Abstract
Health management information systems (HMIS) produce large amounts of data about health service provision and population health, and provide opportunities for data-based decision-making in decentralized health systems. Yet the data are little-used locally. A well-defined approach to district-level decision-making using health data would help better meet the needs of the local population. In this second of four papers on district decision-making for health in low-income settings, our aim was to explore ways in which district administrators and health managers in low- and lower-middle-income countries use health data to make decisions, to describe the decision-making tools they used and identify challenges encountered when using these tools. A systematic literature review, following PRISMA guidelines, was undertaken. Experts were consulted about key sources of information. A search strategy was developed for 14 online databases of peer reviewed and grey literature. The resources were screened independently by two reviewers using pre-defined inclusion criteria. The 14 papers included were assessed for the quality of reported evidence and a descriptive evidence synthesis of the review findings was undertaken. We found 12 examples of tools to assist district-level decision-making, all of which included two key stages—identification of priorities, and development of an action plan to address them. Of those tools with more steps, four included steps to review or monitor the action plan agreed, suggesting the use of HMIS data. In eight papers HMIS data were used for prioritization. Challenges to decision-making processes fell into three main categories: the availability and quality of health and health facility data; human dynamics and financial constraints. Our findings suggest that evidence is available about a limited range of processes that include the use of data for decision-making at district level. Standardization and pre-testing in diverse settings would increase the potential that these tools could be used more widely.
Keywords: Decision-making, evidence-based policy, low-income, health systems, decentralization, health planning
Key Messages
Health management information systems produce large amounts of data, yet little data are used locally in health decision-making.
This systematic literature review explored ways in which district administrators and health managers in low- and lower-middle-income countries used health data to make decisions, to describe the decision-making tools they used and identify challenges encountered when using these tools.
Our findings suggest that evidence is available about a limited range of processes that include the use of data for decision-making at district level.
Introduction
Health management information systems (HMIS) produce data about health service provision and population health status that are intended to be used for decision-making and planning at all levels of the health system, especially in the local area where they have been generated. Examples from research studies to encourage the use of local health data at community level include: a randomized field experiment in Uganda to encourage community monitoring of health services, in which the community used health data to hold their local health workers to account for performance, leading to greater utilization of health services and improved health outcomes (Björkman and Svensson 2009); and a participatory approach to community assessment and planning for maternal and child health programmes in Ethiopia, which resulted in health data and community priorities being used to decide health care activities (Bhattacharyya and Murray 2000). Yet in practice HMIS data are not being used enough at community or district level. One reason for this might be that there is no standardized process for their usage (Harrison and Nutley 2010; Qazi and Ali 2011), or alternatively, data may not be available, maybe incomplete or of poor quality (Braa et al. 2012; Nutley 2012).
When considering information use in organizations, Feldman and March (1981) identified wider impediments to using data rationally for decision-making, which might also be applied to the field of health administration. These are based on users’ perceptions that the data are inadequate or irrelevant, because the data gathers and users are two distinct groups; the data have been collected for a different purpose, e.g. for monitoring rather than decision-making; the data are subject to strategic misrepresentation; or that using data as a symbol of rational decision-making takes on more significance than the outcome of the process.
Yet the formal use of local data can help in setting district health priorities and planning, resource allocation and utilization, managing health workers and introducing new services or improving existing service delivery and quality to better meet the needs of the local population (Smith et al. 1989; Gill and Bailey 2010; Chitama et al. 2011). HMIS provide opportunities for data-based decision-making and are designed for use within decentralized health systems, which are amenable to decision-making at district level (Smith et al. 1989; Kimaro and Sahay 2007; Qazi et al. 2008; Talukder et al. 2008).
The extent to which local public health administrators—those working at district-level, or the equivalent—are able to make health decisions and undertake planning locally is important and is closely linked to strategies for health services administration, such as decentralization (Bossert et al. 2000; Nyamtema 2010). Without some degree of decentralization, local administrators are not able to make meaningful decisions that they can follow through to benefit the community (Bossert and Beauvais 2002).
Much has been written about health systems data collection and ways to improve data quality, e.g. (Braa et al. 2007; Abajebel et al. 2011; Chitama et al. 2011) but what is less well documented is how the data are used. This review explored local decision-making practices in low- and lower-middle-income countries and the types of evidence used to make those decisions. Decision-making in health systems administration is the process by which a group of people reach a collective understanding of a topic, which then helps to build consensus on a particular course of action to address a health service challenge, from two or more possible options. In a rational decision-making process, all the options available are given full and unbiased consideration; relevant data and information are assessed; expertise and experience—either from within the group or from an external source—are drawn upon; the expected result of following each option is assessed; and the option most likely to be successful is chosen (Stone 2012). Ideally, decision-making is based on a full assessment of all the available data that meet accepted quality criteria. This is widely used within the health sector as the standard way in which clinical decisions are made, yet within health systems, data do not always form the basis for managerial or administrative decisions (Pappaioanou et al. 2003; Walshe and Rundall 2001).
From the literature, we sought to identify well-defined ways that data are used locally, through structured processes, tools or guidelines that facilitate the various district level stakeholders to make decisions, and whether any of these processes had been standardized through pretesting and piloting. We consider structured decision-making processes to be those that contain predefined steps, include a consensus building process and incorporate the use of locally generated data.
This is the second paper in a series of four: the first is on the feasibility of establishing a data-informed platform for health to support district data for decision-making in India, Nigeria and Ethiopia (Avan et al. 2016); the third paper presents potential data sources using the World Health Organization’s health-system block framework, showing the huge potential of HMIS data at district level in India and Ethiopia (Bhattacharyya et al. 2016) and the final paper in the series presents prospects for engaging the private sector in health data sharing and collaborative decision-making at district level in India (Gautham et al. 2016).
The objective of this systematic literature review was to look at the ways in which local administrators and managers in the health system—at district level or the equivalent—in low- and lower-middle-income countries, use health data to make decisions. Our aims were to identify and describe the decision-making processes, tools or guidelines used to make decisions that led to changes in local health systems; and understand the key steps within these processes, any common steps in the different processes, and any challenges that affected their implementation.
Methods
The PRISMA 2009 statement and checklist (Moher et al. 2009) were adopted, to ensure this systematic literature review followed a transparent, replicable and iterative process. The date, activities and outcome of each step of the process were recorded in a log of activities. The protocol was published online in the PROSPERO international database of prospectively registered systematic reviews in health and social care, at the Centre for Reviews and Dissemination, University of York, on 3 October 2013; registration number: CRD42013005306 (Center for Reviews Dissemination).
Eligibility criteria
This review comprised qualitative papers and reports, including literature reviews and case studies that described formal decision-making processes used at district level, incorporating the use of health systems data; detailed the steps in an effective process; identified decision-making instruments available and evaluated the effectiveness of a decision-making process. The focus was local health systems administration decision-making, in low- or lower-middle-income countries as classified by the World Bank in 2012 (World Bank 2012). Studies about data collection issues were excluded from this review, as were those that focused on either the process, or the impact of decentralizing of health systems.
Search strategy and information sources
The literature search focused on formal decision-making by local administrators, in low- and lower-middle-income countries, using evidence and information from health systems data (a primary source of which is usually HMIS). While initiated in the public sector, a decision-making process may also involve other stakeholders, including private sector and non-governmental organizations (NGOs) responsible for delivering health services at district level and below.
