Abstract
Lung cancer is the principal cause of cancer-related death worldwide. The use of targeted therapies, especially tyrosine kinase inhibitors (TKIs), in specific groups of patients has dramatically improved the prognosis of this disease, although inevitably some patients will develop resistance to these drugs during active treatment. The most common cancer-associated acquired mutation is the epidermal growth factor receptor (EGFR) Thr790Met (T790M) mutation. During active treatment with targeted therapies, histopathological transformation to small-cell lung carcinoma (SCLC) can occur in 3–15% of patients with non-small-cell lung carcinoma (NSCLC) tumors. By definition, SCLC is a high-grade tumor with specific histological and genetic characteristics. In the majority of cases, a good-quality hematoxylin and eosin (H&E) stain is enough to establish a diagnosis. Immunohistochemistry (IHC) is used to confirm the diagnosis and exclude other neoplasia such as sarcomatoid carcinomas, large-cell carcinoma, basaloid squamous-cell carcinoma, chronic inflammation, malignant melanoma, metastatic carcinoma, sarcoma, and lymphoma. A loss of the tumor-suppressor protein retinoblastoma 1 (RB1) is found in 100% of human SCLC tumors; therefore, it has an essential role in tumorigenesis and tumor development. Other genetic pathways probably involved in the histopathological transformation include neurogenic locus notch homolog (NOTCH) and achaete-scute homolog 1 (ASCL1). Histological transformation to SCLC can be suspected in NSCLC patients who clinically deteriorate during active treatment. Biopsy of any new lesion in this clinical setting is highly recommended to rule out a SCLC transformation. New studies are trying to assess this histological transformation by noninvasive measures such as measuring the concentration of serum neuron-specific enolase.
Keywords: Anaplastic lymphoma kinase (ALK), epidermal growth factor receptor (EGFR), neuroendocrine cells, drug resistance
Introduction
Lung cancer represents the primary cause of cancer mortality worldwide (1). The World Health Organization (WHO) classifies lung cancer into two subtypes: non-small cell lung cancer (NSCLC) and small cell lung cancer (SCLC) (2). NSCLC represents 85% of cases of lung cancer, and is divided into adenocarcinoma, squamous-cell, and large-cell carcinoma (3). SCLC represents 14–15% of all lung cancers, and more than 30,000 new cases are diagnosed each year in the United States (4).The oncogenes involved in lung cancer development have been studied extensively and a great variety of tumor promoter and suppressor genes play important roles in the development of lung cancer (5).
Promoter gene alterations: in NSCLC it is common to observe mutations in KRAS (6), HRAS (7), and NRAS (11p15.5; 1p13) (8). Specifically, lung adenocarcinoma can harbor overexpression of the epidermal growth factor receptor (EGFR) (9), ROS proto-oncogene 1 (10), and rearrangements of the anaplastic lymphoma kinase (ALK) (11). All of these alter autocrine and paracrine cell growth (12). Adenocarcinoma and neuroendocrine large-cell carcinoma, can have amplification and overexpression of c-myc (13), l-myc (14), and n-myc (1p32; 2p2.41) (15). These augment proliferation and inhibit cell differentiation (16). Suppressor gene alterations: neuroendocrine carcinoma and NSCLC can have missense mutation in p53 (17p12-13), which inactivates tumor suppression (17). In SCLC, mutation and deletion in retinoblastoma 1 (RB1) (13q14) can be observed, which produces loss of control of the G1 phase of the cell cycle and the arrest of the cell cycle (18).
Alterations in the methylation pattern of DNA have been recognized in many human cancers, and lung cancer is no exception. Aberrant promoter methylation has been shown in various genes, including the retinoid acid receptor β-2, tissue inhibitor of metalloproteinase-3, p16, O6-methylguanine-DNA-methyltransferase, death-associated protein kinase, E-cadherin, p14, glutathione S-transferase P1, the ras effector homologue RASSF1A, and the protein tyrosine phosphatase receptor type O. The presence of aberrant methylation in precursor lesions of lung carcinomas identifies it as a reasonable candidate biomarker for early lung cancer diagnosis (5).
Advanced clinical stages of NSCLC that harbor mutations in EGFR, ROS-1, or ALK rearrangements have a distinct clinical course compared with conventional NSCLC. The use of modern therapies for lung cancer such as tyrosine kinase inhibitors (TKIs), some of which inhibit EGFR and others ALK, has improved survival in patients with specific genetic anomalies of their tumors (19-21). These treatments are preferred over standard intravenous chemotherapy, not only because of their advantages in terms of outcomes, but also because of the better quality of life that patients report. Other advantages include fewer visits to chemotherapy infusion centers and the convenience of administration (22). However, most patients develop resistance to the treatment after 12–15 months of continuous therapy (23-26). This review is focused on standards not only for analysis of the histopathological structure, but also in the molecular mechanisms that drive the histopathological transformation to SCLC in NSCLC tumors.
Histological and genetic characteristics of lung adenocarcinoma and SCLC
Lung adenocarcinoma is the most prevalent subtype of lung cancer among women, nonsmokers, and young men. It commonly presents with EGFR mutations or ALK translocations, which represent the main objective of current targeted therapies. It is defined as a malignant epithelial neoplasia with glandular differentiation, pneumocyte phenotype, or mucus production. The WHO recognizes many histological subtypes: lepidic, acinar, papillary, micropapillary, and solid (2). In general, the same tumor can have many subtypes and the pathology report must state which one is the most prevalent: this is very important because it can impact the prognosis (27). Immunohistochemistry (IHC) is only recommended in cases in which diagnosis is not made with conventional hematoxylin and eosin (H&E) stain. Typically, the IHC markers used are cytokeratin 7 (CK7) and thyroid transcription factor 1 (TTF-1) (27).
With the development of targeted therapies, molecular testing must be included in the work-up of these tumors. The most common genes targeted by mutations in adenocarcinoma include EGFR, KRAS and BRAF, ALK, ROS1 and RET translocations, MET and FGFR1 amplification. EGFR mutations are observed in 10–15% of European patients, most commonly in nonsmokers and women, but in up to 40% of Asian patients (3,28,29). Commonly, patients with these mutations respond to targeted treatment and these therapies are approved as first-line treatment in these patients (30,31). EGFR activation promotes tumor proliferation and arrests cell apoptosis through stimulation of oncogenic pathways such as MAPK and PIK3/Akt/PTEN/mTOR. Activating mutations of EGFR are localized in exons 18–21, which is the coding region of the intracytoplasmic tyrosine kinase receptor. Ninety percent of these activating mutations are small deletions in exon 19 (deletions of codons 747–750) or point mutations in exon 21 (L858R). Between 5% and 8% are insertions in exon 20 and 2–5% are point mutations of exons 18 and 20. KRAS mutations and MET amplification are associated with a worse prognosis and EGFR mutations with acquired resistance (32,33).
A fusion between echinoderm microtubule-associated protein-like 4 (EML4) and ALK is present in 2–7% of adenocarcinomas and is more commonly observed in nonsmokers. This group of patients benefits from ALK inhibitors (34). The physiological function of ALK is not clearly defined; in adult human tissues it is found in low levels in the small intestine, testicles, and nervous system. Histological subtypes of adenocarcinoma that more commonly harbor ALK rearrangements include the solid—cribriform, papillary, and micropapillary, and the presence of signet cells with abundant intracellular mucin (34-36).
