Abstract
Sleep norms vary between individuals, being affected by personal, communal, and socioeconomic factors. Individuals with sleep time which deviate from the population norm are at risks of adverse mental, cardiovascular, and metabolic health. Sleep-related issues are common agenda for consultation in primary care. This study aimed to determine the sleep time, pattern, and behavior of multiethnic Asian individuals who attended public primary care clinics in an urban metropolitan city-state.
Standardized questionnaires were assistant-administered to adult Asian individuals who visited 2 local public primary care clinics in north-eastern and southern regions of Singapore. The questionnaire included questions on demographic characteristics, self-reported sleep time, patterns, and behavior and those originated from the American National Sleep Foundation Sleep Diary. The data were collated, audited, rectified, and anonymized before being analyzed by the biostatistician. Individuals with 7 h sleep time or longer were deemed getting adequate sleep. Chi-squared or Fisher exact test was used to test the association between the demographic and behavioral variables and sleep time. Next, regression analysis was performed to identify key factors associated with their sleep time.
A total of 350 individuals were recruited, with higher proportion of those of Chinese ethnicity reporting adequate sleep. Almost half (48.1%) of those who slept <7 h on weekdays tended to sleep ≥7 h on weekends. More individuals who reported no difficulty falling asleep, had regular sleep hours and awakening time, tended to sleep adequately. Those who slept with children, studied, read leisurely, used computer or laptops in their bedrooms, drank caffeinated beverages or smoked had inadequate sleep. Those who perceived sufficient sleep and considered 8 h as adequate sleep time had weekday and weekend sleep adequacy.
Sleep time varied according to ethnicity, employment status, personal behavior, and perception of sleep sufficiency. Awareness of sleep time and pattern allows the local physicians to contextualize the discussion of sleep adequacy with their patients during consultation, which is a prerequisite to resolve their sleep-related issues.
Keywords: behavior, sleep, sleep sufficiency, sleep time
1. Introduction
Sleep is a naturally recurring state of mind characterized by altered consciousness, relatively inhibited sensory activity, inhibition of nearly all voluntary muscles, and reduced interactions with surroundings.[1] Sleep aids our learning, memory, attention, and concentration.[2] Thus, it is vital to have sufficient sleep to sustain mental health.
In contrast, sleep insufficiency not only affects learning and concentration, it also leads to adverse health effects. Arbitrarily defined as sleep time of <7 h, sleep insufficiency has been reported to increase the risk of obesity, hypertension, diabetes, metabolic syndrome, and cardiovascular disease.[3–7] Prolonged periods of insufficient sleep can affect an individual's immune system, memory, concentration, and daily functioning.[2] The lack of sleep also increases the risk of physical distress such as chronic pain, and mental distress such as depression and anxiety in men who smoke, drink alcohol excessively and do not exercise regularly.[7] Studies have shown that between 35% and 37% of American adults had <7 h of sleep on average per night.[8,9] Jackson et al[10] revealed that 33% of Americans of Asian ethnicity slept <7 h daily. Aside from sleep time variability across ethnic groups within a population, these studies also highlighted a relatively high prevalence of sleep insufficiency.
Multiple factors are associated with sleep insufficiency. Individuals aged below 45 years old, female gender, and those employed were more likely to report sleep insufficiency.[8] Demographic characteristics such as minority status and lower socioeconomic position have been associated with shorter self-reported sleep time.[9,10] Shift workers who hold multiple jobs and work for very long hours also report insufficient sleep.[11,12] Lifestyle factors may also affect sleep time. Individuals may prefer to devote sleep time to watching television or engage in other modes of entertainment. A Taiwanese study by Yen et al revealed that drinking coffee at night and indiscrete Internet use were significantly associated with short nocturnal sleep time in adolescents.[13]
Sleep time recommendations have been put up by various institutions such as the American Academy of Sleep Medicine, the Sleep Research Society, and the National Sleep Foundation.[11–13] However, sleep time varies between individuals, ethnicities, and populations. What is recommended in the American society may not be applicable and relevant to the populations in Asia with their different sociocultural and environmental background, including those in the developed island-state of Singapore, whose population comprises of Chinese, Malays, and Indians.
Recognizing the typical sleep time of the multiethnic population is a prerequisite to assess their sleep adequacy and its consequences to health. Sleep inadequacy is a common reason of encounter in general practice. As sleep time is associated with a wide range of detrimental medical conditions, it is important to understand the sleep characteristic variance of the residents in metropolitan Singapore. This will allow the physicians to contextualize the discussion of sleep-related complaints with their patients in their clinical practice. This study aims to determine the mean daily sleep time among individuals in primary care, assess their perceptions of sleep sufficiency, and identify the factors which significantly affect their sleep.
