self-made surface locator and puncture-assisted device. The portable surface locator is made up of radiopaque material with a size of 9 × 18 cm and can be repeatedly used without sterilization (Fig. 1A). It consists of 4 longitudinal crossbars and 19 horizontal crossbars with 1 cm interval. Sequential numbers of different patterns (triangles, circle, rectangular, etc) are made on horizontal crossbars for rapid recognition. We can easily and accurately identify the puncture target with the recognition of the surrounding rods under fluoroscopy. The puncture-guided device consists of 3 parts, namely movable supporting base, micro-regulation part, and 90-degree arc for trajectory-guided puncture (Fig. 1B). The movable supporting base has 5 rollers with brakes. The microregulation part can realize 3-dimensional regulation and freely rotate the arc along the vertical axis. The arc has a slider that could slide along the track and be locked. There were 2 infrared generators in the terminal vertex of the arc for location.
FIGURE 1.
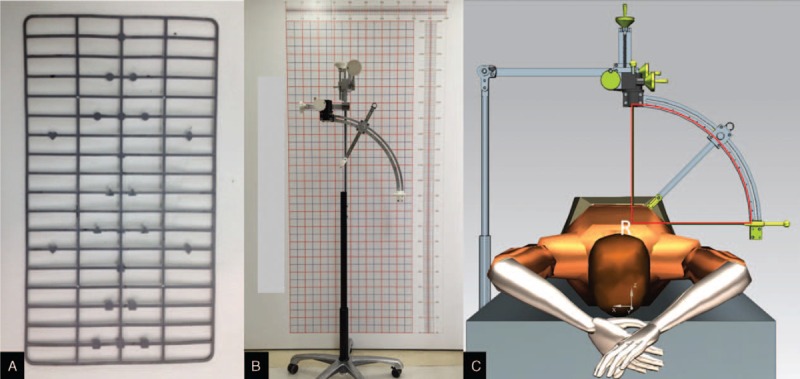
HE's Lumbar lpcation system consisting of surface locator and puncture-guided device. A = real picture of surface locator, B = real picture of puncture-guided device, C = the theory of puncture-guided device.
The basic theory of puncture-guided device is that the puncture target always remains in the center of the 90 degree arc. We can interpret the theory of the puncture-guided device as followed: the back and lateral projections of the puncture target could be marked by the pen on the skin according to the anteroposterior fluoroscopy and lateral fluoroscopy, respectively. Then we located the puncture-guided device with 2 infrared beams on the back marker and lateral marker. At this very position, the puncture target remains in the center of the arc, even we rotate the arc along the vertical axis (Fig. 1C). Then we can freely rotate the arc to a satisfactory angle along the vertical axis and regulate the slider along the tract to an appropriate angle according to the different segment for the puncture. The needle guider on the slider can also be extended and then fixed. After these processes, an optimal puncture trajectory can be realized and the needle can be puncture through the needle guider to the exact target position.
Surgical Procedure
For patients in group A, they were told to get a prone position on the table and parallel to the long axis of operating table. The surface locator was attached to the back and lateral skin of the patient, and then standard anteroposterior and lateral fluoroscopy were obtained by C-arm fluoroscopy (Fig. 2). We identified the puncture target according to the fluoroscopy films and marked them with marker pens on the back and lateral skin. We drew the rough shape of the transverse process near the puncture target and the outline of iliac crest by touching. An assumed approach line was drawn on the back with a certain angle between the approach and the horizontal line. The entry point of the assumed approach was 12 to 13 cm lateral to spinal middle line. A puncture-guided device was moved beside the operating table and fixed by pushing down the brake on the rollers (Fig. 3). The arc was microregulated in 3 different directions to make sure that the infrared beam was right on the skin markers of the puncture target. At this very position, the puncture target remains in the center of the arc. The arc and its slider were regulated to a proper position according to the rough outline of iliac crest and the surgeons experience on different segments. The needle guider was then regulated as near as possible to the patient. A 18G puncture needle could be inserted through the needle guider to the exact puncture target. The following procedures were the same as it was done in the conventional process.
FIGURE 2.