On the other hand, SCLC usually affects men with a mean age of 60 years and 99% of the patients are smokers (37). By definition, it is a high-grade tumor, so it is very aggressive and very common that patients already have mediastinal lymph node metastases at the time of diagnosis. Histologically, it is a malignant epithelial neoplasia composed of small, oval, rounded, and fusiform cells with scarce cytoplasm, irregular borders, fine granular chromatin, and inconspicuous nucleoli. The cells generally have nuclear molding. Necrosis is extensive and the mitosis count is high (19). It was previously known as oat-cell carcinoma, small-cell anaplastic carcinoma, undifferentiated small-cell carcinoma (SCC), intermediate cell type, and mixed small-cell/large-cell carcinoma; however, these terms are no longer recognized (2). By light microscopy, mitotic rates are high, with an average of 80 mitoses per 2-mm2 area (2,38-40). The tumor can show different growth patterns, including nests, rosettes, organoid pattern, tubules, ductules with glandular differentiation, and/or peripheral palisading (2). DNA encrustation on vessel walls, which can be observed as basophilic material (also known as the Azzopardi effect), can also be observed in some necrotic zones (19).
The most recent consensus statement of the WHO in 2015 recognizes only two types of SCLC: pure SCLC and combined SCLC (2). When the tumor is composed exclusively of small cells, it is classified as pure SCLC. However, if in addition to the small cells observed in the tumor, it contains at least 10% of large cells, it is classified as a combined SCLC. In surgical samples, neoplastic cells have better formalin fixation and under the microscope the cells can appear larger (19,38). In addition to combined carcinoma composed of small and large cells, one can have combined SCLC with squamous-cell, spindle-cell, or giant-cell carcinoma or adenocarcinoma. Diagnosis of adenocarcinoma or squamous-cell carcinoma can be made if there is any level of frank disease; unlike combined SCLC, no minimum percentage is required. The frequency of diagnosis of mixed carcinoma depends specifically on the size of the biopsy, the type of specimen, and the pathologist’s experience (1). In a surgically resected case series, Nicholson et al. (38) found combined SCLC in 28% of cases, with 16% combining SCLC with large-cell carcinoma, 9% with adenocarcinoma, and 3% with squamous-cell carcinoma.
Pure SCLC is easily diagnosed in small biopsies (obtained through bronchoscopy) and cytology specimens. The most important technical aspect for accurate diagnosis is a good histological slide and a high-quality H&E stain (Figure 1). In most cases, an H&E stain is enough to establish the diagnosis. IHC is used to confirm the diagnosis and in difficult cases. Staining with pancytokeratins such as AE1/AE3 helps to demonstrate that the tumor is a carcinoma rather than a lymphoid lesion (2,19). The most useful neuroendocrine markers include CD56, chromogranin, and synaptophysin, which are best used as a panel (19,38,41). Up to two-thirds of SCLC will be negative for chromogranin and synaptophysin (19). CD56 will stain 90–100% of cases (Figure 2) (42-44). Nonetheless, neuroendocrine marker staining may be focal or weak and only one or two markers may be positive. In <10% of cases, all neuroendocrine markers may be negative and the diagnosis can still be established by morphology (19).
Figure 1.
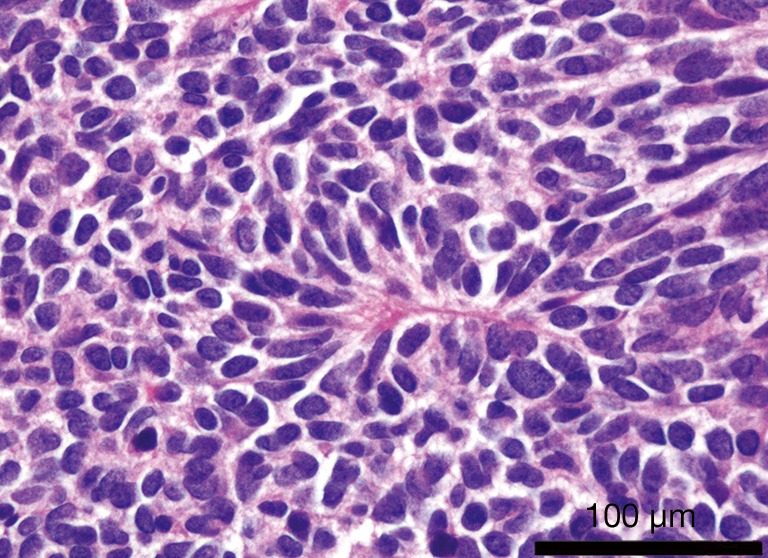
Small cell lung carcinoma. Hematoxylin and eosin (H&E) stain. Tumor composed of nests of small cells with fine granular chromatin nuclei, inconspicuous nucleoli, and scarce cytoplasm.
Figure 2.
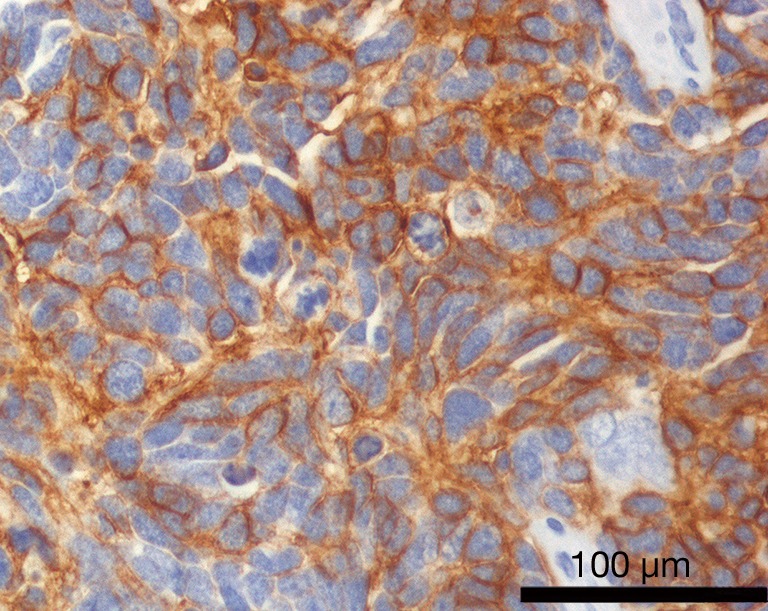
Small cell lung carcinoma. Positive immunohistochemistry (IHC) for CD56, with membranous pattern. This supports the neuroendocrine lineage of the neoplastic cells.
Although a high percentage of SCLC and large-cell neuroendocrine carcinoma (LCNEC) show genetic changes, with some aberrations also seen in carcinoids, some genetic differences between LCNEC and SCLC have been demonstrated (44,45). Therapeutic strategies for SCLC and LCNEC differ substantially. Therefore, because they are two different pathological entities (46), identification of a noninvasive way to detect potential disease transformation before repeated biopsy is crucial.
In addition, an augmented expression of insulin-like growth factor type 1 receptor (IGFR-1) protein and gene copy number has been observed in SCLC, with a significant correlation between protein expression and gene copy number. IGFR-1 inhibitors are beginning to be tested for SCLC in research trials (19,47).
