Abstract
Dental pain and tooth loss are global public health concerns. However, there have been no large cross-sectional epidemiologic studies of a representative sample of an entire country's populations. The purpose of this study was to evaluate the relationships between dental pain and tooth loss with health-related quality of life (HRQOL) using a well characterized, nationally representative, population-based study.
This study analyzed data of 3924, representing 21,836,566 adults from the 2012 Korea National Health and Nutrition Examination Survey. Subjects were divided into 4 groups as follows: tooth loss of up to 8 teeth without dental pain, tooth loss of up to 8 teeth with dental pain, tooth loss of 8 to 28 teeth without dental pain, and tooth loss of 8 to 28 teeth with dental pain. Logistic regression was applied to estimate the adjusted odds ratios (ORs) and 95% confidence intervals (CI), controlling for a range of covariates.
Among the 3924 subjects, representing an estimated 21,836,566 adults, the prevalence of tooth loss of 8 to 28 teeth was 24.6% and the prevalence of dental pain was 35%. The tooth loss of 8 to 28 teeth with dental pain group showed the highest level of impaired HRQOL in all 5 dimensions, and the tooth loss up to 8 teeth without dental pain group showed the lowest level. The proportion of both groups without dental pain decreased significantly from the younger age to older age group. After adjustment for sociodemographic factors, the ORs (95% CI) of mobility, self-case, usual activity, pain/discomfort, and anxiety/depression were 1.93 (1.32–2.84), 1.90 (1.25–2.90), 1.46 (0.88–2.43), 1.48 (0.88–2.49), and 1.46 (0.85–2.51) in tooth loss of 8 to 28 teeth with dental pain group. Although the ORs of tooth loss of 8 to 28 teeth without dental pain group did not significantly increase.
Dental pain and tooth loss has a considerable impact of HRQOL in the Korean adult population. In our study, HRQOL is more closely associated with dental pain than with tooth loss.
Keywords: dental pain, general population, health-related quality of life, Korea National Health and Nutrition Examination Survey, tooth loss
1. Introduction
Dental pain indicates that “toothache” originating from innervated tissues of a tooth or immediately adjacent to it.[1,2] Reversible or irreversible pulpitis can cause toothache, acute, or chronic periodontitis, and symptomatic 3rd molars also can cause toothache. Dental pain is the major cause of impairment of daily activity because individuals who suffer from dental pain have difficulty in chewing foods and have trouble sleeping.[1,3] Therefore, dental pain has social and psychological impacts that can reduce health-related quality of life (HRQOL).[4,5]
Previous studies have demonstrated the impact of tooth loss on HRQOL.[6–9] The loss of natural teeth can compromise normal chewing, speaking, laughing, appearance, self-image, and social interaction. In a recent systematic review, it was concluded that tooth loss impacts on quality of life independently of the instrument used to measure QOL.[10]
The EuroQol Group developed 5-dimension instrument (The EuroQoL 5-dimension [EQ-5D]) to standardize nondisease-specific instrument for describing and valuing HRQOL. The EQ-5D has been translated and used by an increasing number of researchers in various countries.[11,12]
The aim of this study was to analyze the association of tooth loss and dental pain with HRQOL based on the EQ-5D in a well characterized, nationally representative, population-based study. In addition, the prevalence of tooth loss and dental pain and its potential risk factors, including socioeconomic measurements, were also evaluated based on the EQ-5D.
2. Materials and methods
2.1. Survey overview and study subjects
This study analyzed data from the 2012 Korea National Health and Nutrition Examination Survey (KNHANES), a nationwide survey that has been performed since 1998 by the Division of Chronic Disease Surveillance at the Korean Center for Disease Control and Prevention. The KNHANES, designed to assess national health and nutritional levels, consists of a health interview, health examination, and a nutritional assessment, which are carried out by trained interviewers and examiners. The survey subjects were randomly selected using stratified, multistage, and cluster-sampling designs, with proportional allocation based on geographic area, gender, and age from the 2005 National Census Registry, to represent the entire noninstitutionalized civilian population in Korea.
