Abstract
Introduction:
While cigarette smoking prevalence is declining among US adults, quit rates may differ between white and African American smokers. Here, we summarize the literature on smoking cessation behaviors in whites and African Americans across four study designs and report the findings of new analyses of International Tobacco Control (ITC) US Survey cohort data.
Methods:
We reviewed 32 publications containing 39 relevant analyses that compared quit attempts and abstinence between US whites and African Americans. Two additional longitudinal analyses were conducted on 821 white and 76 African American cigarette smokers from Waves 7 and 8 of the ITC US Survey (mean follow-up = 19 months).
Results:
Of 17 total analyses of quit attempts, nine (including the ITC US Survey) observed that African American smokers were more likely than whites to attempt to quit during a given year; seven found no differences. Whites were more likely than African Americans to be abstinent in five of six retrospective cohort analyses and in two of five considered community- and population-based cohort studies. Four of these 11 analyses, including one from the ITC US Survey, found no differences.
Conclusions:
Of 11 population- or community-based analyses, all seven that found significant differences indicated that whites were more likely to quit than African Americans. These findings, combined with the similar results from population-based birth cohort analyses, support the conclusion that white smokers are more likely to quit than African American smokers. Efforts to encourage and support quitting among all tobacco users remain a priority.
Implications:
This article provides a review of the literature on smoking cessation among African American and white smokers, and adds new analyses that compare quit attempts and abstinence between US African Americans and whites. Results demonstrate a clear distinction between the findings of cross-sectional and retrospective cohort studies with those of cohort studies. Reasons for these differences merit further study.
Introduction
Cigarette smoking prevalence continues to decrease among adults in the United States (17.8% among adults in 2013), although prevalence has been found to vary by racial and ethnic group affiliation.1 Throughout the 1970s and 1980s, African American adults had a higher smoking prevalence than white adults, but by the early 1990s, these prevalence estimates had converged.2 In 2013, adult smoking prevalence was statistically similar in non-Hispanic whites (19.4%) and non-Hispanic African Americans (18.3%).1
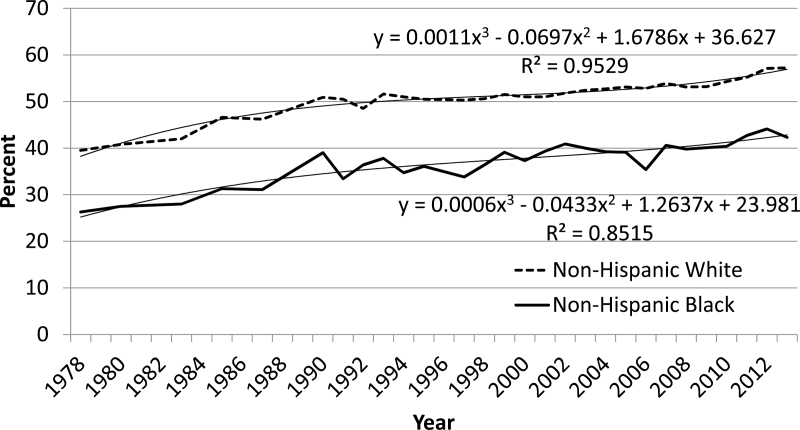
Historical analyses using National Health Interview Survey (NHIS) data have demonstrated that the quit ratio (ie, the percentage of ever-smokers who no longer smoke) is consistently higher among white Americans than among African Americans.3 The quit ratio increased from 1974 to 1985 for both African Americans and whites, with no difference in the rates of change between groups (P = .436).3 The quit ratio has continued to increase similarly among both African American and white ever-smokers (Figure 1).
Figure 1.
Percentage of ever-smokersa who are former smokers (also known as the quit ratio), adults aged ≥ 18 years, by race—United States, 1978–2013. Source: National Health Interview Surveys, 1978–2013; Centers for Disease Control and Prevention: National Center for Health Statistics and Office on Smoking and Health. aEver-smoked >100 cigarettes. Note: Estimates since 1992 incorporate same-day smoking.
