Abstract
Objective
The objective of this study was to determine what aspects of prehospital pediatric airway management may contribute to patient safety events.
Methods
We conducted a 3-phase Delphi survey in prehospital professionals across the US to identify potential contributors to patient safety events. Respondents ranked how likely factors were to contribute on a 9-point Likert-type scale and were allowed to elaborate through open-ended questions. Analysis was conducted using a mixed-methods approach including Likert-type responses and open ended questions which were analyzed for specific themes.
Results
All 3 phases of the survey were completed by 492 participants; 50.8% of respondents were paramedics, 22% were EMT-Basics/first responders, and 11.4% were physicians. Seventy-five percent identified lack of experience with advanced airway management and 44% identified medical decision making regarding airway interventions as highly likely to lead to safety events. Within the domain of technical skills, advanced airway management was ranked in the top 3 contributors to safety events by 71% of participants, and bag mask ventilation by 18%. Qualitative analysis of questions within the domains of equipment and technical skills identified endotracheal intubation as the top contributor to safety events, with bag-mask-ventilation second. In the domains of assessment and decision making respiratory assessment and knowing when to perform and advanced airway were ranked most highly.
Conclusion
This national Delphi survey identified lack of experience with pediatric airway management and challenges in decision making in advanced airway management as high risk for safety events with endotracheal intubation as the most likely of these.
Introduction
Airway management is the cornerstone of clinical resuscitation for many medical conditions and is particularly important in pediatric resuscitation. Prehospital pediatric airway management is a subject of considerable controversy.1 Advanced airway procedures are rare for any individual Emergency Medical Services (EMS) provider, particularly among children: paramedics in urban areas may perform an intubation on a child only once every 4–5 years while potentially intubating adults with greater frequency.2 In conditions such as traumatic brain injury, cardiac arrest, and other medical and traumatic emergencies appropriate airway management, either basic (bag-valve-mask ventilation) or advanced (endotracheal intubation) is critical to successful resuscitation. Endotracheal intubation through rapid sequence intubation (RSI) has long been central to traditional definitive airway management in the hospital setting for emergency airway management of patients of any age, and is assumed by many to be beneficial outside the hospital. However, available evidence suggests that the benefit of prehospital pediatric endotracheal intubation is unclear, with the potential for increased complications compared to intubation in the hospital.3,4,5 A controlled trial in an urban area found that there was no benefit to endotracheal intubation compared to bag-valve-mask (BVM) ventilation with a trend towards harm in one subgroup.6 Another study found increased complications during attempts at endotracheal intubation in rural areas compared to the Emergency Department attempts.3
Although these studies indicate the potential for safety events during pediatric prehospital airway management, they do not describe the mechanisms or specific aspects of advanced airway management that are responsible for such events. A recent national Delphi survey on prehospital patient safety performed by the Children’s Safety Initiative-EMS (CSI-EMS) which is currently in revision identifies advanced airway management as the highest risk area for patient safety events. This hypothesis generating study analyzes this extensive Delphi survey to understand the highest risk aspects of advanced airway management and potential mechanisms for patient safety events.
Methods
We used SurveyMonkey™ to administer a 3-phase Delphi survey among EMS professionals. Traditional Delphi survey methods were used to achieve consensus among a group of informed national EMS experts.7 The Delphi method involves a process where a panel of experts is surveyed in multiple rounds with results from each round informing the next in order to obtain group consensus. This method is significantly different than traditional surveys as the same participants participate in each round of the survey allowing for deeper insight into the topic. Also, the survey questions evolve with each round based on responses in the previous round.
Survey participants included Emergency Physicians, and Nurses, as well all levels of prehospital providers (EMT-Paramedic, EMT-Intermediate, EMT-Basic, and First Responders). Participants were excluded if they were less than 18 years of age or failed to complete the demographics section of the survey. Participants were recruited via email using professional group list serves, State EMS for Children directors throughout the United States and territories, as well as social media. The study was reviewed and approved by the Institutional Review Board of Oregon Health & Science University IRB Number 00006942.
