Abstract
The intention of this study was to compare the biomechanical characteristics using 5 internal fixation methods used clinically to stabilize a pubic symphysis diastasis (PSD, Tile type B1).
A 3-dimensional finite element model of PSD was simulated using 5 implants, including single superior plate (Single-Plate), superior and anterior plate (Dual-Plate), single cannulated screw (Single-Screw), crossed dual cannulated screws (Cross-Screw), and parallel dual cannulated screws (Para-Screw). Three loads were distributed in all models, including dual-leg standing, single-leg stance, and rotation. To evaluate the biomechanical properties, the construct stiffness, the stress distribution, and the von Misses stress were recorded and analyzed. To evaluate pelvic ring stability, the micromotion of the pubic symphysis and iliosacral joint was analyzed.
Disruption of pubic symphysis dramatically decreased the pelvic ring stability. Cross-screw and Para-Screw showed higher stiffness than other methods. All implants endured the maximum von Misses stress under single-leg stance. For Plate-Screw system, the maximum stress occurred at a place where it strides over pubic symphysis and adjacent Plate-Screw interface. The single implant and Para-Screw had a tendency to fail. Para-Screw showed the best fixation effect under dual-leg conditions. Cross-screw showed superior antishearing force capacity under single-leg stance. Dual-Plate provided maximum antihorizontal rotation. Para-Screw provided the maximum stabilization for the posterior pelvic ring.
This study showed the biomechanical advantages of dual-implant for PSD only from the finite element view. The Para-Screw provided high construct stiffness under 3 load conditions. The single implant and Para-Screw had a tendency to fail. The better anterior and posterior pelvic stabilization were obtained by the dual-implant fixation than other methods. Therefore, the Cross-Screw and Dual-Plate fixation methods should be preferred in the treatment of pubic symphysis from the finite element view.
INTRODUCTION
Traumatic pubic symphysis diastasis (PSD) is an uncommon injury caused by high energy.1 Epidemiologic studies show that PSD accounts for 13% to 16%2 of pelvic ring injuries and 4.6%3 of all fractures. The pubic symphysis is an oligodynamic joint, which consists of bilateral pubic bones and fibrocartilaginous disc. It plays a significant role in maintaining the stability of pelvic ring. The structure provides a strong union between 2 innominate bones in order to maintain the stability of anterior pelvic ring. Many ligaments contribute to pelvic stability, such as anterior sacroiliac, posterior sacroiliac, interosseous sacroiliac, sacrospinous, sacrotuberous, superior pubic, and arcuate pubic ligaments. Generally, the PSD exceeds 25 mm, suggesting pelvic ring instability caused by damaged superior pubic, arcuate pubic, anterior sacroiliac, and sacrospinous ligaments.2 Under such circumstances, the PSD causes pelvic ring instability and surgery is indicated to restore stability.
There are several fixation methods to treat PSD, such as external fixation, tension band wiring, plate fixation, cannulated screw fixation, and so on.1 The Plate-Screw system was considered the gold standard for the treatment of PSD.4 However, this method leads to complications such as iatrogenic nerves and blood vessels injury, wound disorders, spermatic cord injury, and so forth.5,6 In order to avoid these issues, a minimally invasive fixation method was introduced. Mu et al5 reported a minimally invasive technique of percutaneous single or dual cannulated screw fixation, which provides enough stability and reduces complications in PSD. Unfortunately, a high rate (19%–90%) of implant failure, loss of reduction, and revision surgery were reported.1,7
The high rate of fixation failure is attributed to the stresses on pubic symphysis. The pubic symphysis is subjected to a variety of forces by body weight, ligament tension, and muscular traction. The superior pubic symphysis endures shearing and compressive, tensile and torsional forces in single-leg stance, dual-leg standing, and rotation, respectively.8–10 These forces are absorbed and dissipated by the fibrocartilaginous disc and ligaments with intact pubic symphysis. When pubic symphysis is disrupted, the fixation is intended to provide a stable environment for soft-tissue repair. However, the fixation technique associated with sufficient strength and appropriate biomechanical reduction is unclear.
Therefore, the intention of this study was to compare the postoperative biomechanical characteristics among single plate, dual plate, single cannulated screw, crossed dual cannulated screws (Cross-Screw), and parallel dual cannulated screws (Para-Screw) under dual-leg standing, single-leg stance, and rotation conditions used clinically to stabilize a PSD (Tile type B1) by finite element analysis. Furthermore, the pelvic ring stability was evaluated by analyzing the micromotion of the pubic symphysis and iliosacral joint.
