Abstract
Context
Measurement of dyspnea is important for clinical care and research.
Objectives
To characterize the relationship between the 0–10 Numerical Rating Scale (NRS) and four-level categorical Verbal Descriptor Scale (VDS) for dyspnea assessment.
Methods
This was a substudy of a double-blind randomized controlled trial comparing palliative oxygen to room air for relief of refractory breathlessness in patients with life-limiting illness. Dyspnea was assessed with both a 0–10 NRS and a four-level categorical VDS over the one-week trial. NRS and VDS responses were analyzed in cross section and longitudinally. Relationships between NRS and VDS responses were portrayed using descriptive statistics and visual representations.
Results
Two hundred twenty-six participants contributed responses. At baseline, mild and moderate levels of breathlessness were reported by 41.9% and 44.6% of participants, respectively. NRS scores demonstrated increasing mean and median levels for increasing VDS intensity, from a mean (SD) of 0.6 (±1.04) for VDS none category to 8.2 (1.4) for VDS severe category. The Spearman correlation coefficient was strong at 0.78 (P < 0.0001). Based on the distribution of NRS scores within VDS categories, we calculated test characteristics of two different cutpoint models. Both models yielded 75% correct translations from NRS to VDS; however, Model A was more sensitive for moderate or greater dyspnea, with fewer misses downcoded.
Conclusion
There is strong correlation between VDS and NRS measures for dyspnea. Proposed practical cutpoints for the relationship between the dyspnea VDS and NRS are 0 for none, 1–4 for mild, 5–8 for moderate, and 9–10 for severe.
Keywords: Dyspnea, Numerical Rating Scale, Verbal Descriptor Scale
Introduction
Dyspnea has been defined as “a subjective experience of breathing discomfort that consists of qualitatively distinct sensations varying in intensity. The experience derives from interactions among multiple physiological, psychological, social, and environmental factors.”1 A common experience among people with life-limiting illness, dyspnea prevalence has been reported to be as high as 65%, 70%, and 90% in advanced-stage patients with heart failure, lung cancer, and chronic obstructive pulmonary disease, respectively.2 Dyspnea is often intractable in advanced disease, frequently escalating in intensity as death approaches,3–6 eroding quality of life, psychological well-being, and social functioning.7
Dyspnea assessment has been an active area of research for many decades. The complex etiology of dyspnea, both pathophysiological and psychosocial, has proven challenging in developing tools that capture its multiple dimensions. Several recent reviews have examined existing validated measurement tools, highlighting the lack of consensus regarding how to best capture the complicated experience of dyspnea in both clinical and research settings.8,9 The spectrum of measures includes single-item ordinal scales, functional assessment scales, global symptom inventories with dyspnea components, and multidimensional dyspnea scales.
The choice of scale depends on purpose, setting, and population. When precision and responsiveness to change are needed, complex multi-item scales may be preferable.10 However, there are a range of scenarios where single-item dyspnea assessment scales are more appropriate, such as when part of routine clinical care, embedded in a larger group of patient-reported outcomes, or completed repeatedly at short intervals. Among single-item patient-reported scales, the Visual Analogue Scale,11 Numerical Rating Scale (NRS, e.g., 0 = no breathlessness to 10 = worst breathlessness possible),12,13 and the modified Borg scale14,15 have all been validated, but none have been preferentially adopted.
The proliferation of assessment tools without standardized adoption of any single tool highlights the need for a simple breathlessness scale that can be reliably and practically used in the clinic, efficiently translating evidence between clinical care and clinical trials. Such a tool should be easily understood across diseases and settings, including advanced life-limiting illness, and by patients and their families. To achieve this, it must focus on the subjective sensation of dyspnea and parallel other scales commonly used (e.g., pain assessment).