The Oral Health Examination Survey was performed by 30 Korea Centers for Disease Control public health dentists. Public health dentists serve a 3-year period in rural health centers in place of military service in Korea. Dentists were trained in theoretical, photographic, and modular education principles to obtain reliable oral health interview data and clinical examination survey data. Dentists examined the subject's oral health only and were not aware of other health interview survey results. During the 4th simulated screening tests, the reliability of the trained dentists in terms of dental status was 0.94.
All participants signed an informed consent form, and this study was approved by the Institutional Review Board of the Seoul St. Mary's Hospital, Catholic University of Korea, Seoul, Korea (KC14QISI0661). Of the 5,757 subjects who participated in both a health interview and a health examination, we excluded 1,833 subjects with missing data and under 40 years old. Thus, a total of 3,924 individuals participated in the study in the general population group, representing an estimated 21,836,566 adults aged 40 years and over.
2.2. Oral health behaviors and status
Oral health behaviors such as daily tooth brushing frequency, the use of oral hygiene devices (floss, interdental brush, and mouthwash), and the use of oral health services were assessed. Daily tooth brushing frequency was categorized into 4 groups: less than once a day, once a day, twice a day, and 3 or more times a day. Answers regarding the use of oral hygiene devices were categorized into 2 groups: yes and no. Questions on the use of oral health services included questions on oral health screening during the previous year and answers were categorized into 2 groups: yes and no.
Periodontal status and caries in permanent teeth were assessed clinically during an oral health examination. The World Health Organization Community Periodontal Index was used to assess periodontal treatment needs and defined subjects with periodontal treatment needs as having a Community Periodontal Index code ≥3. Oral health status including self-perceived oral health status, presence of mastication problems, and presence of speaking problems were determined from an oral health interview. Self-perceived oral health status was assessed with a 5-point scale: subjects with “very poor” or “poor” oral health status were classified as unhealthy, those with “fair” were classified as fair, and those with “good” or “very good” were classified as healthy. Mastication and speaking problems were assessed using a 5-point scale. The answers were classified into 3 groups: “very uncomfortable” and “uncomfortable” were categorized into uncomfortable, “fair” was categorized into fair, and “not uncomfortable” and “not uncomfortable at all” were categorized into comfortable.
2.3. Sociodemographic variables
The sociodemographic characteristics in this study included age, gender, body mass index (BMI), physical activity, marital status, education level (0–9 years, ≥10 years), and monthly household income.[13] In addition, subjects were asked about current smoking status and alcohol consumption during the previous year. “Yes, I smoke” and “I smoke occasionally” were categorized into the current smoker group. In terms of alcohol consumption status, “2 to 3 times a week” and “more than 4 times a week” were categorized into the heavy drinker group.
2.4. Dental pain
Dental pain was defined as a dull and aching tooth, throbbing tooth pain, or pain in the teeth when consuming hot or cold drinks or foods during the previous year.
2.5. Tooth loss
Tooth loss was categorized into 2 groups: “tooth loss of up to 8 teeth” and “tooth loss of 8 to 28 teeth.”
2.6. Quality of life measurements
QOL was evaluated with the EQ-5D and EuroQoL visual analogue scale (EQ-VAS), used with the permission of the EuroQol Group.[14] The EQ-5D instrument has been previously used in Korea, and the validation of the Korean version was demonstrated in previous study.[15] These questionnaires were included in the KNHANES and used for the evaluation of QOL in the Korean population.[16–18]
The EQ-5D questionnaire includes a simple self-classifier section that assesses 5 dimensions, mobility, self-care, usual activities, pain/discomfort, and anxiety/depression, with higher scores reflecting a lower level of HRQOL. The original responses to the EQ-5D, such as “no problems,” “some/moderate problems,” “severe/extreme problems,” and “unable to function,” were reclassified into 2 categories: no problems and any problems.
The EQ-5D index scores were calculated using a formula to estimate the weighted value in the EQ-5D.[19] A higher EQ-5D index score indicated a higher health-related QOL. The EQ-5D index scores ranged from −0.171 (severe problems in all five dimensions) to 1.0 (no problem in any dimension), on a scale where 0 indicates death and 1.0 indicates perfect health. Negative values indicate a health status worse than death. The EQ-VAS is a 20-cm visual analogue scale on which respondents record their perceptions of overall health. EQ-VAS scores range from 0 (worst imaginable health) to 100 (best imaginable health).