The quit ratio, however, is a global indicator that does not provide information on the recency of the quit attempt or the duration of abstinence. In 1993, the Centers for Disease Control and Prevention (CDC) published in the Morbidity and Mortality Weekly Report the results of a retrospective cohort study on smoking cessation. The data indicated that African Americans who were daily smokers in 1990 were more likely than whites to attempt to quit during the subsequent 12 months. Among those who had attempted to quit, African Americans were less likely than whites to report maintaining abstinence for at least 1 month at the time of the survey.4 The findings of this report were frequently cited in peer-reviewed journal articles5–7 and in the popular media.8–10
Other retrospective cohort studies found similar results.11,12 In addition, the report by Holford and his colleagues13 (this issue) demonstrated less quitting and longer duration of smoking among elderly African Americans, which likely contribute to African American versus white disparities in several tobacco-attributable diseases.2 It is possible, however, that the findings about differences in quitting between white and African American smokers vary across study designs. Here, we examine the results reported by publications using four study designs to assess whether the findings observed in several retrospective cohort studies are consistently found in other study designs.
This article has two aims. The first aim is to present a comprehensive literature review on studies assessing whether African Americans and whites differ in quit attempts during the previous 12 months and in maintenance of abstinence, as a function of four study designs: population-based cross-sectional studies, population-based retrospective cohort studies, clinic-based cohort studies, and community/population-based cohort studies. The second aim is to compare smoking cessation rates among African Americans and whites, from new analyses of the International Tobacco Control (ITC) US Survey, a longitudinal cohort study of a nationally representative sample of smokers.
Methods
Literature Review
A systematic search of the literature was conducted through June 2015, seeking articles published in English and reporting on quitting among various races and ethnicities in the United States. Pub Med, Web of Science, and snowball sampling (searches from the references of initially selected articles) were the primary means of publication selection. Search terms included word combinations using the key words quit*, cessation, smoking cessation, tobacco, race, quit rate, African American, black, and/or minority.
Inclusion criteria for the literature review included the type of study design, race/ethnicity of the sample, and country of study origin. There were four study designs reviewed: (1) “population-based cross-sectional studies,” in which participants were queried about their smoking habits at the time of the interview; (2) “population-based retrospective cohort studies,” in which participants reported what their smoking habits were 1 year prior to the interview and subsequent behaviors were assessed; (3) “clinic-based cohort studies” with follow-up of at least 6 months (including “usual care” arms of intervention studies); and (4) “community/population-based cohort studies.” Articles must have reported on quit attempts (all study designs) or abstinence (population-based retrospective cohort studies, clinic-based cohort studies, and community/population-based cohort studies) for African Americans and white Americans; other races or ethnicities may have been reported on as well, but were not inclusion criteria for this effort. Studies that included white race compared with non-white race, or majority race compared with minority race were excluded. While it was noted how the primary authors defined racial categories and cessation, these were not inclusion/exclusion criteria. The numerators and denominators for calculating a “quit attempt” varied among the publications, as did definitions of abstinence and race; definitions are provided in Supplementary Tables 1 and 2 in the Supplementary Material. Studies primarily reporting on data from outside of the United States were excluded. Dates of publication were not restricted.
ITC US Survey Analyses Methods
The ITC Four Country Survey is a prospective cohort study designed to evaluate international tobacco policies at the level of individual smokers, and identify the factors contributing to effective tobacco policies. Further details of the ITC survey methodology have been documented elsewhere.14,15
Study Design and Sample
This analysis uses data from a longitudinal survey of US adult cigarette smokers who were interviewed in Wave 7 (2008–2009) and Wave 8 (2010–2011) of the ITC US Survey. On average, participants completed the Wave 8 interview 18.9 months (SD = 2.2; range = 12 to 25) after completing Wave 7. Eight hundred twenty-one non-Hispanic white and 76 non-Hispanic African American cigarette smokers at Wave 7 responded to both telephone interviews and were included in the analysis. Survey participants included adult smokers (aged 18 and older) who reported that they had smoked at least 100 cigarettes in their lifetime and had smoked at least one cigarette in the 30 days preceding the Wave 7 interview. The response rate was 29.7% for Wave 7; 74.2% of respondents were interviewed at Wave 8.
