Abstract
Inhalation anesthetics provide myocardial protection for cardiac surgery. This study was undertaken to compare the perioperative effects between isoflurane and fentanyl-midazolam-based anesthesia for heart transplantation. A retrospective cohort study was conducted by reviewing the medical records of heart transplantation in a single medical center from 1990 to 2013. Patients receiving isoflurane or fentanyl-midazolam-based anesthesia were included. Those with preoperative severe pulmonary, hepatic, or renal comorbidities were excluded. The perioperative variables and postoperative short-term outcomes were analyzed, including blood glucose levels, urine output, inotropic use, time to extubation, and length of stay in the intensive care units. After reviewing 112 heart transplantations, 18 recipients with fentanyl-midazolam-based anesthesia, and 29 receiving isoflurane anesthesia with minimal low-flow technique were analyzed. After cessation of cardiopulmonary bypass, recipients with isoflurane anesthesia had a significantly lower mean level and a less increase of blood glucose, as compared with those receiving fentanyl-based anesthesia. In addition, there was less use of dobutamine upon arriving the intensive care unit and a shorter time to extubation after isoflurane anesthesia. Compared with fentanyl-midazolam-based anesthesia, isoflurane minimal low-flow anesthesia maintained better perioperative homeostasis of blood glucose levels, less postoperative use of inotropics, and early extubation time among heart-transplant recipients without severe comorbidities.
Keywords: fentanyl, heart transplantation, inhalation anesthetic, isoflurane
1. Introduction
Both inhalation and intravenous anesthetics have been clinically used for cardiac surgery. Numerous clinical trials and meta-analyses[1–5] have demonstrated that inhalation anesthetics can provide less sympathetic activation, more myocardial protection against ischemia-reperfusion injury, and less perioperative metabolic derangement,[6] as compared with high-dose opioids. Isoflurane anesthesia, initially introduced for fast-track cardiac surgery in the 1990s,[7] appears to reduce morbidity and mortality after cardiac surgery as compared with total intravenous anesthesia.[2,3] However, the promising beneficial effects of volatile anesthetics might be limited to isolated low-risk coronary artery bypass grafting surgery and not be applicable to high-risk cardiac surgery.[8]
By contrast, the patients receiving heart transplantation for end-stage heart diseases have a higher risk of preoperative low cardiac output, postbypass ischemia-reperfusion injury, and postoperative hyperlactatemia.[9] A robust donor heart is assumed to provide improved cardiac output and tissue perfusion for post-transplant recovery, especially among those with preoperative stable hemodynamic variables. However, scarce data are available regarding perioperative impacts by different anesthetics.[10,11] Therefore, this retrospective study was undertaken to compare the effects of isoflurane and high dose fentanyl-based anesthesia for heart transplantation.
2. Materials and methods
2.1. Patients
This retrospective cohort study reviewed medical records of heart transplantation from January 1990 to May 2013 after obtaining approval of Tri-Service General Hospital Institutional Review Board (TSGHIRB-1–102–05–051). Patients receiving fentanyl-midazolam-based or isoflurane general anesthesia were included. Those with complicated comorbidities were not analyzed, such as acute hepatic, renal, or cardiopulmonary failure requiring mechanical ventilation, intra-aortic balloon pump, or extracorporeal membrane oxygenation.
2.2. Preoperative management
Routine physiologic monitoring, including 3-lead electrocardiogram, pulse oximetry, and an invasive arterial blood pressure monitoring were set up immediately before anesthesia induction. After tracheal intubation, pulmonary artery catheterization and transesophageal echocardiography were performed for all patients. Inotropic infusion was administered to keep acceptable hemodynamic variables before initiation of cardiopulmonary bypass.
2.3. Fentanyl-midazolam-based anesthesia
General anesthesia was induced with intravenous fentanyl 5 to 15 μg/kg, midazolam 0.05 to 0.1 mg/kg, and pancuronium 0.15 mg/kg. Tracheal intubation was performed after 6 minutes and anesthesia was maintained with infusion of fentanyl 5 to 15 μg/kg/h, midazolam 0.05 mg/kg/h, and pancuronium 0.15 mg/kg/h to keep acceptable hemodynamic variables.