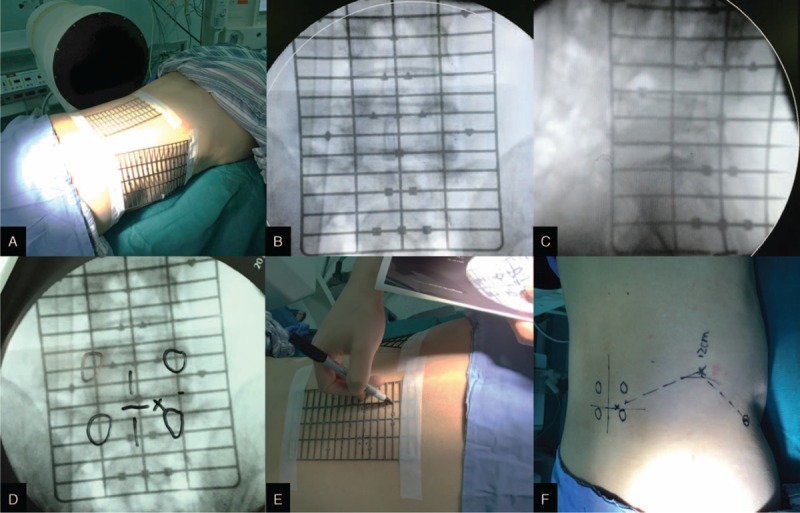
The usage of surface locator in percutaneous transforaminal endoscopic discectomy. A = attachment of surface locator to the back and the lateral skin, B = anteroposterior fluoroscopy of surface locator, C = lateral fluoroscopy of surface locator, D = identifying the puncture target on the film, E = marking the puncture target on the skin, F = drawing the entry point and planned trajectory.
FIGURE 3.

The usage of puncture-guided device in percutaneous transforaminal endoscopic discectomy. A = post-sterilization of puncture-guided device, B = positioning the infrared ray to the back and lateral markers, C = rotating the arc to an appropriate angle, D = regulating the slider and locking it, E = positioning the needle guider to the entry point, F = inserting the needle through the needle guider.
In Group B, the location of puncture target and puncture procedure were undergoing the conventional methods and relied on the experience of the surgeons. Briefly, we touched the iliac crest and spinous process to roughly judge the position of the target segment. Then we used needles to identify the puncture target and the fluoroscopy channel to roughly outline the puncture trajectory under fluoroscopy. We might also draw an assumed approach line and then inserted the 18G needle into the target dependent on the surgeons’ experience after disinfection and local anesthesia. Then a guide wire was inserted through the needle into the target foramen and the needle was removed. An incision of 8 mm was made, and guiding rods were introduced step by step. Then a cannulated dilator was inserted and the guide wire was removed. A working channel was inserted into the area of the extruding fragment followed by an endoscope. The extruding disc was removed using endoscopic forceps and radio frequency. After the herniated fragment was completely removed, the endoscope and cannula was removed, and the skin was closed with 1 stitch. For those with foraminal stenosis or lateral recess stenosis, the PTED was performed according to the standard procedure described by Thomas Hoogland.14
Statistical Analysis
Statistic software SPSS17.0 (IBM Corporation, 1 New Orchard Road Armonk, New York, United States) was adopted to conduct the statistical analysis. Enumeration data were demonstrated as mean ± SD. Independent student t test was used to compare the difference of continuous variables between the 2 groups. Chi square test was used to compare the difference of categorical variables between the 2 groups. We also conducted the Pearson correlation test to analyze the potential correlation between puncture times and fluoroscopic time, fluoroscopic time and operation time, location time and operation time. P < 0.05 was considered as statistical significance.