In the survey, participants ranked how likely certain factors were to contribute to safety events on a 9-point Likert-type scale and answered free text open-ended questions to elaborate in the following domains: equipment; technical and procedural skills; assessment and decision making; training and equipment; medications; and scene management. In round one of the survey we included Likert-type questions related to airway management for each domain. For example, in the domain of assessment and decision making, we asked participants to rank the likelihood that knowing when to perform and advanced airway procedure is an important contributor to safety events or errors, with 1 indicating not at all likely and 9 indicating highly likely.
Questions were advanced from the first to the second round of the survey based on the percent of participants who ranked the item highly likely to contribute to safety events (choices 7–9 on the Likert-type scale). In addition to the questions advanced from round 1, the second round of the survey included 18 open-ended questions intended to aid interpretation of the quantitative results and to identify major domains that may not have been covered in other questions. For example, for each domain in the second round, participants were asked to provide free text responses describing the top clinical scenarios in which safety events were likely. In addition, participants were asked to identify the most challenging procedural and technical skills. Items were advanced to the third survey round in a similar manner and participants again ranked likelihood that each factor was a contributor to safety events.
Survey results were analyzed using SPSS™. Qualitative analysis was performed by developing and ecological model of pediatric airway management, identifying themes in the responses under these domains, and counting the frequency with which these themes were mentioned using NVivo™ software. Two research assistants experienced in conducting qualitative analysis independently reviewed the responses and analyzed the data using a hierarchical framework with initial themes/nodes, which were then broken into subthemes. All themes and subthemes were reviewed and verified by the larger study team and any discrepancies were resolved through group consensus.
Results
Initially, 755 participants consented to participate in the study. Two were excluded due to age (under 18) and 16 were excluded due to lack of specifying profession in the demographic section. Thus, 737 participants were included in the analysis of round 1 of the survey. Of the 753 round 1 participants who met age criteria and were invited to participate in round 2, 614 (82%) completed round 2 and 492 (65%) completed round 3. EMT Paramedics made up 50.8% of the original cohort and 51.5% of the round 3 cohort. The proportion of all professional groups varied less than 2% across the 3 phases of the survey. In the end, 492 participants completed all 3 phases of the survey: 50.8% of respondents were paramedics; 22% were EMT-Basics/first responders, and 11.4% were physicians.
Quantitative Questions
In the final round of the survey, airway management was ranked as the most likely aspect of care to lead to patient safety events. Seventy-five percent of survey participants identified lack of experience with advanced airway management as highly likely to lead to safety events with Likert-type scale scores 7–9 on the scale of 1–9. Forty-four percent identified medical decision making with regard to advanced airway interventions as highly likely to lead to patient safety events. Within the domain of technical skills, advanced airway was ranked as one of the top 3 potential contributors to safety events by 71% of participants while bag mask ventilation was ranked in the top 3 by only 18%.
Qualitative Questions
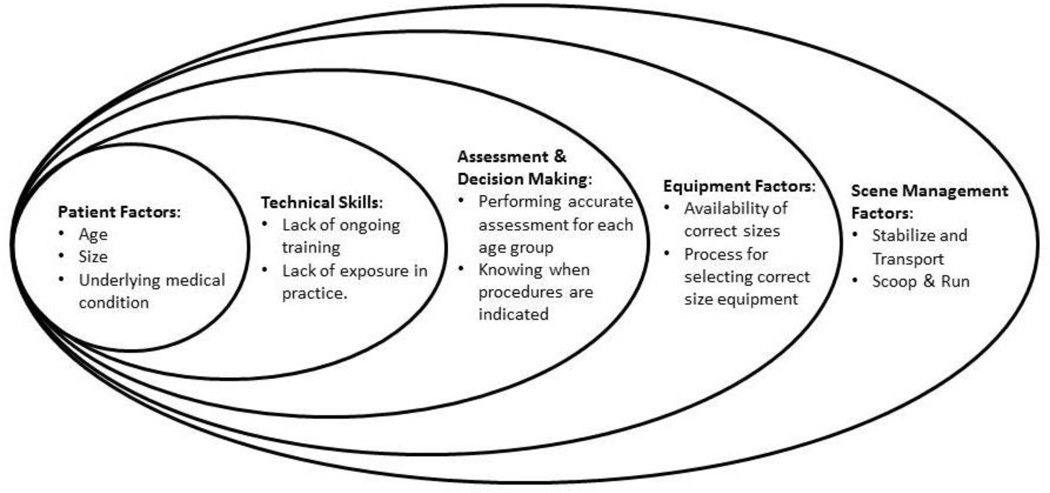
Themes from the qualitative analysis were organized into an ecological model of pediatric airway management, displayed in Figure 1.8,9 The figure provides a motif for understanding the multiple domains contributing to safety events, beginning with characteristics of the child as most central and expanding to more distal influences such as scene management factors. Under technical and procedural skills, respondents quantitatively identified intubation and bag mask ventilation as areas likely to contribute to safety events with 71% and 18% of respondents ranking them in the top 3 areas likely to contribute to safety events respectively. They qualified this in their open-ended responses by describing that the specific factors responsible for this included lack of experience taking care of children, too little training, and lack of familiarity with the specific pediatric equipment needed.
