Abstract
The different levels of health information technology (IT) adoption and its integration into hospital workflow can affect the maximization of the benefits of using of health IT. We aimed at sharing our experiences and the journey to the successful adoption of health IT over 13 years at a tertiary university hospital in South Korea. The integrated system of comprehensive applications for direct care, support care, and smart care has been implemented with the latest IT and a rich user information platform, achieving the fully digitized hospital. The users experience design methodology, barcode and radio-frequency identification (RFID) technologies, smartphone and mobile technologies, and data analytics were integrated into hospital workflow. Applications for user-centered electronic medical record (EMR) and clinical decision support (CDS), closed loop medication administration (CLMA), mobile EMR and dashboard system for care coordination, clinical data warehouse (CDW) system, and patient engagement solutions were designed and developed to improve quality of care, work efficiency, and patient safety. We believe that comprehensive electronic health record systems and patient-centered smart hospital applications will go a long way in ensuring seamless patient care and experience.
Keywords: Hospital information system (HIS), electronic health records (EHR), health information technology (health IT), patient safety, patient engagement
Introduction
Health information technology (IT) and electronic health records (EHR) have the benefits of improving the quality of patient care, work efficiency of healthcare professionals, and satisfaction of patients as well as providers (1). However, the different levels of health IT adoption and its integration into hospital workflow can affect the maximization of the benefits of using of health IT. The implementation and use of health IT includes various challenging organizational aspects in terms of the structure of healthcare organizations, tasks, people policies, incentives, and information and decision processes (2).
This article is aimed at sharing the experiences and main achievements over 13 years of implementing hospital information systems (HIS) that include comprehensive EHR systems and patient-centered smart hospital applications in a tertiary university hospital, Seoul National University Bundang Hospital (SNUBH) in South Korea. SNUBH opened as a fully digitized hospital in May 2003, free of any paper-based medical records and with a homegrown EHR system. It was accredited as a HIMSS Analytics EMR Adoption Model Stage 7 hospital in October 2010. Notably, SNUBH was the first hospital outside the US to receive Stage 7 accreditation, a rating that was revalidated in March 2016 with the optimal use of health IT. Thus, our use of health IT to maximize its benefits and provide patient care in a more comprehensive manner would be expected to be helpful in adopting health IT systems and designing new innovative applications to other healthcare organizations.
Applications of a HIS
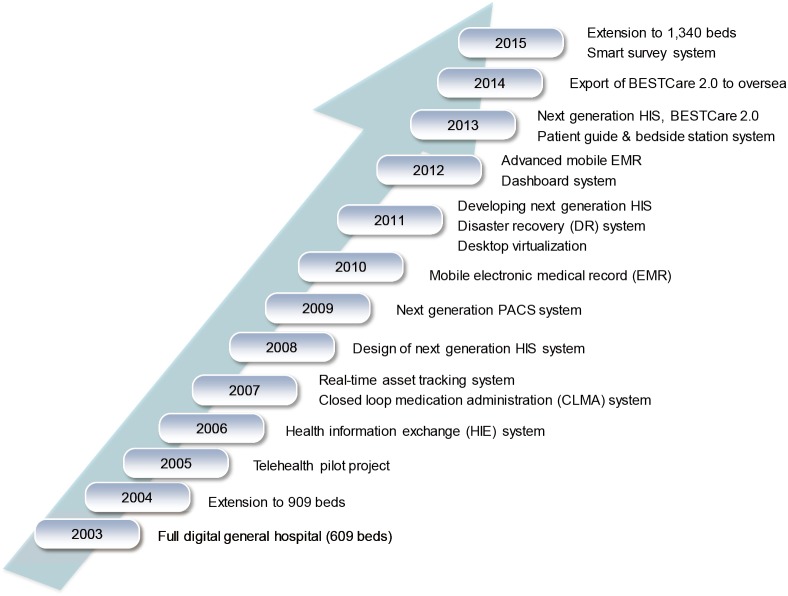
SNUBH’s HIS, named BESTCare, “Bundang hospital Electronic System for Total Care”, is an integrated system of comprehensive applications for direct care and support care of outpatients, inpatients, intensive care units, emergency room, and operating room units (3). Figure 1 shows the health IT adoption journey of SNUBH with the recent development of the next generation HIS, BESTCare 2.0, based on the latest IT and a rich user information platform.
Figure 1.
The health information technology adoption journey of Seoul National University Bundang Hospital.