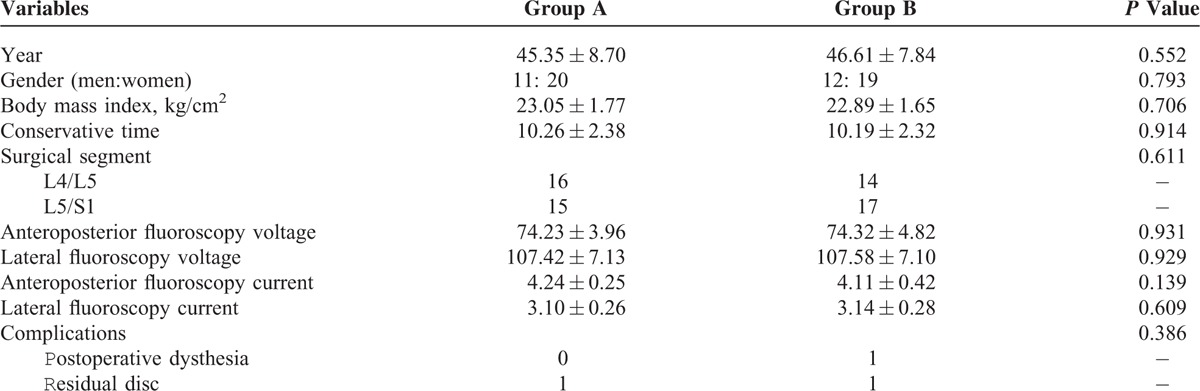
RESULTS
By September 10th 2015, a total of 62 patients who received PTED were included in this study with 31 cases in the 2 groups, respectively (Fig. 4). Totally 68 patients were initially identified, and 6 patients were excluded (1 highly free intervertebral disc, 2 combined with lumbar instability, 3 multilevel lumbar disc herniation). All 62 included patients completed the PTED surgery, and intraoperative blood loss was negligible without blood transfusion (Table 1). There were 11 men and 20 women in Group A, and there were 12 men and 19 women in Group B (P = 0.793). The average age was 45.35 ± 8.70 years in Group A and 46.61 ± 7.84 years in Group B (P = 0.552). The body mass index (BMI) was 23.05 ± 1.77 in Group A and 22.89 ± 1.65 in Group B (P = 0.706). The conservative time was 10.26 ± 2.38 months in Group A and 10.19 ± 2.32 months in Group B (P = 0.914). The number of surgical segments was 16 cases at the L4/5 level and 15 cases at the L5/S1 level in Group A. The number of surgical segments was 14 cases at the L4/5 level and 17 cases at the L5/S1 level in Group B. There were no significant differences in surgical segments between the 2 groups (P = 0.611). There were no significant differences in anteroposterior fluoroscopy voltage, lateral fluoroscopy voltage, anteroposterior fluoroscopy current, and lateral fluoroscopy current between the 2 groups (P > 0.05).
FIGURE 4.
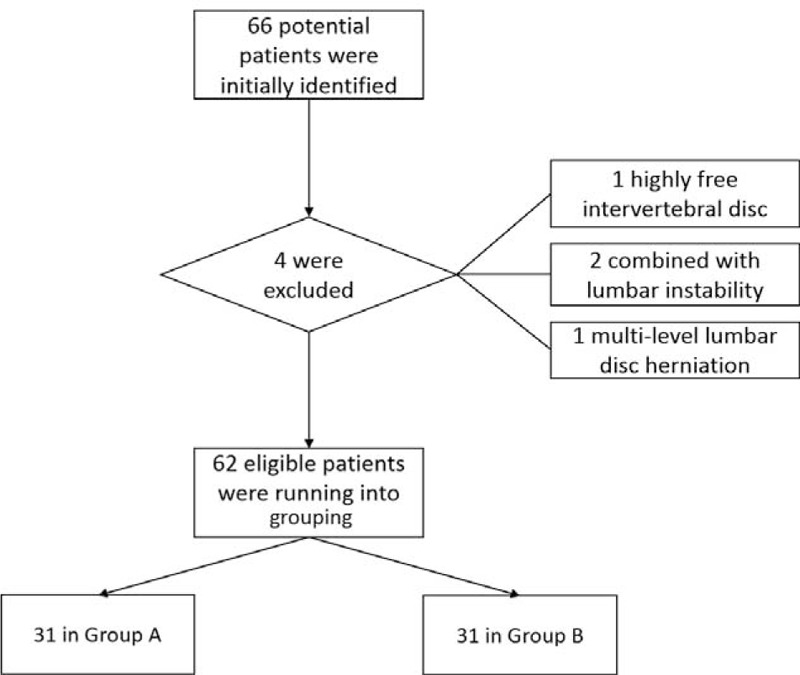
Flow chart of included patients undergoing percutaneous transforaminal endoscopic discectomy in the study.