2. Methods
2.1. Study sites
Sleep-related complaints are common symptoms in the community and are largely managed in primary care. SingHealth Polyclinics (SHP) is a public primary care institution in Singapore, which managed over 1.76 million patient attendances in 2015.[14] Its network of 9 polyclinics in the eastern and southern region of the metropolitan island-state, provides subsidized and affordable primary healthcare services to almost half of the local population. The investigators had selected the polyclinics at Seng Kang (SK) and Bukit Merah (BM) estates, respectively, for this nonfunded study. The deliberate choices of the study sites allowed the investigators to compare and contrast the sleep time and pattern of the population residing in the 2 districts with distinct estate designs. SK incorporates the estate residential design in the post-2000 era and has a predominantly younger population in north-east Singapore.[15] More senior residents aged 65 years and older live in BM, based on the 2015 National Population Census.[15] Located in the southern region of the island, BM is among the first batch of estates which were developed in the 1930s to 1950s.
2.2. Participants
The target individuals were adult patients and accompanying persons who visited the study sites from February to June 2015. Patients with acute conditions were specifically asked to relate their sleep-related information during the period when they were well. The individuals included multiethnic Asian citizens or permanent residents of both genders and aged between 21 and 80 years. After initial screening by the investigators during their interaction with potential subjects at the study sites, individuals with cognitive and hearing impairments, and those who did not communicate in the main local languages or refused consent were excluded.
2.3. Recruitment
The investigators screened potential subjects consecutively at the following service points at the study sites: waiting areas near registration kiosks and in-house pharmacy, and inside the consultation rooms. Eligible subjects provided verbal consent and were interviewed by investigators using a standardized questionnaire. The latter attended training by the principal investigator to standardize and ensure consistency during the questionnaire administration. The recruited subjects did not receive any form of compensation.
2.4. Instrument and questionnaire
The investigators devised the questionnaire as there was no existing sleep assessment for Asian population. The questionnaire collected data on subjects’ demographic characteristics and employment details such as shift work; personal views and perception of their sleep sufficiency; self-reported sleep time and behavior during weekdays and weekends. Questions pertaining to the latter were adapted from the National Sleep Foundation Sleep Diary.[13] These variables are segregated into weekdays and weekends for comparison. The questionnaire was filled on a hardcopy on-site and the data were subsequently transcribed into a spreadsheet. Audit checks were performed by the data management officer in the SHP Department of Research to identify any data entry error.
2.5. Sample size
As no a priori local data on sleep time in primary care were available, the 33% prevalence rate of American Asians who had short sleep duration of <7 h reported by Jackson et al[10] was used to estimate the sample size for this study. A study population size of 340 individuals was computed to be sufficient to determine a similar prevalence rate of individuals with short sleep duration, which would include a standard error of 5% with a 95% confidence interval. The target sample size was rounded up to 350, to allow a small buffer for isolated or unexpected withdrawal of consent by subjects.
2.6. Statistical analysis
Sleep time was transformed into dichotomous variables with the cut-off defined by the literature and recommended guidelines, respectively. Individuals who obtained 7 h of sleep or more a night were defined as having adequate sleep time, regardless of weekdays and weekends. Those who had <7 h sleep time were defined as having inadequate sleep.
Together with other data in the questionnaire, descriptive statistics were computed as categorical and continuous variables. Missing data were excluded from the analysis. Chi-squared or Fisher exact test was used to test the association between the demographics and sleep time. All factors that were significant at 0.05 were entered into the logistic regression model. Logistic regression analyses were done to determine the predictive factors for sleep duration of <7 h with the level of significance set at 0.05. Data were analyzed using SPSS version 22.0.
2.7. Ethics approval
The study protocol was approved by the SingHealth Centralized Institution Review Board (CIRB: 2014/223/E).
3. Results
There were 211 and 177 eligible individuals being approached at SK and BM, of which 11 and 27 declined participation, respectively, leading to a response rate of 94.8% and 84.7% at the 2 sites. Eventually, a total of 350 individuals were recruited, comprising of 200 from SK and 150 from BM. Their demographic characteristics and sleep profiles are presented in Table 1.
Table 1.
Individuals’ demographic profiles and their sleep time on weekends and weekdays.