Figure 1.
Ecological model of pediatric airway management
In the domain of assessment and decision making, assessment of patients with respiratory arrest was often mentioned as likely to contribute to safety events. One representative quote from a Paramedic was: “Advanced airway emphasis has changed greatly in last few years; particularly with younger pediatric patients, we have to be careful to ’do no harm’ by going to intubation with the limited pediatric experience in the field.” Additional comments indicated challenges in general assessment of respiratory distress with specific indication that asthma may be an area likely to lead to safety events.
Lack of experience and training in the respiratory assessment of children were again indicated as reasons for difficulty in assessment and decision making. A physician respondent indicated that there are commonly problems with: “Accuracy of vital signs, accuracy of overall assessment as to how sick child is.” One respondent commented that: “EMS providers need to know what patient history information is most essential to assessment and making treatment decision. In addition, knowing how to communicate with children with and without parental or caretaker involvement is not dealt well in most EMS courses.” Table 1 includes additional comments from the qualitative analysis related to assessment and decision making.
Table 1.
Qualitative responses related to assessment and decision making in patients with respiratory distress or failure
| “[I have difficulty] knowing when to start BVM ventilation.” |
| “[I have difficulty] knowing when to perform [an] advanced airway over BLS.” |
| “Providers are not versed enough in pediatric assessment and treatment. [Even] 5 years out from EMT or paramedic education they may have only dealt with pediatrics on 2–5% of their calls.” |
| “[I worry about causing] airway trauma due to fact of smaller airways and smaller equipment.” |
| “EMS providers frequently err in wasting time attempting to obtain a "definitive" airway when they could have easily bag mask ventilated safely.” |
In the domain of equipment, providers indicated that equipment use in endotracheal intubation, bag mask ventilation, and oxygen administration was likely to lead to safety events. Respondents noted that identification of the correct size of equipment for the patient and then having that equipment available could lead to safety events. Few providers discussed airway adjuncts such as supraglottic devices, which may be due to lack of availability with one paramedic commenting: “the use of adjuncts and prompts are only as good as their availability and being able to find them in an emergency.” One provider noted their sentiment that, “choosing the wrong size intubation equipment…, preventing being able to secure an airway could lead to death.” This comment seems to reflect the concern that children may die due to lack of endotracheal intubation.
Using length-based equipment sizing systems was also noted to be a potential source of errors related to equipment and medications needed to facilitate intubation. One paramedic commented that: “Although the Broselow tape and other adjuncts are available, they aren't practiced with enough to make the rescuer comfortable using them.” Another paramedic noted: “Broselow tapes only have a few doses and some concentrations are not clear enough for most under pressure.” Related to medications one paramedic noted the trend that: “Many EMS agencies purchase medications from whichever company provides the item for the least amount of money. This causes inconsistency in pre-packaged medications.” Several additional quotes from the qualitative analysis related to equipment are included in Table 2.
Table 2.