A comprehensive literature search strategy was developed, incorporating the different elements of the enquiry: decision-making, evidence, district, health systems data and the countries in the inclusion criteria. It included both free text and medical subject headings (MESH terms). It was tested, reviewed and refined; and searches were conducted in 11 electronic databases of peer-reviewed work: EconLit, EMBASE, Global Health, Health Systems Evidence, HMIC (Health Management Information Consortium), LILACS (Health Science Literature from and relevant to Latin America and the Caribbean), MEDLINE, PsychINFO, Scopus, Social Policy and Practice, and Web of Science. MESH terms, or the equivalent, were tailored to individual databases. The search strategy for Medline is available in Supplementary file 1. A search for grey literature was conducted, through semi-structured interviews with experts in this field, to identify possible sources and documents, and a search of grey literature databases: Popline, New York Academy of Medicine Grey Literature Report and Google Scholar.
Selection of studies
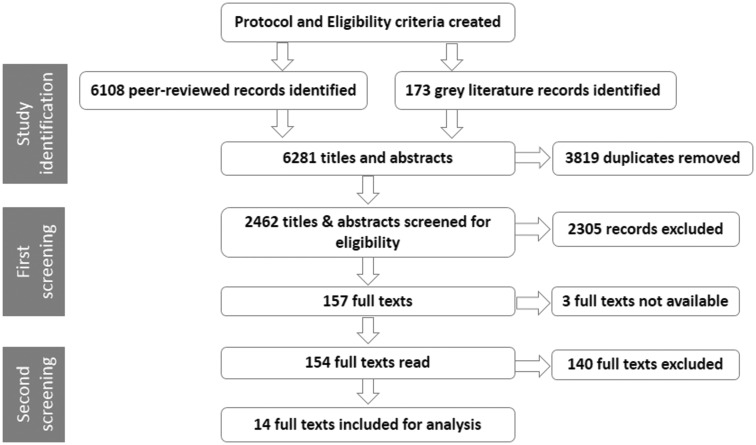
Figure 1 is a flow diagram, showing the number of records at each stage of the systematic review process.
Figure 1.
Flow diagram of the systematic review process.
The literature searches were conducted, records were uploaded to EndNote X7 and duplicates were removed (D.W.).
The titles and abstracts were screened independently by two reviewers (initially D.W. and M.T., then D.W. and I.E.H.) to identify studies that met two criteria: that they related to a low- or lower-middle-income country and focused on the district level. Where either reviewer excluded a record, or was unsure, the reason was recorded in EndNote. They compared their decisions and reached consensus about which records should be included. Full texts were sought for records for definite inclusion and those marked unsure. All but three full texts were found, however each of these records had been marked as unsure during the initial screening. A standardized data extraction form was developed, (see Supplementary file 2) modified from the Health Care Provider Performance data extraction form produced by CDC Foundation (2015), and incorporating the three characteristics of a structured decision-making process—that it consists of a series of steps, includes a consensus process and uses locally generated data. For the second screening, the two reviewers divided the full texts and worked independently, reading them and completing the form for those relevant to the review and noting the reason for excluding studies and those they were unsure about whether to include in this review. Online database software was used to store the information. To ensure a consistent approach between both reviewers, each then read a random selection of 10 papers from the full texts they had not read initially and made an independent decision about whether or not they should be included. The two reviewers then discussed all the studies that either was unsure about including in the review, to check whether they met the eligibility criteria. They reached agreement about whether or not to include all but one paper, for which it was not very clear whether it met the criteria, and this was referred to a third reviewer (B.I.A.) for a final decision. Supplementary file 3 lists the 14 papers included for review, of which three are about the same study.
Assessment of quality of evidence
To assess the quality of the reporting of evidence in the papers for review, a form was adapted from various existing quality assessment forms for qualitative research (National Institute for Health and Care Excellence 2007; Critical Appraisal Skills programme 2010; Tong et al. 2012). This consisted of 15 criteria covering features that might be expected in the abstract and introduction; study design; methodology; results and discussion sections of observational studies. Each question could be answered ‘yes’ or ‘no’. Adapting the Scottish Intercollegiate Guidelines Network (SIGN) levels (Scottish Intercollegiate Guidelines Network 2012), studies meeting over 75% of the quality criteria were considered to be of high quality ( +++), those with between 50% and 75% were considered to be of acceptable quality ( ++) and those with <50% were considered to be of low quality (+).
Results
Overview
Details of the quality assessment for the way each study was reported in the papers included in this review are given in Supplementary file 4; 10 papers were found to report a high quality of evidence, (Sandiford et al. 1994; Heinonen et al. 2000; Mubyazi et al. 2004; Chaulagai et al. 2005; Mutemwa 2006; Soeung et al. 2006; Maluka et al. 2010, 2011a; Nnaji et al. 2010; La Vincente et al. 2013) and four to report an acceptable quality (Murthy 1998; de Savigny et al. 2008; Maluka et al. 2011b; Mutale et al. 2013).
Study characteristics
Table 1 shows the characteristics for the studies in this review including the study location, study design, study participants and the quality assessment level assigned.
Table 1.
Characteristics of studies of a decision-making process for public health
| Article (ID number, author, year) | Location | Study design | Study participants | Study qualitya |
|---|---|---|---|---|
| 1. La Vincente et al. (2013) | Philippines | Case study | Regional health office staff (province and city), covering three Local Government Units | +++ |
| 2. Mutale et al. (2013) | Ghana | Case study | Community health officers, District leaders and managers working in public health | ++ |
| Mozambique | Case study | District and provincial health managers, Facility managers and staff | ||
| 3. Maluka et al. (2011a) | Tanzania | Realist evaluation | Government policy makers | +++ |
| 4. Maluka et al. (2011b) | Tanzania | Case study | Administrators, Health Managers, NGO Staff, members of Council Health Management Team (CHMT), Council Health Services Board, district administrative officials, private health service providers, advocacy organizations, knowledgeable community members | ++ |
| 5. Maluka et al. (2010) | Tanzania | Case study | Administrators, Health Managers, NGO Staff, Members of FBOs, knowledgeable members of the community | +++ |
| 6. Nnaji et al. (2008) | Nigeria | Case study | District Health Board Chief Executive Officer, Local Health Authority secretaries, Members of DHB | +++ |
| 7. de Savigny et al. (2008)b | Tanzania | Case study | District health council management teams | ++ |
| 8. Mutemwa (2006) | Zambia | Case series in 2 district health systems (4 retrospective, 4 concurrent) | District health managers and other members of District Health Management Team or broader district health office | +++ |
| 9. Soeung et al. (2006) | Cambodia | Case study | Health manager, Health centre staff | +++ |
| 10. Chaulagai et al. (2005) | Malawi | Case study | Health Managers, District Health Management Team | +++ |
| 11. Mubyazi et al. (2004) | Tanzania | Case series in 4 districts | District Commissioners, Administrative Secretaries, Medical Officers, Health Secretaries, Treasurers, Hospital Medical Superintendents; Council Executive Directors, Health Officers and Planning Officers; Dispensary and Health centre staff; Village leaders and development committees; Ward Development Committees; Heads of households | +++ |
| 12. Heinonen et al. (2000) | Philippines | Case study | Administrators, Health Managers, General population | +++ |
| 13. Murthy (1998) | India | Case series in 2 districts | NGO programme officers, District Health Officer, District Family Welfare Officer, Primary health centre staff | ++ |
| 14. Sandiford et al. (1994) | Tanzania | Exploratory case study: situation analysis (rapid appraisal & information audit) | Government Policy Makers, Administrators, Health Managers | +++ |
aLevel of overall methodological quality of the study adapted from SIGN levels: +++ high quality; ++ acceptable quality, some flaws in the study design; + low quality, significant flaws in the study design.
bAdditional information found at http://network.idrc.ca/en/ev-56203-201-1-DO_TOPIC.html.