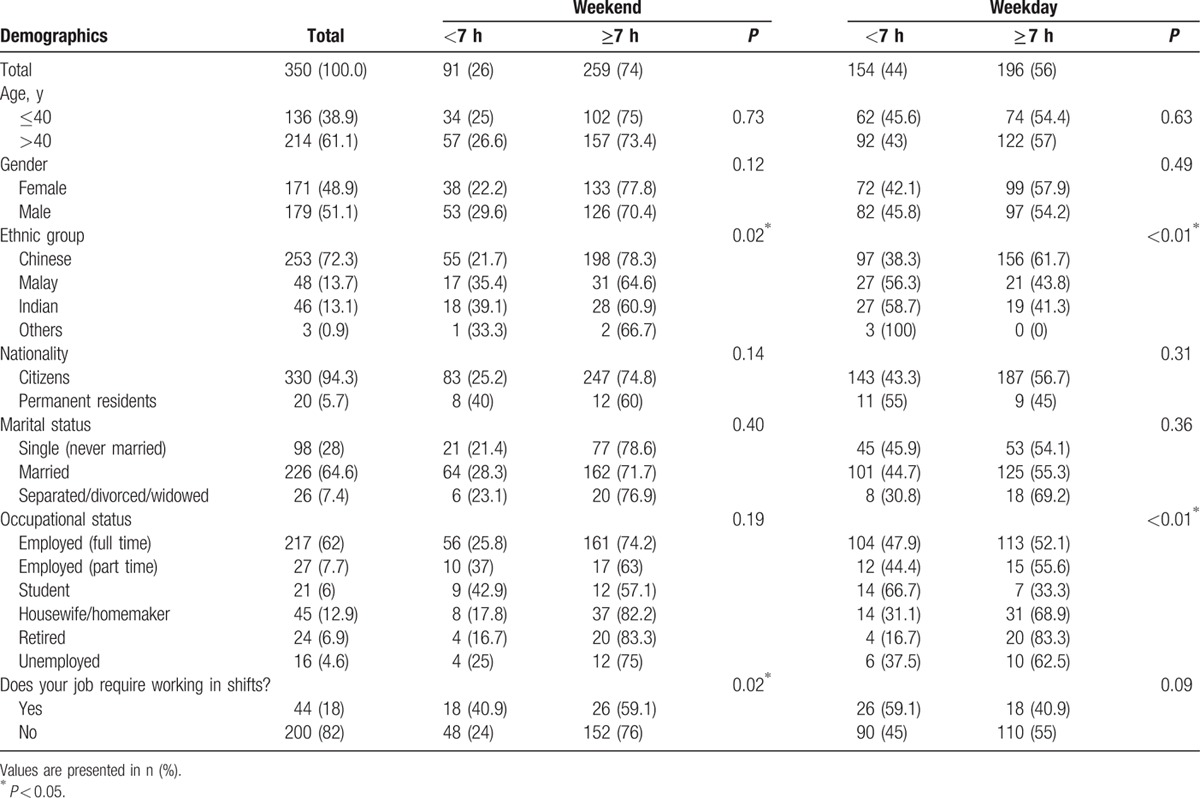
3.1. Sleep time
Among 350 individuals, 44% of them have inadequate sleep on weekdays and 26% of them have inadequate sleep on weekends. More individuals of Chinese ethnicity obtained ≥7 h of sleep than those of Malay and Indian ethnicities during weekdays (P < 0.01) and weekends (P = 0.02). Proportionately more full-time employees and students slept <7 h on weekdays (P = 0.01), compared with those who were housewives or homemakers, retired, and the unemployed. More shift workers failed to get more than 7 h of sleep on weekends (P = 0.02).
Majority of those with adequate sleep on weekdays would have sufficient sleep on weekends; 94.4% of those who slept ≥7 h on weekdays also slept ≥7 h on weekends. The day of the week did not matter to slightly half of those with inadequate sleep: 51.9% of those who slept <7 h on weekdays also had <7 h of sleep on weekends. On the other hand, 48.1% of those who slept <7 h on weekdays tended to sleep ≥7 h on weekends.
3.2. Sleep pattern and home environment
Table 2 shows the sleep pattern and environment of the study population. More individuals who fell asleep with difficulty tended to get <7 h of sleep on weekends (P = 0.02) and weekdays (P = 0.02). More individuals with regular sleep time would sleep more than 7 h on weekends (P < 0.01) and weekdays (P < 0.01). A higher proportion of individuals with regular awakening time obtained 7 or more hours of sleep on weekends (P = 0.01) and weekdays (P = 0.03).
Table 2.
Sleep patterns/habits of subjects in relation to their sleep time on weekends and weekdays.