Qualitative responses related to equipment used in airway management
| “When faced with the situation to control a pediatric airway the provider is faced not only with the infrequency of the skill… but the ability to identify the proper sized equipment such as ET Tube, laryngoscope blade, method of tube confirmation, securing device, etc.” |
| “Inability to choose the correct airway management equipment could lead to disastrous consequences, whether related to inappropriate ET tube size, ventilation volumes with manual BVM or inspiration pressures if using manometers or ventilator settings.” |
| “Equipment bags not based on color codes from length based measurement devices.” |
| “Lack of a Broselow device or measurement tool to determine appropriate sizes.” |
In an effort to determine how scene management may impact safety in airway management, we asked respondents to identify scenarios where the “scoop and run” and/or “stabilize and transport” strategies may contribute to errors or cause harm. In the “stabilize and transport” strategy, providers may be more likely to intubate prior to transport compared to the “scoop and run” where the focus is on getting to the hospital as quickly as possible. Responses were highly variable with respiratory arrest, respiratory distress, airway management, and asthma all frequently mentioned as potentially being high risk for safety events with both strategies. One paramedic noted: “There is a lack of comfort with most EMS providers when it comes to pediatric patients. Most want to do a ‘scoop and run’. Most do not do an adequate assessment. Few feel comfortable treating [children].” Physicians commented that the decision to scoop and run vs. stabilize and transport was a situation in which errors were likely to occur.
Discussion
This national mixed methods Delphi study identified several aspects of airway management as important potential contributors to safety events. Endotracheal intubation was frequently identified as having a high risk for safety events. Bag-mask ventilation, assessment of respiratory distress, identification of appropriate sized equipment, tracheostomy care, and scene management were also identified as areas of airway management which are likely to contribute to safety events. Through all of these aspects of airway management, lack of experience and training in pediatric airway management and respiratory assessment seemed to be at the root of potential errors.
Endotracheal intubation is a controversial topic in pediatric prehospital airway management. Studies demonstrating safety, efficacy, and improved outcomes compared to bag-mask ventilation are lacking. The existing literature, though sparse and mostly observational, has generally found worse outcomes or no difference when comparing prehospital intubation to bag-mask ventilation, though one rural study identified increased complications in prehospital intubations compared to intubations in the Emergency Department.3,10,6,4 Lack of experience in pediatric airway management is one of the fundamental factors making errors likely in these scenarios: advanced airway management in children is very rare for any individual paramedic, with less than 1% of pediatric calls needing advanced airway management and paramedics, who have limited baseline training, averaging only one pediatric intubation every 5 years even in densely populated urban areas.2,11 One comment seemed to reflect the sentiment that inability to intubate could result in death, though this is clearly not the case in the vast majority of cases and is not supported by current literature. The combination of inexperience with intubation and lack of knowledge of the safety of other modalities of airway management could be a very high risk situation, though one which may be corrected with an educational intervention.
Some of the available adult literature has found prehospital intubation to be safe and effective.12,13,14 However the existing literature is largely observational and many studies find no benefit or harm, and methodological issues make causative conclusions difficult from these studies.15,16,17 A recent randomized controlled trial did find favorable neurologic outcomes at 6 months in adults with severe traumatic brain injury who were intubated in the prehospital setting, rather than waiting to intubate until they reached the hospital.18 This contradicts the only pediatric controlled trial, which found a trend towards harm in brain injured children intubated prior to hospital arrival.6 These seemingly conflicting data may stem from fundamental differences between adult and pediatric diseases with different pathophysiology in the various age groups. For example, the pulmonary functional residual capacity is much lower in children compared to adults, and pediatric patients experience oxygen desaturation much more quickly after apnea compared to adults. Intubation attempts in children may be more likely to cause secondary brain injury due to the potential for rapid oxygen desaturation if meticulous attention is not given to oxygenation during attempts. It is also possible that the technical aspects of pediatric intubation are different that in adults and the general lack of experience makes this a rare and high risk procedure. Anxiety in caring for pediatric patients may distract providers and lead to suboptimal peri-intubation care such as unrecognized hypoxia, or hyper/hypo ventilation.