Measures
Outcomes of interest include quit attempts, abstinence from cigarettes for at least 1 month at Wave 8, and any period of abstinence from cigarettes lasting at least 30 days since Wave 7. Quit attempt information was obtained by asking respondents in Wave 8 whether or not they had made any attempts to stop smoking since the previous interview. Smoking abstinence of at least 1 month at Wave 8 was determined by assessing the current smoking status of respondents who were smoking at Wave 7. Respondents reporting abstinence from cigarettes for at least 1 month at Wave 8 were coded as currently being abstinent. Longest reported smoking abstinence since Wave 7 was assessed by several questions that determined the longest period of time they refrained from smoking since the last survey. Those reporting periods of at least 30 days were categorized as positive, while those reporting less than 30 days or no quit attempts were categorized as negative. The race variable was coded as “non-Hispanic white” or “non-Hispanic black.”
Data and Statistical Analysis
Logistic regression analyses using survey weighting were used to estimate associations between race and attempts to quit smoking and smoking abstinence variables (30+ day abstinence at follow-up among those who attempted to quit during the study period, 30+ day abstinence at any time during the study period for all previous wave smokers, and 30+ day abstinence at follow-up for all previous wave smokers). We present data for a (1) crude model, (2) a model that adjusted for demographic variables, and (3) a model that adjusted for demographic variables, menthol, and Heaviness of Smoking Index16 score (at Wave 7). All models, including the crude model, were additionally adjusted for time-in-sample, since this has been shown to affect each of the outcomes. Demographic variables used in adjustments included age (at recruitment as: 18–24, 25–39, 40–54, or ≥55 years), sex (male/female), income (low, moderate, or high), and education (low, moderate, or high). Menthol status was ascertained from the cigarette label information at Wave 7. All analyses were performed using SAS 9.3.
Results
Literature Review Results
Population-Based Cross-Sectional Studies
Of the publications on population-based cross-sectional studies, 11 were reviewed and met the inclusion criteria. Tables for these publications are presented in the Supplementary Material.
Quit Attempts During the Previous 12 Months
Of the 11 publications reporting on quit attempts during the previous 12 months, 12 separate analyses were conducted (two in one of the publications17). Five reported that African Americans were significantly more likely than whites to have made a quit attempt.18–22 Five other analyses reported nonsignificant differences between white and African American smokers in past-year quit attempts,23–27 as did an analysis of nondaily smokers.17 That publication17 also reported that among daily smokers, whites were more likely than African Americans to have tried to quit for at least 1 day during the previous year.
Population-Based Retrospective Cohort Studies
Four publications reporting the results from population-based retrospective cohort studies met the inclusion criteria for this review.
Quit Attempts During the Previous 12 Months
As shown in Table 1, all three of the publications using population-based retrospective cohort designs to report on quit attempts demonstrated that African American smokers were more likely than white smokers to have made a quit attempt during the previous 12 months.4,11,12
Table 1.
Key Characteristics and Findings of Reviewed Studies Reporting on Quit Attempts
| Study | Data source | Sample size | Findings |
|---|---|---|---|
| Population-based retrospective cohort studies | |||
| CDC4 | 1991 NHIS; ages ≥ 18 years; 1-year follow-up | Total n = 43 732 | White: AOR = 1.0 (referent) |
| Black: AOR = 1.6 (1.3–1.8) | |||
| USDHHS12 | 1995/1996 TUS-CPS; ages ≥ 25 years; 1-year follow-up | White: 27 991 | White: 22.6% ± 0.6 |
| Black: 2681 | Black: 26.7% ± 1.7 | ||
| Levy et al.11 | 2003 and 2006–2007 TUS-CPS; ages > 18 years; 4 years follow-up | Not reported | White: AOR = 1.0 (referent) |
| Black: AOR = 1.35 (1.35–1.35)a | |||
| Community/population-based cohort study | |||
| Rafful et al.28 | NESARC; ages > 18 years; 3 years follow-up | White: 1070 | White: 39.72% (referent) |
| Black: 375 | Black: 45.33% (AOR = 1.10; 0.80–1.51) | ||
AOR = adjusted odds ratio; CDC = Centers for Disease Control and Prevention; NESARC = National Epidemiologic Survey on Alcohol and Related Conditions; NHIS = National Health Interview Study; TUS-CPS = Tobacco Use Supplement to the Current Population Survey; USDHHS = United States Department of Health and Human Services. Bolded indicates significance of P < .05 or nonoverlapping 95% confidence intervals. Exact definition of race is provided once, in the “race definitions” column in Supplementary Table 1; columns here use only “white” or “black.”
aFurther models (adding cigarettes per day and adding smoking < 30 minutes of waking to the original model) continued to maintain significance.