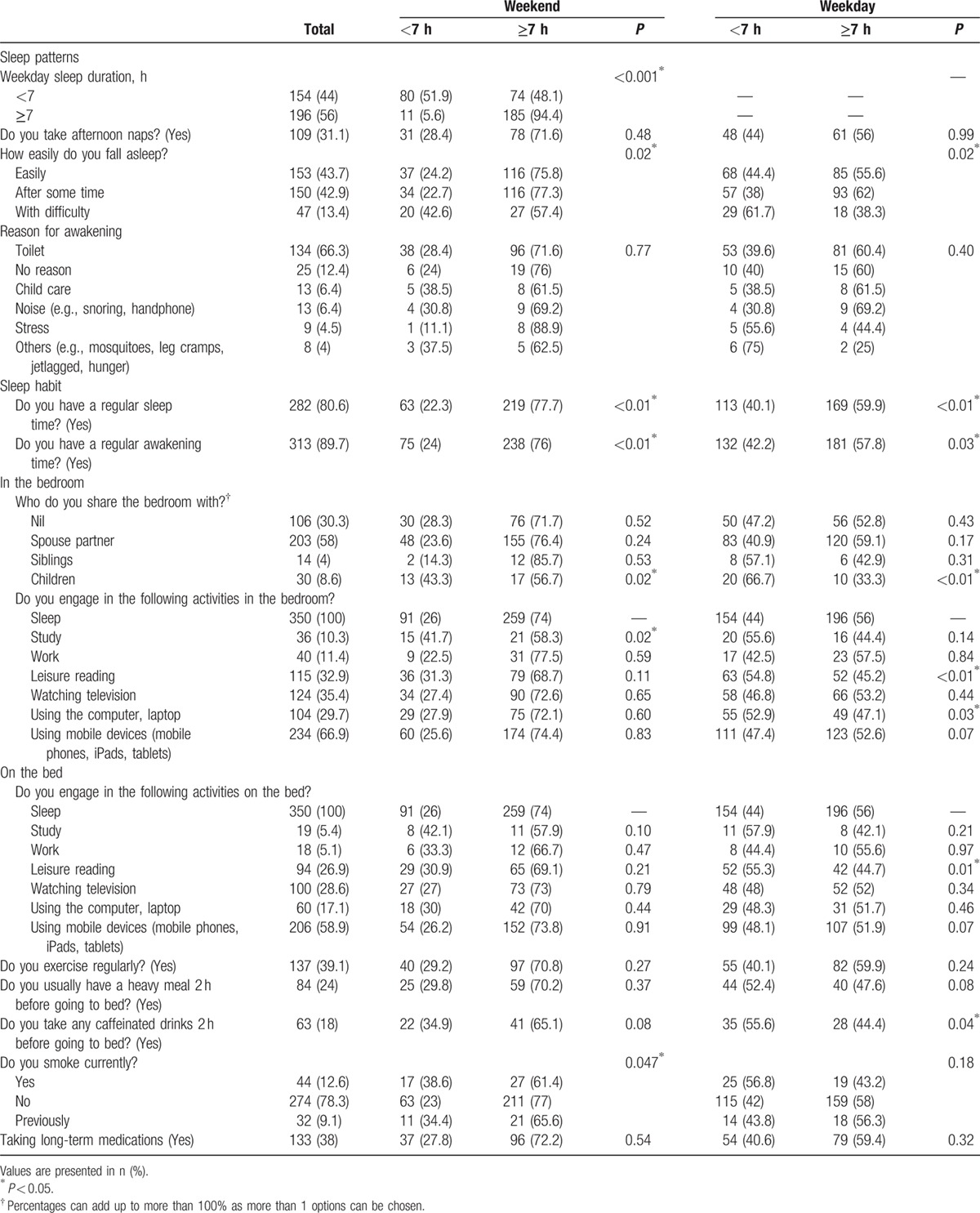
The majority of adults who shared the bedroom with children tended to sleep <7 h daily on weekends (P = 0.02) and weekdays (P = 0.01). Among individuals who studied in the bedroom, more of them slept <7 h on weekends (P = 0.02) but not on weekdays. Those who reported to read leisurely in their bedroom tended to get <7 h of sleep on weekdays (P < 0.01). Higher proportion of those who read leisurely on their bed also slept <7 h on weekdays (P = 0.01). Individuals who used computer or laptop in their bedroom tended to sleep <7 h on weekdays (P = 0.03).