METHODS
This study was done at the Provincial Hospital Affiliated to Shandong University in Jinan, Shandong, China and permission was obtained from the hospital Ethics Committee. Authors had to obtain patient consent before enrolling participants in this study.
Finite Element Models and Implants
A 3-dimensional finite element model was developed from computed tomography scan. The DICOM format files of computed tomography scan were processed by MIMICS 15.0 (Materialise, Belgium). An intact pelvis model with anterior sacroiliac, posterior sacroiliac, interosseous sacroiliac, sacrospinous, sacrotuberous, superior pubic, and arcuate pubic ligaments was created to simulate the normal (Nor) condition (Fig. 1A). To simulate the Tile B1 situation, the PSD model was made by removing superior pubic, arcuate pubic, right anterior sacroiliac, right sacrospinous, and right sacrotuberous ligaments from the Nor model (Fig. 1B).11
FIGURE 1.
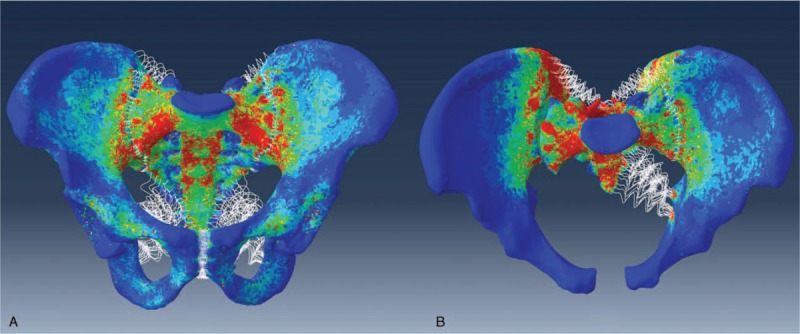
The Nor and PSD models. (A) An intact pelvis model with anterior sacroiliac, posterior sacroiliac, interosseous sacroiliac, sacrospinous, sacrotuberous, superior pubic, and arcuate pubic ligaments was created to simulate the normal condition. (B) To simulate the Tile B1 situation, the PSD model was made by removing superior pubic, arcuate pubic, right anterior sacroiliac, right sacrospinous, and right sacrotuberous ligaments from the intact model. Nor = normal bone, PSD = pubic symphysis diastasis.
Five implants were used in the PSD model, including the single superior plate (Single-Plate), superior and anterior plate (Dual-Plate), single cannulated screw (Single-Screw), Cross-Screw and Para-Screw (Fig. 2). The superior reconstruction plate (Synthes, Oberdorf, Switzerland) was 4-hole and the anterior was 5-hole. The length and diameter of the primary cannulated screws (Synthes, Oberdorf, Switzerland) were 60 and 7.3 mm, respectively. The length and diameter of the additional cannulated screws (Synthes, Oberdorf, Switzerland) were 60, 6.5 mm (Cross-Screw) and 30, 6.5 mm (Para-Screw), respectively. The construction plates and cannulated screws were inserted into the PSD model using the standard surgical technique.5,12 The contact behavior of cortical-screw/bone interfaces was set as a rigid bond and that of plate/bone interfaces as surface-to-surface. The threads and screwheads of cannulated screws were fully fixed into cortical bones. The threads of cortical screws were omitted in order to simplify the models. The intact model without implants had a total of 781,838 elements and 202,616 nodes. The elements for implants were 35,567, 65,388, 20,027, 48,294, and 42,583 for Single-Plate, Dual-Plate, Single-Screw, Cross-Screw, and Para-Screw, respectively. The nodes for implants were 8,604, 15,828, 5,432, 12,394, and 10,784, respectively.
FIGURE 2.