Abstinence
The four publications reporting on smoking cessation in Supplementary Table 3 provided data on six analyses.2,4,11,12 One found no difference4; the remainder found that white Americans were more likely to have been abstinent than African Americans.2,4,11,12
Clinic-Based Cohort Studies
Ten publications on cohort studies based in clinic settings met inclusion criteria and were included in this review. Two other studies that met inclusion criteria45,46 were not included, as relevant data were not reported directly in each paper.
Quit Attempts During the Cohort Study
None of the clinical-based cohort studies presented data on quit attempts during the study period.
Abstinence
Ten publications29–38 reported on ten relevant analyses. As shown in Supplementary Table 3, three33,36,38 of the 10 analyses indicated white smokers were significantly more likely than African American smokers to be abstinent. Two of these were biochemically validated.33,36 Six analyses,29–32,34,35 four29–32 of which were biochemically verified, reported no significant differences in smoking cessation between white and African American smokers. One analysis,37 among smokers utilizing the Veterans Health Administration, found African American smokers were significantly more likely than white smokers to remain abstinent. One clinic-based cohort analysis34 included both cigarettes and other tobacco products in the definition of abstinence and did not find a difference in abstinence between African American and white smokers. Smith and his colleagues36 calculated model-based estimates of the probability of abstinence in their cohort study, and found that 17% of female African American menthol smokers were abstinent at follow-up compared with 35% of female white menthol smokers. There was no difference in quitting between African American and white male menthol smokers.
Community/Population-Based Cohort Studies
A total of seven publications met inclusion criteria as community/population-based cohort studies. One other study that met inclusion criteria47 was not included, as relevant data were not reported directly in the paper.
Quit Attempts
The single community/population-based cohort study reported that 45.3% of African American and 39.7% of white smokers28 made a quit attempt, which was a nonsignificant difference (Table 1).
Abstinence
Six39–44 publications reported on seven relevant analyses on cessation. Five found no significant difference in cessation between African American and white smokers (Supplementary Table 3).40–44 Two of these publications reported on follow-ups from the COMMIT study, one of 5 years40 and the other of 13 years.42 Two publications reported that whites were more likely than African Americans to be abstinent at follow-up.39,44 One analysis42 included both cigarettes and other tobacco products in the definition of abstinence and reported no difference between African American and white smokers.
Results of ITC Analyses
Among cigarette smokers at Wave 7, non-Hispanic African Americans were more likely than non-Hispanic whites to report having made a quit attempt during the study period in the crude analysis, in the analysis that adjusted for demographics, and in the analysis that controlled for demographics, menthol, and Heaviness of Smoking Index (Table 2). There were no differences between whites and African Americans for any of the three abstinence variables examined across the three logistic regression models.
Table 2.