2.4. Isoflurane-based anesthesia
General anesthesia was induced with thiopental 3 to 4 mg/kg or propofol 1 to 1.5 mg/kg, and pancuronium 0.15 mg/kg. After tracheal intubation, an inspired concentration of 2% isoflurane in 6 L/min oxygen flow was administered to wash in functional residual capacity for 5 minutes, and then fresh gas flow was reduced to 0.3 L/min for the maintenance of minimal low flow anesthesia with inspired 2% to 5% isoflurane,[12] according to the hemodynamic status and surgical stimuli. During cardiopulmonary bypass, the perfusionist administered 1.5% to 2.5% isoflurane into the bypass circuit to maintain mean arterial blood pressure 50 to 80 mm Hg. After weaning from bypass, recipients were ventilated again and the rate of fresh gas oxygen flow was kept with 0.3 L/min, along with inspired 2% to 5% isoflurane for anesthesia maintenance.
2.5. Cardiopulmonary bypass
The bypass was set up uniformly for all patients by qualified perfusionists, with routine crystalloid priming, membrane oxygenation, moderate hypothermia (28°C), hemodilution to hematocrit 20% to 25%, and alpha stat pH management. The administration of sodium bicarbonate for correcting metabolic acidosis was performed by the perfusionist according to the arterial blood gas analysis.
2.6. Postoperative recovery
Inotropic drugs, including isoproterenol, dopamine, dobutamine, or epinephrine, were consequently infused to maintain a heart rate between 100 and 120 beats per minute and stable hemodynamic status, while nitroglycerin infusion was temporarily administered to control blood pressure, if needed. Patients were continually intubated upon arriving at the cardiac intensive care unit (ICU), and mechanical ventilation was adjusted to keep normocapnia. The maintenance doses of inotropic drugs and the ventilation status were recorded periodically. According to the routine criteria, extubation was performed after obtaining oriented consciousness, normothermia (patient rewarmed and shivering controlled), and hemodynamic stability with no uncontrolled arrhythmias and no excessive bleeding (as defined by loss of < 100 mL/h).
The perioperative variables were collected, including acid-base status, glucose level, and urine output. Postoperative inotropic use, time to extubation, lengths of ICU and hospital stay, and 30-day mortality were also recorded from the hospital's registry database.
2.7. Statistical analysis
The patient demographic data and perioperative variables were summarized as mean ± SD. Student t test was used for determining the significance of parametric values, and the Mann–Whitney U test, for nonparametric values. The chi-square test was used for postoperative events. A P value of less than 0.05 was considered statistically significant.
3. Results
In total, 58 heart transplant recipients received high-dose fentanyl anesthesia and 54 patients received isoflurane anesthesia (Fig. 1). After excluding those with preoperative severe pulmonary, hepatic, or renal comorbidities, 29 with isoflurane anesthesia (isoflurane group) and 18 with fentanyl-midazolam-based anesthesia (fentanyl group) were analyzed.
Figure 1.
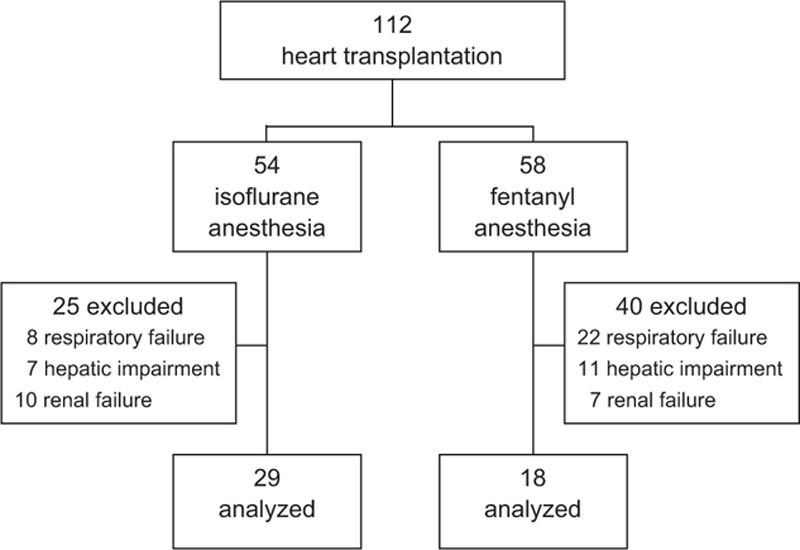
Progress of the enrolled and analyzed patients.