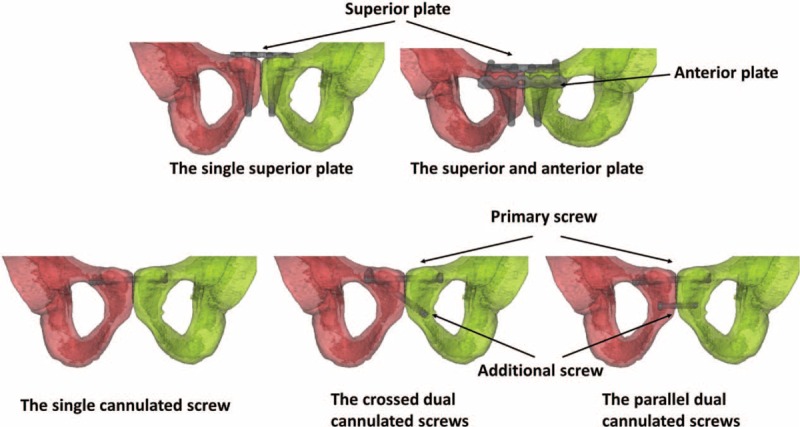
The construction plates and cannulated screws were instrumented into the pubic symphysis diastasis (PSD) model using standard surgical techniques, including the single superior plate, superior and anterior plate, single cannulated screw, crossed dual cannulated screws, and parallel dual cannulated screws.
Finite Element Analysis
The finite element analysis was performed by Abaqus 6.13 (3DS, Waltham, MA). Linear elastic isotropic material properties were assigned to all models and implants. All contact elements were defined as deformable elements. The ligaments were simulated as nonlinear spring elements. The properties of bones, ligaments, and implants are shown in Table 1.13
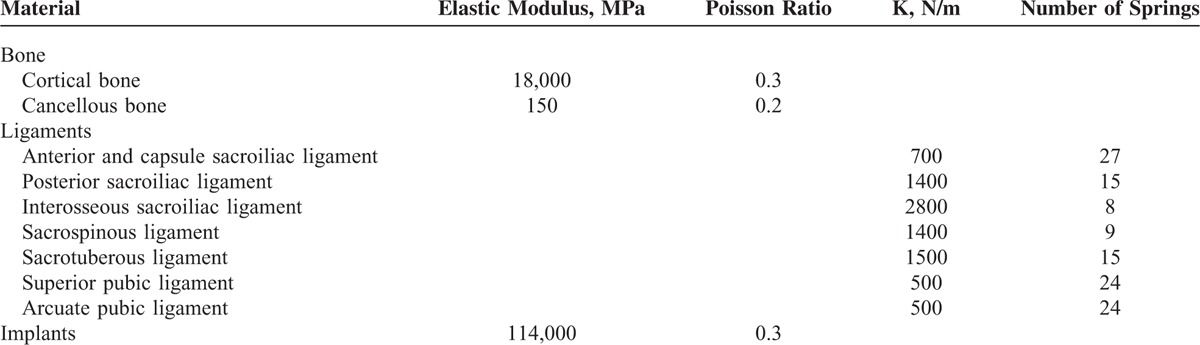
TABLE 1.
Material Properties of Finite Element Models
The superior segment of S1 of models was fixed. To observe the biomechanical characteristics under specific stresses, 3 types of load condition were used in all models (Fig. 3A), including dual-leg standing, single-leg stance, and rotation. To simulate dual-leg standing, a vertical force of 500 N was distributed to the bilateral acetabulums, respectively. To simulate single-leg stance, a vertical force of 750 N was distributed to the right acetabulum. For rotation, a follower load of 500 N and a torque of 7 Nm were applied to the bilateral acetabulums to simulate right rotation.
FIGURE 3.
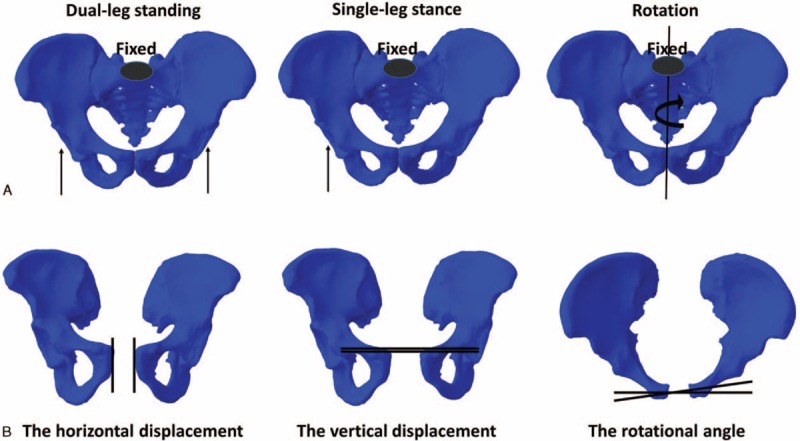
Three types of load were applied in all models and micromotion of the pubic symphysis were recorded. (A) The superior segment of S1 of models was fixed. To simulate dual-leg standing, a vertical force of 500 N was distributed to the bilateral acetabulums, respectively. To simulate single-leg stance, a vertical force of 750 N was distributed to the right acetabulum. For rotation, a follower load of 500 N and a torque of 7 Nm were applied to the bilateral acetabulums to simulate right rotation. (B) The incremental micromotion of the pubic symphysis was recorded to evaluate the stability of anterior pelvic ring. The increment of horizontal displacements under dual-leg standing, the incremental vertical displacements under single-leg stance, and increment of rotational angle under rotation were described.