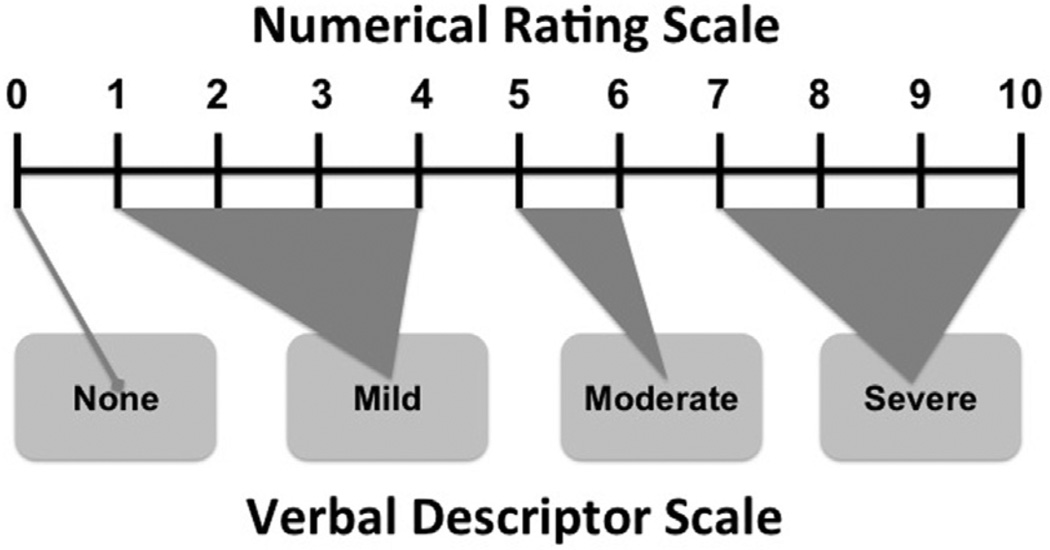
Wilcock et al.13 advocated that the NRS is more practical than the Visual Analogue Scale for repeated measures in cancer patients. However, ordered categorical scales (e.g., none, mild, moderate, or severe) may be even more practical, would more clearly communicate what is meant clinically, and are less abstract for patients, especially if there is any cognitive impairment. For example, an ordered categorical scale is frequently used for pain assessment, and its relationship to the 0–10 NRS is well characterized (Fig. 1), although minor differences in cutpoints exist, depending on population and methods.16–18 The cutpoint between mild/moderate is often used as a lower threshold limit for eligibility in symptom controlled trials.19,20
Fig. 1.
Practical relationship between Numerical Rating Scale and Verbal Descriptor Scale for pain (based on results from Refs.15,16).
The aim of this article, therefore, was to determine the relationship between an ordered categorical Verbal Descriptor Scale (VDS) of dyspnea and the dyspnea NRS, in a similar way that these two scales are related for pain assessment.
Methods
This was an a priori planned substudy intentionally embedded within an international, multicenter, double-blind, randomized controlled trial assessing the effect of palliative oxygen vs. room air in relief of refractory dyspnea.21 The parent study protocol was approved by the Duke University Health System Institutional Review Board, all nine local research and ethics committees or institutional review boards of all participating sites, and was registered with ClinicalTrials.gov (NCT00327873) and International Standard Randomised Controlled Trial Number (ISRCTN) (ISRCTN67448752).
Participants
In the parent study, patients (N = 239) were recruited from pulmonary, palliative care, oncology, and primary care services at five sites in Australia, two in the U.S., and two in the U.K. Participants were consenting adults with refractory dyspnea, partial pressure of oxygen in arterial blood (PaO2) >55 mmHg, and life-limiting illness where the underlying cause had been maximally treated. Participants had dyspnea at rest or with minimal exertion, corresponding to a Medical Research Council categorical dyspnea score of ≥3;22 however, patient data were pooled for this project, and there was no analysis according to the intervention used for the parent study. Additional eligibility criteria were that the participants must have been on stable medications for the seven days before randomization; hemoglobin >10 gm/dL; prognosis for survival of at least one month; and ability to complete the symptom diary, including ability to sufficiently understand English. Participants were randomized to medical air or oxygen, delivered at 2 L per minute via nasal cannula, for at least 15 hours daily for seven days.
Outcomes
The primary outcome was breathlessness right now, recorded by the participant twice a day (within 30 minutes of waking up [morning] and going to bed [evening]) in a diary with a 0–10 NRS, anchored at 0 = not breathless at all and 10 = breathlessness as bad as you can imagine, which is a valid instrument for this population of patients.23 In addition to the dyspnea NRS scale, participant diaries also included a four-point VDS for dyspnea severity (none, mild, moderate, or severe).
Thus, participants answered the following questions daily on both the NRS and VDS scales:
Morning assessment: How is your breathlessness right now?
Evening assessment: How is your breathlessness right now?
Evening assessment: How has your breathlessness been over the last 24 hours, on average?
Evening assessment: What is the worst your breathlessness has been over the last 24 hours?
The participants were not instructed to respond to the questions in a specific order or to rate each scale independently; the daily diary provided to participants was ordered as shown previously. Participants were not asked to distinguish between the somatosensory intensity, affective distress, or other contributors to the perception of dyspnea in rating this item. Related symptoms, such as anxiety, functional limitations, and quality of life, were assessed with subsequent items in the diary.
For convenience, the preceding questions will henceforth be referred to as follows: Question 1: “AM now,” Question 2: “PM now,” Question 3: “24 hours average,” and Question 4: “24 hours worst.” The intervention comparing palliative oxygen and medical air lasted seven days, but patients began maintaining symptom diaries two days before the start of the intervention, thus documenting symptoms twice daily for nine days total.
Statistical Analysis
The relationship between the NRS and VDS responses for each of the four questions described previously was examined two ways: crosssectionally, using a single baseline time point (morning assessment on the day before the study intervention started, labeled Day −1) and longitudinally, across all time points. For the cross-sectional analysis, only participants who responded to both NRS and VDS forms of the question were included. For the longitudinal analysis, we created a single cross-tabulation of NRS and VDS scores regardless of question or time point (i.e., thus implicitly ignoring for the present purposes the multiple observations per patient). Descriptive statistics were used to evaluate and portray relationships. In both the cross-sectional and longitudinal analyses, missing data were not imputed. Although responses for both VDS and NRS were collected longitudinally throughout the study period, the purpose of this substudy was not to compare the responsiveness to change these rating scales.