3.3. Behavior and activities before sleep
Presleep habits and activities also affected sleep. More individuals who reported taking caffeinated drinks 2 h before going to bed, slept <7 h on weekdays (P = 0.04). Overall, nonsmokers were more likely to get ≥7 h of sleep than current or ex-smokers (P = 0.047) on weekends. History of exercise did not affect sleep time in this study.
3.4. Personal perception of sleep sufficiency
Table 3 shows the personal views of sleep sufficiency among the study population. More individuals who reported waking up in the morning feeling refreshed tended to have ≥7 h of sleep on weekends (P = 0.01) and weekdays (P < 0.001). In contrast, those who woke up in the morning feeling fatigued were more likely to have <7 h of sleep on weekends (P = 0.01) and weekdays (P < 0.001).
Table 3.
Self-perception of sleep time on weekends and weekdays.
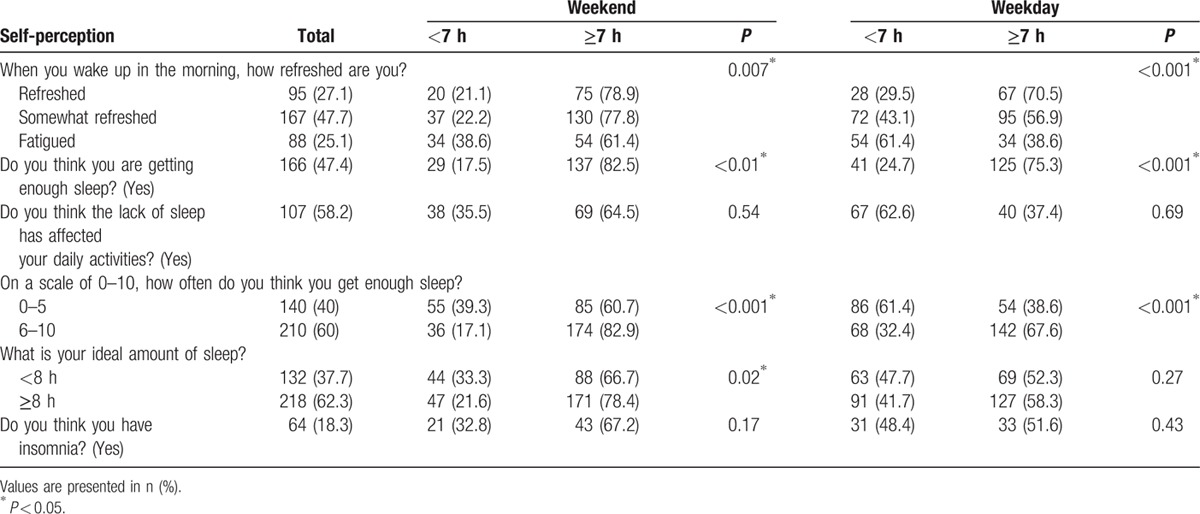
More individuals who perceived to have enough sleep tended to sleep ≥7 h on weekends (P = 0.001) and weekdays (P < 0.001). Those who felt that they did not get enough sleep more than half the time tended to have <7 h of sleep any day of the week (both P < 0.001). Individuals who perceived to have sufficient sleep more than half the time were more likely to get ≥7 h of sleep on any day of the week (both P < 0.001). Those individuals whose perceived ideal amount of sleep would be 8 or more hours daily were more likely to sleep ≥7 h on weekends (P = 0.02).
3.5. Summary of key findings after logistic regression analysis
Table 4 shows the circumstances which affect sleep time on weekends and weekdays in a logistic regression model. After adjusting the effect of other covariates, individuals who read in bedroom (OR = 2.1, 95% CI: 1.2–3.8, P = 0.01) or those who drink caffeinated drinks 2 h before their sleep (OR = 2.2, 95% CI: 1.1–4.4, P = 0.03) were twice more likely to have insufficient sleep during weekdays. In contrast, those who regarded that they were getting adequate sleep and whose perceived ideal sleep time was 8 h or more, were more likely to have ≥7 h of sleep.
Table 4.
Stepwise backward logistic regression for weekday and weekend sleep time.