Table 2 shows the characteristics of the health system in each study area to help understand the context in which the decision-making tools were used. Six of the studies took place in countries where decentralization of power in the health system (including budgetary control) was theoretically complete to district level (Sandiford et al. 1994; Mutemwa 2006; de Savigny et al. 2008; Maluka et al. 2010, 2011a). Yet in practice district administrators had limited financial autonomy, affecting their ability to see their decisions through. The rest of the studies took place in countries with limited decentralization and little, or no financial autonomy.
Table 2.
Characteristics of the health systems in the study areas
| Articles (ID number, author, year) | Level of health care | Level of decentralization (for decision-making, authority and power at district level) | Degree of financial autonomy (to set budget and allocate funds accordingly) | Degree of autonomy to move/transfer staff and to allocate non-financial resources |
|---|---|---|---|---|
| 1. La Vincente et al. (2013) | primary and secondary | Limited | limited | not stated |
| 2. Mutale et al. (2013) | Ghana: primary | limited | none | not stated |
| Mozambique: primary | limited | limited | limited | |
| 3. Maluka et al. (2011a) | primary and secondary | full (taking national planning guidelines into account) | limited | full |
| 4. Maluka et al. (2011b) | primary and secondary | full (taking national planning guidelines into account) | limited | full |
| 5. Maluka et al. (2010) | primary and secondary | full (taking national planning guidelines into account) | limited | full |
| 6. Nnaji et al. (2008) | primary and secondary | Limited | limited | full |
| 7. de Savigny et al. (2008) | primary | full | limited | full |
| 8. Mutemwa (2006) | primary and secondary | full | limited | full |
| 9. Soeung et al. (2006) | primary | limited (specifically immunization programme and implementation management) | none | limited |
| 10. Chaulagai et al. (2005) | primary and secondary | limited (in process of gaining autonomy for planning and management of health services) | none | limited |
| 11. Mubyazi et al. (2004) | primary and secondary | limited | limited | limited (some functions still with central government) |
| 12. Heinonen et al. (2000) | primary | limited | limited | full |
| 13. Murthy (1998) | primary and secondary | limited | none | none |
| 14. Sandiford et al. (1994) | primary | full | limited | limited |
Evidence-based decision-making processes with set steps and topics addressed
Thirteen of the papers in this literature review outlined the steps involved in the decision-making process used, with three reporting on the same study (Maluka et al. 2010, 2011a,b) and one describing two separate decision-making processes (Murthy 1998). Table 3 summarizes these 11 decision-making processes and outlines the topics to which they were applied. The studies described the frameworks or tools used for evidence-based decision-making in health systems at district level, addressing a wide range of different topics. Seven of these studies related to priority setting, annual health planning and budgeting (Murthy 1998; Heinonen et al. 2000; Mubyazi et al. 2004; Soeung et al. 2006; Nnaji et al. 2010; Maluka et al. 2010, 2011a,b; La Vincente et al. 2013), with two of them focussed on decision-making specifically related to maternal and child health, (Murthy 1998; La Vincente et al. 2013;) and two based on national agendas (Heinonen et al. 2000; Soeung et al. 2006). Of these latter two, one was about delivery of immunization services, (Soeung et al. 2006) and the other looked at a Minimum Basic Needs (MBN) approach linked to the Government of the Philippines’ national poverty alleviation policy, a broad drive tackling the survival, security and enabling needs of poor people, of which health was just one part (Heinonen et al. 2000). MBN aimed to enhance local government autonomy; increase collaboration and coordination between NGOs, people’s organizations and local government; and encourage community members and relevant sectors to participate in planning and project implementation.
Table 3.
Description of the tool/approach for decision-making (described in 10 studies)a
| Articles (ID number, author, year) | Themes for decisions | Decision-making framework | Generic steps for decision-making | |
|---|---|---|---|---|
| 1. La Vincente et al. (2013) | Priority setting; Budget setting by local government units | Investment Case Approach - structured problem solving to identify and develop strategies to overcome key health system problems. A decision-support model estimates cost and impact, guides strategy selection and prioritization | 1. Critical assessment of available evidence on six parameters related to the performance of health systems | |
| 2. Structured, systematic examination of the key constraints hampering the scaling-up of priority maternal, newborn and child health interventions in disadvantaged populations to identify root cause | ||||
| 3. Identification of feasible strategies to address constraints, and estimate made of the resultant increases in coverage of relevant health services | ||||
| 4. Estimate of the impact and associated costs of different strategies made, using an epidemiological and economic decision-support model | ||||
| 5. Review of estimated impact and cost of the different identified strategies, to guide decision-making for planning and priority setting | ||||
| 2. Mutale et al. (2013) | Priority setting and resource allocation | Ghana: District Health Planning and Reporting Toolkit (DiHPART)b | 1. Priorities identified: through overview of local burden of disease profile and its implications for current plans and activities | |
| 2. Resource allocation: through identification of adaptations to align spending priorities with risk patterns | ||||
| 3. Maluka et al. (2011a) | Priority setting | Accountability for Reasonableness (A4R) Framework; Core principle: that priority setting decisions should be based on evidence, reasons and principles accepted by stakeholders as relevant to meet health needs fairly in their context. Priority setting process evaluated against A4R: Relevance; Publicity; Appeals and revision; Enforcementc | 1. Priorities identified in 6 areas: reproductive and child health; communicable diseases; non-communicable diseases; treatment of common diseases of local priority in districts; community health promotion; strengthening capacity; and organizational structure of health service management; based on local epidemiological data, health service statistics and survey of priorities/needs of hospitals, health centres, dispensaries and the community | |
| 4. Maluka et al. (2011b) | ||||
| 2. Activities for each priority set for the year, based on magnitude, severity, feasibility & cost | ||||
| 5. Maluka et al. (2010) | 3. Rationale developed for each priority selected, based on evidence, reasons and principles accepted as relevant by stakeholders | |||
| 4. Priorities and their rationales made public | ||||
| 5. Appeals/revisions of decisions made, in light of new evidence | ||||
| 6. Review of plans and budget by Council Health Services Board and Full Council, to ensure they meet and address local health priorities | ||||
| 7. Implementation of interventions (in each priority area, based on magnitudes, severity, feasibility and control at low cost) | ||||
| 8. Monitoring and evaluation of health service delivery (Community engagement at each stage) | ||||
| 6. Nnaji et al.(2008) | Annual budget preparation | Unnamed bottom-up approach for preparing budget estimates for resource allocation | 1. Review of how community needs, government policies, expected cost effectiveness and distributional impact are met, through pre-budget seminars of programmes, projects and activities | |
| 2. Use of one or both expenditure classification systems: 1) Functional classification based on programmes, converted into 2) Economic classification (costing) to assist in preparing budget estimates | ||||
| 3. Budget mid-term review | ||||
| 4. Budget end-term review | ||||
| 8. Mutemwa RI, (2006) | 8 decision-making processes: 6 administrative, 2 epidemiological | No name; 3 stage process | 1. Identification of problem (understanding the problem situation and identifying the problem to be targeted) | |