Crude and Adjusted Logistic Regression Models of Race as a Predictor of Making a Quit Attempt, Abstinencea at Follow-Up Among Attempters, Abstinence for At Least 30 Days During Study Period, and Overall Abstinence at Follow-Up—Between Waves 7 and 8 of the International Tobacco Control Policy Evaluation Project, US Survey
| Crude analyses | Analyses adjusted for demographics | Analyses adjusted for demographics, menthol, and HSI | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| N | % | OR | 95% CI | N | AOR | 95% CI | N | AOR | 95% CI | |
| Made a quit attempt | ||||||||||
| Non-Hispanic white | 821 | 44.6 | 1.0 | 1.0 | 821 | 1.0 | Referent | 691 | 1.0 | Referent |
| Non-Hispanic black | 76 | 55.4 | 1.5 | 1.02–2.34 | 75 | 1.8 | 1.19–2.82 | 57 | 1.9 | 1.10–3.39 |
| 30± day abstinence at follow-up among attempters | ||||||||||
| Non-Hispanic white | 334 | 13.3 | 1.0 | 1.0 | 334 | 1.0 | Referent | 298 | 1.0 | Referent |
| Non-Hispanic black | 40 | 14.7 | 1.1 | 0.49–2.58 | 40 | 1.8 | 0.74–4.58 | 33 | 2.2 | 0.68–7.09 |
| 30± day abstinence anytime during the study period among all baseline cigarette smokers | ||||||||||
| Non-Hispanic white | 815 | 21.4 | 1.0 | 1.0 | 815 | 1.0 | Referent | 713 | 1.0 | Referent |
| Non-Hispanic black | 71 | 24.0 | 1.2 | 0.58–2.34 | 70 | 1.4 | 0.66–2.88 | 57 | 1.4 | 0.59–3.30 |
| 30± day abstinence at follow-up among all baseline cigarette smokers | ||||||||||
| Non-Hispanic white | 815 | 8.3 | 1.0 | Referent | 815 | 1.0 | Referent | 713 | 1.0 | Referent |
| Non-Hispanic black | 71 | 8.2 | 1.0 | 0.32–3.12 | 70 | 1.4 | 0.43–4.46 | 57 | 1.8 | 0.44–5.79 |
AOR = adjusted odds ratio; CI = confidence interval; HSI = Heaviness of Smoking Index; OR = odds ratio. All logistic regression analyses adjusted for time in sample. Demographics include age, sex, household income and education. Bolded text indicates significance of P < .05.
aAbstinence = abstinence from cigarettes.
Conclusions
The objectives of this study were to evaluate and summarize the literature on race as a predictor of smoking cessation, and to add to this literature with an analysis of ITC US Survey cohort data. As shown in Figure 1 and previously by Fiore and his colleagues,3 the percentage of ever-smokers who have quit has consistently been higher among whites than African Americans, a finding that is supported from studies in individual years.2,17,18,22,26,48–53 One study,51 and an analysis presented in Table 34 of Chapter 2 of the 1998 Report of the Surgeon General,2 indicate that the differences by race persist even after statistical adjustment was made for variables such as age, gender, and indicators of socioeconomic status (SES).
Burns and his colleagues presented birth cohort analyses of whites and African Americans born during the 20th century that help explain these disparities.54 Among white males, the percentage of former smokers began to rise during the 1950’s and 1960’s and increased dramatically in the late 1960’s. Among white women, quitting in the 1950’s was less prominent than quitting among white males, and while it increased substantially by the late 1960’s, the peak was not as high as for white males. For African American males and females, the prevalence of former smokers remained very low until the late 1960’s, when quitting increased substantially, but not as high as for whites.54 Burns et al. observed that smoking behavior among white males coincided with the initial wave of public information on the dangers of smoking that first appeared during the mid-1950’s.54,55 Since these initial studies were on white men, the absence of data on African American men and women may have resulted in media coverage that did not stimulate quitting among African Americans as it did among white males.55 During 1967–1970, when the Fairness Doctrine antismoking messages appeared on television and radio, cessation increased for all four groups but especially for white males and females. The data in Figure 1 and many of the population-based cross-sectional studies2,17,18,22,26,48–53 likely reflect, at least in part, the “head start” that white males and females had in terms of quitting smoking. Among all four groups, cessation rates increased during the 1970’s and 1980’s,54 which is consistent with the increasing slopes for both whites and African Americans that are seen in Figure 1.
In our survey of the relevant literature, we reviewed 32 publications, containing 39 relevant analyses that were published between 1986 and 2015 and we added two relevant ITC analyses, one on quit attempts and another on abstinence. Of 17 total analyses on quit attempts, which were conducted mainly in population-based cross-sectional studies and population-based retrospective cohort studies, nine observed that African American smokers were more likely than white smokers to try to quit during a given year and seven found no differences in quit attempts between white and African American smokers. It seems plausible that a nontrivial percentage of some-day smokers will confuse days on which they didn’t smoke with quit attempts when queried as part of a major survey. Since African American smokers are more likely than white smokers to smoke on some days,2,56,57 then misclassification of nonsmoking days with quit attempts could be more frequent among African American smokers, compared with whites. Cognitive testing of questions used in the surveys to specifically probe for this possible phenomenon, as well as other methodological studies of different question formats, are warranted.