Cutpoints were determined first by analyzing the distribution of NRS responses within each VDS category, looking for clear breaks in the data distribution. For example, if 80% of participants with a breathlessness NRS of 1 reported a VDS category of mild, NRS Level 1 would be associated with the mild category for conversion purposes. In cases where no clear break could be identified, we made cutpoint determinations with the goal of minimizing instances where breathlessness is downgraded in translating the NRS to the VDS. An example of downgrading might be an instance where a patient’s recorded NRS score of 4 might be translated as mild in the VDS according to the derived cutpoints, but the patient had reported moderate dyspnea corresponding to this instance.
Results
Of the 239 participants, 61.5% were males and 63.5% had a diagnosis of chronic obstructive pulmonary disease (Table 1). Thirteen patients withdrew before the study started and completed no assessments and, therefore, were excluded from analysis. An additional 15 participants withdrew before completing the final assessment. Across the entire study period, 3.3% of morning NRS assessments and 3.6% of morning VDS assessments were missing—predominantly because of dropout.
Table 1.
Baseline Demographics and Breathlessness Ratings Before Intervention (Day −1)
| N = 239 | Mean (SD) or % |
|---|---|
| Age, yrs | 73 (10) |
| Male | 62% |
| Chronic obstructive pulmonary disease | 64% |
| Cancer | 16% |
| Baseline PaO2, mm Hg | 76 (12) |
| Baseline dyspnea intensity | |
| NRS (N = 225) | 4.5 (2.3) |
| None (VDS) | 6.8% |
| Mild (VDS) | 41.9% |
| Moderate (VDS) | 44.6% |
| Severe (VDS) | 6.7% |
NRS = Numerical Rating Scale; VDS = Verbal Descriptor Scale.
Cross-Sectional Analysis
The NRS and VDS were compared before any intervention (baseline, Day −1). Current breathlessness at the time of the morning assessment (AM now) was recorded for 222 participants, with 41.9% reporting mild and 44.6% reporting moderate levels of breathlessness, and mean (SD) NRS of 4.5 (2.3) (Table 1). NRS values clustered within each VDS category. There was a direct relationship between mean (and median) NRS value with VDS category, with mean (SD) NRS scores of 0.3 (0.5) for VDS none category to 8.2 (1.1) for VDS severe category (Table 2). The NRS ranges that capture increasing percentages of patients in each VDS category were consistent (Table 2). The association between the NRS and VDS, reflected by Spearman’s correlation coefficient of 0.77 (P < 0.0001), was strong. Associations of similar strength, via Spearman’s correlation coefficient, were found for the other three questions on Day −1: Evening right now = 0.74; 24 hours average = 0.79; and 24 hours worst = 0.76.
Table 2.
Cross-Sectional Analyses Compared with Longitudinal Analyses of VDS and NRS Dyspnea Scores, Reflecting Current Morning Breathlessness at Baseline (Day −1) as Compared with All Entries on All Days
| Cross-Sectional Analysis |
Longitudinal Analysis |
|||
|---|---|---|---|---|
| Corresponding NRS | ||||
| VDS Categories | N | Mean (SD) | N | Mean (SD) |
| None | 15 | 0.33 (0.49) | 455 | 0.62 (1.0) |
| Mild | 93 | 3.4 (1.5) | 1898 | 3.4 (1.5) |
| Moderate | 99 | 5.8 (1.4) | 1386 | 5.9 (1.4) |
| Severe | 15 | 8.2 (1.1) | 143 | 8.2 (1.5) |
| Total | 222 | 3882 | ||
VDS = Verbal Descriptor Scale; NRS = Numerical Rating Scale.