| 2. Investigation (information gathering to understand the root cause of the problem and its impact on the organization or services) | ||||
| 3. Solution development (activities to develop a solution - may be a complex programme or simple list of intervention activities)(not implementation)(Each stage has transitional links but also a distinct set of activities) | ||||
| 9. Soeung et al. (2006) | Improvement in coverage of Immunization through micro-planning | Coverage Improvement Planning (CIP) from which micro plans were developed for health centres and villages with local area populations of ∼10 000 per health centre | 1. Mapping of health centre areas to identify unimmunized children and barriers to improved coverage | |
| 2. Identification of solutions to remove barriers to improved coverage and identify projected costs for reaching coverage goals, in initial workshop for health workers and managers | ||||
| 3. Development of coverage improvement plan in further workshop | ||||
| 4. Development of budget for plan | ||||
| 5. Setting of performance agreements between various government levels | ||||
| 6. Financing and implementation of plan | ||||
| 7. Monitoring of plan | ||||
| 10. Chaulagai et al. (2005) | Devising tool to improve management and use of health information | No specific named tool for decision-making. Brings all stakeholders together in a workshop and all the decisions are made by understanding and agreeing to the fact the a new improved HMIS is needed which then is devised and introduced | 1. Identification of minimum indicators, datasets and a 5 year strategy for strengthening the routine HMIS | |
| 2. Consensus on indicators for inclusion | ||||
| 3. Revision of tools for data collection, processing, reporting and use of information in routine management at local and district level | ||||
| 4. Testing of revised procedures and manuals, for 18 months in phases (starting with 3 health facilities, then entire district and tertiary care facility) | ||||
| 5. Training of District Health Management Team members in 6 months using cascade-training approach | ||||
| 6. System implemented throughout the country from January 2002 | ||||
| 7. Revised curricula of pre-service health training programmes, to include newly devised HMIS tools and procedures | ||||
| 8. Amended job descriptions for health and support staff, to include information management and use, with regular meetings and reporting | ||||
| 9. Development of tools for annual health sector joint review, health information policy, indicator handbook, routine monitoring and guidelines | ||||
| 11. Mubyazi et al. (2004) | Priority setting in primary and secondary health problems for annual district health plans | Ministry of Health/Ministry of Regional Administration and Local Government Council Planning Guidelines for Health Basket Grant. National essential health package, used to identify local health problems | 1. Identification of health problems, by Council Health Management Team for district using guidelines | |
| 2. Development of comprehensive district health plan with District Planning Officer and District Treasurer | ||||
| 3. Endorsement of plan by District Council | ||||
| 4. Review and feedback at regional level | ||||
| 5. Review and approval by Ministry of Health before funding is released | ||||
| 12. Heinonen et al. (2000) | Linked in to central government poverty alleviation policy, that includes: people’s Survival, Security andEnabling needs | Minimum Basic Needs Approach (MBN), to enhance local government autonomy, increase collaboration and coordination between NGOs, community based organizations and local government units, and encourage participation of community members and various sectors in planning and project implementation | 1. Formation of MBN team, by existing inter-agency technical working group convened by local government (MBN includes municipal planners and local representatives from Departments of Health, Agriculture and Social Welfare & Development) | |
| 2. Planning and delivery of training on MBN Approach, to mobilize local health volunteers, community organization leaders and grassroots groups | ||||
| 3. Identification of basic needs not being met, (out of ∼33) from household data collected by trained volunteers | ||||
| 4. Management and analysis of household data by community members with assistance from the MBN Team | ||||
| 5. Findings summarized and presented at a public forum | ||||
| 6. Identification and ranking of unmet needs by degree of importance according to community’s criteria | ||||
| 7. Planning of interventions and activities by community members | ||||
| 13. Murthy (1998) | District health planning and implementation to improve maternal care | No names; different decision-making process in each of two districts | District A: | 1. Formation of district planning team |
| 2. Primary data collection to identify priorities, through household survey based on gap between priority goals and achievement levels in Primary Health Centres (PHCs) | ||||
| 3. Initiation of planning process, by District Family Welfare Officer (DFWO) | ||||
| 4. Review of performance in 15/33 below average PHCs | ||||
| 5. Development of 6-point action plan, by PHC staff | ||||
| 6. Implementation on 2 planning points agreed by DFWO | ||||
| District B: | 1. Formation of state level steering committee and implementing committee | |||
| 2. Suggestions for improving services made by expert group appointed by the government | ||||
| 3. Household survey conducted | ||||
| 4. Review of findings by PHC staff | ||||
| 5. District facility survey conducted | ||||
| 6. Decision on focus for district plan, by Implementation Committee | ||||
| 7. Pilot implementation of actions listed in plan | ||||
| 8. Revision of implementation | ||||
| 9. Actions checked against government guidelines | ||||
| 10. Full implementation of actions listed in plan | ||||
| 11. Monitoring of implementation | ||||
| 12. Selection of new problems for action | ||||
| 14. Sandiford et al. (1994) | Testing hypothesis: that decentralized decision-making, can improve management of health services through; Training, Elaboration and use of procedures, and Development of improved HMIS | Audit by Issue for Health Management (AIHM); it is based closely on the District Action Research and Evaluation process, but differs by employing strict criteria for issue selection and bases decision-making on the information generated through prior analyses of relevant data, derived from routine HMIS or ad hoc inquiries. | 1. A priori appraisal of the scope for management intervention | |
| 2. Audit protocol developed, tested and applied to generate information relevant to the issue | ||||
| 3. Results presented to a meeting of District Health Management Team where decisions are taken and a detailed action plan agreed | ||||
aOne study (7. de Savigny et al. 2008) did not outline the steps in the decision-making process that was used, so has not been included in this table.
bNo framework described for Mozambique, where there is a strategy to improve the quality of HMIS data used for district-level decision-making to improve service delivery.
The other four studies were about decision-making on different topics: one helped district managers with health resource allocation based on the local burden of disease profile (Mutale et al. 2013); one evaluated eight decision-making processes (four historical and four concurrent with the study), of which six were administrative decisions and two were epidemiological; (Mutemwa 2006) and one tested the hypothesis that in decentralized decision-making, health services management can be improved by employing three training approaches—training health systems’ managers; the elaboration and use of procedures for regular planning and evaluation; and the development of improved HMIS to ensure a good evidence base for decision-making (Sandiford et al. 1994). The other study focused on HMIS and the decisions for developing a tool to improve the management and use of health information (Chaulagai et al. 2005).
In all, only five of the studies linked the decision-making process used to a system or service outcome (Sandiford et al. 1994; Murthy 1998; Mubyazi et al. 2004; Chaulagai et al. 2005; Soeung et al. 2006). None of the studies reported any steps that evaluated effectiveness of the decision-making processes they described.