2.7. Statistical analyses
Statistical analyses were conducted using the SAS software version 9.2 (SAS Institute Inc., Cary, NC) to account for the complex sampling design and to provide nationally representative prevalence estimates. All data were presented as the mean ± standard error or proportions (standard error) for continuous or categorical variables, respectively. We compared the differences in general characteristics between the 4 groups according to the presence of dental pain and tooth loss using the Chi-square test for categorical data and the Student t test for continuous data.
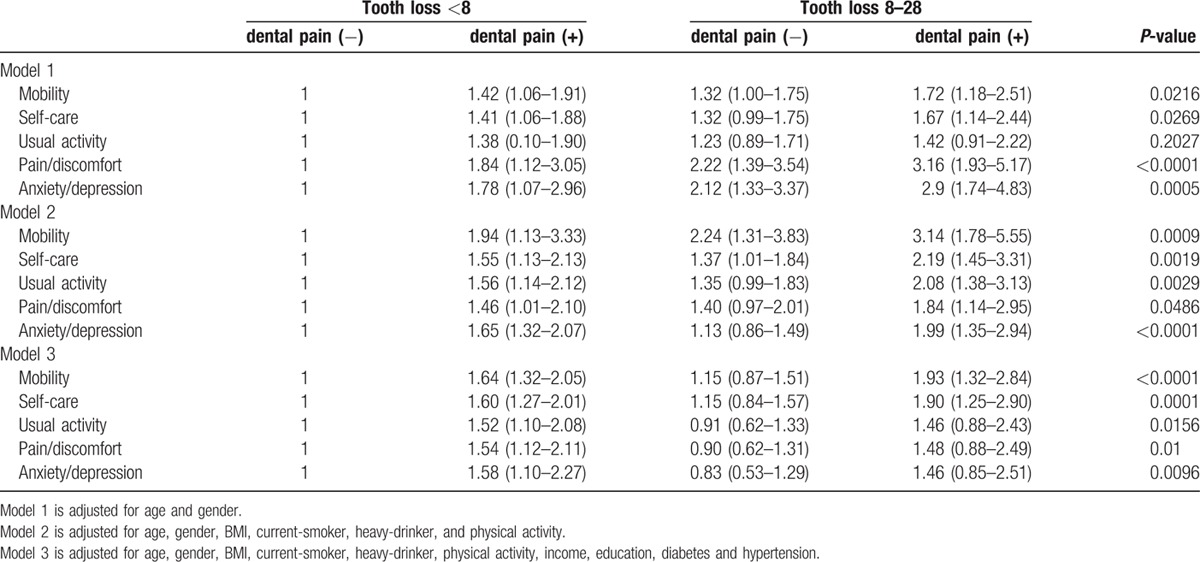
We used multiple logistic regression analyses to examine the association between dental pain and tooth loss with HRQOL. The adjusted odds ratios (ORs) and 95% confidence intervals for dental pain were calculated using tooth loss of up to 8 teeth without dental pain as the reference group.
Calculations were made adjusting for age, gender, and sociodemographic factors, current smoking status, and alcohol consumption. Model 1 included only basic variables (age and gender), model 2 included the variables in model 1 with the addition of BMI, current smoker, heavy drinker, and physical activity. Model 3 included the variables in model 2 with addition of income, education, diabetes, and hypertension. P-values of less than 0.05 were considered statistically significant.