Twenty-four separate analyses of abstinence were observed. We included observations from six population-based retrospective cohort analyses, 10 clinical cohort analyses and eight community/population-based cohort analyses (including the ITC US Survey). Five of the six analyses from population-based retrospective cohorts found that white Americans were more likely to have been abstinent than African Americans. Of the 10 clinical cohort analyses, six found no differences between white and African American smokers in abstinence at follow-up and three found that whites were more likely than African Americans to be abstinent at follow-up. One publication found African American smokers were significantly more likely than white smokers to remain abstinent.37 The authors hypothesized this was due to the high numbers of participants of both races receiving smoking cessation services at the Veterans Health Administration.37
An important question is why the population-based retrospective cohort studies appear to provide different results than the clinical cohort studies. Clinical cohort participants differ from the general population in that they, even those in the usual care arm, receive regular contact with clinical staff29 or primary care providers,38 are at higher risk of morbidity,29 or are currently receiving provider care.30,31,33 Clinical cohort participants may have been derived from people recently filling a prescription for nicotine replacement therapy,35 and in some instances, “modified” usual care was provided, so the nonintervention participants received smoking cessation manuals and resources,33 newsletters and self-help materials,34 or counseling sessions.36 Inclusion criteria, such as a minimum number of cigarettes per day, limited age ranges, and the requirement for no current mental health diagnosis likely made the clinical cohort studies less representative of the population. For these reasons, the clinical cohort design does not provide the optimal mechanism for assessing patterns in the population. However, clinic based studies do inform efforts to reduce disparities, as indicated by studies that provide support during the cessation process.37,58
Overall abstinence rates (not just abstinence among attempters) varied considerably among the community/population-based cohort analyses. These studies use abstinence prevalence as their measures of quitting. With such measures, the probability of being abstinent increases over time, because people in cohorts continue to try to quit over time. The differences in length of follow-up become important. Not surprisingly, the studies with the longest periods of follow-up (ie, Hymowitz et al.40; Hyland et al.42; Caraballo et al.44) have the highest abstinence rates. Abstinence in the paper by Messer and her colleagues is much lower and is similar to that in our ITC analyses. Both have relatively short periods of follow-up.
We reviewed five analyses from community-based cohort studies: three from CARDIA41,44 and two from COMMIT.40,42 For parsimony, we consider the two analyses of quitting with the longest durations of follow-up: Hyland et al’s 13-year follow-up of the COMMIT cohort, which found no racial difference, and Caraballo et al’s 25-year follow-up of CARDIA, which found that whites (54.0%) were more likely to quit than African Americans (33.2%). Regarding the population-based cohort studies, the McWhorter et al.39 study found that whites were more likely to quit and Messer et al.43 and our ITC analyses reported no differences. Thus, one community-based analysis and one population-based analysis found that whites were more likely to quit than African Americans, with three analyses showing no differences. Based on this, the consistency of the population-based retrospective cohort studies and the work of Holford, Levy and Maza13 (this issue) and Burns et al.,54,55 which report on population-based data across birth cohorts, use large sample sizes, and demonstrate trends over time, we are of the opinion that white smokers in the United States are more likely to quit smoking than African American smokers.
Multiple factors could contribute to lower probabilities of cessation among African American smokers. At the individual level, African Americans are less likely than whites to have health insurance,59 which is associated with higher rates of cessation.27 African Americans are less likely to use a pharmaceutical aid for quitting smoking during a quit attempt.17,19 Smoking cessation pharmacotherapy is required to be provided by most private health insurance plans, per the Affordable Care Act, and this will likely offset the costs associated with pharmacotherapy.27
Factors associated with lower SES, which is more common among African Americans than whites, may impede efforts to quit.17,60 One publication reviewed here that controlled only for SES found that SES explained the racial disparities in abstinence.41 Among publications that have controlled for SES along with other variables, some found no differences in abstinence among blacks and whites29,31,32,34,40,42,44 and others continued to find significant differences in abstinence.2,4,11,39 Living in physically and socially impoverished environments enhance drug effects, likely making quitting more difficult.60 Urban African Americans often live in food deserts.61 Limited access to nutritious foods might undermine quitting.62 Stressful events, other than traumatic, are more commonly experienced by African Americans than whites.63 These findings highlight the need for further research addressing the interaction between race and SES.