Data sources used and their quality
Table 4 shows the various sources of data used in each study. While HMIS is a widely used source of data, (Sandiford et al. 1994; Murthy 1998; Mubyazi et al. 2004; Chaulagai et al. 2005; Mutemwa 2006; de Savigny et al. 2008; Maluka et al. 2010, 2011a, b; Nnaji et al. 2010; La Vincente et al. 2013; Mutale et al. 2013 (Ghana)) in no case was it the sole source. A few studies highlighted weaknesses in HMIS data (Mubyazi et al. 2004; Nnaji et al. 2010; Maluka et al. 2011a; La Vincente et al. 2013); that they were generally produced for national use and had some limitations in local scope, reliability, validity and timeliness. La Vincente et al. (2013) considered the lack of local data to be ‘…a major impediment to local planning’, particularly in relation to mortality rates and causes, health service coverage parameters and health system costs.
Table 4.
Sources of data used for decision-making
| Article (ID number, author, date) | HMIS data | Facility records | Document reviews | Other sources of dataa |
|---|---|---|---|---|
| 1. La Vincente et al. (2013) | Yes | Limited | Yes | Special surveys and studies |
| 2. Mutale et al. (2013) | Ghana: Yes | Yes | Yes | No |
| Mozambique: No | Yes | No | No | |
| 3. Maluka et al. (2011a) | Yes | Yes | No | Expert opinion (from workshops), National policy requirements, Conducted survey of priorities/needs of hospitals, health centres, dispensaries and community |
| 4. Maluka et al. (2011b) | ||||
| 5. Maluka et al. (2010) | ||||
| 6. Nnaji et al. (2008) | Yes | No | Yes | No |
| 7. de Savigny et al. (2008) | Yes | No | Yes | Demographic Surveillance System |
| 8. Mutemwa (2006) | Yes | No | Yes | Observational, Discussion, Experiential (through supervisory visits and consultative visits), Training |
| 9. Soeung et al. (2006) | No | No | Yes | Data from CIP micro-plan activities; Observational description of introduction of a pilot project |
| 10. Chaulagai et al. (2005) | Yes | Yes | Yes | Findings from an analysis of strengths and weaknesses of the existing information system |
| 11. Mubyazi et al. (2004) | Yes | No | Yes | Studies and information collected by vertical programmes, information through community channels |
| 12. Heinonen et al. (2000) | No | No | No | Conducted household surveys, Focus group discussions, Discussion |
| 13. Murthy (1998) | Yes | Yes | No | Conducted household and facility surveys, Observation at mother and child protection camps |
| 14. Sandiford et al. (1994) | Yes | Yes | Yes | Catchment population estimates |
aBrief description of other data sources, where applicable.
Consensus building mechanisms and their effectiveness
Decision-making processes may be considered successful if they help decision makers reach consensus. Over 80% of the studies described decision-making processes with a built-in consensus mechanism (Sandiford et al. 1994; Murthy 1998 (District B); Heinonen et al. 2000; Mubyazi et al. 2004; Chaulagai et al. 2005; Mutemwa 2006; Soeung et al. 2006; Maluka et al. 2011a; La Vincente et al. 2013; Mutale et al. 2013 (Ghana)), whereas in the rest it was lacking. Consensus decision-making is a way in which common agreement is reached and supported by all members of a group. La Vincente et al. (2013) noted problem solving workshops at which stakeholders had structured discussions to develop strategies to overcome constraints in scaling up maternal, newborn and child health interventions. In Zambia, (Mutemwa 2006) a three-stage decision-making process was described, consisting of problem recognition, investigation and solution development, in which the third stage entailed agreeing a list of recommendations for action. In practice, some consensus mechanisms did not function properly; Maluka et al. (2010) found an imbalance of power among stakeholders with some participants feeling ill-prepared because of insufficient time or access to documentation; others did not have a full awareness of their role and responsibilities (Maluka et al. 2011a); and some felt that decisions were made by the District Medical Officer, without recourse to the agreed decision-making process (Maluka et al. 2011b).
Challenges to decision-making processes
The decision-making processes described above and in Table 3 have not always worked smoothly in practice. This review shows that the challenges fall broadly into three categories; the availability and quality of health and health facility data; human dynamics within a formal, data-based decision-making process; and decisions compromised by financial constraints.
1. Availability, quality and use of health and health facility data
A lack of data available at sub-national level and difficulties in accessing data were reported (La Vincente et al. 2013). Some data were found to be unreliable, not produced in a timely manner to contribute to the decision-making process (Maluka et al. 2010, 2011a; Nnaji et al. 2010). In Tanzania, HMIS data, being centrally defined and geared towards upward reporting, did not allow for the adaptations needed for local planning, moreover data for vertically funded programmes were not always copied to the District Medical Officer (Mubyazi et al. 2004). In Nigeria, data from HMIS, the Human Resources Management and Financial Management Systems were not considered reliable (Nnaji et al. 2010). Although information on the cost of health system inputs was critical for the development of sound plans, La Vincente et al. (2013) found that many costs were not routinely available for Local Government Units to use in planning. In Malawi, when deciding the minimum data set for inclusion in HMIS, reaching consensus was considered a challenge because stakeholders wanted to include all possible indicators for routine collection, including financial, human resources, physical assets and logistical information (Chaulagai et al. 2005).
2. Social and political dynamics in the decision-making process
Some concerns were raised that decisions were not always based on data. In one study the decision-making process was derailed, or ‘corrupted’, e.g. due to political conflict, so that no decision was made and the original problem remained unresolved (Mutemwa 2006). Heinonen et al. (2000) noted that people who had influence in the community could sway decisions, and thus the needs of some groups were not heard. In one district in India, the intention was to prioritize planning on the issue with the greatest gap between health goals and the level of achievement. However, health programme officers ignored local data and made a decision based on national priorities, workers’ previous achievements and those health care facilities responsible for the majority of antenatal service provision (Murthy 1998 (District A)).
In Tanzania, de Savigny et al. (2008) emphasized that tools are necessary but not sufficient, and that capacity strengthening in the form of training to develop management, administration and other skills related to planning and informal mentoring to cultivate a team approach was also needed. Mubyazi et al. (2004) suggested a lack of clarity about the conceptualization and operationalization of multisectoral planning and participation, as well as limited capacity to manage the democratic participatory and multidisciplinary processes involved. Inequity in participatory processes was also an issue. Maluka et al. (2011b) noted that community members raised concerns that their voices were not heard, and mechanisms for disseminating the priorities identified were found to be ineffective (Maluka et al. 2010). Moreover, decision-making processes were seen as dominated by district health professionals on the Council Health Management Team (CHMT), because although the planning guidelines included provision for community and other stakeholder representation, through members of health committees and boards that worked in partnership with the CHMT to provide input for the Comprehensive Council Health Plan, in practice the health committees rarely met (Maluka et al. 2010). In addition, there was no mechanism in place to ensure that the community received the plan and only limited opportunities for them to appeal against a decision, both of which were included in the conditions for the Accountability for Reasonableness priority-setting framework (Maluka et al. 2011a). In Nigeria too, it was noted that neither community nor private sector representatives were fully involved in decision-making processes (Nnaji et al. 2010).
3. Decisions compromised by financial constraints
Local decisions were expected to be made taking account of available funding, but this was not always the case. Four studies noted financial constraints: in Ghana, a lack of flexible funds led to a disconnect between plans and expenditure (Mutale et al. 2013). Maluka et al. (2011b) also found National Planning Guidelines and budget ceilings limited local level planning and financial allocation, and efforts to engage multiple stakeholders in decision-making process were constrained by delays in the disbursement of funds from central government (Maluka et al. 2011a). Heinonen et al. (2000) noted that in the Philippines greater financial autonomy had brought with it an expectation that funds would be raised locally, but that securing finance was both competitive and time-consuming, and with limited overall funding, it was easy to lose motivation over time.