TABLE 1.
Clinical Characteristics of Included Patients Between the 2 Groups
As demonstrated in Table 2, the puncture times were 1.19 ± 0.48 in Group A and 6.03 ± 1.87 in Group B (P = 0.000). The fluoroscopic time(s) were 14.03 ± 2.54 in Group A and 25.19 ± 4.28 in Group B (P = 0.000). The location time was 4.67 ± 1.41 minutes in Group A and 6.98 ± 0.94 minutes in Group B (P = 0.000). The operation time was 79.42 ± 10.15 minutes in Group A and 89.65 ± 14.06 minutes in Group B (P = 0.002). The hospital stay was 2.77 ± 0.95 days in Group A and 2.87 ± 1.02 days in Group B (P = 0.702). There was strong correlation between puncture times and fluoroscopic time (r = 0.951, P < 0.001). There was mild correlation between fluoroscopic time and operation time (r = 0.392, P = 0.002). However, there was no correlation between location time and operation time (r = 0.251, P = 0.049). There were 1 case of postoperative dysthesia in Group B, and 2 cases of residual disc in Group A and Group B, respectively (P = 0.386).
TABLE 2.
Clinical Outcomes of HE's Lumbar Location System in Percutaneous Transforaminal Lumbar Discectomy
DISCUSSION
Accurate puncture is an essential step in the MISS technique for minimizing puncture injury and radiation exposure, especially in PTED. The present study introduced the HELLO system into clinical practice and confirmed that our self-made HELLO system could significantly improve the puncture accuracy and reduce its fluoroscopic time, preoperative location time as well as operation time. The highlight of HELLO system was accurate preoperative location and definite trajectory. The surface locator could obtain an accurate preoperative location of puncture target in PTED, even could be in any other spinal surgery. The puncture-guided device allowed the surgeon to regulate the angles freely to obtain an ideally definite trajectory and the puncture target still remained in the center of the arc.
The HELLO system might be a promising approach for minimizing strategy of radiation protection. There were several strategies to minimize the radiation exposure in current fluoroscopy-related room, such as reducing fluoroscopy duration, extending distance to the radiation source, optimizing the C-arm fluoroscopy setting, wearing leaded shields, as well as avoiding direct exposure.15 Shielding prevention such as lead aprons or thyroid gland shield was regarded as the most efficient method.11 Keeping away from the tube like 3 feet way or more was considered as the second important method to reduce the radiation.16 Optimizing the C-arm fluoroscopy setting means using automatic pulse mode as much as possible and keeping the tube under the operating table.17,18 In addition, we are supposed to use the hand-free technique to keep the hands away from the beam if possible.8 All these strategies or protection tips could be summed up as 4 main theories based on the ALARA (as low as reasonably achievable) principle,19 namely time minimizing, distance increasing, shield protection, and source control. As for our HELLO system, we realized the fluoroscopy reduction based on the theory of time minimizing.
The HELLO system might also have some advantages over other novel navigation instruments with less radiation in the MISS field. O-arm fluoroscopy was considered to be more accurate in navigation and very efficient in minimizing radiation dosage in MISS.20,21 Moreover, intraoperative magnetic resonance imaging (MRI) navigation and ultrasonic navigation were also 2 novel techniques without x-ray radiation to operating room staff.8,22 However, it should be pointed out that O-arm fluoroscopy has not been widely applied especially in developing countries. Intraoperative MRI navigation is extremely expensive and ultrasonic navigation were not well validated. In contrast, the HELLO system offered a practical alternative to minimize the fluoroscopy time. The average fluoroscopy time reduction could be achieved by 44.30%, and the average operation time reduction was 10.23 minutes. In addition, the surface locator reduced an average preoperative location time of 2.31 minutes, and more importantly, the puncture-guided device could obtain an ideal needle position by 1 puncture basically (Fig. 5). Last but not least, the HELLO system was portable and very flexible, and the puncture-guided device could also be widely used in epidural steroid injection, intraspinal tumor biopsy, spine abscess drainage, and other spine surgeries.