Longitudinal Analyses
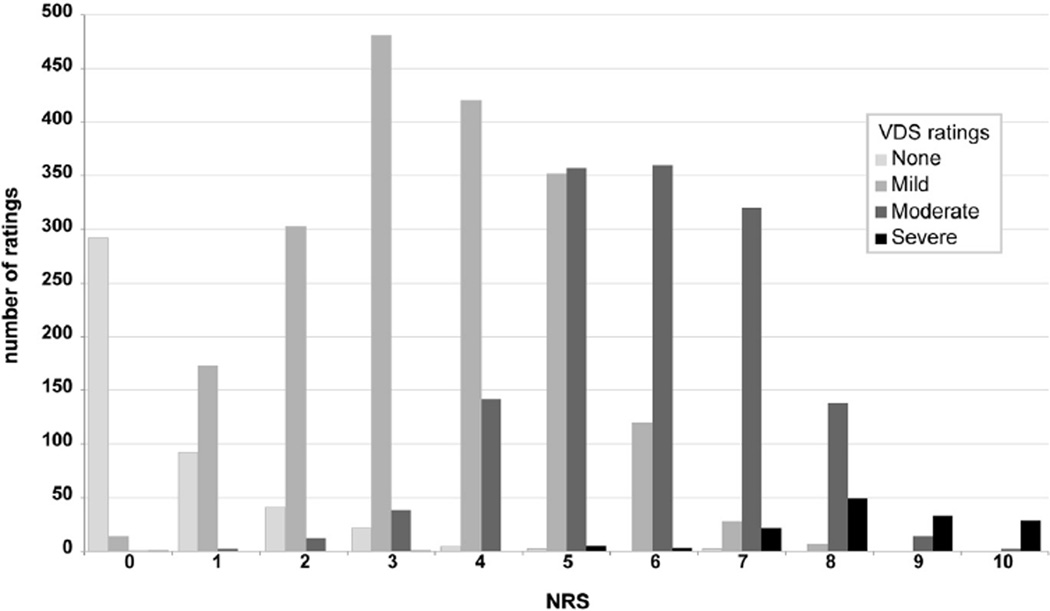
Combining responses to all four questions across all nine days of the study yielded 3882 paired observations for NRS and VDS. The results of analyses were substantively similar to those from the cross-sectional analysis of the AM now assessment on Day −1. The distribution of NRS scores within VDS categories is similar to that observed for the AM now assessment on Day −1 (Fig. 2). Specifically, the mean (SD) NRS scores were 0.61 (1.0) for VDS none, 3.4 (1.5) for VDS mild, 5.8 (1.4) for VDS moderate, and 8.2 (1.5) for VDS severe. The Spearman correlation coefficient for the VDS and NRS ratings was 0.78.
Fig. 2.
Distribution of Verbal Descriptor Scale (VDS) categories at each Numerical Rating Scale (NRS) score, reflecting current breathlessness across all study days.
Cutpoint Analyses
Using the longitudinal data, analysis of the distribution of VDS category by NRS reveals that 94% of NRS responses of 0 correspond to VDS reports of none (Fig. 2). At NRS of 1, only 34% of responses corresponded with none; all but two of the remaining responses corresponded with mild. Similarly, the transition from moderate to severe was relatively clear, with 71% of patients with NRS of 8 reporting moderate breathlessness. At NRS of 9, 70% reported severe breathlessness. The transition from mild to moderate is less clear, with 49% of patients with NRS of 5 reporting mild dyspnea and 49% reporting moderate dyspnea.
Based on the distribution of NRS scores within VDS categories, we examined the performance characteristics of two different cutpoint models. For Model A, NRS 0 corresponded to VDS none, NRS 1–4 corresponded to VDS mild, NRS 5–8 corresponded to VDS moderate, and NRS 9–10 corresponded to VDS severe. In Model B, NRS 0 corresponded to VDS none, NRS 1–5 corresponded to VDS mild, NRS 6–8 corresponded to VDS moderate, and NRS 9–10 corresponded to VDS severe (Table 2). Both models had a roughly 75% rate of correct translations from NRS to VDS; however, Model A had fewer misses downcoded (e.g., where the NRS attributed a lower VDS than the patient had reported at the corresponding time). Model A yields an 87% sensitivity and 78% specificity for moderate or severe dyspnea, whereas Model B yields only a 63% sensitivity but is more specific at 93% (Table 3).
Table 3.
Metrics Associated with Two Models for Cutpoints Between Mild and Moderate Breathlessness
| Sensitivity (%) | Specificity (%) | % Correcta | % Upcodedb | % Downcodedc | |
|---|---|---|---|---|---|
| Model A (0, 1–4, 5–8, and 9–10) | 87 | 78 | 74.8 | 17.8 | 9.6 |
| Model B (0, 1–5, 6–8, and 9–10) | 63 | 93 | 74.7 | 8.1 | 17 |
Model A uses a Numerical Rating Scale (NRS) cutpoint of 4, whereas Model B uses an NRS cutpoint of 5. Sensitivity and specificity of these cutpoints to distinguish moderate or greater dyspnea are reported. The % correct, upcoded, and downcoded reflects the aggregate of all patients, all questions, and all days.
Percent of patients where the NRS and Verbal Descriptor Scale (VDS) were equivalent.
Percent of patients where the NRS attributed a higher VDS than the patients attributed themselves.
Percent of patients where the NRS attributed a lower VDS than the patients attributed themselves.
Discussion
VDSs are practical tools for dyspnea monitoring in the clinic when more complicated scales such as a full 0–10 NRS may not be feasible. In this analysis, we demonstrate that the dyspnea VDS performs as expected, with tight clustering of NRS scores within VDS categories. Corresponding VDS and NRS scores have face validity.