SCLC and LCNEC show a high frequency of loss of heterozygosity (LOH) for 3p, RB, 5q21, 9p, and p53 compared with typical carcinoid and atypical carcinoid (19). LOH of 5q21 was found significantly more frequently in SCLC than in LCNEC, and in high-grade carcinoma than in carcinoid (48). The P16INK4/cyclin D1/RB pathway that is involved in the regulation of G1 arrest in the cell cycle is frequently affected in neuroendocrine tumors (49,50). RB loss is frequent in SCLC and LCNEC, but not in typical carcinoid, although it can be found in 60% of atypical carcinoid. Igarashi et al. demonstrated overexpression of cyclin B1 in a high percentage of LCNEC and SCLC (50).
Positive membranous-cytoplasmic expression of the c-kit protein (also known as CD117) is frequently observed in high-grade pulmonary neuroendocrine tumors. Pelosi et al. reported expression in 44–77% of LCNEC and 67–80% of SCLC (51), but in only 7% of carcinoid tumors. Araki et al. (52) and Casali et al. (53) found c-kit staining in 55% and 61% of SCLC and LCNEC, respectively. Casali et al. reported a significantly worse prognosis and a higher rate of recurrence for patients with c-kit-positive LCNEC (53). In contrast, neither Pelosi et al. (51) nor Araki et al. (52) found any prognostic significance of c-kit expression within LCNEC or SCLC tumors.
Mechanisms of acquired resistance to targeted cancer therapies
This section reviews the molecular characteristics that are secondarily acquired during histopathological transformation. Oral TKI-targeted therapies approved for locally advanced or metastatic EGFR-mutated NSCLC adenocarcinoma have changed substantially the way this aggressive tumor is treated. They are approved as first-line therapies, based on the observation that 90% of active mutations arise from exon 19 deletion and exon 21 L858R point mutation (54,55). Currently, three drugs are available in most countries as first-line therapies: afatinib, gefitinib, and erlotinib (23,24,56). Unfortunately, some patients develop resistance to the therapy after 1 year or less of response to active treatment (57).
Repeated biopsies in this group of patients have been the vehicle to understand the underlying molecular mechanisms of acquired resistance to EGFR TKIs. These include mechanisms that are related to the reactivation of intracellular signal pathways: secondary mutations of EGFR Thr790Met (T790M), MET receptor tyrosine kinase amplification, and PIK3CA mutations (1,58).
These biopsies have also been very useful to observe the phenotypic and histological changes of the so-called histological transformation from NSCLC to SCLC (1,3,59) and epithelial-to-mesenchymal transition (EMT) (60). EMT consists of the loss of the epithelial morphology of the neoplastic cells that develop into a form that resembles that of mesenchymal neoplasms. These phenotypic changes include changes in the IHC-detected expression of vimentin and E-cadherin and also the preservation of the EGFR mutations (1).
The most common acquired resistance mechanism is the T790M mutation of EGFR (1,61), which is reported in 50–60% of biopsies of patients who develop resistance to current targeted therapies. This acquired mutation augments the ATP receptor and allows signaling from the EGFR in the presence of the inhibitor drug (59). Published data from clinical trials focused on this subgroup of patients showed that treatment with a new generation of TKIs resulted in excellent outcomes and drug tolerability (62,63). Other mechanisms that do not involve signaling through the EGFR, such as MET and HER2 amplification, make up 15–20% of acquired resistance to EGFR-targeted therapies (64-66).
Histopathological transformation to SCLC from NSCLC has been reported as a mechanism of acquired resistance to EGFR TKIs in 3–15% of patients (1,3,67). This phenomenon of transformation has been previously reported in case reports and has been confirmed with repeated biopsies in patient cohorts (59,60,68,69). Clinicians must be aware of this possibility in patients receiving targeted therapies who clinically deteriorate. Little is known about the exact mechanisms that lead to this transformation, but two hypotheses have been proposed to explain it. One states that NSCLC and SCLC have a common cell of origin and that the morphological-phenotypic transformation occurs after treatment with TKIs. The other hypothesis proposes that at the time of the original tissue diagnosis, both types of carcinoma were present, but because of the sampling only the adenocarcinoma was diagnosed (54). The scientific evidence suggests that this latter hypothesis is probably wrong and in many cases it is discredited because some patients originally respond to targeted therapies for months or even years (3).
Synchronous development of adenocarcinoma and SCLC has been observed in EGFR-mutated tumors before active targeted therapy (67). This observation suggests that the presence of SCLC in EGFR-mutated carcinomas is not exclusively the result of EGFR inhibition. In addition, in a series of cases of combined carcinoma, the original biopsy of two adenocarcinomas that transformed to SCLC did not show an EGFR mutation. It is improbable that the original EGFR report of the tumors was a false-negative result, because both cases were whole resections and one had a KRAS mutation (67). This suggests that the transformation can occur independently of the EGFR mutational status.
In a 1986 case series, before the discovery of the EGFR-activating mutations, when some patients developed conventional chemotherapy or radiotherapy resistance, around 5% of patients with an original diagnosis of NSCLC presented with recurrences in the form of SCLC (70). It is unknown whether the tumors of these patients had any EGFR-activating mutations, but they showed SCLC transformation independent of EGFR inhibition. Sequist et al. (1) did not find any SCLC transformations among 79 patients with stage III NSCLC using surgical samples of tumors with nonmutated EGFR that were treated with chemotherapy and radiotherapy (1). This suggests that NSCLC with nonmutated EGFR has less tendency to SCLC transformation compared with EGFR-mutated tumors. There is a need for studies of larger cohorts of patients to understand better the histological transformation to SCLC from NSCLC with mutated and nonmutated EGFR.
In addition, the common clinical presentation differs between these two clinical entities. EGFR-mutated adenocarcinomas are more common among nonsmokers and have a more indolent clinical course compared with classical SCLC, which is exclusively a disease of smokers with a rapid growth and early metastases. Clinically, patients with histological transformation to SCLC have an accelerated decline after an initial response to therapy (60).
In many cases that have been studied with repeated biopsies, all the SCLC-transformed tumors retained the initial EGFR mutations of the adenocarcinoma (68,69). An autopsy of a patient with histological transformation of NSCLC into extensive metastatic SCLC disease in the lungs, mediastinal and subdiaphragmatic lymph nodes, and liver demonstrated conservation of the EGFR L858R mutation of the original lung adenocarcinoma without any additional mutation. However, there are reports of rare cases where tumors not only maintain the original mutations, but also acquire additional changes such as mutations in PIK3CA (3,70). These findings suggest that resistance mechanisms involve the phenotypic transformation of the tumor.
Zhang et al. (71) reported the case of an 80-year-old man with lung adenocarcinoma (stage IB) who had an EGFR mutation (deletion of exon 19). Second-line treatment with EGFR-TKI after progression failed, and the progression was accompanied by increased concentrations of the serum tumor marker neuron-specific enolase. The patient’s disease progressed during one month of active TKI therapy. Later, repeated biopsies of the metastatic and primary surgical lesions identified a pathological transformation from adenocarcinoma to SCLC, which retained the same EGFR mutation. Chen et al. (46) suggest that, in the case reported by Zhang et al. (71), the transformation occurred before the initial period of TKI treatment. By contrast, in most cases, patients have a long progression-free survival under TKI treatment, which supports the possibility that the transformation might occur during TKI treatment. These conflicting findings suggest the possible existence of factors other than EGFR inhibition that might promote the transformation from EGFR-mutant adenocarcinoma to SCLC (46). In this case, in addition to the poor response to TKIs, the increased concentration of serum neuron-specific enolase, which rose from 17.9 ng/mL at the early stage of the disease to 211.10 ng/mL at the stage when progression was detected (reference range <15 ng/mL), could be a way to predict potential disease transformation (71).