3. Results
3.1. General characteristics of the study population
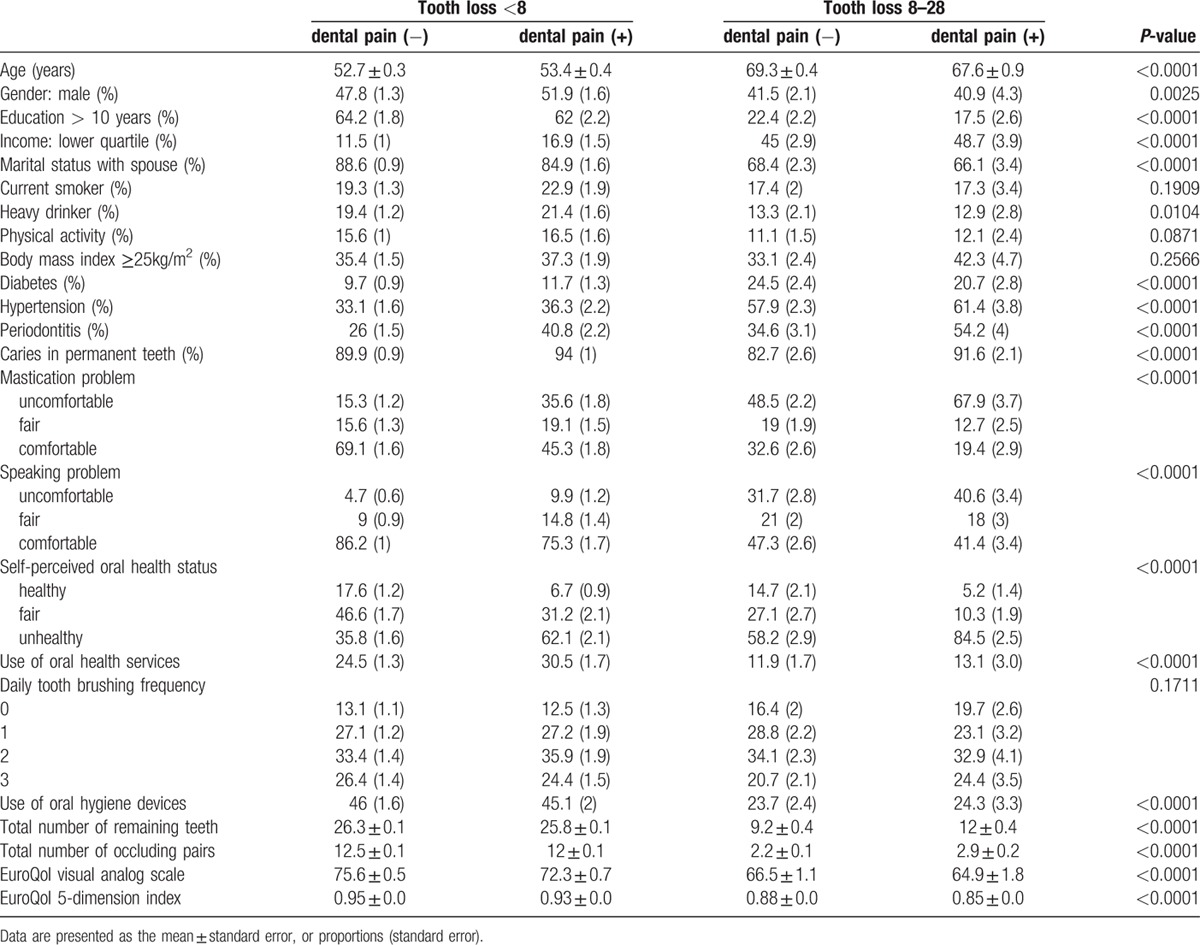
Among the weighted 21,836,566 subjects, the prevalence of tooth loss of 8 to 28 teeth was 24.6% and the prevalence of dental pain was 35%. In both groups with dental pain and without dental pain, subjects with tooth loss of 8 to 28 teeth were older and less likely to be educated, less likely to be married, more likely to have a low income, and more likely to have a chronic disease such as diabetes or hypertension compared with subjects with tooth loss of up to 8 teeth. Subjects with tooth loss of 8 to 28 teeth were more likely to have speaking and mastication problems, and less likely to use oral health services and oral hygiene devices (Table 1). In both the tooth loss of up to 8 teeth and tooth loss of 8 to 28 teeth groups, subjects with dental pain had a higher percentage of periodontitis, decayed-missing-filled index, and poor self-perceived oral health status.
Table 1.
Analysis of factors potentially associated with tooth loss and dental pain (n = 21,836,566; weighted).