In translating NRS to VDS, identification of NRS cutpoints for the transition from mild to moderate or moderate to severe is an important consideration. In pain, cutpoint identification has been addressed in multiple studies, across multiple disease states.24 In general, most studies yielded cutpoints identical to those identified by Serlin et al.,16 who used functional impairment to inform on pain severity in patients with metastatic cancer. The optimal NRS ranges identified in that study were 1–4 for mild, 5–6 for moderate, and 7–10 for severe. The consistency and similarities between the VDS for pain and ours for dyspnea suggest that verbal rating scales may have better inter-rater reliability. As shown previously in pain and confirmed here, there appears to be a uniform semantic meaning of the verbal descriptors mild, moderate, and severe.25,26 Notably, these verbal descriptors and their numerical associations differ from the modified Borg scale.
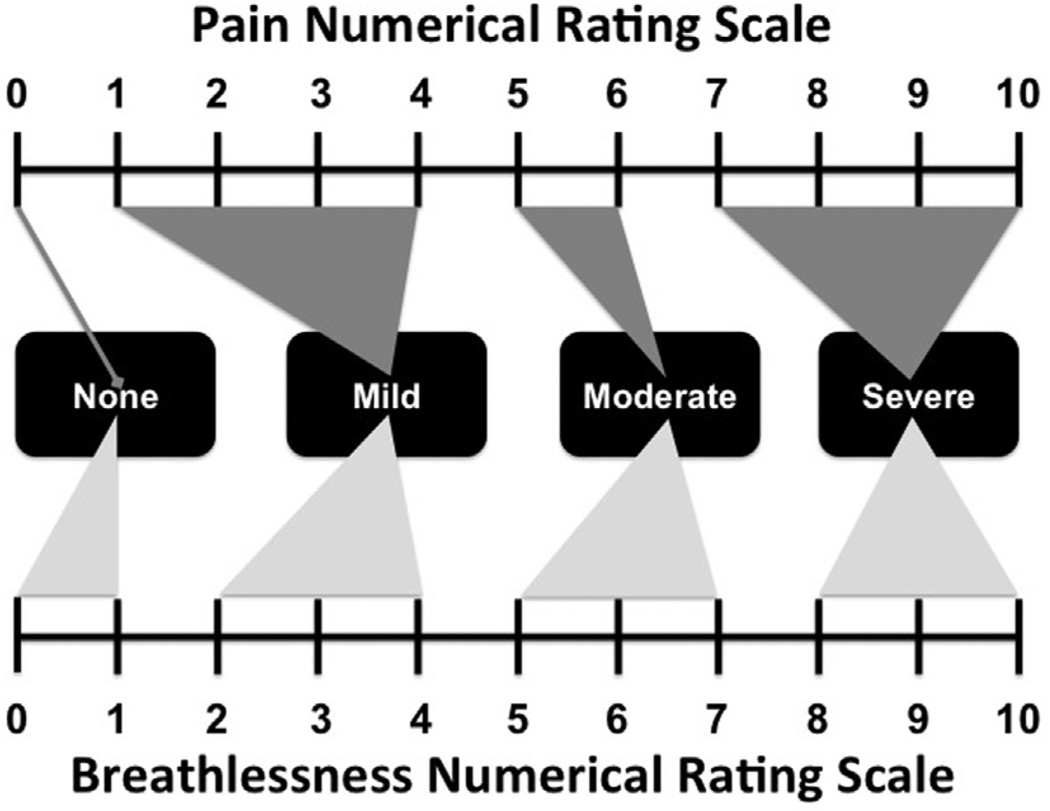
For dyspnea, we have identified reasonable clustering of NRS scores among VDS categories and established practical cutpoints. Based on the transition points (Fig. 2), in combination with the comparative performance characteristics, we propose the following cutpoints: 0 for none, 1–4 for mild, 5–8 for moderate, and 9–10 for severe (Table 3, Model A; Fig. 3). The cutpoints from none to mild and moderate to severe, based on the distribution of responses, are straightforward. The cutpoint from mild to moderate is less clear, though, because of the nearly even distribution of VDS and NRS around this transition. We made the recommendation for a mild to moderate cutpoint of 5 based on the superior sensitivity of this cutpoint to minimize downgrading. Clinically, downgrading symptom severity poses the risk of leaving clinical needs unaddressed, which is potentially more harmful than overestimating symptom burden. Of course, this consideration also must be balanced against the potential of exposing patients to unnecessary treatments if their symptoms are upgraded.
Fig. 3.
Practical relationships between Numerical Rating Scale and Verbal Descriptor Scale for pain (top, based on results from Refs.15,16) and breathlessness (bottom, based on this study).
As discussed in the longitudinal analysis, the VDS tracked with the NRS, suggesting both are responsive to changes in dyspnea. Furthermore, this study demonstrates that, for these data, numerical differences between pairs of subsequent verbal descriptors are equal (Table 2), which may allow subsequent analyses to treat these VDS categories as interval variables, rather than ordinal, where this is appropriate. This provides practical opportunities for analyses when the VDS is incorporated into clinical research and quality monitoring programs.