Genetic analyses of EGFR-mutated adenocarcinomas with acquired resistance to TKIs secondary to histological SCLC transformation showed that these tumors can lose EGFR expression and have low levels of EGFR amplification (60). It is known that SCLC has lower expression of EGFR compared with NSCLC, but the underlying mechanism of this is unknown (68). SCLC with EGFR mutations responds less strongly to TKIs compared with EGFR-mutated NSCLC, probably secondary to mechanisms that suppress EGFR expression in these tumors (3). However, Araki et al. (52) reported the case of a patient with SCLC with mutated EGFR that responded to conventional TKI treatment. This must be confirmed with studies that include more patients. A summary of mechanisms of acquired resistance to EGFR TKIs is listed on Table 1.
Table 1. Demonstrated mechanisms of acquired resistance to EGFR TKIs. The most common is the acquired mutation of EGFR Thr790Met, which has been reported in 50–60% of studied biopsies.
| Secondary mutation of EGFR (T790M) |
| MET receptor tyrosine kinase amplification |
| HER2 amplification |
| PIK3CA mutations |
| Histopathological transformation from NSCLC to SCLC |
| Epithelial to mesenchymal transition |
EGFR, epidermal growth factor receptor; TKI, tyrosine kinase inhibitor; T790M, Thr790Met; NSCLC, non-small cell lung carcinoma; SCLC, small-cell lung carcinoma.
EGFR-mutated carcinomas that transform to SCLC also have epigenetic changes; miRNA analyses have demonstrated that SCLC-transformed cells express miRNAs that are commonly upregulated in classical SCLC. However, SCLC-transformed cells also express miRNA subtypes that are typically expressed in adenocarcinomas, but not in SCLC. This suggests that transformed SCLCs have some characteristics of the original adenocarcinoma, but that the mRNA expression profile and the clinical course indicate that this neoplasia behaves similarly to classical SCLC (60,62,63,72).
In laboratory studies, the BCL-2, BCL-XL inhibitor ABT-263 is one of the few therapies to date to exhibit marked efficacy against SCLC, although recent results from single-agent clinical trials with ABT-263 demonstrated responses in only a minority of SCLC patients. Transformed SCLC EGFR-mutant cells were highly sensitive to single-agent ABT-263, and markedly more sensitive than EGFR-TKI-resistant NSCLC cell lines harboring the T790M resistance mutation. ABT-263 treatment induced a robust apoptotic response in EGFR-mutant SCLC compared with the resistant EGFR-mutant NSCLC. The gene expression and drug sensitivity of the SCLC-transformed cells more closely resemble classical SCLC than EGFR-mutant NSCLC (73).
ALK inhibitors provide a better response than cytotoxic chemotherapy in patients with ALK-positive NSCLC (34,36). Despite these favorable results, a group of patients will have progression of the disease after 1 or 2 years of active treatment. The resistance mechanisms to TKIs for ALK-positive patients include ALK domain modification and upregulation of parallel signaling pathways such as those involving EGFR and cKIT (36,74). To our knowledge, there are only three case reports in the literature describing SCLC transformation in ALK-positive patients. The first detected an EML4-ALK fusion gene through ALK IHC analysis and direct sequencing of cDNA in a surgically resected specimen (75). The second confirmed ALK rearrangement by multiplex reverse transcription-polymerase chain reaction (PCR) in a biopsy before treatment (76). The third case described a 67-year-old nonsmoking woman with a diagnosis of ALK-positive adenocarcinoma that underwent SCLC transformation during active treatment with the ALK inhibitor alectinib (36).
Molecular mechanisms involved in the transformation from NSCLC to SCLC
Two SCLC genome-sequencing projects have been completed, which included analysis of the genome, transcriptome, and the copy number. Both identified a high prevalence of TP53 and RB1 mutations (77,78). MYC amplification was observed in 16% of the studied cases (77). MYCL1 knockdown produces diminished proliferation in cells of SCLC (78), which suggests that MYC can function as an oncogenic controller in a subgroup of SCLC tumors. Signal activators including ERK, EGFR, and KRAS are more common in adenocarcinomas. By contrast, the loss of RB1 is more common in SCLC (79).
Because the loss of RB1 was found in 100% of sequences of SCLC tumors in humans, it was concluded that it plays an important role in tumorigenesis and is essential for its development (3,77,79). Analyses of repeated biopsies of patients with EGFR-mutated adenocarcinomas that underwent SCLC transformation have shown that all the tumors had lost RB1 (60). Evaluation of RB1 status in 11 samples of EGFR-mutated tumors by analysis with IHC, quantitative PCR, next-generation sequencing (NGS), and array comparative genomic hybridization showed that classical SCLC had alterations in RB1 and did not express EGFR (60,77,79-81). However, it is of interest that in RB1 knockdown experiments in EGFR-mutant cell lines, the loss of RB1 was insufficient to cause resistance or induce neuroendocrine differentiation. These cell lines do not possess the pluripotent cells that are present in a tumor in vivo and that have the capacity to differentiate into many cell types including SCLC. It is suggested that pluripotent cells differentiate to NSCLC when EGFR is active, in the same way as EGFR activity is associated with alveolar differentiation (60,82). The SCLC transformation could suggest that adenocarcinoma and SCLC originate from a common cell, probably a multipotent stem cell (3). If this could be confirmed, the genetic heterogeneity of neoplasia would again be demonstrated.
Western blotting revealed loss of RB expression specifically in resistant EGFR-mutant cell lines with SCLC histology also lacking RB expression. The universal nature of RB loss suggests that this may be a necessary event for the resistant SCLC tumors to emerge. RB-deficient adenocarcinomas serve as further evidence that loss of RB alone is insufficient to promote transformation to SCLC (83).