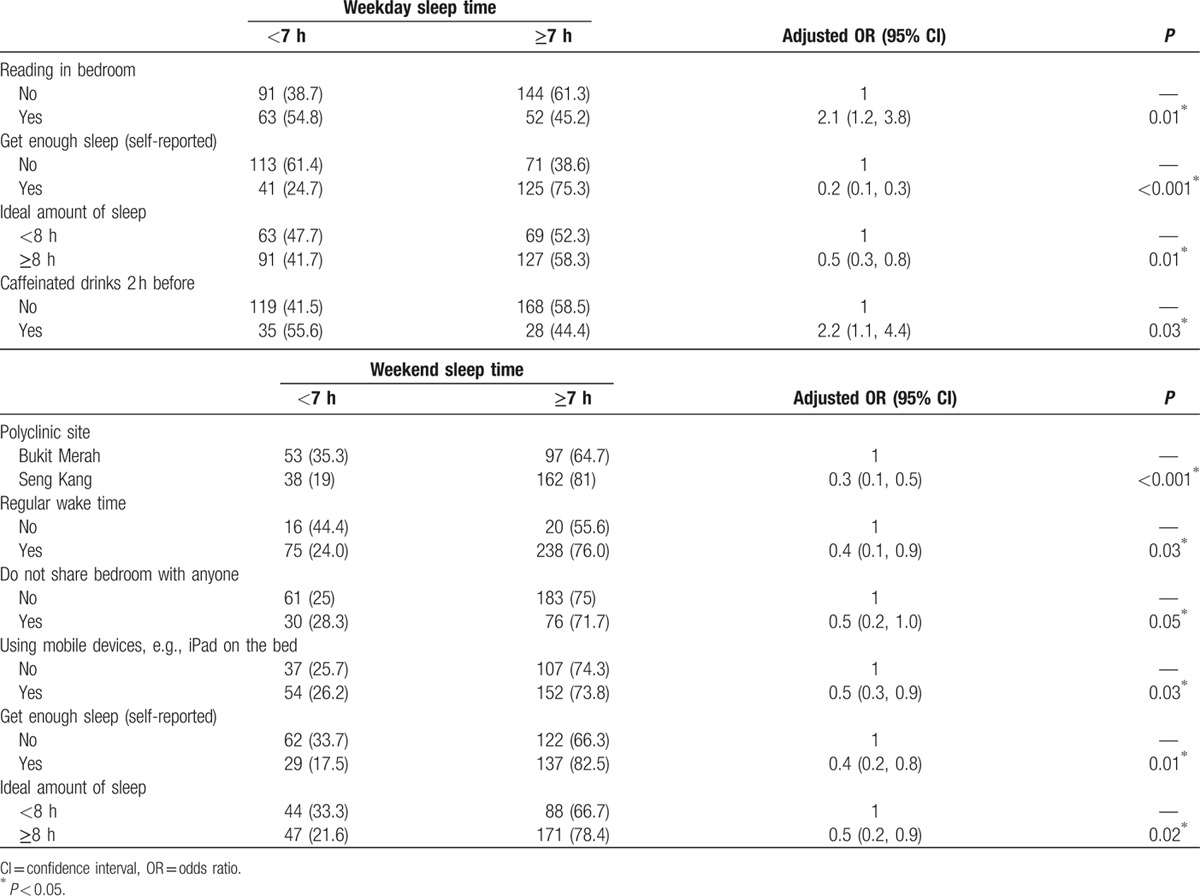
For weekends, individuals with regular awakening time (OR = 0.4, 95% CI: 0.1–0.9, P = 0.03), perceived having enough sleep (OR = 0.4, 95% CI = 0.2–0.8, P = 0.01), and those who felt that ≥8 h is ideal sleep time (OR = 0.5, 95% CI = 0.2–0.9, P = 0.02) were less likely to have insufficient sleep. What seemed surprising was that those who used mobile devices in bed were more likely to have adequate sleep time (OR = 0.5, 95% CI: 0.3–0.9, P = 0.03).
4. Discussion
The results provide a timely update on the impact on the sleep pattern and behavior of a study population living within a multiethnic Asian community of high mobile phone penetration rate and widespread web-based connectivity.[16] In summary, sleep time during weekdays was associated with reading activities, caffeinated beverages, and perception of sleep sufficiency. Over weekends, adequate sleep time was associated with regular awakening hours, perception of sleep sufficiency, and even use of mobile devices in bed. These associated factors are largely modifiable. With appropriate recommendations by the healthcare professionals, these factors can potentially be adjusted such that the sleep hygiene of the individuals is not compromised.