The biomechanical characteristics of Single-Plate, Dual-Plate, Single-Screw, Cross-Screw, and Para-Screw models were analyzed and compared with the Nor and PSD models. The construct stiffness was used to compare the construct stability. To evaluate the force condition, the stress distribution and the maximum von Misses stresses were described. The stability of pelvic ring was evaluated under different circumstances by recording the micromotion of anterior and posterior pelvic ring. For anterior pelvic ring, the horizontal displacements under dual-leg standing, the vertical displacements under single-leg stance, and increment of rotational angle under rotation were determined and analyzed (Fig. 3B). For posterior pelvic ring, the micromotion of illiosacral joint in horizontal, coronal, and sagittal planes was determined and analyzed.
RESULTS
Biomechanical Characteristics
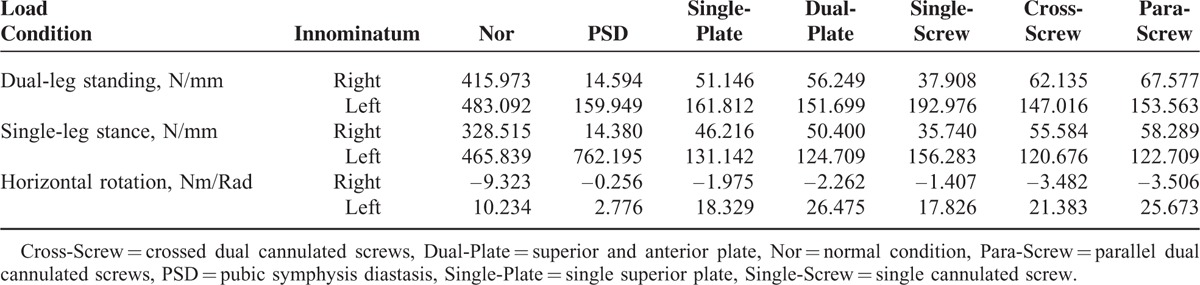
The construct stiffness of the Nor, PSD, Single-Plate, Dual-Plate, Single-Screw, Cross-Screw, and Para-Screw models under dual-leg standing, single-leg stance, and rotation condition is displayed in Table 2. When pubic symphysis was disrupted, the construct stiffness was decreased dramatically under 3 conditions. In general, the construct stiffness was not restored significantly by the 5 internal fixation methods. Dual cannulated screws showed higher stiffness than dual plates, especially in rotational stiffness. The Single-Screw showed almost minimum construct stiffness.
TABLE 2.
The Construct Stiffness of Models
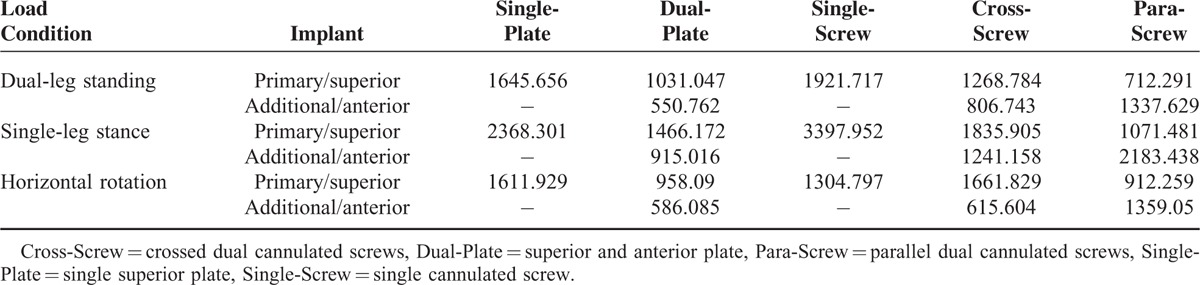
The maximum von Misses stress of implants is described in Figure 4 and Table 3. In general, the implants endured the maximum von Misses stress under single-leg stance. An additional implant was conducive to stress dispersion from a primary implant. Negatively, the additional cannulated screw endured higher stress than the primary cannulated screw in Para-Screw. For Plate-Screw system, the maximum von Misses stress occurred at a place where it strides over pubic symphysis and adjacent Plate-Screw interface. The maximum von Misses stress with the cannulated screw system occurred at the thread-cortical bone interface. Stress concentration appeared on Plate-Screw system, whereas stress equidistribution was observed in the caudomedial part of cannulated screws.