Discussion
We found 12 examples of the implementation of tools to assist a structured process for district level decision-making using local health data, all of which included two key stages—the identification of priorities and the development of an action plan to address them. In eight of these tools HMIS data were used for prioritization. The use of HMIS data at other stages in the process was explicitly stated in one study, which documented three separate cases of HMIS data being used throughout a three-step decision-making process—problem recognition, investigation and solution development—and also gave three cases where HMIS data were used in two of those three steps (Mutemwa 2006). A further four tools identified included a step to review or monitor the action plan agreed, suggesting HMIS data use (Murthy 1998 (District B); Maluka et al. 2010, 2011a; Nnaji et al. 2010; La Vincente et al. 2013).Yet the effectiveness of these formal processes may be limited by various factors, including the poor quality and limited availability of health and health facility data, lack of coordination and capacity among decision makers, and lack of autonomy, (Shaikh et al. 2012) which may restrict how closely local health priorities are reflected in service provision. This suggests that for a standardized tool to function properly it needs to be introduced, alongside formal and/or informal support to strengthen the capacity and skills of district level decision makers, (de Savigny et al. 2008) within a setting where formal, decentralized authority with the financial autonomy to be able to implement decisions, allows them to make and carry through decisions.
Limitations
This literature review included peer-reviewed studies in English and French, and grey literature in English. We focused on identifying examples of data being used for decision-making (rather than for any other use, e.g. service coverage) and on any structured decision-making processes, rather than considering other factors that may influence the process, such as the need to work within budgetary or resource constraints; the political will of group members; the amount of time available to assess all the options to be considered and the leadership style within the group. None of the studies we identified outlined any formative work that had been done to develop and test the decision-making process described.
Limitations of the field mean that much of the knowledge generated by NGO projects and interventions is not widely available on the Internet. Therefore, this literature review can only provide a snapshot of activity that has taken place to encourage data used in district-level decision-making.
Structured decision-making processes
Insights from experts working in the water and energy sectors provide both a definition and an example of a structured decision-making process for a multi-stakeholder group. A structured decision-making process is a set of predefined steps that includes consensus building and incorporates the use of locally generated data, to offer a consistent approach for use in complex situations, through recognizing and understanding the context, and developing and evaluating innovative solutions (Compass Resource Management Ltd. 2013, 2014). To this definition we would add that a structured decision-making process for the health sector would also be replicable within different health systems. Drawing on behavioural decision research, Wilson and Arvai (2011) have developed one such approach, called Structured Decision Making, which was designed to improve stakeholder participation, through a series of facilitated steps for analysing the context, evaluating potential solutions and considering trade-offs between possible solutions. Structured Decision Making was predicated on ways to cope with disagreements and reach an agreement that all the stakeholders can own and will then help to implement.
Sandiford et al. (1994) described the use of a structured process—Audit by Issue for Health Management (AIHM)—in two decision-making exercises in Kisarawe District, Tanzania using health facility and staffing data: one for staff distribution and one for drug kit distribution. AIHM was a three-step process: an a priori appraisal of the scope for management intervention; an audit protocol, tested and applied to generate relevant information and a meeting of the District Health Management Team to discuss and agree an action plan. AIHM was successful in one instance, in that it led to a better distribution of staff at dispensaries in the district, but not in the other instance, due to the team’s limited autonomy, primarily limited financial autonomy, to make decisions about the issue being discussed. Documentation of any subsequent use of AIHM is not available in the public sphere.
Key features of a decision-making process
After reviewing the data, we found three features that kept recurring: that relevant and good quality data are prerequisite; that a structured decision-making process needs to include characteristics that will help to build consensus; and that the community can to have a well-defined role.
Timely, accurate and relevant health data contributes to decisions that will bring about improvements to the functioning of health facilities and the health system (AbouZahr and Boerma 2005). Yet the relevance and quality of HMIS data in low- and lower-middle-income countries are often compromised and accessing data in a timely manner is usually difficult (Braa et al. 2007, 2012). To improve the reliability and comparability of data from different sources HMIS data need to be standardized and harmonized. Useful data relating to the local population and services they use, can be drawn from a range of sectors including health, education, economics and transport, as well as census and national survey data (Stansfield et al. 2006). Close interaction between data producers—those who design, implement and manage information systems—(including, but not limited to those producing data for HMIS) and data users are essential if the data are to be relevant, comprehensible and timely for district-level decision makers, as well as those at national level (Nutley 2012).
In reaching consensus, those involved may take ownership of the decisions made, resulting in greater support for implementation (Wilson and Arvai 2011). The inclusion of a facilitated, structured mechanism to build consensus will help to make the decision-making process smooth and efficient. While documented examples of consensus-based decision-making at district level were limited, there were good examples at community level. In a study from Ethiopia, health staff and community members listed and ranked critical maternal and child health behaviours that caused childhood mortality and morbidity; produced a joint action plan to explore these behaviours and the constraints to adopting healthy ones, and strategies to overcome them both, before undertaking joint data analysis of household surveys. At each stage, community meetings to discuss social mapping, free listing, questionnaire development, matrix ranking, constraints and strategies to overcome them, all involved reaching consensus (Bhattacharyya and Murray 2000). Bhattacharyya and Murray (2000) also describe activities to help with a consensus-based decision-making approach, such as training for facilitators to support the process, and training for participants, ‘…to improve their skills in building rapport, listening, and asking open-ended questions’.
Involving the community in the decision-making process helps to identify local health priorities and encourage uptake and monitoring of health services, enhancing a sense of ownership and improving accountability (Israr and Islam 2006).
To these prerequisites and characteristics we add a recommendation that the decision-making process is standardized to help replicability. Operationally, we define standardization as a well-defined protocol for specifying and implementing a process which is intended to be used repeatedly, in order to achieve operational consistency provided the process is repeated in the same context. The ISO (International Organization for Standardization) sees standardization of processes as creating guidelines that can be used consistently to ensure processes are fit for purpose (ISO website). Its guidelines for developing standards for processes recommend collaboration between stakeholders. While the technical aspects of a standardized decision-making process are likely to be broadly the same across the sub-national level, local socio-political priorities within a district will play a part in the interpretation and application of that process. The interplay of such elements should be acknowledged openly to ensure that the process is transparent and decision makers are accountable to their local population. Transparency and accountability are underlying factors for a standardized decision-making process. None of the studies we found mentions using a standardized process or tool for decision-making (i.e. adopting one grounded in a theoretical framework, and for which stakeholders were engaged in the development process, pretesting and pilot testing) which would offer decision makers some methodological assurance of a reliable process for making decisions.