3.2. EQ-5D scores according to dental pain and tooth loss
The tooth loss of 8 to 28 teeth with dental pain group showed the highest level of impaired HRQOL in all 5 dimensions of EQ-5D, and the tooth loss up to 8 teeth without dental pain group showed the lowest level of impaired HRQOL (mobility, P < 0.0001; self-care, P < 0.0001; usual activity, P < 0.0001; pain/discomfort, P < 0.0001; and anxiety/depression, P = 0.0004). All 4 subgroups showed higher level of impaired HRQOL in pain/discomfort dimension than other dimensions of EQ-5D (Fig. 1).
Figure 1.
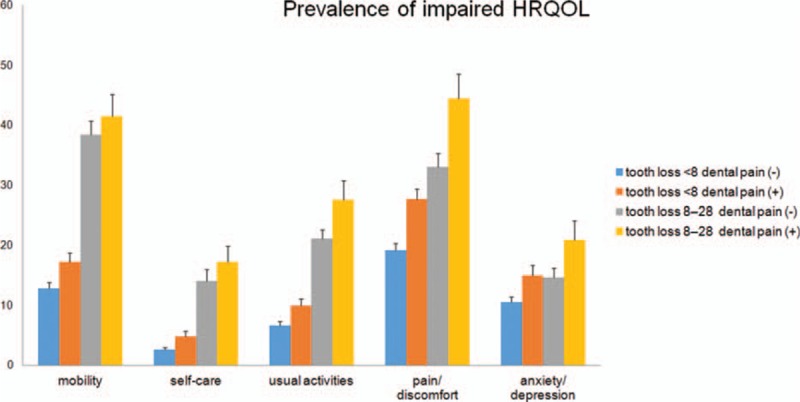
Prevalence of impaired health-related quality of life according to four subgroups based on tooth loss and dental pain. Percentage of subjects who responded “some or extreme problems” in each dimension of the EQ-5D (mobility, P < 0.0001; self-care, P < 0.0001; usual activity, P < 0.0001; pain/discomfort, P < 0.0001; anxiety/depression P = 0.0004). Bars represent standard error.
We analyzed the 4 subgroups according to age. The proportion of both groups without dental pain (tooth loss of up to 8 teeth without dental pain group and tooth loss of 8 to 28 teeth without dental pain group) decreased significantly from the younger age to older age group. Although the proportion of both groups with dental pain (tooth loss of up to 8 teeth with dental pain group and tooth loss of 8 to 28 teeth with dental pain group) increased significantly with age (Fig. 2, P for trend <0.0001).
Figure 2.
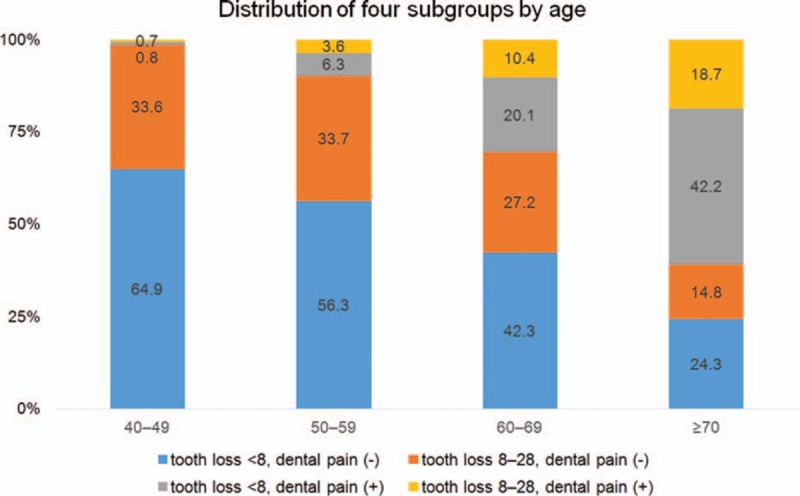
The distribution of the four subgroups according to age groups (P for trend < 0.001).
We analyzed the EQ-5D index and EQ-VAS by the number of remaining teeth. The EQ-5D index and EQ-VAS were low when the remaining number of teeth was less than 5, and were high when the remaining number of teeth was more than 20. The EQ-5D and EQ-VAS levels increased linearly increasing number of remaining teeth (Fig. 3).
Figure 3.