FIGURE 4.
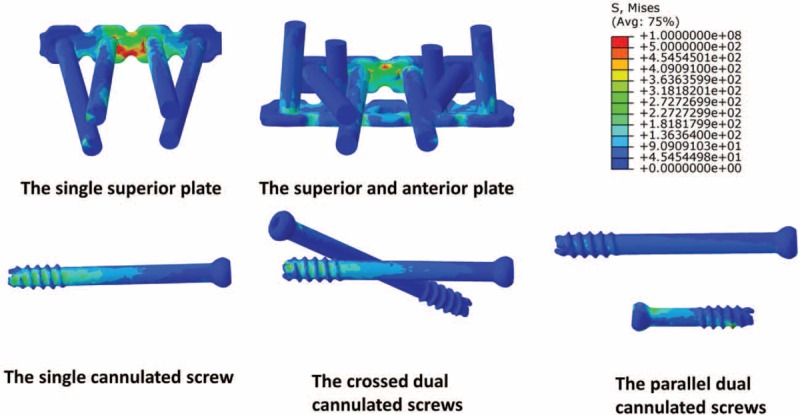
The von Misses stress distribution on 5 implants in dual-leg standing. For Plate-Screw system, the maximum von Misses stress occurred at a place where it strides over pubic symphysis and adjacent Plate-Screw joints. The maximum von Misses stress with the cannulated screw system occurred at the thread-cortical bone interface. Stress concentration appeared on Plate-Screw system, whereas stress equidistribution was observed in the caudomedial part of cannulated screws.
TABLE 3.
The Maximum von Misses Stress of Implants (MPa)
Pelvic Ring Stability
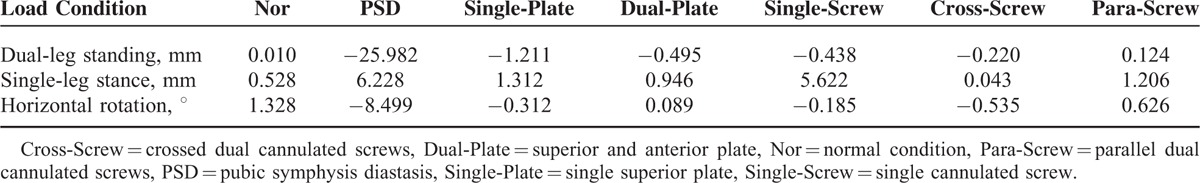
The incremental micromotion of anterior pelvic ring is shown in Table 4. For dual-leg standing, the increment of horizontal displacement was 0.010 mm and −25.982 mm under intact and PSD conditions. Para-Screw showed the best fixation effect (0.124 mm). For single-leg stance, the incremental vertical displacement was increased dramatically in PSD model (6.228 mm) than in Nor model (0.528 mm). In this situation, Cross-Screw showed superior antishearing force capacity (0.043 mm). For rotation, the incremental rotation was increased significantly in PSD model (−8.499°) than in Nor model (1.328°). Dual-Plate offered maximum antihorizontal rotation (0.089°).
TABLE 4.