Ethnicity seems to have an influence on the sleep time. More individuals of Chinese ethnicity seemed to have adequate sleep compared with the other minority ethnic groups during both weekdays and weekends. Aside from ethnical differences in lifestyles, this could also stem from socioeconomic differences among the different ethnic groups in Singapore. Household income is notably higher in Chinese households as compared to Malay and Indian households.[17]
Previous studies have reported a negative sleep correlation with those from a lower educational level or income group. The Shanghai Women's Health Study found that manual laborers and clerical staff were in general, getting less sleep than those from the professional occupation.[18] Lallukka et al revealed that low education levels, low income, and being unemployed were associated with increased insomnia symptoms in Finland.[19]
The employment status, be it full-time or part-time employment, was found to have an influence on sleep time. In this study, individuals who were committed to work or school as full-time employees or students had higher likelihood of having inadequate sleep on weekdays, but it appeared that they would try to catch up with the sleep deprivation over the weekend. Workers and students would likely need additional time to maintain work life balance during weekdays. In contrast, those without any fixed work commitment such as homemakers, retirees, and unemployed more often had adequate sleep consistently over each day of the week.
The prevalent use of infocommunication via Internet and mobile phone in the home environment is another factor affecting sleep time. In this study, users of laptop computers, surfing the Internet or computer gaming in the bedroom tended to have sleep time of <7 h over weekdays. Interestingly, the use of these devices in bed did not shorten their sleep duration. We postulate that these handy devices can be used anywhere in the bedroom, not necessarily in bed. Most people carry their phones all day long and are able to use them any time anywhere. The setting in which individuals use their mobile devices and its impact on the various aspects of their personal lives, especially in the advent of rapid development of immersive multimedia or virtual reality, await further examination in future research.
Smoking has consistently been shown to affect sleep as nicotine is a well-known stimulant. This study showed that smokers or previous smokers tended to have lesser sleep compared with nonsmokers. Smoking alone significantly increases risks of vascular diseases. Such risks would be further heightened by the lack of sleep as insufficient sleep is also associated with the cardio-metabolic syndrome.[20] Consultation relating to sleep-related complaints is an opportunity for the physician to persuade the patients to quit smoking as a measure to ameliorate sleep insufficiency.
4.1. Strength and weakness
Objective and accurate measurement of sleep time for any population is challenging. Conducting large-scale, population-based sleep studies using epidemiological approaches and neurophysiological testing would be ideal but is resource intensive and challenging to execute. The lack of a common electronic healthcare database for the public and private primary healthcare system in Singapore compounds any implementation of community-based study as local residents can seek medical attention in 1 or more registered healthcare providers of their preference. The response rates of the consecutive sampling of subjects at the study sites were satisfactory, suggesting a relatively efficient direct-encounter recruitment strategy despite the absence of incentives and other constraints.
In addition, the investigators had to assemble a questionnaire de novo with segments adapted from an American instrument due the paucity of validated sleep assessment instruments for Asian population. While important findings are presented here will be invaluable to develop a better-designed community-based study, we will caution in any attempt to extrapolate the results from these 2 study sites to the whole of our local population.
Acknowledgments
The authors would most appreciative of the altruistic nature of the study participants who contributed their time and effort to complete the questionnaire. The authors thank to nurse clinician Frida Wong, nurse manager Beatty-Low, and the nurses of SHP-SK and BM for facilitating the study implementation at the sites. The authors are also grateful to the staff of the Department of Research at SingHealth Polyclinics, in particular Ms Usha, the data management officer, and Ms Caris Tan for the project management and administrative matters pertaining to ethical approval of the study.
Footnotes
Abbreviations: BM = Bukit Merah, SHP = SingHealth Polyclinics, SK = Seng Kang.
MST initiated the study. She designed the questionnaire with assistance from HCH. MST recruited individuals in SK while JYJS, ZKNL, and CCT surveyed those in BM with assistance and support from SWH. Data were analyzed by NCT and YLEK. NCT, SWH, MST, YLEK, JYJS, ZKNL, and CCT discussed the results and drafted the preliminary manuscript. MST, NCT, YLEK, SWH, and HCH revised and finalized the manuscript for submission.
Ethics approval was granted from the Centralized Institutional Review.
The authors report no specific funding in relation to this research and no conflict of interest to disclose.