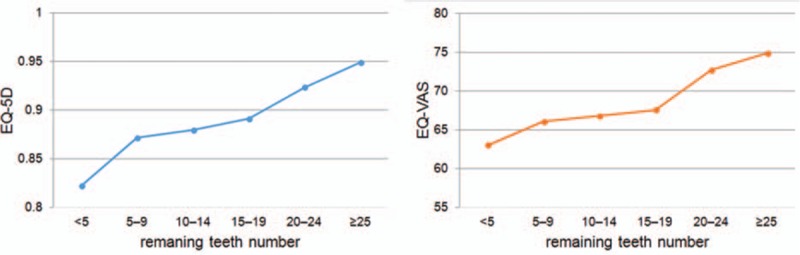
The EQ-VAS and EQ-5D index according to the number of remaining teeth (P for trend < 0.001).
3.3. Multivariable analyses for the associations between the EQ-5D and dental pain and tooth loss
After adjustment for sociodemographic factors such as age and gender (model 1), the ORs of the EQ-5D increased according to the following order, tooth loss of up to 8 teeth without dental pain, tooth loss of up to 8 with dental pain, and tooth loss of 8 to 28 teeth with dental pain. After adjusting for BMI, current smokers, heavy drinkers, physical activity (model 2), the trend of ORs were same. However, the ORs of tooth loss of 8 to 28 teeth without dental pain group did not significantly increase. Adding other factors such as lower quartile income, education level, diabetes and hypertension (model 3), the ORs (95% confidence interval) of mobility, self-case, usual activity, pain/discomfort, and anxiety/depression were 1.93 (1.32–2.84), 1.90 (1.25–2.90), 1.46 (0.88–2.43), 1.48 (0.88–2.49), and 1.46 (0.85–2.51) in tooth loss of 8 to 28 teeth with dental pain group (Table 2).
Table 2.
Adjusted odd ratios and 95% confidence intervals for health-related quality of life (n = 21,836,566; weighted).
4. Discussion
The purpose of this study was to investigate the association between tooth loss and dental pain with HRQOL using a well characterized, nationally representative, population-based study. In this study, we found that subjects with tooth loss and dental pain appear to have a greater risk in HRQOL than those who simply have tooth loss or dental pain. HRQOL is more closely associated with dental pain than with tooth loss.
In this cohort, the tooth loss of 8 to 28 teeth with dental pain group showed a higher proportion of subjects who responded “some or extreme problems” in all 5 dimensions of the EQ-5D than the other 3 groups by univariate analysis (Fig. 1). Subjects with dental pain regardless of tooth loss numbers were older that those without dental pain (Fig. 2). The older age group generally had more comorbidities and other risk factors; therefore, these conditions might also be associated the much poorer HRQOL in older subjects with dental pain than in younger subjects. However, after adjusting for age and gender, the tooth loss of 8 to 28 teeth groups also showed increased levels in all 5 dimensions of HRQOL (Table 2, model 1). In a previous study, Steele et al[6] found that age and tooth loss had independent effects on HRQOL. In this study, HRQOL in the tooth loss of 8 to 28 teeth with dental pain group was significantly impaired compared with that in the tooth loss of up to 8 teeth with no dental pain group. However, using multiple logistic regression analyses after adjusting for comorbidities, there was no significant effect of the tooth loss of 8 to 28 teeth without dental pain group in all 5 dimensions of HRQOL (Table 2, model 3). Our data indicate that HRQOL is more closely related with dental pain than with tooth loss.