The Incremental Micromotion of the Anterior Pelvic Ring
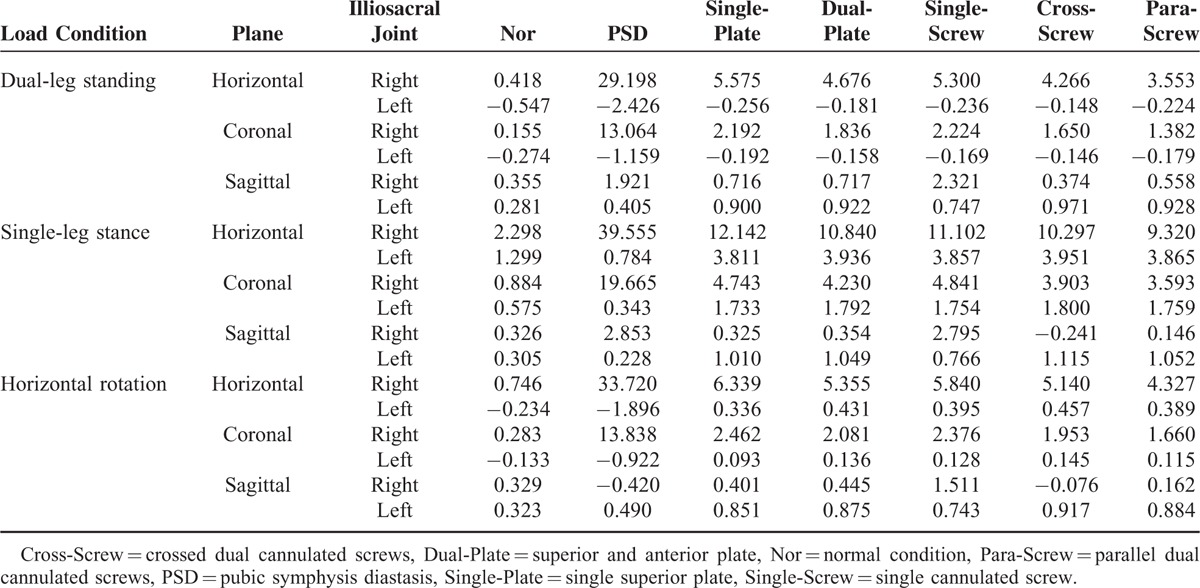
The incremental micromotion of posterior pelvic ring is shown in Table 5. In general, the PSD model showed extreme instability, especially in horizontal plane. The 2 cannulated screws provided the optimal posterior pelvic ring stabilization. The Para-Screw provided the most stability in horizontal, coronal, and sagittal planes under 3 load conditions. Compared with dual cannulated screws, the Dual-Plate also provided the satisfied posterior stabilization. However, the single implant did not achieve posterior pelvic ring stabilization, especially with single cannulated screw.
TABLE 5.
The Incremental Rotational Angle of the Posterior Pelvic Ring (mm)
DISCUSSION
The pubic symphysis is an amphiarthrodial joint, which consists of bilateral pubic bones and intercalated disc. The pubic symphysis maintains anterior pelvic ring stability and protects organs from trauma. The tensile, shearing, and compressive forces caused by trauma are absorbed and dissipated by the fibrocartilaginous disc and ligaments in intact pubic symphysis. It is generally accepted that the pubic symphysis resists tensile stresses in dual-leg standing, compressive and shearing pressures in single-leg stance, and torsional forces in horizontal rotation. The inferior pubic symphysis endures tractional force.9 Pubic symphysis disruption leads to instability. The diastasis exceeding 25 mm due to broken soft tissues is considered an indication for surgery.2
In the current study, we simulated a Tile type B1 model with a disruption of 25.992 mm. In this condition, the stabilization of posterior pelvic ring was affected by the unstable anterior pelvic ring and broken ligaments. Therefore, to evaluate pelvic ring stability, the micromotion of the pubic symphysis and iliosacral joint was recorded and analyzed in this study.
Open reduction and internal fixation with symphysis plates is thought to be the gold standard.4 The Pfannenstiel approach is the most common incision.2 However, this method may lead to complications due to extensive exposure, such as iatrogenic nerves and blood vessel injury, wound disorders, and spermatic cord injury.5Further, it is associated with a high rate of implant failure, loss of reduction, and revisional surgery. The implant failure in pubic symphysis was 19% to 90% in previous reports.7 The high rate of fixation failure can be attributed to the stresses of pubic symphysis. Pubic symphysis disruption represents a discontinuous bridge, not a fracture. A better understanding of the biomechanical effect by the fixation methods should improve treatment outcome.
Our results show that, when pubic symphysis was disrupted, the construct stiffness of bilateral innominate bones was decreased dramatically under 3 conditions. In general, the construct stiffness was not restored by 5 internal fixation methods, this may be attributed to the unstable posterior pelvic ring. In internal fixation, the dual-implant can provide more construct stiffness than the single-implant. Dual cannulated screws showed higher stiffness than dual plates, especially in rotational stiffness. The Single-Screw failed to enhance the stability, which only provided 9.113%, 10.879%, and 15.091% construct stiffness of intact condition under 3 load conditions. These results may be attributed to the inadequacy of single screw to provide a planar fixation observed with plate and dual screws.