FIGURE 5.
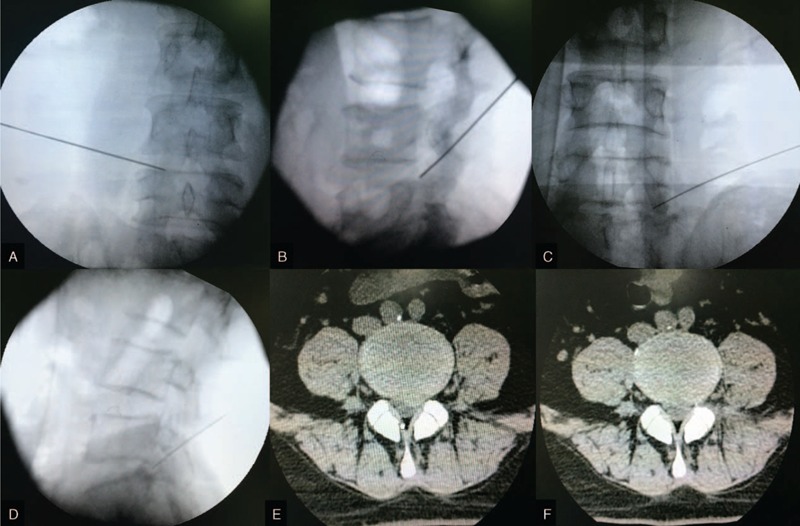
Ideal position of needle by 1 puncture and successful removal of herniated disc. A = anteroposterior fluoroscopy at L4/5, B = lateral fluoroscopy at L4/5, C = anteroposterior fluoroscopy at L5/S1, D = lateral fluoroscopy at L5/S1, E = preoperative magnetic resonance imaging of lumbar disc herniation, F = postoperative magnetic resonance imaging confirming the removal of herniated disc.
Further potential of HELLO system and some limitations of the study should also be noted. Learning curve of the PTED is quite steep, and beginners tend to quit due to the difficult punctures.23–28 This MISS technique heavily relies on the puncture experience of subjective feeling at the very beginning. Countless punctures will defeat the confidence of junior surgeons, especially at the L5/S1 level with high iliac crest and large transversus process. With accurate preoperative location of puncture target and definite trajectory, the HELLO system might has the potential to help the junior surgeons to get command of PTED easily. Further research studying the potential of HELLO system in reducing learning difficulty of PTED for junior surgeons are under investigation. However, when using our HELLO system, the surface locators should be placed as near as possible to the skin and could be fixed by tapes. As for the puncture-guided device, the tube of the C-arm fluoroscopy should be parallel to the ground as much as possible when taking anteroposterior films. Meanwhile, it should be perpendicular to the ground as much as possible when taking lateral films. In addition, this was not a randomized control study, which we might optimize the design in the following days. Last but may not the least, we did not demonstrated the radiation dosage to sensitive organs of the surgeons in this preliminary report as many other studies did.8,17,29–32 It was because the thermoluminescence dosimeter were measured by cumulative dosage and we would present the radiation reduction in future papers with larger participants.
CONCLUSIONS
The highlight of HELLO system is accurate preoperative location and definite trajectory. The HELLO system can significantly improve the puncture accuracy of PTED and reduces the fluoroscopic time, preoperative location time, as well as operation time. This preliminary report of HELLO study indicates the significant benefits of HELLO system in minimizing puncture injury and radiation exposure of PTED, which may have a great potential application in clinical practice. Further researches studying the potential of HELLO system in reducing learning difficulty of PTED for junior surgeons are also under investigation.
Acknowledgments
The authors thank academic club SHEPHERD for providing language help.
Footnotes
Abbreviations: BMI = body mass index, HELLO system = HE's Lumbar LOcation system, LDH = lumbar disc herniation, MISS = minimally invasive spine surgery, MRI = intraoperative magnetic resonance imaging, PTED = percutaneous transforaminal endoscopic discectomy.