African Americans are more likely than whites to smoke mentholated brands.22,49,53,64 In cross-sectional studies, African Americans who smoked menthol cigarettes exhibited the lowest rates of abstinence compared with African Americans who smoked nonmentholated cigarettes, whites who smoked menthol brands, and whites who smoked nonmentholated brands.22,49,64 However, other publications, not meeting the inclusion criteria for this review, found no differences in abstinence between white and African American smokers, even after controlling for menthol in the models.65,66 In another study, African Americans who smoked mentholated brands were more likely than African Americans who smoked nonmentholated brands to intend to quit and have confidence in their ability to quit.53 It is possible that the biological effects of menthol cigarettes counteract these psychosocial phenomena.67,68 For example, lower SES smokers might use mentholated cigarettes “to facilitate increased nicotine intake from fewer cigarettes where economic pressure restricts the number of cigarettes smokers can afford to purchase.”69 It is also possible that efforts to quit are undermined by erroneous beliefs that menthol cigarettes are less dangerous than nonmentholated brands.70–72
At the environmental level, African American smokers are less likely than white smokers to have total bans on smoking in their homes.17 Low-SES urban African American women report finding quitting difficult because cigarettes help them cope with their highly stressful environments.73 Those African Americans living in higher stress neighborhoods, and those living in less socially cohesive neighborhoods, are more likely to smoke.74,75 Some evidence suggests that retail marketing of cigarettes is higher in African American neighborhoods.76 Marketing of menthol cigarettes and little cigars and cigarillos are clearly higher in African American neighborhoods.76
This study is not without limitations. For example, it is difficult to make comparisons among studies, even among those of the same study design, as many methodological differences exist in the published literature. The definitions of “quit attempt” and “abstinence” varied greatly, and in some cases the definition of abstinence included cigarettes and other tobacco products.34,42 The definition of “current smoker” varied considerably as well, with definitions ranging from those who took at least one puff of one cigarette within the past week30 to those smoking at least five cigarettes per week, for most days of the week, for at least 3 months.41,44 Racial and ethnic category definitions were not consistent: in some cases the racial categories of African American and white were inclusive of Hispanic ethnicity, while in other instances they were not.
While a significant attempt was made to use comprehensive search strategies, it is possible that relevant studies were missed. Other limitations include those inherent in the primary studies, such as the use of self-reported information. While the ITC analysis presented here uses nationally representative cohort data, it is limited by a low response rate, and some of these analyses used small samples sizes (n < 40) and therefore may not have had enough power to detect differences between groups.
Further research using rigorous study designs with adequate power, and perhaps over-sampling racial and ethnic minorities, will be valuable. In addition, further exploration of the potential roles of SES, health insurance access, menthol, multiple tobacco product use, and nicotine addiction should be included in future models. Analyses of data from the Population Assessment of Tobacco and Health study,77 would ideally assess interactions between menthol and race, taking into account the factors cited above.
Efforts to motivate quit attempts and maintain and support abstinence among all segments of the US population of smokers, using evidence-based tobacco control programs and policies, should increase. At the individual level, the provision of support to African Americans from treatment providers, and provisions of health insurance, health care, and social support may assist in addressing disparities in smoking-attributable diseases. Messaging that dispels the belief that menthol products are safer (as they are easier to inhale) may aid in supporting quit attempts and the maintenance of cessation. Addressing psychosocial determinants that reduce the likelihood of quitting or remaining quit, such as perceived stress, depressive symptoms, and perceived discrimination, are essential. Some research has been done citing the importance and efficacy of developing skills to manage and reduce stress among African American smokers, such as through the use of cognitive behavioral therapy.58 The provision of more intensive pharmacotherapy for those of lower SES may also be warranted.78
At the policy level, the increase in smokefree multiunit housing regulations79 may help reduce African American smoking rates, as African Americans are less likely than white smokers to have smoke-free homes. Raising taxes could help,80 especially if a fair proportion of the income generated were used to support quitting. Perceptions of discrimination have been associated with higher odds of smoking,81 and addressing broader, societal-level issues such as discrimination, poverty, and inequity may aid in reducing disparities in cigarette smoking prevalence and smoking morbidity and mortality.