The parameter of “number of lost teeth” has been thought to be the most important predictor for assessing the HRQOL. For example, the variable of missing teeth number was significantly associated with the HRQOL scores independent of gender, age, and denture wearing in Japanese young and middle-aged adults.[20] However, in Sri Lanka older adults,[21] “wearing denture” and “having halitosis” were significant predictors of the HRQOL score, and only weak association was observed between the “number of missing teeth” and HRQOL. Recently, Batista el al[9] demonstrated that the HRQOL can be differently percepted even when the number of lost teeth was same. They showed the highest HRQOL score in “lost 13 to 31 teeth” group. However, “lost up to 12 teeth including any anterior teeth” group showed higher scores than “lost up to 12 posterior teeth” group. Therefore, they insisted that impact of tooth loss has to be evaluated quantitatively and qualitatively. Our study classified tooth loss into “tooth loss of up to 8 teeth” and “tooth loss of 8 to 28 teeth,” and we found that the “tooth loss of 8 to 28 teeth” group had relatively lower level of HRQOL. The 20 or more remaining teeth threshold has been regarded as a functional dentition for some years. Because the subjects with 20 or more natural teeth were assumed to have a good masticate capability and nutritional intake.[22,23] Other studies have found that chewing ability was impaired in subject with less than 20 well-distributed teeth or 10 occluding pairs of teeth.[24,25]
Our study reflects that subjects with dental pain regardless of tooth loss experience more impaired HRQOL than subjects without dental pain (Fig. 1). Tooth loss has been considered as an important factor in global health and HRQOL;[9,10] however, dental pain had more important negative impact of HRQOL in this study. Furthermore, many patients with orofacial pain including dental pain are known to suffer from insomnia.[26] Therefore, dental pain should not be considered in isolation. Preventive and treatment approaches for reducing dental pain have positive effects on general health condition.
Some limitations have to be considered in a discussion about the results of this study. First, there is possibility of temporal relationship between dental pain and tooth loss with HRQOL because this study was cross-sectional survey. Second, this study was conducted by using self-reported questionnaires to report some data such as EQ-5D and dental pain. Third, self-reported dental pain was particularly subjective experience, and the duration and severity of dental pain were not known.
5. Conclusions
In conclusion, subjects with tooth loss and dental pain appear to have a greater risk of deterioration in their HRQOL than those who simply have tooth loss or dental pain. Dental pain compared with tooth loss has a strong association with HRQOL.
Acknowledgements
The authors thank Catholic Medical Center Research Foundation made in the program year of 2016 for the support.
Footnotes
Abbreviations: BMI = body mass index, EQ-5D = The EuroQoL 5-dimension, EQ-VAS = EuroQoL visual analogue scale, HRQOL = health-related quality of life, KNHANES = Korea National Health and Nutrition Examination Survey, OR = odds ratio.
The authors have no conflicts of interest to disclose.
Funding/support: This study was supported by Catholic Medical Center Research Foundation made in the program year of 2016.
References
- 1.Pau AK, Croucher R, Marcenes W. Prevalence estimates and associated factors for dental pain: a review. Oral Health Prev Dent 2003; 1:209–220. [PubMed] [Google Scholar]
- 2.Peres MA, Peres KG, Frias AC, et al. Contextual and individual assessment of dental pain period prevalence in adolescents: a multilevel approach. BMC Oral Health 2010; 10:20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Slade GD, Foy SP, Shugars DA, et al. The impact of third molar symptoms, pain, and swelling on oral health-related quality of life. J Oral Maxillofac Surg 2004; 62:1118–1124. [DOI] [PubMed] [Google Scholar]
- 4.Goes PS, Watt RG, Hardy R, et al. Impacts of dental pain on daily activities of adolescents aged 14–15 years and their families. Acta Odontol Scand 2008; 66:7–12. [DOI] [PubMed] [Google Scholar]
- 5.Yang SE, Park YG, Han K, et al. Dental pain related to quality of life and mental health in South Korean adults. Psychol Health Med 2015; 1–12. [DOI] [PubMed] [Google Scholar]