The parallels we have drawn between pain and dyspnea are supported elsewhere in the literature,27 especially in light of growing evidence for dyspnea management strategies that parallel pain management strategies such as opioids.28 Similarly, there is more focus on integrated assessment and care models for dyspnea that parallel pain. For example, total breathlessness describes the concept whereby, like pain, breathlessness is experienced as an amalgamation of physical, psychosocial, and spiritual problems.25 This concept is supported by involvement of both cortical and subcortical central pathways in the perception of breathlessness,26,29 with strong similarities with those involved in the perception of pain and similar patterns demonstrated by functional magnetic resonance imaging.30
Pain management has become an integral component of most clinical assessments, but only after consensus regarding routine pain assessment tools was achieved. Similarly, as therapeutic options for dyspnea evolve, widespread clinical implementation will depend on ubiquitous and longitudinal dyspnea assessment using a simple, intuitive, and practical tool.31 The VDS and NRS are intended to fill this role, with the VDS being the most practical and efficient, and the NRS most useful when more fine-tuned information is needed. For purposes of simplicity, we anticipate that some health care providers, health systems, or electronic health records may choose to adopt the VDS for routine monitoring of dyspnea.
Beyond being simple, intuitive, and practical, the VDS scale and the proposed corresponding NRS cutpoints have implications for efficacy trials. In many pain management efficacy trials, the cutpoint for inclusion is the NRS cutpoint corresponding to moderate pain.19,20 Considering the VDS to NRS cutpoints for moderate dyspnea identified in this study (i.e., moderate dyspnea corresponds to a starting point of NRS of 5), it is sensible to use an NRS of 5 or greater as a practical eligibility criterion for trials of novel dyspnea therapeutic interventions. Despite the distributional overlap between mild and moderate dyspnea, this cutpoint yields an 87% sensitivity and 78% specificity for moderate or severe dyspnea. If some enrolling centers use an NRS, whereas others use a VDS, understanding this relationship may be useful in screening records for recruitment or informing multicenter research.
This study has several limitations. As has previously been described, VDSs offer less granularity, are unidimensional, and may be insufficiently sensitive to detect small, but potentially meaningful, changes in symptom severity.32 Further work is needed to better characterize the reliability, validity, responsiveness, and determine clinically relevant changes of this VDS for breathlessness, all of which are beyond the scope of this analysis. Additionally, the assumption that increments between each ordinal category are numerically similar is frequently cited as a limitation of VDSs. In this study, however, the difference in mean NRS score for each VDS category was very consistent (Table 2), suggesting that, at least from a population standpoint, there is a consistent incremental stepwise relationship between the VDS categories. One limitation of single-item scales is that they can be influenced by the affective experience of dyspnea and may not completely isolate the somatosensory intensity of dyspnea. These instruments are not designed to discriminate between the various contributors to dyspnea (e.g., pulmonary disease, mood disturbance, lack of social support, existential distress). It has been demonstrated that single-item ratings of pain are more reflective of psychosocial distress than pathophysiologic processes.33 Neither the parent study nor this substudy intended to evaluate the primary drivers of the experience of breathlessness. Thus, heterogeneity in the components of breathlessness between participants is likely; in fact, there was marked heterogeneity among the diagnoses driving the breathlessness in this study. These scales are not intended to replace such instruments in research protocols where the components of breathlessness are of interest.
As dyspnea management continues to evolve, implementation of an assessment tool that is clinically practical and intuitive is necessary. We have demonstrated good correlation between verbal descriptor and NRSs for dyspnea in a population with life-limiting illness and refractory dyspnea and have identified practical cutpoints relating the NRS to VDS. These scales are practical and clinically intuitive and can be easily integrated into routine clinical practice and provide cutpoints that can be used to screen for inclusion in clinical dyspnea management trials.
Acknowledgments
This was a planned substudy of a randomized controlled trial funded by the U.S. National Institutes of Health/National Institute of Aging, Australian National Health and Medical Research Council, Duke Institute for Care at the End of Life, and Doris Duke Charitable Foundation. The funding sources had no role in the study design, collection, analysis, and interpretation of the data, in the writing of this report, or the decision to submit this article for publication. Dr. Abernethy has research funding from DARA Biosciences, GlaxoSmithKline, Celgene, Helsinn Therapeutics, Dendreon, Kanglaite, Bristol-Myers Squibb, and Pfizer, as well as federal sources (National Institute of Nursing Research U24 NR014637-02; UC4-12584); these funds are all distributed to Duke University Medical Center to support research including salary support for Dr. Abernethy. Pending industry-funded projects include Galena Biopharma and Insys Therapeutics. She has consulting agreements with or received honoraria from Novartis and from Pfizer (<$5000 annually) and from Bristol-Myers Squibb (>$5000 annually). Dr. Abernethy has corporate leadership responsibility in Flatiron Health, Inc. (Chief Medical Officer & Senior Vice President), athena-health, Inc. (Director), Advoset LLC (Owner), and Orange Leaf Associates LLC (Owner). Dr. Currow is an unpaid advisory board member to Helsinn Pharmaceuticals.