GF and XG equally contributed to this study.
Stating: Not any portion of the contents of the paper has been presented.
The authors have no conflicts of interest to disclose.
REFERENCES
- 1.Cheng YP, Lee KW, Lin PY, et al. Full-endoscopic interlaminar removal of chronic lumbar epidural hematoma after spinal manipulation. Surg Neurol Int 2014; 5:55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Brouwer PA, Brand R, Van Den Akker-Van Marle ME, et al. Percutaneous laser disc decompression (PLDD) versus conventional microdiscectomy in sciatica: a randomized controlled trial. Spine J 2015; 15:857–865. [DOI] [PubMed] [Google Scholar]
- 3.Ahn Y. Transforaminal percutaneous endoscopic lumbar discectomy: technical tips to prevent complications. Expert Rev Med Devices 2012; 9:361–366. [DOI] [PubMed] [Google Scholar]
- 4.Li M, Yang H, Yang Q. Full-endoscopic technique discectomy versus microendoscopic discectomy for the surgical treatment of lumbar disc herniation. Pain Physician 2015; 18:359–363. [PubMed] [Google Scholar]
- 5.Ahn Y. Percutaneous endoscopic decompression for lumbar spinal stenosis. Expert Rev Med Devices 2014; 11:605–616. [DOI] [PubMed] [Google Scholar]
- 6.Nellensteijn J, Ostelo R, Bartels R, et al. Transforaminal endoscopic surgery for lumbar stenosis: a systematic review. Eur Spine J 2010; 19:879–886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nellensteijn J, Ostelo R, Bartels R, et al. Transforaminal endoscopic surgery for symptomatic lumbar disc herniations: a systematic review of the literature. Eur Spine J 2010; 19:181–204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ahn Y, Kim CH, Lee JH, et al. Radiation exposure to the surgeon during percutaneous endoscopic lumbar discectomy: a prospective study. Spine 2013; 38:617–625. [DOI] [PubMed] [Google Scholar]
- 9.Choi G, Modi HN, Prada N, et al. Clinical results of XMR-assisted percutaneous transforaminal endoscopic lumbar discectomy. J Orthop Surg Res 2013; 8:14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Srinivasan D, Than KD, Wang AC, et al. Radiation safety and spine surgery: systematic review of exposure limits and methods to minimize radiation exposure. World Neurosurg 2014; 82:1337–1343. [DOI] [PubMed] [Google Scholar]
- 11.Fan G, Fu Q, Gu G, et al. Radiation exposure to surgeon in minimally invasive transforaminal lumbar interbody fusion with novel spinal locators. J Spinal Disord Tech 2015; 28:E173–180. [DOI] [PubMed] [Google Scholar]
- 12.Gu G, Zhang H, He S, et al. Percutaneous pedicle screw placement in lumbar spine: a comparison study between the novel guidance system and the conventional fluoroscopy method. J Spinal Disord Tech 2015; 28:E522–E527. [DOI] [PubMed] [Google Scholar]
- 13.Gu G, Zhang H, He S, et al. Preoperative localization methods for minimally invasive surgery in lumbar spine: comparisons between a novel method and conventional methods. J Spinal Disord Tech 2013; 26:E277–280. [DOI] [PubMed] [Google Scholar]
- 14.Hoogland T, Van Den Brekel-Dijkstra K, Schubert M, et al. Endoscopic transforaminal discectomy for recurrent lumbar disc herniation: a prospective, cohort evaluation of 262 consecutive cases. Spine 2008; 33:973–978. [DOI] [PubMed] [Google Scholar]
- 15.Lee K, Lee KM, Park MS, et al. Measurements of surgeons’ exposure to ionizing radiation dose during intraoperative use of C-arm fluoroscopy. Spine 2012; 37:1240–1244. [DOI] [PubMed] [Google Scholar]