User-centered EHR & clinical decision support systems (CDSS)
As the clinician’s user experience and satisfaction with the EHR system is one of the challenging barriers to health IT adoption, the BESTCare 2.0 system was re-designed to meet the increasing demands for ease of use and the ability for users to set preferences. The presentation of information in terms of layout and structure is important because it can influence data retrieval, interpretation, and clinical decision-making. Thus, we aimed at improving users’ work performance and satisfaction by providing a personalized, optimized, and common user interface (UI) to very busy clinicians.
By applying a user experience design methodology and analyzing over 3,000 requirements and new ideas collected from hospital users, we derived and implemented several key concepts as outlined below:
A patient journey map and patient summary sheet: a patient journey map shows all patient-related longitudinal events in the outpatient clinic, inpatient department, emergency department, and various examination suites in a visualized form. The patient summary sheet shows all the medical information about an individual patient, such as their history of surgical procedures, diagnoses, discharge summaries, test results, and medications. The tools enable medical staff to understand complex patient information at a glance;
Embedded picture archiving and communication systems (PACS): in order to increase the usability of accessing image testing, PACS was embedded into the EHR. Therefore, physicians do not need to open an additional popup window to view PACS. Different images, such as cardiology PACS and radiology PACS, can be easily and efficiently compared in a single window;
Flexible and interactive UI: using the window tile function, each user can configure and use his or her own UI rather than using fixed, common UI;
UI based on full high-dimension (HD) and a wide and large monitor: the large and wide single monitor can help medical staff to effectively review various and complex medical information;
Unified communication (UC) integrated with EHR: the integration of communication tools, such as telephone, email, cell phone, messenger, video call, and video conference systems, into the EHR system, enhances communication between co-operative users in real time.
A CDSS combined with an EHR system prevents human error during order entries and helps clinicians to make a decision on diagnosis and treatment with the latest scientific evidence, resulting in improved patient safety and quality of care.
Using a CDSS rule engine, we have implemented and supported several types of rules, such as overlapping prescriptions, drug-drug interaction, renal dosing guidelines, overdose prevention, contradictions for age, pregnancy, and breast feeding, and drug-disease interaction.
In addition, clinical pathways (CP) integrated with the EHR system can ensure standard care with best practice and expected care processes. Through a CP task force team of doctors, nurses, pharmacists, a health insurance review team, and IT experts, we designed and implemented over 150 CPs from 13 departments. This resulted in a CP application rate of over 85%, achieved by active participation from hospital staff and periodic monitoring/feedback and modification processes.
Patient safety with barcode enablement
Real-time documentation and cross-checking of care practices in the EMR using radio-frequency identification (RFID) and barcode technology have the potential to ensure patient safety, increase work efficiency, and improve care processes. It can reduce the administrative workload for nurses giving them more face-to-face time with patients, thus increasing patient satisfaction.
In SNUBH, RFID wristbands containing patient information were issued to inpatients. Then, the closed loop medication administration (CLMA) system using RFID and barcode technology was implemented in several areas: pharmacy, medication administration, blood bank, and a communal space storing human milk.
The RFID and barcode system enabled a hospital environment where care practices provided to inpatients could be conveniently and accurately documented by cross-checking patient information with medical orders. Furthermore, the delivery or transfer of medication, specimens, and materials could be tracked real-time. This traceable system improves the quality of care, prevents medical errors, and promotes efficient use of resources by emphasizing accountability.
Care coordination using n-device strategies
Mobile access to EHR systems anytime, anywhere, and from any device is essential for effective access to patient’s data and effective communication among healthcare professionals and patients. With n-device strategies for smart and mobile hospitals, we adopted and implemented the virtual desktop infrastructure (VDI), mobile EMR system, and large touch-screen based dashboard system.
The enterprise-wide adoption of cloud-based VDI allowed healthcare professionals to access the EHR system with full functionality outside the hospital. It also enabled nurses to visit a patient’s home without any paper/printed records and to both access and capture patient’s data on site, resulting in improved quality of care, reduced paper resources, and efficient access to medical records.
The mobile EMR system had features such as accessibility to most of the EMR data, including medical images, by integrating Mobile PACS, an easy-to-use UI, and support of all devices regardless of OS, as well as enhanced security with mobile device management (MDM) solutions.
The dashboard system on a 55-inch touchscreen monitor is a concise and context-specific display system showing all the clinical and business data in text, graphic, and image form on a single screen with at-a-glance view to facilitate ease of understanding and mutual communication between healthcare personnel and even with patients and family members. It has been utilized in wards and ICUs for team rounding, education of residents and students, and explanation of a patient’s medical status to patients and their families. It can also be effectively utilized for research that requires a group discussion and also a case conference for a collaborative study.