Achaete-scute homolog 1 (ASCL1) is a basic helix-loop-helix transcription factor pivotal for neuroendocrine differentiation that is expressed in pulmonary neuroendocrine cells and in SCLC. ASCL1 promotes more aggressive adenocarcinoma growth in vivo and may interact with the central retinoblastoma protein-tumor protein 53 (RB-p53) axis in the carcinogenesis of neuroendocrine lung cancers. ASCL1 contributes to enhanced proliferation and migration in lung cancer cells in vitro by targeting cyclin-dependent kinase 5 (CDK5). ASCL1 expression is regulated downstream of neurogenic locus notch homolog (NOTCH) signaling, mediated through four different receptors, which causes polyubiquitination-mediated ASCL1 degradation. Alteration in NOTCH receptor signaling is frequently found in malignant neoplasms. The mutated domain determines the functionality, because activating mutations are located in the proline-glutamic acid-serine-threonine-rich (PEST) domain and inactivating mutations in the EGF-like and ankyrin (ANK) repeats. Meder et al. investigated signaling via the NOTCH- and ASCL1-dependent pathway in vitro (83). They used amplicon-based NGS to identify mutations on RB1 and TP53. Mutual RB1 and TP53 mutations were identified only in SCLC cell lines. Thus, RB1 mutations correlated with the lack of RB protein expression. Using different amplicon-based panels, they identified other oncogenic mutations, including EGFR mutations in PC9 and H1975, while RB can be inactivated by phosphorylation. They also performed Western blot analysis to determine the total RB protein and phosphorylation status. ASCL1 clones showed higher expression of serine-phosphorylated RB. Therefore, ASCL1 overexpression caused inactivation of RB by phosphorylation. Phosphorylation of RB is triggered by CDKs. CDK5 was upregulated in ASCL1 clones compared with the EV control. Because ASCL1 is targeted by NOTCH signaling, Meder et al. also performed siRNA-mediated knockdown of NOTCH1 and NOTCH2 in PC9 cells, and observed increased ASCL1 and CD56 expression. Flow cytometry revealed stable RB protein expression and significantly increased phosphorylation of RB at Ser780, but this was not as strong as in ASCL1 clones. Meder et al. proposed that ASCL1 overexpression induced CDK5 upregulation and thereby RB inactivation by phosphorylation, and that p53-mutated cells had a selective advantage when RB was inactivated. ASCL1 assists the central RB-p53 signaling axis in the establishment of a SCC phenotype. Meder’s group examined four mutations in NOTCH genes (NOTCH1-4), RB1, and p53 by NGS and also assessed representative cases of neuroendocrine pulmonary carcinomas. They suggested that mutual biallelic alterations of both genes were a prerequisite for SCC formation. For secondary SCC, biallelic TP53 mutations in the non-small-cell precursor, which are more frequent in squamous cell carcinoma than in adenocarcinoma, may be a prerequisite. ASCL1 expression alone was not sufficient to induce a full SCC phenotype but it was reported that ASCL1 may cooperate with RB and p53 loss when forming SCC. However, clinical observations also suggest that SCCs may arise as secondary neoplasms from a non-small cell cancer background in the form of relapses after genotoxic chemotherapies or targeted therapies (1,84,85). The complex patterns of inactivating NOTCH mutations in the context of mutual RB1 and TP53 alteration in tumors with neuroendocrine differentiation indeed suggest that some neuroendocrine neoplasms may represent a NSCLC-dependent secondary tumor overgrowing its non-small cell origin. The results suggested that one inactivating NOTCH mutation was sufficient to induce neuroendocrine differentiation from nonneuroendocrine tumor cells or tumor precursors (Figure 3). Reactivating NOTCH signaling may represent an important therapy option for SCLC patients (86,87).
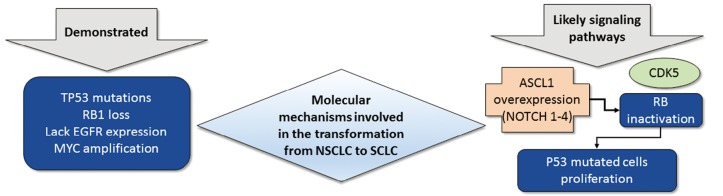
Figure 3.
Molecular mechanisms involved in the transformation from NSCLC to SCLC. They include TP53 mutations, RB1 loss, lack of EGFR expression and MYC amplification. The most studied signaling pathway is the ASCL1 which is regulated by four different NOTCH receptors. NOTCH alterations promote ASCL1 and CD56 overexpression. These changes induce CDK5 activity and inactivation of RB by phosphorylation. With inactivated RB, p53 mutated cells have a selective advantage. NSCLC, non-small cell lung carcinoma; SCLC, small cell lung carcinoma; RB1, retinoblastoma 1; EGFR, epidermal growth factor receptor; NOTCH, neurogenic locus notch homolog; ASCL1, achaete-scute homolog 1; CDK5, cyclin-dependent kinase 5.
We lack clinical trials that address the best way to treat SCLC transformed from NSCLC tumors. Case-reports and series of cases in the literature, used standard chemotherapy (platinum-based and etoposide) and reported a response in 75% of the patients. The benefit of radiotherapy to the chest is unknown in this group of patients (1,69,88).
Conclusions
Clinicians must be aware that transformation to SCLC from NSCLC can occur at any time during active treatment. The specific moment when the transformation occurs has not been elucidated. After EGFR-specific TKI treatment, resistant pluripotent cells can accumulate genetic alterations (such as the loss of RB1 and TP53), which give them a distinct epigenetic state and capability of differentiation in a lineage that does not require EGFR signaling, such as SCLC. The EGFR-specific TKIs silence that signaling pathway, facilitating differentiation to other lineages. This same mechanism could also explain SCLC transformation in patients with ALK-positive NSCLC receiving targeted therapy. Other genetic pathways that are probably involved in the histopathological transformation are NOTCH and ASCL1. A biopsy is recommended for patients with NSCLC and rapid clinical decline to rule out SCLC transformation.
Acknowledgements
The authors would like to thank the guest editors Dr. Niki Karachaliou and Dr. Daniela Morales Espinosa for their invitation to write this review.
Footnotes
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- 1.Sequist LV, Waltman BA, Dias-Santagata D, et al. Genotypic and histological evolution of lung cancers acquiring resistance to EGFR inhibitors. Sci Transl Med 2011;3:75ra26. 10.1126/scitranslmed.3002003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Travis WD, Brambilla E, Burke AP, et al. editors. WHO classification of tumours of the lung, pleura, thymus and heart. World Health Organization classification of tumours. 4th edition. France, Lyon: International Agency for Research on Cancer, 2015. [DOI] [PubMed] [Google Scholar]