Challenges to data-based decision-making at district level
It should be possible to overcome the three challenges to formal data-based decision-making for health at district level in low- and lower-middle-income countries that we have identified:
1. Limited health system decentralization
Within a centralized health system district-level decision makers have no autonomy to make and implement decisions to improve local health outcomes. Yet where there has been decentralization, the level of autonomy that the decision makers have over resources depends largely on the type of decentralization that has been introduced and whether it includes financial autonomy to put decisions into practice. In an analysis of decision space, Bossert et al. compared decision-making in decentralized health systems in four countries with four different types of autonomy: deconcentration, devolution, delegation and privatization (Bossert and Beauvais 2002). Of these, devolution, gave district level decision makers in the Philippines a greater degree of autonomy over finances, service organization, human resources and governance, because of their apparent fiscal and administrative capacity. In comparison, when authority was delegated to semi-autonomous agencies in the Ghanaian health system, autonomy over finances, resources and management was compromised. Decentralization through devolution theoretically gives decision makers full financial and administrative autonomy, yet where this has not happened in practice, as is often the case, the benefits are more limited (Somanje et al. 2012).
2. Quality and availability of health data for district-level use
We mentioned above the need for timely, accurate and relevant data for decentralized decision making. Local health data are usually collected for amalgamation into national HMIS from which reports are created largely for central use, but which may also be cascaded back to district level. This process takes time and therefore local utilization of the data at the point of collection is delayed and data may have been superseded in relevance. Moreover, the granularity of the data is lost in national reports, thus compromising the detail required by local users. Harrison and Nutley (2010) suggest that reasons for problems with data accuracy, completeness and quality include complex procedures for reporting data; limited access to computers to record data digitally and the prevalence of inaccuracies made through manual recording; and the limited time available to health facility staff to compile data.
3. Capacity development of decision makers to use data
Alongside the need improve the quality and availability of health data, there is also the challenge of district health officers often having limited capacity to understand and utilize it for decision-making. This could be addressed in part by equipping the stakeholders involved with the knowledge and skills to do so. For example, a recent study in Kenya showed the positive impact on improving and planning health services of a decision support tool for aggregating, analysing and presenting data in a faster and more simplified format (Nutley et al. 2013). The use of a structured process can not only help decision makers make priority decisions, but can also increase the demand for, and the availability and quality of data.
Conclusion
We found a number of examples of decision-making processes that include the use of local HMIS data, yet there was limited evidence about their sustained impact on district level decision-making and whether they have led to changes in resource allocation patterns. Operational research could reveal adaptations needed for a variety of local contexts and if research was undertaken to assess whether their use had brought about revisions in the allocation of resources. In addition, we found no information of steps taken to create and pilot these decision-making processes. Such information would contribute to their standardization. Further research evidence in these areas would help to address the limitations of the current body of evidence.
Supplementary Material
Acknowledgements
We would like to thank Mosisa Tefera for his contribution to the first screening of assessing 500 titles and abstracts for relevance.
Funding
This work was supported by IDEAS—Informed Decisions for Actions to improve maternal and newborn health (http://ideas.lshtm.ac.uk), which is funded through a grant from the Bill and Melinda Gates Foundation to the London School of Hygiene & Tropical Medicine (Gates Global Health Grant Number: OPP1017031).
Conflict of interest statement. None declared.
Supplementary data
Supplementary data are available at Health Policy and Planning online.
References
- Abajebel S, Jira C, Beyene W. 2011. Utilization of health information system at district level in Jimma zone Oromia regional state, South West Ethiopia. Ethiopian Journal of Health Sciences 21: 65–76. [PMC free article] [PubMed] [Google Scholar]
- AbouZahr C, Boerma T. 2005. Health information systems: the foundation of public health. Bulletin of the World Health Organization 83: 578–83. [PMC free article] [PubMed] [Google Scholar]
- Avan BI, Berhanu D, Umar N et al.District decision-making for health in low-income settings: a feasibility study of a data-informed platform for health in India, Nigeria and Ethiopia Health Policy and Planning 201631:ii3–ii11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bhattacharyya K, Murray J. 2000. Community assessment and planning for maternal and child health programs: a participatory approach in Ethiopia. Human Organization 59: 255–66. [Google Scholar]
- Bhattacharyya S, Berhanu D, Taddesse N et al.District decision-making for health in low-income settings: a case study of the potential of public and private sector data in India and Ethiopia Health Policy and Planning 201631:ii25–ii34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Björkman M, Svensson J. 2009. Power to the people: evidence from a randomized field experiment on community-based monitoring in Uganda. Quarterly Journal of Economics 124: 735–69. [Google Scholar]
- Bossert T, Beauvais JC, Bowser D. 2000. Decentralization of Health Systems: Preliminary Review of Four Country Case Studies. Major Applied Research 6, Technical Report No. 1. Bethesda, Maryland: Partnerships for Health Reform Project, Abt Associates Inc.
- Bossert TJ, Beauvais JC. 2002. Decentralization of health systems in Ghana, Zambia, Uganda and the Philippines: a comparative analysis of decision space. Health Policy and Planning 17: 14–31. [DOI] [PubMed] [Google Scholar]
- Braa J, Hanseth O, Heywood A, Mohammed W, Shaw V. 2007. Developing health information systems in developing countries: the flexible standards strategy. MIS Quarterly 31: 1–21. [Google Scholar]
- Braa J, Heywood A, Sahay S. 2012. Improving quality and use of data through data-use workshops: Zanzibar, United Republic of Tanzania. Bulletin of the World Health Organization 90: 379–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- CDC Foundation. 2015Improving health care provider performance in developing countries. 2015accessed 12 January: http://www.cdcfoundation.org/what/program/improving-health-care-provider-performance-developing-countries [Google Scholar]
- Center for Reviews and Dissemination, University of York: PROSPERO: International Prospective Register of Systematic Reviews. http://www.crd.york.ac.uk/prospero/index.asp, accessed 12 January 2015.
- Chaulagai CN, Moyo CM, Koot J. et al. 2005. Design and implementation of a health management information system in Malawi: issues, innovations and results. Health Policy and Planning 20: 375–84. [DOI] [PubMed] [Google Scholar]
- Chitama D, Baltussen R, Ketting E. et al. 2011. From papers to practices: district level priority setting processes and criteria for family planning, maternal, newborn and child health interventions in Tanzania. BMC Womens Health 11: 46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Compass Resource Management Ltd. 2013. Structured decision making: Welcome! http://www.structureddecisionmaking.org/uncategorized/welcome-2/#more-120, accessed 12 January 2015.