The implants endured the maximum von Misses stress under single-leg stance. This phenomenon was attributed to the huge vertical shearing forces. In general, the risk of implant failure depends mainly on excessive stress load. The implant failure in Plate-Screw system involves breakage and screw losing. Stress concentration phenomenon and the maximum von Misses stress occurred at a place where the pubic symphysis strides over and the adjacent Plate-Screw interface in the plate system. In the cannulated screw system, stress concentration was observed on the joints of cortical bone and cannulated screw threads. The caudomedial part of cannulated screw showed stress equidistribution. This result can be explained by the fact that the primary type of failure is a pull-out for cannulated screws. Surprizingly, the additional cannulated screw endured higher stress than the primary cannulated screw in Para-Screw, due to the short length of inefficient stress dispersion. Even though the stresses were dispersed by 2 implants, the place of stress concentration and the maximum stress had a high rate of implant failure, especially for Para-Screw and Single-Plate. In the present study, we inserted a Para-Screw to enhance the stabilization of the lower pubic symphysis. Unfortunately, this method had a tendency to fail due to the huge stresses. Perhaps, the Cross-Screw is a better choice to maintain balance in lower symphysis stability and implant failure. These results were confirmed by previous reports showing 19% to 90% rate of implant failure.7
For dual-leg standing, the increment of horizontal displacement was 0.010 mm and −25.982 mm under intact and PSD conditions. The distance of pubic symphysis was 25.992 mm, which is an indication for surgery. The Para-Screw showed the best fixation effect (0.124 mm) under dual-leg standing with a double pulling force. The incremental vertical displacement of Single-Screw under single-leg stance was 5.622 mm, which meant that a single cannulated screw was not a good option to resist vertical shearing forces. On the contrary, Cross-Screw performed better (0.043 mm) due to an oblique pulling force. For rotation, the Dual-Plate offered maximum antihorizontal rotation due to multiplanar fixation. However, further clinical and biomechanical studies are needed to determine the fixation method in treatment of PSD.
Without intact ligaments, the stabilization of posterior pelvic ring was affected by the fixation methods of anterior pelvic ring. For posterior pelvic ring, the results of this study showed that Single-Plate and Single-Screw displayed the maximum range of motion in horizontal and coronal planes under dual-leg standing. The Single-Screw provided the maximum motion in all the 3 planes. A single implant, especially for cannulated screw, did not provide enough stability for posterior pelvic ring. Similar results were obtained with the single-leg stance and rotation conditions. With the dual-plane or multiplane fixation, the dual implants provided sufficient antirotational stabilization. Due to the oblique pulling force and crossed screws placement, the Cross-Screw provided antirotation and antishearing forces. However, the intact pelvis is a very complex construct which cannot be simulated perfectly by finite element method. In the present study, we mainly concerned the fixation methods rather than other influencing factors (age, sex, body mass index, and so on). So, the conclusion from the present study should not be a guide for clinical practice easily. Large clinical studies must be investigated before this conclusion can be recommended.
There were other limitations in this study. The finite element models were based on skeleton-ligament system and the muscle forces were neglected, similarly to other finite element studies.14–18 A single pelvic model was used for analysis, just the same as other works,14–18 which may avoid the high variation rate of bone and ligament characteristics. There were some limitations to simulating a single-leg stance using a simple method. However, this simple single-leg stance model may provide clinical data of implant failure and pelvic ring stability. To avoid the influence by suboptimal position of implants, the hardwares were inserted into the models using the standard surgical technique. This finite element study has only measured the early postoperative stability, but the long-term biomechanical stabilization has not been evaluated. Considering these limitations, the conclusions should be studied using clinical retrospective analysis and biomechanical testing to determine the feasibility.
In conclusion, this study showed the biomechanical advantages of dual-implant for PSD from the finite element view. The Para-Screw provided high construct stiffness under 3 load conditions. The single implant and Para-Screw had a tendency to fail. The better anterior and posterior pelvic stabilization were obtained by the dual-implant fixation than other methods. Therefore, the Cross-Screw and Dual-Plate fixation methods should be preferred in the treatment of pubic symphysis only from the finite element view.
Footnotes
Abbreviations: Cross-Screw = crossed dual cannulated screws, Dual-Plate = superior and anterior plate, Nor = normal condition, Para-Screw = parallel dual cannulated screws, PSD = pubic symphysis diastasis, Single-Plate = single superior plate, Single-Screw = single cannulated screw.