Data analytics & research support
For the use of EHR data in monitoring the quality of patient care and patient safety, as well as supporting clinical research, we implemented a clinical data warehouse (CDW) system. As demand for clinical quality improvement increased, we developed clinical quality indicators based on the CDW from 2005 and upgraded it with in-memory computing appliance in 2013 for faster access and search capability. Since its implementation, additional indicators including a 6-sigma indicator, clinical pathway indicator, performance indicator, customer indicator, quality medical record indicator, and infection control and insurance management indicators were further developed, maintained, and managed, resulting in over 400 electronic clinical indicators utilizing its CDW. As one of the many uses that contributed to improving the quality of patient care, the system was able to maintain optimal dosages of preoperative antibiotics by giving feedback of preoperative antibiotic prescription through continual monitoring (4).
The CDW system that provides big data analytics tools based on in-memory database technology enables better support data retrieval, extraction, and analysis for research as the big data issue is becoming a challenging research topic in healthcare. Thus, the CDW system included functions to retrieve unstructured medical records with free-text search and scenario-based retrieval of EMR data with a user-friendly interface.
Patient engagement using mobile technologies
Patient participation and engagement is significant in upholding the continuum of care and improving patients’ health by empowering self-management with greater information sharing. With the aim of reinforcing patient engagement, we developed various patient-centered systems using mobile technologies, such as personal health records (PHR), a smart survey system, and a smart bedside station system.
The patient portal and PHR app (5) provided patients with a personalized health record on their PC and smart devices, showing their medical records, medications, and laboratory test results. Patient-generated data such as weight, blood pressure, glucose, diet, and exercise was captured and stored into the EHR system, facilitating seamless communication between medical professionals and patients.
The smart survey system digitized and integrated self-administered questionnaires to assess patient condition and was utilized in various clinical departments including pediatric neurology, rehabilitation medicine, and oncology. As the questionnaires were completed by patients on various mobile devices and PCs in outpatient and inpatient settings, the questionnaire responses appeared as part of the respective patient’s EMR, thus enhancing the quality of care by providing physicians with more comprehensive data and by engaging physicians through a more responsive process.
The smart bedside station system (6) is a personal concierge device on all inpatient beds that provides entertainment services, internet access, and educational content customized to each patient’s diagnosis and treatment. Patients have access to relevant information about their treatment such as their current medication and examination scheduling and objectives. It empowers inpatients by giving them more information and creates a new channel for two-way communication between medical staff and patients.
Conclusions
From our experiences on the use of health IT at SNUBH, one of the success factors for achieving the adoption of health IT is that hospital staff and end-users of the system should be actively involved from the beginning of driving user requirements until the end of testing. It can effectively reflect end-users’ needs and workflow in the system, thus improving user satisfaction and experience.
The future use of health IT will be advanced with state-of-the-art mobile technology and Internet-of-Things (IoT), big data analytics, and cloud computing to provide personalized, preventive, and predictive care to patients.
Acknowledgements
None.
Footnotes
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- 1.Buntin MB, Burke MF, Hoaglin MC, et al. The benefits of health information technology: a review of the recent literature shows predominantly positive results. Health Aff (Millwood) 2011;30:464-71. 10.1377/hlthaff.2011.0178 [DOI] [PubMed] [Google Scholar]
- 2.Lluch M. Healthcare professionals' organisational barriers to health information technologies-a literature review. Int J Med Inform 2011;80:849-62. 10.1016/j.ijmedinf.2011.09.005 [DOI] [PubMed] [Google Scholar]
- 3.Yoo S, Lee KH, Lee HJ, et al. Seoul National University Bundang Hospital's Electronic System for Total Care. Healthc Inform Res 2012;18:145-52. 10.4258/hir.2012.18.2.145 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yoo S, Kim S, Lee KH, et al. Electronically implemented clinical indicators based on a data warehouse in a tertiary hospital: its clinical benefit and effectiveness. Int J Med Inform 2014;83:507-16. 10.1016/j.ijmedinf.2014.04.001 [DOI] [PubMed] [Google Scholar]
- 5.Ro HJ, Jung SY, Lee K, et al. Establishing a Personal Health Record System in an Academic Hospital: One Year's Experience. Korean J Fam Med 2015;36:121-7. 10.4082/kjfm.2015.36.3.121 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Yoo S, Lee KH, Baek H, et al. Development and User Research of a Smart Bedside Station System toward Patient-Centered Healthcare System. J Med Syst 2015;39:86. 10.1007/s10916-015-0273-8 [DOI] [PubMed] [Google Scholar]