- Compass Resource Management Ltd. 2014Structured decision making: SDM brings innovative methods from the decision sciences into the real world. 2015accessed 12 January: http://www.compassrm.com/services/structured_decision_making.php [Google Scholar]
- Critical Skills Appraisal Programme. 2013. 10 questions to help you make sense of qualitative research http://media.wix.com/ugd/dded87_29c5b002d99342f788c6ac670e49f274.pdf, accessed 15 December 2015. [Google Scholar]
- de Savigny D, Kasale H, Mbuya C, Reid G. 2008. Fixing Health Systems. Ottawa: International Development Research Centre. [Google Scholar]
- Feldman MS, March JG. 1981. Information in organizations as signal and symbol. Administrative Science Quarterly 26: 171–86. [Google Scholar]
- Gautham M, Spicer N, Subharwal M et al.District decision-making for health in low-income settings: a qualitative study in Uttar Pradesh, India, on engaging the private health sector in sharing health-related data Health Policy and Planning 201631:ii35–ii46. [DOI] [PMC free article] [PubMed]
- Gill Z, Bailey PE. 2010. Bottom up and top down: a comprehensive approach to improve care and strengthen the health system. JPMA: Journal of the Pakistan Medical Association 60: 927–35. [PubMed] [Google Scholar]
- Harrison T, Nutley T. 2010. A Review of Constraints to Using Data for Decision Making: Recommendations to Inform the Design of Interventions. Chapel Hill, N Carolina: MEASURE Evaluation. [Google Scholar]
- Heinonen T, Mercader M, Quianzon JL, Penera-Torralba M, Baluis L. 2000. Conceptualizing and applying a minimum basic needs approach in southern Philippines. Health Policy and Planning 15: 194–206. [DOI] [PubMed] [Google Scholar]
- International Standards Organization (ISO) Standards. accessed 12 January: 2015. http://www.iso.org/iso/home/standards.htm [Google Scholar]
- Israr SM, Islam A. 2006. Good governance and sustainability: a case study from Pakistan. International Journal of Health Planning Management 21: 313–25. [DOI] [PubMed] [Google Scholar]
- Kimaro HC, Sahay S. 2007. An institutional perspective on the process of decentralization of Health Information Systems: a case study from Tanzania. Information Technology for Development 13: 363–90. [Google Scholar]
- La Vincente S, Aldaba B, Firth S. et al. 2013. Supporting local planning and budgeting for maternal, neonatal and child health in the Philippines. Health Research Policy and Systems 11: 3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maluka S, Kamuzora P, Sebastian MS. et al. 2010. Decentralized health care priority-setting in Tanzania: evaluating against the accountability for reasonableness framework. Social Science & Medicine 71: 751–59. [DOI] [PubMed] [Google Scholar]
- Maluka S, Kamuzora P, Sansebastian M. et al. 2011a. Implementing accountability for reasonableness framework at district level in Tanzania: a realist evaluation. Implementation Science 6: 11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maluka SO, Hurtig AK, Sebastian MS. et al. 2011b. Decentralization and health care prioritization process in Tanzania: from national rhetoric to local reality. The International Journal of Health Planning Management 26: e102–20. [DOI] [PubMed] [Google Scholar]
- Moher D, Liberati A, Tetzlaff J, Altman D, Group TP. 2009. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Medicine 6: e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mubyazi G, Kamugisha M, Mushi A, Blas E. 2004. Implications of decentralization for the control of tropical diseases in Tanzania: a case study of four districts. International Journal of Health Planning Management 19(Suppl 1): S167–85. [DOI] [PubMed] [Google Scholar]
- Murthy N. 1998. Decentralized health planning: lessons from two districts in India. Journal of Health & Population in Developing Countries 1: 1–10. [PubMed] [Google Scholar]
- Mutale W, Chintu N, Amoroso C. et al. 2013. Improving health information systems for decision making across five sub-Saharan African countries: implementation strategies from the African Health Initiative. BMC Health Services Research 13(Suppl 2): S9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mutemwa RI. 2006. HMIS and decision-making in Zambia: re-thinking information solutions for district health management in decentralized health systems. Health Policy and Planning 21: 40–52. [DOI] [PubMed] [Google Scholar]
- National Institute for Health and Care Excellence. 2007. Appendix H: Methodology Checklist: Qualitative Studies. London: NICE. [Google Scholar]
- Nnaji GA, Oguoma C, Nnaji LI, Nwobodo E. 2010. The challenges of budgeting in a newly introduced district health system: a case study. Global Public Health 5: 87–101. [DOI] [PubMed] [Google Scholar]
- Nutley T. 2012. Improving Data Use in Decision Making: an Intervention to Strengthen Health Systems. Chapel Hill, N Carolina: MEASURE Evaluation. [Google Scholar]
- Nutley T, McNabb S, Salentine S. 2013. Impact of a decision-support tool on decision making at the district level in Kenya. Health Research Policy and Systems 11: 8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nyamtema AS. 2010. Bridging the gaps in the Health Management Information System in the context of a changing health sector. BMC Medical Informatics & Decision Making 10: 36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pappaioanou M, Malison M, Wilkins K. et al. 2003. Strengthening capacity in developing countries for evidence-based public health: the data for decision-making project. Social Science & Medicine 57: 1925–37. [DOI] [PubMed] [Google Scholar]
- Qazi MS, Ali M. 2011. Health Management Information System utilization in Pakistan: challenges, pitfalls and the way forward. Bioscience Trends 5: 245–54. [DOI] [PubMed] [Google Scholar]
- Qazi MS, Ali M, Kuroiwa C. 2008. The Health Management Information System of Pakistan under devolution: health managers' perceptions. Bioscience Trends 2: 75–80. [PubMed] [Google Scholar]
- Sandiford P, Kanga GJ, Ahmed AM. 1994. The management of health services in Tanzania: Aa plea for health sector reform. International Journal of Health Planning Management 9: 295–308. [DOI] [PubMed] [Google Scholar]
- Scottish Intercollegiate Guidelines Network. 2012. Notes on Methodology Checklist: Systematic Reviews and Meta-Analyses. Edinburgh: Healthcare Improvement Scotland. [Google Scholar]
- Shaikh S, Naeem I, Nafees A. et al. 2012. Experience of devolution in district health system of Pakistan: perspectives regarding needed reforms. JAMA: Journal of the Pakistan Medical Association 62: 28. [PubMed] [Google Scholar]
- Smith DL, Hansen H, Karim MS. 1989. Management information support for district health systems based on primary health care. Information Technology for Development 4: 779–811. [Google Scholar]
- Soeung SC, Grundy J, Ly CK. et al. 2006. Improving immunization coverage through budgeted microplans and sub-national performance agreements: early experience from Cambodia. Asia Pacific Journal of Public Health 18: 29–38. [DOI] [PubMed] [Google Scholar]
- Somanje H, Barry SP, Dramé B, Mwikisa-Ngenda C. 2012. Health systems strengthening: improving district health service delivery and community ownership and participation. African Health Monitor 15: 48–54. [Google Scholar]
- Stansfield SK, Walsh J, Prata N, Evans T. 2006. Information to Improve Decision Making for Health In: Jamison DT, Breman JG, Measham AR. et al. (eds). Chapter 54 Disease Control Priorities in Developing Countries. 2nd edn Washington, DC: World Bank; http://www.ncbi.nlm.nih.gov/books/NBK11731/, accessed 12 January 2015. [Google Scholar]
- Stone D. 2012. Policy Paradox: The Art of Political Decision Making. 3rd edn New York, London: WW Norton & Company. [Google Scholar]
- Talukder N, Rob U, Mahabub-Ul-Anwar M. 2008. Lessons learned from health sector reform: a four-country comparison. International Quarterly of Community Health Education 28: 153–64. [DOI] [PubMed] [Google Scholar]
- Tong A, Flemming K, McInnes E, Oliver S, Craig J. 2012. Enhancing transparency in reporting the synthesis of qualitative research: ENTREQ. BMC Medical Research Methodology 12: 8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walshe K, Rundall TG. 2001. Evidence-based management: from theory to practice in health care. Milbank Quarterly 79: 429–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson RS, Arvai JL. 2011. Structured Decision Making: Using Decision Research to Improve Stakeholder Participation and Results. Corvallis, OR: Oregon Sea Grant, Oregon State University. [Google Scholar]
- World Bank. 2012. Country and lending groups. http://data.worldbank.org/about/country-classifications/country-and-lending-groups, accessed 13 March 2013.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.