Pediatric airway management is a low-frequency, high-risk event for prehospital providers with lack of experience affecting every aspect from equipment sizing and medication use to technical skills such as bag mask ventilation and endotracheal intubation. It is unlikely that in our current EMS system prehospital providers will increase their exposure to pediatric patient to the degree needed. Educational interventions, including simulation, are a promising avenue to improve experience though simulation is financially costly and resource intensive with a relatively limited group of providers who are experts in pediatric prehospital care to oversee the training. Such trainings need to be repeated regularly to ensure skill retention. Several rigorous pediatric prehospital simulation programs have been described but were generally funded by grants with a limited audience and funding period. High quality realistic online training modules which potentially incorporate videos of patients could be a more cost effective and scalable solution. However, this type of training are likely better suited to domains of assessment and clinical decision making than technical skill competency. As the ecological model in Figure 1 illustrates, airway issues span many domains of prehospital safety with technical skills being only one such domain.
Medication facilitated intubation is routine practice in some areas. One respondent noted inconsistent packaging and labeling of the medications and other supplies by various companies. Recent medication shortages have made frequent changes of medication suppliers common, and exposed providers to a varying array of packaging and labeling increasing the opportunity for error. It is interesting to note that many other industries, such as computing, have adopted certain standards across manufacturers and unfortunate that in medicine it is not the case. We advocate for national standardization of medications and supplies in order to improve safety.
Our study has several important limitations. As a qualitative study the results represent consensus opinion but do not address the epidemiology of airway management problems and the frequency of the actual safety issues. Our study participants included a high proportion of EMT paramedics whose scope of practice included advanced airway management, and the perceived importance of this skill may reflect response bias and underestimate important basic airway skills utilized by EMT basics and EMT intermediates with different scopes of practice.
Conclusions
Prehospital providers face many challenges in pediatric airway management including advanced and basic airway skills, equipment availability and the ability to choose appropriately sized equipment, accurate patient assessment, medical decision making, and scene management issues. Overall, endotracheal intubation was identified as a procedure with the highest potential risk. Provider inexperience and lack of training was the most common theme across all domains of airway management.
Acknowledgments
Grant support: this work is supported by the National Institute of Child Health and Human Development grant: “Epidemiology of Preventable Safety Events in Pre-hospital EMS of Children,” Grant # 1R01HD062478-04.
Footnotes
Conflicts of Interest: We have no conflicts of interests
Author Contributions Statement:
Drs. Guise and Meckler conceived the initial study idea and obtained the funding. Drs. Guise, Meckler, O’Brien, Jui, Lambert, and Cottrell refined the study ideas, interpreted study results, refined each survey round, and participated in analysis and revision. Mr. Engle helped recruit subjects and interpret study results. Ms C. and K. Dickenson administered the survey, collected, and analyzed data. Dr. Hansen assisted in data interpretation and analysis and was the primary author of the manuscript. All listed authors contributed substantially to revisions of the manuscript.
References
- 1.Anders J, Brown K, Simpson J, Gausche-Hill M. Evidence and Controversies in Pediatric Prehospital Airway Management. Clin Pediatr Emerg Med. 2014;15(1):28–37. [Google Scholar]