References
- 1.Oxford University Press. Oxford Dictionaries. In: British and World English; 2015. http://www.oxforddictionaries.com/definition/english/sleep Accessed January 6, 2016. [Google Scholar]
- 2.Colten HR, Altevogt BM, Institute of Medicine (US) Committee on Sleep Medicine and Research, eds. Sleep Disorders and Sleep Deprivation: An Unmet Public Health Problem. Washington, DC: National Academies Press (US); 2006. http://www.ncbi.nlm.nih.gov/books/NBK19960/ Accessed January 6, 2016. [PubMed] [Google Scholar]
- 3.Buxton OM, Marcelli E. Short and long sleep are positively associated with obesity, diabetes, hypertension, and cardiovascular disease among adults in the United States. Soc Sci Med 2010; 71:1027–1036. [DOI] [PubMed] [Google Scholar]
- 4.Faraut B, Touchette E, Gamble H, et al. Short sleep duration and increased risk of hypertension: a primary care medicine investigation. J Hypertens 2012; 30:1354–1363. [DOI] [PubMed] [Google Scholar]
- 5.Lee J, Choi YS, Jeong YJ, et al. Poor-quality sleep is associated with metabolic syndrome in Korean adults. Tohoku J Exp Med 2013; 231:281–291. [DOI] [PubMed] [Google Scholar]
- 6.Bjorvatn B, Sagen IM, Øyane N, et al. The association between sleep duration, body mass index and metabolic measures in the Hordaland Health Study. J Sleep Res 2007; 16:66–76. [DOI] [PubMed] [Google Scholar]
- 7.Strine TW, Chapman DP. Associations of frequent sleep insufficiency with health-related quality of life and health behaviors. Sleep Med 2005; 6:23–27. [DOI] [PubMed] [Google Scholar]
- 8.Centers for Disease Control and Prevention. Unhealthy Sleep-Related Behaviors, Morbidity and Mortality Weekly Report; 2011. http://www.cdc.gov/mmwr/preview/mmwrhtml/mm6008a2.htm Accessed January 6, 2016. [Google Scholar]
- 9.Centers for Disease Control and Prevention. Effect of Short Sleep Duration on Daily Activities, Morbidity and Mortality Weekly Report. Effect of Short Sleep Duration on Daily Activities, Morbidity and Mortality Weekly Report; 2011. http://www.cdc.gov/mmwr/preview/mmwrhtml/mm6008a3.htm Accessed January 6, 2016. [PubMed] [Google Scholar]
- 10.Jackson CL, Kawachi I, Redline S, et al. Asian-White disparities in short sleep duration by industry of employment and occupation in the US: a cross-sectional study. BMC Public Health 2014; 14:552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Blair PS, Humphreys JS, Gringras P, et al. Childhood sleep duration and associated demographic characteristics in an English Cohort. Sleep 2012; 35:353–360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Watson NF, Badr MS, et al. Consensus Conference Panel. Recommended amount of sleep for a healthy adult: a joint consensus statement of the American Academy of Sleep Medicine and Sleep Research Society. J Clin Sleep Med 2015; 11:591–592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sleep Foundation. How Much Sleep Do We Really Need?; 2015. http://sleepfoundation.org/how-sleep-works/how-much-sleep-do-we-really-need Accessed August 4, 2015. [Google Scholar]
- 14.Top 4 Conditions of Polyclinic Attendances|Ministry of Health. https://www.moh.gov.sg/content/moh_web/home/statistics/Health_Facts_Singapore/Top_4_Conditions_of_Polyclinic_Attendances.html Accessed May 25, 2015. [Google Scholar]
- 15.Population Trends 2015. Department of Statistics, Ministry of Trade & Industry, Republic of Singapore. https://www.singstat.gov.sg/docs/default-source/default-document-library/publications/publications_and_papers/population_and_population_structure/population2015.pdf Accessed October 10, 2015. [Google Scholar]
- 16.Infocomm Development Authority of Singapore. Mobile Penetration Rate. Data.gov.sg. https://data.gov.sg/dataset/mobile-penetration-rate/resource/26e9766b-a42d-468c-9c25-88d89b850823/view/3fed45d7-7f86-4422-872a-e6d0a0154b06 Accessed June 3, 2016. [Google Scholar]
- 17.Department of Statistics, Singapore. Monthly Household Income from Work. Department of Statistics Singapore. Census of Population 2010 Statistical Release 2: Households and Housing; 2015. http://www.singstat.gov.sg/publications/publications-and-papers/cop2010/census10_stat_release2 Accessed January 12, 2016. [Google Scholar]
- 18.Tu X, Cai H, Gao Y-T, et al. Sleep duration and its correlates in middle-aged and elderly Chinese women: the Shanghai Women's Health Study. Sleep Med 2012; 13:1138–1145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lallukka T, Sares-Jäske L, Kronholm E, et al. Sociodemographic and socioeconomic differences in sleep duration and insomnia-related symptoms in Finnish adults. BMC Public Health 2012; 12:565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hung H-C, Yang Y-C, Ou H-Y, et al. The association between self-reported sleep quality and metabolic syndrome. PLoS ONE 2013; 8:e54304. [DOI] [PMC free article] [PubMed] [Google Scholar]