- 6.Steele JG, Sanders AE, Slade GD, et al. How do age and tooth loss affect oral health impacts and quality of life? A study comparing two national samples. Community Dent Oral Epidemiol 2004; 32:107–114. [DOI] [PubMed] [Google Scholar]
- 7.Sanders AE, Slade GD, Lim S, et al. Impact of oral disease on quality of life in the US and Australian populations. Community Dent Oral Epidemiol 2009; 37:171–181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gilbert GH, Meng X, Duncan RP, et al. Incidence of tooth loss and prosthodontic dental care: effect on chewing difficulty onset, a component of oral health-related quality of life. J Am Geriatr Soc 2004; 52:880–885. [DOI] [PubMed] [Google Scholar]
- 9.Batista MJ, Lawrence HP, de Sousa Mda L. Impact of tooth loss related to number and position on oral health quality of life among adults. Health Qual Life Outcomes 2014; 12:165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gerritsen AE, Allen PF, Witter DJ, et al. Tooth loss and oral health-related quality of life: a systematic review and meta-analysis. Health Qual Life Outcomes 2010; 8:126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Brooks R. EuroQol: the current state of play. Health Policy 1996; 37:53–72. [DOI] [PubMed] [Google Scholar]
- 12.The EuroQol Group. EuroQol-a new facility for the measurement of health-related quality of life. Health Policy 1990; 16:199–208. [DOI] [PubMed] [Google Scholar]
- 13.Lötzke D, Heusser P, Büssing A. A systematic literature review on the effectiveness of eurythmy therapy. J Integr Med 2015; 13:217–230. [DOI] [PubMed] [Google Scholar]
- 14.Hurst NP, Kind P, Ruta D, et al. Measuring health-related quality of life in rheumatoid arthritis: validity, responsiveness and reliability of EuroQol (EQ-5D). Br J Rheumatol 1997; 36:551–559. [DOI] [PubMed] [Google Scholar]
- 15.Kim MH, Cho YS, Uhm WS, et al. Cross-cultural adaptation and validation of the Korean version of the EQ-5D in patients with rheumatic diseases. Qual Life Res 2005; 14:1401–1406. [DOI] [PubMed] [Google Scholar]
- 16.Lee YJ, Woo SY, Ahn JH, et al. Health-related quality of life in adults with metabolic syndrome: the Korea national health and nutrition examination survey, 2007–2008. Ann Nutr Metab 2012; 61:275–280. [DOI] [PubMed] [Google Scholar]
- 17.Kim KI, Lee JH, Kim CH. Impaired health-related quality of life in elderly women is associated with multimorbidity: results from the Korean National Health and Nutrition Examination Survey. Gend Med 2012; 9:309–318. [DOI] [PubMed] [Google Scholar]
- 18.Lee JA, Kim SY, Kim Y, et al. Comparison of health-related quality of life between cancer survivors treated in designated cancer centers and the general public in Korea. Jpn J Clin Oncol 2014; 44:141–152. [DOI] [PubMed] [Google Scholar]
- 19.Lee YK, Nam HS, Chuang LH, et al. South Korean time trade-off values for EQ-5D health states: modeling with observed values for 101 health states. Value Health 2009; 12:1187–1193. [DOI] [PubMed] [Google Scholar]
- 20.Ide R, Yamamoto R, Mizoue T. The Japanese version of the Oral Health Impact Profile (OHIP)–validation among young and middle-aged adults. Community Dent Health 2006; 23:158–163. [PubMed] [Google Scholar]
- 21.Ekanayake L, Perera I. The association between clinical oral health status and oral impacts experienced by older individuals in Sri Lanka. J Oral Rehabil 2004; 31:831–836. [DOI] [PubMed] [Google Scholar]
- 22.Shimazaki Y, Soh I, Saito T, et al. Influence of dentition status on physical disability, mental impairment, and mortality in institutionalized elderly people. J Dent Res 2001; 80:340–345. [DOI] [PubMed] [Google Scholar]
- 23.Sheiham A, Steele JG, Marcenes W, et al. The relationship among dental status, nutrient intake, and nutritional status in older people. J Dent Res 2001; 80:408–413. [DOI] [PubMed] [Google Scholar]
- 24.Aukes JN, Kayser AF, Felling AJ. The subjective experience of mastication in subjects with shortened dental arches. J Oral Rehabil 1988; 15:321–324. [DOI] [PubMed] [Google Scholar]
- 25.Witter DJ, Cramwinckel AB, van Rossum GM, et al. Shortened dental arches and masticatory ability. J Dent 1990; 18:185–189. [DOI] [PubMed] [Google Scholar]
- 26.Sommer I, Lavigne G, Ettlin DA. Review of self-reported instruments that measure sleep dysfunction in patients suffering from temporomandibular disorders and/or orofacial pain. Sleep Med 2015; 16:27–38. [DOI] [PubMed] [Google Scholar]