- 3.Oser MG, Niederst MJ, Sequist LV, et al. Transformation from non-small-cell lung cancer to small-cell lung cancer: molecular drivers and cells of origin. Lancet Oncol 2015;16:e165-72. 10.1016/S1470-2045(14)71180-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Siegel R, Ward E, Brawley O, et al. Cancer statistics, 2011: the impact of eliminating socioeconomic and racial disparities on premature cancer deaths. CA Cancer J Clin 2011;61:212-36. 10.3322/caac.20121 [DOI] [PubMed] [Google Scholar]
- 5.Weidner N, Cote RJ, Suster S, et al. Modern Surgical Pathology. 2nd ed. United States: Saunders, 2009. [Google Scholar]
- 6.Sunaga N, Shames DS, Girard L, et al. Knockdown of oncogenic KRAS in non-small cell lung cancers suppresses tumor growth and sensitizes tumor cells to targeted therapy. Mol Cancer Ther 2011;10:336-46. 10.1158/1535-7163.MCT-10-0750 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lea IA, Jackson MA, Li X, et al. Genetic pathways and mutation profiles of human cancers: site- and exposure-specific patterns. Carcinogenesis 2007;28:1851-8. 10.1093/carcin/bgm176 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ohashi K, Sequist LV, Arcila ME, et al. Characteristics of lung cancers harboring NRAS mutations. Clin Cancer Res 2013;19:2584-91. 10.1158/1078-0432.CCR-12-3173 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Inamura K, Ninomiya H, Ishikawa Y, et al. Is the epidermal growth factor receptor status in lung cancers reflected in clinicopathologic features? Arch Pathol Lab Med 2010;134:66-72. [DOI] [PubMed] [Google Scholar]
- 10.Gainor JF, Shaw AT. Novel targets in non-small cell lung cancer: ROS1 and RET fusions. Oncologist 2013;18:865-75. 10.1634/theoncologist.2013-0095 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Soda M, Choi YL, Enomoto M, et al. Identification of the transforming EML4-ALK fusion gene in non-small-cell lung cancer. Nature 2007;448:561-6. 10.1038/nature05945 [DOI] [PubMed] [Google Scholar]
- 12.Korpanty GJ, Graham DM, Vincent MD, et al. Biomarkers That Currently Affect Clinical Practice in Lung Cancer: EGFR, ALK, MET, ROS-1, and KRAS. Front Oncol 2014;4:204. 10.3389/fonc.2014.00204 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rapp UR, Korn C, Ceteci F, et al. MYC is a metastasis gene for non-small-cell lung cancer. PLoS One 2009;4:e6029. 10.1371/journal.pone.0006029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Shih CM, Kuo YY, Wang YC, et al. Association of L-myc polymorphism with lung cancer susceptibility and prognosis in relation to age-selected controls and stratified cases. Lung Cancer 2002;36:125-32. 10.1016/S0169-5002(01)00467-6 [DOI] [PubMed] [Google Scholar]
- 15.Bernasconi NL, Wormhoudt TA, Laird-Offringa IA. Post-transcriptional deregulation of myc genes in lung cancer cell lines. Am J Respir Cell Mol Biol 2000;23:560-5. 10.1165/ajrcmb.23.4.4233 [DOI] [PubMed] [Google Scholar]
- 16.Wu DW, Hsu NY, Wang YC, et al. c-Myc suppresses microRNA-29b to promote tumor aggressiveness and poor outcomes in non-small cell lung cancer by targeting FHIT. Oncogene 2015;34:2072-82. 10.1038/onc.2014.152 [DOI] [PubMed] [Google Scholar]
- 17.Gibbons DL, Byers LA, Kurie JM. Smoking, p53 mutation, and lung cancer. Mol Cancer Res 2014;12:3-13. 10.1158/1541-7786.MCR-13-0539 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.George J, Lim JS, Jang SJ, et al. Comprehensive genomic profiles of small cell lung cancer. Nature 2015;524:47-53. 10.1038/nature14664 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Travis WD. Update on small cell carcinoma and its differentiation from squamous cell carcinoma and other non-small cell carcinomas. Mod Pathol 2012;25 Suppl 1:S18-30. 10.1038/modpathol.2011.150 [DOI] [PubMed] [Google Scholar]
- 20.Bogdanowicz BS, Hoch MA, Hartranft ME. Flipped script for gefitinib: A reapproved tyrosine kinase inhibitor for first-line treatment of epidermal growth factor receptor mutation positive metastatic nonsmall cell lung cancer. J Oncol Pharm Pract 2016. [Epub ahead of print]. 10.1177/1078155216634179 [DOI] [PubMed] [Google Scholar]
- 21.Rosell R, Moran T, Queralt C, et al. Screening for epidermal growth factor receptor mutations in lung cancer. N Engl J Med 2009;361:958-67. 10.1056/NEJMoa0904554 [DOI] [PubMed] [Google Scholar]
- 22.Oizumi S, Kobayashi K, Inoue A, et al. Quality of life with gefitinib in patients with EGFR-mutated non-small cell lung cancer: quality of life analysis of North East Japan Study Group 002 Trial. Oncologist 2012;17:863-70. 10.1634/theoncologist.2011-0426 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rosell R, Carcereny E, Gervais R, et al. Erlotinib versus standard chemotherapy as first-line treatment for European patients with advanced EGFR mutation-positive non-small-cell lung cancer (EURTAC): a multicentre, open-label, randomised phase 3 trial. Lancet Oncol 2012;13:239-46. 10.1016/S1470-2045(11)70393-X [DOI] [PubMed] [Google Scholar]
- 24.Sequist LV, Yang JC, Yamamoto N, et al. Phase III study of afatinib or cisplatin plus pemetrexed in patients with metastatic lung adenocarcinoma with EGFR mutations. J Clin Oncol 2013;31:3327-34. 10.1200/JCO.2012.44.2806 [DOI] [PubMed] [Google Scholar]
- 25.Wu YL, Zhou C, Hu CP, et al. Afatinib versus cisplatin plus gemcitabine for first-line treatment of Asian patients with advanced non-small-cell lung cancer harbouring EGFR mutations (LUX-Lung 6): an open-label, randomised phase 3 trial. Lancet Oncol 2014;15:213-22. 10.1016/S1470-2045(13)70604-1 [DOI] [PubMed] [Google Scholar]
- 26.Zhou C, Wu YL, Chen G, et al. Erlotinib versus chemotherapy as first-line treatment for patients with advanced EGFR mutation-positive non-small-cell lung cancer (OPTIMAL, CTONG-0802): a multicentre, open-label, randomised, phase 3 study. Lancet Oncol 2011;12:735-42. 10.1016/S1470-2045(11)70184-X [DOI] [PubMed] [Google Scholar]
- 27.Travis WD, Brambilla E, Nicholson AG, et al. The 2015 World Health Organization Classification of Lung Tumors: Impact of Genetic, Clinical and Radiologic Advances Since the 2004 Classification. J Thorac Oncol 2015;10:1243-60. 10.1097/JTO.0000000000000630 [DOI] [PubMed] [Google Scholar]
- 28.Ohashi K, Maruvka YE, Michor F, et al. Epidermal growth factor receptor tyrosine kinase inhibitor-resistant disease. J Clin Oncol 2013;31:1070-80. 10.1200/JCO.2012.43.3912 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ou SH. Lung cancer in never-smokers. Does smoking history matter in the era of molecular diagnostics and targeted therapy? J Clin Pathol 2013;66:839-46. 10.1136/jclinpath-2012-201296 [DOI] [PubMed] [Google Scholar]
- 30.Paez JG, Janne PA, Lee JC, et al. EGFR mutations in lung cancer: correlation with clinical response to gefitinib therapy. Science 2004;304:1497-500. 10.1126/science.1099314 [DOI] [PubMed] [Google Scholar]
- 31.Tan CS, Gilligan D, Pacey S. Treatment approaches for EGFR-inhibitor-resistant patients with non-small-cell lung cancer. Lancet Oncol 2015;16:e447-59. 10.1016/S1470-2045(15)00246-6 [DOI] [PubMed] [Google Scholar]