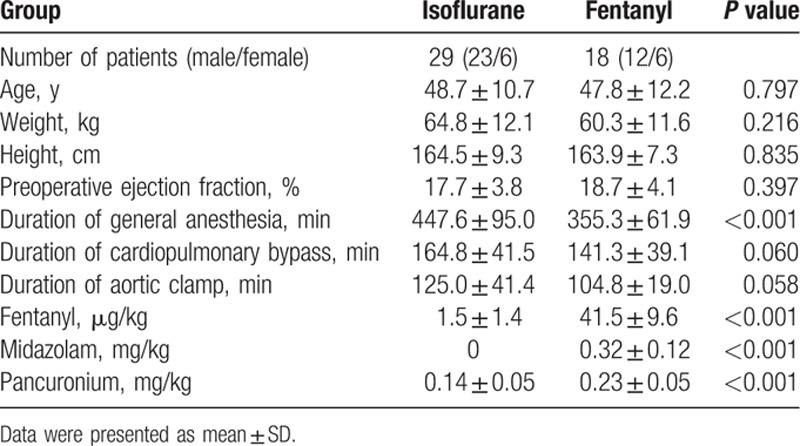
Table 1 demonstrates comparable demographic data and perioperative settings in both groups, with the exception of significantly longer duration of general anesthesia and much less consumption of fentanyl and pancuronium in the isoflurane group.
Table 1.
Patient demographic data.
The perioperative variables and postoperative outcomes are shown in Table 2. After cessation of cardiopulmonary bypass, the isoflurane group had a significantly lower level of blood glucose, with much less elevation of glucose level. The fentanyl group had a greater decrease of bicarbonate level and a lower amount of urine output during cardiopulmonary bypass, but without statistical significance.
Table 2.
Perioperative variables and postoperative outcomes in heart transplant patients receiving isoflurane or fentanyl-based anesthesia.
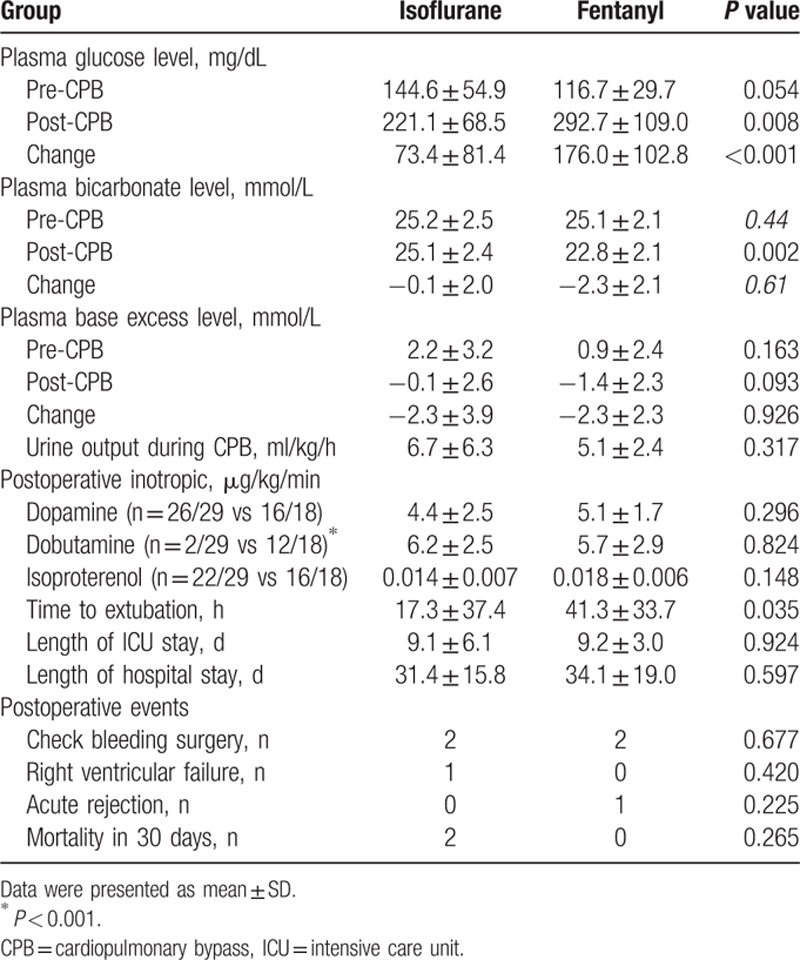
Regarding postoperative outcomes, a significantly less use of dobutamine (2/29 vs 12/18) upon arriving ICU was recorded in the isoflurane group. The isoflurane group had a shorter time to extubation, but the lengths of ICU and hospital stay were comparable in the 2 groups. There were no significant differences in major cardiac events and 30-day mortality in both groups.