The authors acknowledge Tracie Locklear, PhD, for her assistance in the preparation of this article.
Footnotes
Disclosures
Drs. Miriovsky, Wysham, Herndon, Samsa, and Wilcock have no disclosures to report.
References
- 1.American Thoracic Society. Dyspnea. Mechanisms, assessment, and management: a consensus statement. Am J Respir Crit Care Med. 1999;159:321–340. doi: 10.1164/ajrccm.159.1.ats898. [DOI] [PubMed] [Google Scholar]
- 2.Lynn J, Teno JM, Phillips RS, et al. Perceptions by family members of the dying experience of older and seriously ill patients. Ann Intern Med. 1997;126:97–106. doi: 10.7326/0003-4819-126-2-199701150-00001. [DOI] [PubMed] [Google Scholar]
- 3.Mercadante S, Casuccio A, Fulfaro F. The course of symptom frequency and intensity in advanced cancer patients followed at home. J Pain Symptom Manage. 2000;20:104–112. doi: 10.1016/s0885-3924(00)00160-3. [DOI] [PubMed] [Google Scholar]
- 4.Seow H, Barbera L, Sutradhar R, et al. Trajectory of performance status and symptom scores for patients with cancer during the last six months of life. J Clin Oncol. 2011;29:1151–1158. doi: 10.1200/JCO.2010.30.7173. [DOI] [PubMed] [Google Scholar]
- 5.Bausewein C, Booth S, Gysels M, et al. Individual breathlessness trajectories do not match summary trajectories in advanced cancer and chronic obstructive pulmonary disease: results from a longitudinal study. Palliat Med. 2010;24:777–786. doi: 10.1177/0269216310378785. [DOI] [PubMed] [Google Scholar]
- 6.Currow DC, Smith J, Davidson PM, et al. Do the trajectories of dyspnea differ in prevalence and intensity by diagnosis at the end of life? A consecutive cohort study. J Pain Symptom Manage. 2010;39:680–690. doi: 10.1016/j.jpainsymman.2009.09.017. [DOI] [PubMed] [Google Scholar]
- 7.Tanaka K, Akechi T, Okuyama T, et al. Prevalence and screening of dyspnea interfering with daily life activities in ambulatory patients with advanced lung cancer. J Pain Symptom Manage. 2002;23:484–489. doi: 10.1016/s0885-3924(02)00394-9. [DOI] [PubMed] [Google Scholar]
- 8.Dorman S, Byrne A, Edwards A. Which measurement scales should we use to measure breathlessness in palliative care? A systematic review. Palliat Med. 2007;21:177–191. doi: 10.1177/0269216307076398. [DOI] [PubMed] [Google Scholar]
- 9.Bausewein C, Farquar M, Booth S, Gysels M, Higginson IJ. Measurement of breathlessness in advanced disease: a systematic review. Respir Med. 2007;101:399–410. doi: 10.1016/j.rmed.2006.07.003. [DOI] [PubMed] [Google Scholar]
- 10.Tanaka T, Akechi T, Okuyama T, Nishiwaki Y, Uchitomi Y. Development and validation of the Cancer Dyspnoea Scale: a multidimensional, brief, self-rating scale. Br J Cancer. 2000;82:800–805. doi: 10.1054/bjoc.1999.1002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mador MJ, Kufel TJ. Reproducibility of visual analog scale measurements of dyspnea in patients with chronic obstructive pulmonary disease. Am Rev Respir Dis. 1992;146:82–87. doi: 10.1164/ajrccm/146.1.82. [DOI] [PubMed] [Google Scholar]
- 12.Gift AG, Narsavage G. Validity of the numeric rating scale as a measure of dyspnea. Am J Crit Care. 1998;7:200–204. [PubMed] [Google Scholar]
- 13.Wilcock A, Crosby V, Clarke D, Tattersfield A. Repeatability of breathlessness measurements in cancer patients. Thorax. 1999;54:375. doi: 10.1136/thx.54.4.374b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Borg GA. Psychophysical bases of perceived exertion. Med Sci Sports Exerc. 1982;14:377–381. [PubMed] [Google Scholar]
- 15.Burdon J, Juniper E, Killian K, et al. The perception of breathlessness in asthma. Am Rev Respir Dis. 1982;126:825–828. doi: 10.1164/arrd.1982.126.5.825. [DOI] [PubMed] [Google Scholar]
- 16.Serlin RC, Mendoza TR, Nakamura Y, Edwards KR, Cleeland CS. When is cancer pain mild, moderate or severe? Grading pain severity by its interference with function. Pain. 1995;61:277–284. doi: 10.1016/0304-3959(94)00178-H. [DOI] [PubMed] [Google Scholar]