- 32.Maus MK, Grimminger PP, Mack PC, et al. KRAS mutations in non-small-cell lung cancer and colorectal cancer: implications for EGFR-targeted therapies. Lung Cancer 2014;83:163-7. 10.1016/j.lungcan.2013.11.010 [DOI] [PubMed] [Google Scholar]
- 33.Menis J, Giaj Levra M, Novello S. MET inhibition in lung cancer. Transl Lung Cancer Res 2013;2:23-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Solomon BJ, Mok T, Kim DW, et al. First-line crizotinib versus chemotherapy in ALK-positive lung cancer. N Engl J Med 2014;371:2167-77. 10.1056/NEJMoa1408440 [DOI] [PubMed] [Google Scholar]
- 35.Shaw AT, Kim D-W, Mehra R, et al. Ceritinib in ALK-rearranged non–small-cell lung cancer. N Engl J Med 2014;370:1189-97. 10.1056/NEJMoa1311107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Fujita S, Masago K, Katakami N, et al. Transformation to SCLC after treatment with the ALK inhibitor alectinib. J Thorac Oncol 2016;11:e67-72. 10.1016/j.jtho.2015.12.105 [DOI] [PubMed] [Google Scholar]
- 37.Fukushima T, Tateishi K, Yamamoto H, et al. Clinical characteristics and outcomes of patients with small cell lung cancer detected by CT screening. Med Oncol 2013;30:623. 10.1007/s12032-013-0623-7 [DOI] [PubMed] [Google Scholar]
- 38.Nicholson SA, Beasley MB, Brambilla E, et al. Small cell lung carcinoma (SCLC): a clinicopathologic study of 100 cases with surgical specimens. Am J Surg Pathol 2002;26:1184-97. 10.1097/00000478-200209000-00009 [DOI] [PubMed] [Google Scholar]
- 39.Travis WD. Advances in neuroendocrine lung tumors. Ann Oncol 2010;21 Suppl 7:vii65-71. 10.1093/annonc/mdq380 [DOI] [PubMed] [Google Scholar]
- 40.Karachaliou N, Pilotto S, Lazzari C, et al. Cellular and molecular biology of small cell lung cancer: an overview. Transl Lung Cancer Res 2016;5:2-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Maleki Z. Diagnostic issues with cytopathologic interpretation of lung neoplasms displaying high-grade basaloid or neuroendocrine morphology. Diagn Cytopathol 2011;39:159-67. [DOI] [PubMed] [Google Scholar]
- 42.Bobos M, Hytiroglou P, Kostopoulos I, et al. Immunohistochemical distinction between merkel cell carcinoma and small cell carcinoma of the lung. Am J Dermatopathol 2006;28:99-104. 10.1097/01.dad.0000183701.67366.c7 [DOI] [PubMed] [Google Scholar]
- 43.Kontogianni K, Nicholson AG, Butcher D, et al. CD56: a useful tool for the diagnosis of small cell lung carcinomas on biopsies with extensive crush artefact. J Clin Pathol 2005;58:978-80. 10.1136/jcp.2004.023044 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Hiroshima K, Iyoda A, Shida T, et al. Distinction of pulmonary large cell neuroendocrine carcinoma from small cell lung carcinoma: a morphological, immunohistochemical, and molecular analysis. Mod Pathol 2006;19:1358-68. 10.1038/modpathol.3800659 [DOI] [PubMed] [Google Scholar]
- 45.Nasgashio R, Sato Y, Matsumoto T, et al. The balance between the expressions of hASH1 and HES1 differs between large cell neuroendocrine carcinoma and small cell carcinoma of the lung. Lung Cancer 2011;74:405-10. 10.1016/j.lungcan.2011.04.012 [DOI] [PubMed] [Google Scholar]
- 46.Chen B, Hu B, Li W, et al. Transformation from NSCLC to SCLC: when did it happen? Lancet Oncol 2015;16:e309. 10.1016/S1470-2045(15)00059-5 [DOI] [PubMed] [Google Scholar]
- 47.Badzio A, Wynes MW, Dziadziuszko R, et al. Increased insulin-like growth factor 1 receptor protein expression and gene copy number in small cell lung cancer. J Thorac Oncol 2010;5:1905-11. 10.1097/JTO.0b013e3181f38f57 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Onuki N, Wistuba II, Travis WD, et al. Genetic changes in the spectrum of neuroendocrine lung tumors. Cancer 1999;85:600-7. [DOI] [PubMed] [Google Scholar]
- 49.Beasley MB, Lantuejoul S, Abbondanzo S, et al. The P16/cyclin D1/Rb pathway in neuroendocrine tumors of the lung. Hum Pathol 2003;34:136-42. 10.1053/hupa.2003.8 [DOI] [PubMed] [Google Scholar]
- 50.Igarashi T, Jiang SX, Kameya T, et al. Divergent cyclin B1 expression and Rb/p16/cyclin D1 pathway aberrations among pulmonary neuroendocrine tumors. Mod Pathol 2004;17:1259-67. 10.1038/modpathol.3800176 [DOI] [PubMed] [Google Scholar]
- 51.Pelosi G, Masullo M, Leon ME, et al. CD117 immunoreactivity in high-grade neuroendocrine tumors of the lung: a comparative study of 39 large-cell neuroendocrine carcinomas and 27 surgically resected small-cell carcinomas. Virchows Arch 2004;445:449-55. 10.1007/s00428-004-1106-1 [DOI] [PubMed] [Google Scholar]
- 52.Araki K, Ishii G, Yokose T, et al. Frequent overexpression of the c-kit protein in large cell neuroendocrine carcinoma of the lung. Lung Cancer 2003;40:173-80. 10.1016/S0169-5002(03)00034-5 [DOI] [PubMed] [Google Scholar]
- 53.Casali C, Stefani A, Rossi G, et al. The prognostic role of c-kit protein expression in resected large cell neuroendocrine carcinoma of the lung. Ann Thorac Surg 2004;77:247-52; discussion 52-3. 10.1016/S0003-4975(03)01294-3 [DOI] [PubMed] [Google Scholar]
- 54.Kim WJ, Kim S, Choi H, et al. Histological transformation from non-small cell to small cell lung carcinoma after treatment with epidermal growth factor receptor-tyrosine kinase inhibitor. Thorac Cancer 2015;6:800-4. 10.1111/1759-7714.12217 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Lee JC, Jang SH, Lee KY, et al. Treatment of non-small cell lung carcinoma after failure of epidermal growth factor receptor tyrosine kinase inhibitor. Cancer Res Treat 2013;45:79-85. 10.4143/crt.2013.45.2.79 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Maemondo M, Inoue A, Kobayashi K, et al. Gefitinib or chemotherapy for non-small-cell lung cancer with mutated EGFR. N Engl J Med 2010;362:2380-8. 10.1056/NEJMoa0909530 [DOI] [PubMed] [Google Scholar]
- 57.Mok TS, Wu Y-L, Thongprasert S, et al. Gefitinib or carboplatin–paclitaxel in pulmonary adenocarcinoma. N Engl J Med 2009;361:947-57. 10.1056/NEJMoa0810699 [DOI] [PubMed] [Google Scholar]
- 58.Majem M, Remon J. Tumor heterogeneity: evolution through space and time in EGFR mutant non small cell lung cancer patients. Transl Lung Cancer Res 2013;2:226-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Yu HA, Arcila ME, Rekhtman N, et al. Analysis of tumor specimens at the time of acquired resistance to EGFR-TKI therapy in 155 patients with EGFR-mutant lung cancers. Clin Cancer Res 2013;19:2240-7. 10.1158/1078-0432.CCR-12-2246 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Niederst MJ, Sequist LV, Poirier JT, et al. RB loss in resistant EGFR mutant lung adenocarcinomas that transform to small-cell lung cancer. Nat Commun 2015;6:6377. 10.1038/ncomms7377 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Hata A, Katakami N, Yoshioka H, et al. Rebiopsy of non-small cell lung cancer patients with acquired resistance to epidermal growth factor receptor-tyrosine kinase inhibitor: Comparison between T790M mutation-positive and mutation-negative populations. Cancer 2013;119:4325-32. 10.1002/cncr.28364 [DOI] [PubMed] [Google Scholar]