- 2.Babl FE, Vinci RJ, Bauchner H, Mottley L. Pediatric pre-hospital advanced life support care in an urban setting. Pediatr Emerg Care. 2001;17(1):5–9. doi: 10.1097/00006565-200102000-00002. [DOI] [PubMed] [Google Scholar]
- 3.Ehrlich PF, Seidman PS, Atallah O, Haque A, Helmkamp J. Endotracheal intubations in rural pediatric trauma patients. J Pediatr Surg. 2004;39(9):1376–1380. doi: 10.1016/j.jpedsurg.2004.05.010. [DOI] [PubMed] [Google Scholar]
- 4.Holmes J, Peng J, Bair A. Abnormal end-tidal carbon dioxide levels on emergency department arrival in adult and pediatric intubated patients. Prehospital Emerg Care. 2012;16(2):210–216. doi: 10.3109/10903127.2011.640416. [DOI] [PubMed] [Google Scholar]
- 5.Gerritse BM, Draaisma JMT, Schalkwijk A, van Grunsven PM, Scheffer GJ. Should EMS-paramedics perform paediatric tracheal intubation in the field? Resuscitation. 2008;79(2):225–229. doi: 10.1016/j.resuscitation.2008.05.016. [DOI] [PubMed] [Google Scholar]
- 6.Gausche M, Lewis RJ, Stratton SJ, et al. Effect of out-of-hospital pediatric endotracheal intubation on survival and neurological outcome: a controlled clinical trial. 2000;283(6):783–790. doi: 10.1001/jama.283.6.783. [DOI] [PubMed] [Google Scholar]
- 7.Dalkey Norman C. The Delphi method : an experimental study of group opinion. Santa Monica: Rand Corporation, Distributed by Clearinghouse for Federal Scientific and Technical Information, U.S. Dept. of Commerce, National Bureau of Standards, Institute for Applied Technology; 1969. [Google Scholar]
- 8.Bronfenbrenner U. The Ecology of Human Development: Experiments by Nature and Design. Cambidge, MA: Harvard University Press; [Google Scholar]
- 9.Glass TA, McAtee MJ. Behavioral science at the crossroads in public health: extending horizons, envisioning the future. Soc Sci Med 1982. 2006;62(7):1650–1671. doi: 10.1016/j.socscimed.2005.08.044. [DOI] [PubMed] [Google Scholar]
- 10.DiRusso SM, Sullivan T, Risucci D, Nealon P, Slim M. Intubation of pediatric trauma patients in the field: predictor of negative outcome despite risk stratification. J Trauma. 2005;59(1):84–90. doi: 10.1097/01.ta.0000171462.28379.f3. [DOI] [PubMed] [Google Scholar]
- 11.Lerner EB, Dayan PS, Brown K, et al. Characteristics of the Pediatric Patients Treated by the Pediatric Emergency Care Applied Research Network’s Affiliated EMS Agencies. Prehosp Emerg Care. 2014;18(1):52–59. doi: 10.3109/10903127.2013.836262. [DOI] [PubMed] [Google Scholar]
- 12.Winchell RJ, Hoyt DB. ENdotracheal intubation in the field improves survival in patients with severe head injury. Arch Surg. 1997;132(6):592–597. doi: 10.1001/archsurg.1997.01430300034007. [DOI] [PubMed] [Google Scholar]
- 13.Ochs M, Davis D, Hoyt D, Bailey D, Marshall L, Rosen P. Paramedic-performed rapid sequence intubation of patients with severe head injuries. Ann Emerg Med. 2002;40(2):159–167. doi: 10.1067/mem.2002.126397. [DOI] [PubMed] [Google Scholar]
- 14.Davis DP, Peay J, Sise MJ, et al. Prehospital airway and ventilation management: a trauma score and injury severity score-based analysis. J Trauma. 2010;69(2):294–301. doi: 10.1097/TA.0b013e3181dc6c7f. [DOI] [PubMed] [Google Scholar]
- 15.Wang HE, Peitzman AB, Cassidy LD, Adelson PD, Yealy DM. Out-of-hospital endotracheal intubation and outcome after traumatic brain injury. Ann Emerg Med. 2004;44(5):439–450. doi: 10.1016/j.annemergmed.2004.04.008. [DOI] [PubMed] [Google Scholar]
- 16.Cudnik MT, Newgard CD, Daya M, Jui J. The impact of rapid sequence intubation on trauma patient mortality in attempted prehospital intubation. J Emerg Med. 2010;38(2):175–181. doi: 10.1016/j.jemermed.2008.01.022. [DOI] [PubMed] [Google Scholar]
- 17.Davis DP, Peay J, Sise MJ, et al. The impact of prehospital endotracheal intubation on outcome in moderate to severe traumatic brain injury. J Trauma. 2005;58(5):933–939. doi: 10.1097/01.ta.0000162731.53812.58. [DOI] [PubMed] [Google Scholar]
- 18.Bernard SA, Nguyen V, Cameron P, et al. Prehospital rapid sequence intubation improves functional outcome for patients with severe traumatic brain injury: a randomized controlled trial. Ann Surg. 2010;252(6):959–965. doi: 10.1097/SLA.0b013e3181efc15f. [DOI] [PubMed] [Google Scholar]