4. Discussion
In this retrospective cohort study of heart transplantation, isoflurane anesthesia with minimal low-flow technique was observed to provide less perioperative hyperglycemia, less postoperative inotropic use, and a shorter time to extubation in the ICU, as compared with fentanyl-midazolam-based anesthesia.
High-dose opioids have been applied for cardiac surgery since the late 1980s on account of the isoflurane-induced coronary steal phenomenon in a canine model.[13] The subsequent human studies demonstrated that volatile anesthetics were relatively weak coronary vasodilators that are incapable of causing coronary steal under the vast majority of clinical conditions.[14] Among heart transplant recipients, pharmacodynamic properties of anesthetic agents should be taken into consideration during induction and maintenance for the left ventricle function. Also, the implanted heart is prone to a long duration of myocardial ischemia and reperfusion injury. The volatile anesthetics at clinical concentrations may exert protection against perioperative myocardial ischemia by a mechanism independent of myocardial oxygen balance.[1] The depressant effects of volatile anesthetics may decrease myocardial oxygen demand of a reactivated donor heart and therefore have beneficial effects on the extent of reperfusion injury, especially when used early in the reperfusion period.[15] In this study, less postoperative requirement of dobutamine was observed in patients following isoflurane anesthesia, indicating better perioperative cardioprotection during heart transplant surgery.
Heart-transplant recipients suffer from symptomatic heart failure, with physiologic consequences of activated renin-angiotensin system with fluid and sodium retention, and elevated sympathetic tone with resultant vasoconstriction.[10] During cardiopulmonary bypass, the stress response is difficult to suppress with sufentanil or fentanyl, perhaps due to no dose–response relationship for opioid-associated control of the stress response.[16] The increased incidence of cardiac arrhythmia in the heart transplant recipients with opioid-based anesthesia reflects less sympathetic depression.[11] The less stress reduction by opioid-based anesthesia may also increase endogenous catecholamine production and stimulate an increased blood glucose concentration and glycolysis, resulting in lactate production and metabolic acidosis.[17] In our study, less hyperglycemia was observed, indicating less stress response by optimal anesthetic depth following isoflurane anesthesia with minimal low-flow technique. However, it only provided short-term beneficial effects in these uncomplicated heart-transplant recipients, which effects were consistent with those receiving low-risk coronary artery bypass grafting surgery and were not applied to high-risk cardiac surgery.[8]
4.1. Limitations
First, the extubation protocol after surgery was not available in the medical records. When high-dose opioid anesthesia was used in the cardiac surgery, the incidences of intraoperative awareness[18] and delayed extubation[19] were higher, which may impede the approach of fast-track to cardiac patients. As expected, the time to extubation was significantly shorter in the isoflurane group in this study. Second, perioperative awareness was not recorded in this retrospectively study. High-dose opioids do not produce or potentiate anterograde or retrograde amnesia.[10] It is thus essential to use amnestic agents as supplements, such as benzodiazepines or inhalation anesthetics. The incident of perioperative awareness was routinely inquired after surgery, but not compulsorily recorded before discharge, which were not detected in the records of these relatively stable patients. It should be a required item in the postoperative medical records for quality improvement. Third, all of our heart-transplant recipients were cared by experienced cardiac anesthesiologists. The rate of death or major complications among patients undergoing coronary artery bypass graft surgery varies markedly across anesthesiologists.[20] Patients managed by low-performance anesthesiologists experienced nearly twice the rate of death or serious complications, as patients managed by high-performance anesthesiologists. This performance gap was not observed in our patients.
In conclusion, this retrospective analysis demonstrated low-risk heart-transplant recipients receiving isoflurane anesthesia had less metabolic stress, less inotropic requirement, and shorter extubation time, as compared with those receiving fentanyl-based anesthesia.
Acknowledgments
This work was funded by grants from Tri-Service General Hospital (TSGH-C103–184 and TSGH-C105–100).
Footnotes
Abbreviation: ICU = intensive care unit.
Chien-Sung Tsai contributed equally to this work.
The authors have no conflicts of interest to declare.