The authors have no funding and conflicts of interest to disclose.
REFERENCES
- 1.Morris SAC, Loveridge J, Smart DKA, et al. Is fixation failure after plate fixation of the symphysis pubis clinically important? Clin Orthop Relat Res 2012; 470:2154–2160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Aggarwal S, Bali K, Krishnan V, et al. Management outcomes in pubic diastasis: our experience with 19 patients. J Orthop Surg Res 2011; 6:21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Yang NP, Chan CL, Yu IL, et al. Estimated prevalence of orthopaedic fractures in Taiwan – a cross-sectional study based on nationwide insurance data. Injury 2010; 41:1266–1272. [DOI] [PubMed] [Google Scholar]
- 4.Cano-Luis P, Giráldez-Sanchez MA, Martínez-Reina J, et al. Biomechanical analysis of a new minimally invasive system for osteosynthesis of pubis symphysis disruption. Injury 2012; 43:S20–S27. [DOI] [PubMed] [Google Scholar]
- 5.Mu W, Wang H, Zhou D, et al. Computer navigated percutaneous screw fixation for traumatic pubic symphysis diastasis of unstable pelvic ring injuries. Chin Med J 2009; 122:1699–1703. [PubMed] [Google Scholar]
- 6.Ghanayem AJ, Wilber JH, Lieberman JM, et al. The effect of laparotomy and external fixator stabilization on pelvic volume in an unstable pelvic injury. J Trauma Acute Care Surg 1995; 38:396–401. [DOI] [PubMed] [Google Scholar]
- 7.Collinge C, Archdeacon MT, Dulaney-Cripe E, et al. Radiographic changes of implant failure after plating for pubic symphysis diastasis: an underappreciated reality? Clin Orthop Relat Res 2012; 470:2148–2153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Icke C, Koebke J. Normal stress pattern of the pubic symphysis. Anat Cell Biol 2014; 47:40–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Becker I, Woodley SJ, Stringer MD. The adult human pubic symphysis: a systematic review. J Anat 2010; 217:475–487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.MacAvoy MC, McClellan RT, Goodman SB, et al. Stability of open-book pelvic fractures using a new biomechanical model of single-limb stance. J Orthop Trauma 1997; 11:590–593. [DOI] [PubMed] [Google Scholar]
- 11.Stuby FM, Doebele S, Agarwal Y, et al. Influence of flexible fixation for open book injury after pelvic trauma – a biomechanical study. Clin Biomech 2014; 29:657–663. [DOI] [PubMed] [Google Scholar]
- 12.Chen L, Zhang G, Song D, et al. A comparison of percutaneous reduction and screw fixation versus open reduction and plate fixation of traumatic symphysis pubis diastasis. Arch Orthop Trauma Surg 2012; 132:265–270. [DOI] [PubMed] [Google Scholar]
- 13.Zhao Y, Zhang S, Sun T, et al. Mechanical comparison between lengthened and short sacroiliac screws in sacral fracture fixation: a finite element analysis. Orthop Traumatol Surg Res 2013; 99:601–606. [DOI] [PubMed] [Google Scholar]
- 14.He Y, He J, Wang F, et al. Application of additional medial plate in treatment of proximal humeral fractures with unstable medial column: a finite element study and clinical practice. Medicine 2015; 94:e1775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zhang L, Peng Y, Du C, et al. Biomechanical study of four kinds of percutaneous screw fixation in two types of unilateral sacroiliac joint dislocation: a finite element analysis. Injury 2014; 45:2055–2059. [DOI] [PubMed] [Google Scholar]
- 16.Zhu R, Cheng L, Yu Y, et al. Comparison of four reconstruction methods after total sacrectomy: a finite element study. Clin Biomech 2012; 27:771–776. [DOI] [PubMed] [Google Scholar]
- 17.Zhao Y, Li J, Wang D, et al. Comparison of stability of two kinds of sacro-iliac screws in the fixation of bilateral sacral fractures in a finite element model. Injury 2012; 43:490–494. [DOI] [PubMed] [Google Scholar]
- 18.Li C, Zhou Y, Wang H, et al. Treatment of unstable thoracolumbar fractures through short segment pedicle screw fixation techniques using pedicle fixation at the level of the fracture: a finite element analysis. PLoS One 2014; 9:e99156. [DOI] [PMC free article] [PubMed] [Google Scholar]