- 62.Jänne PA, Yang JC, Kim DW, et al. AZD9291 in EGFR inhibitor-resistant non-small-cell lung cancer. N Engl J Med 2015;372:1689-99. 10.1056/NEJMoa1411817 [DOI] [PubMed] [Google Scholar]
- 63.Sequist LV, Soria JC, Goldman JW, et al. Rociletinib in EGFR-mutated non-small-cell lung cancer. N Engl J Med 2015;372:1700-9. 10.1056/NEJMoa1413654 [DOI] [PubMed] [Google Scholar]
- 64.Tan CS, Cho BC, Soo RA. Next-generation epidermal growth factor receptor tyrosine kinase inhibitors in epidermal growth factor receptor -mutant non-small cell lung cancer. Lung Cancer 2016;93:59-68. 10.1016/j.lungcan.2016.01.003 [DOI] [PubMed] [Google Scholar]
- 65.Tanizaki J, Okamoto I, Okabe T, et al. Activation of HER family signaling as a mechanism of acquired resistance to ALK inhibitors in EML4-ALK-positive non-small cell lung cancer. Clin Cancer Res 2012;18:6219-26. 10.1158/1078-0432.CCR-12-0392 [DOI] [PubMed] [Google Scholar]
- 66.van der Wekken AJ, Saber A, Hiltermann TJ, et al. Resistance mechanisms after tyrosine kinase inhibitors afatinib and crizotinib in non-small cell lung cancer, a review of the literature. Crit Rev Oncol Hematol 2016;100:107-16. 10.1016/j.critrevonc.2016.01.024 [DOI] [PubMed] [Google Scholar]
- 67.Norkowski E, Ghigna MR, Lacroix L, et al. Small-cell carcinoma in the setting of pulmonary adenocarcinoma: new insights in the era of molecular pathology. J Thorac Oncol 2013;8:1265-71. 10.1097/JTO.0b013e3182a407fa [DOI] [PubMed] [Google Scholar]
- 68.Zakowski MF, Ladanyi M, Kris MG. EGFR mutations in small-cell lung cancers in patients who have never smoked. N Engl J Med 2006;355:213-5. 10.1056/NEJMc053610 [DOI] [PubMed] [Google Scholar]
- 69.Morinaga R, Okamoto I, Furuta K, et al. Sequential occurrence of non-small cell and small cell lung cancer with the same EGFR mutation. Lung Cancer 2007;58:411-3. 10.1016/j.lungcan.2007.05.014 [DOI] [PubMed] [Google Scholar]
- 70.Adelstein DJ, Tomashefski JF, Jr, Snow NJ, et al. Mixed small cell and non-small cell lung cancer. Chest 1986;89:699-704. 10.1378/chest.89.5.699 [DOI] [PubMed] [Google Scholar]
- 71.Zhang Y, Li XY, Tang Y, et al. Rapid increase of serum neuron specific enolase level and tachyphylaxis of EGFR-tyrosine kinase inhibitor indicate small cell lung cancer transformation from EGFR positive lung adenocarcinoma? Lung Cancer 2013;81:302-5. 10.1016/j.lungcan.2013.04.005 [DOI] [PubMed] [Google Scholar]
- 72.Niu FY, Wu YL. Novel agents and strategies for overcoming EGFR TKIs resistance. Exp Hematol Oncol 2014;3:2. 10.1186/2162-3619-3-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Faber AC, Farago AF, Costa C, et al. Assessment of ABT-263 activity across a cancer cell line collection leads to a potent combination therapy for small-cell lung cancer. Proc Natl Acad Sci U S A 2015;112:E1288-96. 10.1073/pnas.1411848112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Katayama R, Lovly CM, Shaw AT. Therapeutic targeting of anaplastic lymphoma kinase in lung cancer: a paradigm for precision cancer medicine. Clin Cancer Res 2015;21:2227-35. 10.1158/1078-0432.CCR-14-2791 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Toyokawa G, Taguchi K, Ohba T, et al. First case of combined small-cell lung cancer with adenocarcinoma harboring EML4-ALK fusion and an exon 19 EGFR mutation in each histological component. J Thorac Oncol 2012;7:e39-41. 10.1097/JTO.0b013e3182762bcb [DOI] [PubMed] [Google Scholar]
- 76.Toyokawa G, Takenoyama M, Taguchi K, et al. An extremely rare case of small-cell lung cancer harboring variant 2 of the EML4-ALK fusion gene. Lung Cancer 2013;81:487-90. 10.1016/j.lungcan.2013.05.022 [DOI] [PubMed] [Google Scholar]
- 77.Peifer M, Fernandez-Cuesta L, Sos ML, et al. Integrative genome analyses identify key somatic driver mutations of small-cell lung cancer. Nat Genet 2012;44:1104-10. 10.1038/ng.2396 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Rudin CM, Durinck S, Stawiski EW, et al. Comprehensive genomic analysis identifies SOX2 as a frequently amplified gene in small-cell lung cancer. Nat Genet 2012;44:1111-6. 10.1038/ng.2405 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Meuwissen R, Linn SC, Linnoila RI, et al. Induction of small cell lung cancer by somatic inactivation of both Trp53 and Rb1 in a conditional mouse model. Cancer Cell 2003;4:181-9. 10.1016/S1535-6108(03)00220-4 [DOI] [PubMed] [Google Scholar]
- 80.van Meerbeeck JP, Fennell DA, De Ruysscher DK. Small-cell lung cancer. Lancet 2011;378:1741-55. 10.1016/S0140-6736(11)60165-7 [DOI] [PubMed] [Google Scholar]
- 81.Byers LA, Wang J, Nilsson MB, et al. Proteomic profiling identifies dysregulated pathways in small cell lung cancer and novel therapeutic targets including PARP1. Cancer Discov 2012;2:798-811. 10.1158/2159-8290.CD-12-0112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Miettinen PJ, Berger JE, Meneses J, et al. Epithelial immaturity and multiorgan failure in mice lacking epidermal growth factor receptor. Nature 1995;376:337-41. 10.1038/376337a0 [DOI] [PubMed] [Google Scholar]
- 83.Meder L, Konig K, Ozretic L, et al. NOTCH, ASCL1, p53 and RB alterations define an alternative pathway driving neuroendocrine and small cell lung carcinomas. Int J Cancer 2016;138:927-38. 10.1002/ijc.29835 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.D'Angelo SP, Janjigian YY, Ahye N, et al. Distinct clinical course of EGFR-mutant resected lung cancers: results of testing of 1118 surgical specimens and effects of adjuvant gefitinib and erlotinib. J Thorac Oncol 2012;7:1815-22. 10.1097/JTO.0b013e31826bb7b2 [DOI] [PubMed] [Google Scholar]
- 85.Alam N, Gustafson KS, Ladanyi M, et al. Small-cell carcinoma with an epidermal growth factor receptor mutation in a never-smoker with gefitinib-responsive adenocarcinoma of the lung. Clin Lung Cancer 2010;11:E1-4. 10.3816/CLC.2010.n.046 [DOI] [PubMed] [Google Scholar]
- 86.Hassan WA, Yoshida R, Kudoh S, et al. Notch1 controls cell invasion and metastasis in small cell lung carcinoma cell lines. Lung Cancer 2014;86:304-10. 10.1016/j.lungcan.2014.10.007 [DOI] [PubMed] [Google Scholar]
- 87.Wael H, Yoshida R, Kudoh S, et al. Notch1 signaling controls cell proliferation, apoptosis and differentiation in lung carcinoma. Lung Cancer 2014;85:131-40. 10.1016/j.lungcan.2014.05.001 [DOI] [PubMed] [Google Scholar]
- 88.Watanabe S, Sone T, Matsui T, et al. Transformation to small-cell lung cancer following treatment with EGFR tyrosine kinase inhibitors in a patient with lung adenocarcinoma. Lung Cancer 2013;82:370-2. 10.1016/j.lungcan.2013.06.003 [DOI] [PubMed] [Google Scholar]