References
- 1.Pagel PS. Myocardial protection by volatile anesthetics in patients undergoing cardiac surgery: a critical review of the laboratory and clinical evidence. J Cardiothorac Vasc Anesth 2013; 27:972–982. [DOI] [PubMed] [Google Scholar]
- 2.Landoni G, Greco T, Biondi-Zoccai G, et al. Anaesthetic drugs and survival: a Bayesian network meta-analysis of randomized trials in cardiac surgery. Br J Anaesth 2013; 111:886–896. [DOI] [PubMed] [Google Scholar]
- 3.Bignami E, Greco T, Barile L, et al. The effect of isoflurane on survival and myocardial infarction: a meta-analysis of randomized controlled studies. J Cardiothorac Vasc Anesth 2013; 27:50–58. [DOI] [PubMed] [Google Scholar]
- 4.Van Allen NR, Krafft PR, Leitzke AS, et al. The role of Volatile Anesthetics in Cardioprotection: a systematic review. Med Gas Res 2012; 2:22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hausenloy DJ, Boston-Griffiths E, Yellon DM. Cardioprotection during cardiac surgery. Cardiovasc Res 2012; 94:253–265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lu CC, Ho ST, Wang JJ, et al. Minimal low-flow isoflurane-based anesthesia benefits patients undergoing coronary revascularization via preventing hyperglycemia and maintaining metabolic homeostasis. Acta Anaesthesiol Sin 2003; 41:165–172. [PubMed] [Google Scholar]
- 7.Glass PS. Pharmacokinetic and pharmacodynamic principles in providing “fast-track” recovery. J Cardiothorac Vasc Anesth 1995; 9:16–20. [PubMed] [Google Scholar]
- 8.Landoni G, Guarracino F, Cariello C, et al. Volatile compared with total intravenous anaesthesia in patients undergoing high-risk cardiac surgery: a randomized multicentre study. Br J Anaesth 2014; 113:955–963. [DOI] [PubMed] [Google Scholar]
- 9.Hsu YC, Hsu CH, Huang GS, et al. Extreme hyperlactatemia after heart transplantation: one center's experience. Transplant Proc 2015; 47:1945–1948. [DOI] [PubMed] [Google Scholar]
- 10.Ramakrishna H, Rehfeldt KH, Pajaro OE. Anesthetic pharmacology and perioperative considerations for heart transplantation. Curr Clin Pharmacol 2015; 10:3–21. [DOI] [PubMed] [Google Scholar]
- 11.Demas K, Wyner J, Mihm FG, et al. Anaesthesia for heart transplantation. A retrospective study and review. Br J Anaesth 1986; 58:1357–1364. [DOI] [PubMed] [Google Scholar]
- 12.Lu CC, Tsai CS, Hu OY, et al. Pharmacokinetics of isoflurane in human blood. Pharmacology 2008; 81:344–349. [DOI] [PubMed] [Google Scholar]
- 13.Buffington CW, Romson JL, Levine A, et al. Isoflurane induces coronary steal in a canine model of chronic coronary occlusion. Anesthesiology 1987; 66:280–292. [DOI] [PubMed] [Google Scholar]
- 14.Tanaka K, Ludwig LM, Kersten JR, et al. Mechanisms of cardioprotection by volatile anesthetics. Anesthesiology 2004; 100:707–721. [DOI] [PubMed] [Google Scholar]
- 15.Kato R, Foex P. Myocardial protection by anesthetic agents against ischemia-reperfusion injury: an update for anesthesiologists. Can J Anaesth 2002; 49:777–791. [DOI] [PubMed] [Google Scholar]
- 16.Philbin DM, Rosow CE, Schneider RC, et al. Fentanyl and sufentanil anesthesia revisited: how much is enough? Anesthesiology 1990; 73:5–11. [DOI] [PubMed] [Google Scholar]
- 17.Handy J. The origin and interpretation of hyperlactataemia during low oxygen delivery states. Crit Care 2007; 11:104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hilgenberg JC. Intraoperative awareness during high-dose fentanyl--oxygen anesthesia. Anesthesiology 1981; 54:341–343. [DOI] [PubMed] [Google Scholar]
- 19.Bell J, Sartain J, Wilkinson GA, et al. Propofol and fentanyl anaesthesia for patients with low cardiac output state undergoing cardiac surgery: comparison with high-dose fentanyl anaesthesia. Br J Anaesth 1994; 73:162–166. [DOI] [PubMed] [Google Scholar]
- 20.Glance LG, Kellermann AL, Hannan EL, et al. The impact of anesthesiologists on coronary artery bypass graft surgery outcomes. Anesth Analg 2015; 120:526–533. [DOI] [PubMed] [Google Scholar]