- 16.Mulconrey DS. Fluoroscopic radiation exposure in spinal surgery: in vivo evaluation for operating room personnel. J Spinal Disord Tech 2013; doi: 101097/BSD0b013e31828673c1. [DOI] [PubMed] [Google Scholar]
- 17.Taher F, Hughes AP, Sama AA, et al. 2013 Young Investigator Award winner: how safe is lateral lumbar interbody fusion for the surgeon? A prospective in vivo radiation exposure study. Spine 2013; 38:1386–1392. [DOI] [PubMed] [Google Scholar]
- 18.Choi HC. Fluoroscopic radiation exposure during percutaneous kyphoplasty. J Korean Neurosurg Soc 2011; 49:37–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jindal T. The risk of radiation exposure to assisting staff in urological procedures: a literature review. Urol Nurs 2013; 33:136–139.147. [PubMed] [Google Scholar]
- 20.Tabaraee E, Gibson AG, Karahalios DG, et al. Intraoperative cone beam-computed tomography with navigation (O-ARM) versus conventional fluoroscopy (C-ARM): a cadaveric study comparing accuracy, efficiency, and safety for spinal instrumentation. Spine 2013; 38:1953–1958. [DOI] [PubMed] [Google Scholar]
- 21.Abdullah KG, Bishop FS, Lubelski D, et al. Radiation exposure to the spine surgeon in lumbar and thoracolumbar fusions with the use of an intraoperative computed tomographic 3-dimensional imaging system. Spine -1078; 37: E1074–1078. [DOI] [PubMed] [Google Scholar]
- 22.Moses ZB, Mayer RR, Strickland BA, et al. Neuronavigation in minimally invasive spine surgery. Neurosurg Focus 2013; 35:E12. [DOI] [PubMed] [Google Scholar]
- 23.Ruetten S, Komp M, Merk H, et al. Use of newly developed instruments and endoscopes: full-endoscopic resection of lumbar disc herniations via the interlaminar and lateral transforaminal approach. J Neurosurg Spine 2007; 6:521–530. [DOI] [PubMed] [Google Scholar]
- 24.Lee DY, Lee SH. Learning curve for percutaneous endoscopic lumbar discectomy. Neurol Med Chir (Tokyo) 2008; 48:383–388. [DOI] [PubMed] [Google Scholar]
- 25.Wang H, Huang B, Li C, et al. Learning curve for percutaneous endoscopic lumbar discectomy depending on the surgeon's training level of minimally invasive spine surgery. Clin Neurol Neurosurg 2013; 115:1987–1991. [DOI] [PubMed] [Google Scholar]
- 26.Wang B, Lü G, Patel AA, et al. An evaluation of the learning curve for a complex surgical technique: the full endoscopic interlaminar approach for lumbar disc herniations. Spine J 2011; 11:122–130. [DOI] [PubMed] [Google Scholar]
- 27.Hsu H-T, Chang S-J, Yang SS, et al. Learning curve of full-endoscopic lumbar discectomy. Eur Spine J 2012; 22:727–733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Chaichankul C, Poopitaya S, Tassanawipas W. The effect of learning curve on the results of percutaneous transforaminal endoscopic lumbar discectomy. J Med Assoc Thai 2012; 95 suppl 10:S206–S212. [PubMed] [Google Scholar]
- 29.Fitousi NT, Efstathopoulos EP, Delis HB, et al. Patient and staff dosimetry in vertebroplasty. Spine 2006; 31:E884–889. [DOI] [PubMed] [Google Scholar]
- 30.Mroz TE, Yamashita T, Davros WJ, et al. Radiation exposure to the surgeon and the patient during kyphoplasty. J Spinal Disord Tech 2008; 21:96–100. [DOI] [PubMed] [Google Scholar]
- 31.Mroz TE, Abdullah KG, Steinmetz MP, et al. Radiation exposure to the surgeon during percutaneous pedicle screw placement. J Spinal Disord Tech 2011; 24:264–267. [DOI] [PubMed] [Google Scholar]
- 32.Bindal RK, Glaze S, Ognoskie M, et al. Surgeon and patient radiation exposure in minimally invasive transforaminal lumbar interbody fusion. J Neurosurg Spine 2008; 9:570–573. [DOI] [PubMed] [Google Scholar]