- 17.Jones KR, Vojir CP, Hutt E, Fink R. Determining mild, moderate, and severe pain equivalency across pain-intensity tools in nursing home residents. J Rehabil Res Dev. 2007;44:305–314. doi: 10.1682/jrrd.2006.05.0051. [DOI] [PubMed] [Google Scholar]
- 18.Edelen MO, Saliba D. Correspondence of verbal descriptor and numeric rating scales for pain intensity: an item response theory calibration. J Gerontol A Biol Sci Med Sci. 2010;65:778–785. doi: 10.1093/gerona/glp215. [DOI] [PubMed] [Google Scholar]
- 19.Muriel C, Failde I, Mico JA, et al. Effectiveness and tolerability of the buprenorphine transdermal system in patients with moderate to severe chronic pain: a multicenter, open-label, uncontrolled, prospective, observational clinical study. Clin Ther. 2005;27:451–462. doi: 10.1016/j.clinthera.2005.04.007. [DOI] [PubMed] [Google Scholar]
- 20.Mercadante S, Porzio G, Ferrera P, et al. Sustained-release oral morphine versus transdermal fentanyl and oral methadone in cancer pain management. Eur J Pain. 2008;12:1040–1046. doi: 10.1016/j.ejpain.2008.01.013. [DOI] [PubMed] [Google Scholar]
- 21.Abernethy AP, McDonald CF, Frith PA, et al. Effect of palliative oxygen versus room air in relief of breathlessness in patients with refractory dyspnoea: a double-blind, randomised controlled trial. Lancet. 2010;376:784–793. doi: 10.1016/S0140-6736(10)61115-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Fletcher CM, Clifton M, Fry J, et al. Standardized questionnaire on respiratory symptoms. BMJ. 1960;2:1665. [Google Scholar]
- 23.Fierro-Carrion G, Mahler DA, Ward J, et al. Comparison of continuous and discrete measurements of dyspnea during exercise in patients with COPD and normal subjects. Chest. 2004;125:77–84. doi: 10.1378/chest.125.1.77. [DOI] [PubMed] [Google Scholar]
- 24.Li KK, Harris K, Hadi S, Chow E. What should be the optimal cut points for mild, moderate, and severe pain? J Palliat Med. 2007;10:1338–1346. doi: 10.1089/jpm.2007.0087. [DOI] [PubMed] [Google Scholar]
- 25.Abernethy AP, Wheeler JL. Total dyspnoea. Curr Opin Support Palliat Care. 2008;2:110–113. doi: 10.1097/SPC.0b013e328300cad0. [DOI] [PubMed] [Google Scholar]
- 26.Abernethy AP, Kamal AH, Wheeler JL, Cox C. Management of dyspnea within a rapid learning healthcare model. Curr Opin Support Palliat Care. 2011;5:101–110. doi: 10.1097/SPC.0b013e32834582b3. [DOI] [PubMed] [Google Scholar]
- 27.Currow DC, Abernethy AP. Therapeutic nihilism: the next hurdle in improving the treatment of breathlessness. Curr Opin Support Palliat Care. 2011;5:69–70. doi: 10.1097/SPC.0b013e32834680ea. [DOI] [PubMed] [Google Scholar]
- 28.Mahler DA, Selecky PA, Harrod CG, et al. American College of Chest Physicians consensus statement on the management of dyspnea in patients with advanced lung or heart disease. Chest. 2010;137:674–691. doi: 10.1378/chest.09-1543. [DOI] [PubMed] [Google Scholar]
- 29.Banzett RB, Mulnier HE, Murphy K, et al. Breathlessness in humans activates insular cortex. Neuroreport. 2000;11:2117–2120. doi: 10.1097/00001756-200007140-00012. [DOI] [PubMed] [Google Scholar]
- 30.Evans KC, Banzett RB, Adams L, et al. Bold fMRI identifies limbic, paralimbic, and cerebellar activation during air hunger. J Neurophysiol. 2002;88:1500–1511. doi: 10.1152/jn.2002.88.3.1500. [DOI] [PubMed] [Google Scholar]
- 31.von Leupoldt A, Sommer T, Kegat S, et al. Dyspnea and pain share emotion-related brain network. Neuroimage. 2009;48:200–206. doi: 10.1016/j.neuroimage.2009.06.015. [DOI] [PubMed] [Google Scholar]
- 32.Deschamps M, Band PR, Coldman AJ. Assessment of adult cancer pain: shortcomings of current methods. Pain. 1988;32:133–139. doi: 10.1016/0304-3959(88)90061-9. [DOI] [PubMed] [Google Scholar]
- 33.Clark WC, Yang JC, Tsui S-L, Ng K-F, Bennett Clark S. Unidimensional pain rating scales: a multidimensional affect and pain survey (maps) analysis of what they really measure. Pain. 2002;98:241–247. doi: 10.1016/S0304-3959(01)00474-2. [DOI] [PubMed] [Google Scholar]