Supplementary Material
Supplementary Material and Tables 1–3 can be found online at http://www.ntr.oxfordjournals.org
Funding
The ITC US Project was supported by grants from the US National Cancer Institute at the National Institutes of Health (R01 CA100362, R01 CA125116, P01 CA138389, R25 CA113951); the Roswell Park Transdisciplinary Tobacco Use Research Center (P50 CA111236); Robert Wood Johnson Foundation (045734); Canadian Institutes for Health Research (57897, 79551, and 115016). Additional support was provided to GTF from a Senior Investigator Award from the Ontario Institute for Cancer Research and a Prevention Scientist Award from the Canadian Cancer Society Research Institute. GG received a small contract from the CDC’s Office on Smoking and Health (through Carter Consulting) to work on this project.
Declaration of Interests
None declared.
Disclaimer
The findings and conclusions are the author’s, not necessarily the CDC’s.
Supplement Sponsorship
This article appears as part of the supplement “Critical Examination of Factors Related to the Smoking Trajectory among African American Youth and Young Adults,” sponsored by the Centers for Disease Control and Prevention contract no. 200-2014-M-58879.
Supplementary Material
References
- 1. Jamal A, Agaku IT, O’Connor E, King BA, Kenemer JB, Neff L. Current cigarette smoking among adults--United States, 2005–2013. MMWR Morb Mortal Wkly Rep. 2014;63(47):1108–1112. www.cdc.gov/mmwr/preview/mmwrhtml/mm6347a4.htm Accessed August 3, 2015. [PMC free article] [PubMed] [Google Scholar]
- 2. U.S. Department of Health and Human Services. Tobacco Use Among U.S. Racial/Ethnic Minority Groups--African Americans, American Indians and Alaska Natives, Asian Americans and Pacific Islanders, Hispanics. A Report of the Surgeon General. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 1998. www.google.com/url?sa=t&rct=j&q=&esrc=s&source=web&cd=1&cad=rja&uact=8&ved=0CB4QFjAAahUKEwjM7vGL0_bHAhXCND4KHcdRAqU&url=http%3A%2F%2Fwww.cdc.gov%2Ftobacco%2Fdata_statistics%2Fsgr%2F1998%2Fcomplete_report%2Fpdfs%2Fcomplete_report.pdf&usg=AFQjCNExEz9GD8dG0QQvRVzeoaqJUIHdTg&bvm=bv.102537793,d.cWw Accessed August 3, 2015. [Google Scholar]
- 3. Fiore MC, Novotny TE, Pierce JP, Hatziandreu EJ, Patel KM, Davis RM. Trends in cigarette smoking in the United States. The changing influence of gender and race. JAMA. 1989;261(1):49–55. [PubMed] [Google Scholar]
- 4. Centers for Disease Control and Prevention. Smoking cessation during previous year among adults--United States, 1990 and 1991. MMWR Morb Mortal Wkly Rep. 1993;42(26):504–507. www.cdc.gov/mmwr//preview/mmwrhtml/00021062.htm Accessed August 3, 2015. [PubMed] [Google Scholar]
- 5. Businelle MS, Kendzor DE, Costello TJ, et al. Light versus heavy smoking among African American men and women. Addict Behav. 2009;34(2):197–203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Collins BN, Lepore SJ. Association between anxiety and smoking in a sample of urban black men. J Immigr Minor Health. 2009;11(1):29–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. McGrady GA, Ahluwalia JS, Pederson LL. Smoking initiation and cessation in African Americans attending an inner-city walk-in clinic. Am J Prev Med. 1998;14(2):130–137. www.sciencedirect.com/science/article/pii/S0749379797000251 Accessed August 3, 2015. [DOI] [PubMed] [Google Scholar]
- 8. Quitline NC. African American Communities and Tobacco www.quitlinenc.com/docs/patient-fact-sheets/african-american-communities-fact-sheet.pdf?sfvrsn=4 Accessed November 3, 2014.
- 9. Randall VR. Race, Health Care and the Law: Speaking Truth to Power! Being a Black Smoker 2008. http://academic.udayton.edu/health/01status/smoking/tobacco7.htm#N_88_. Accessed November 3, 2014.
- 10. Way to Quit. African Americans & Smoking Cessation 2014. http://waytoquit.org/uploads/files/AfricanAmerican_Tobacco.pdf Accessed November 3, 2014.
- 11. Levy DT, Blackman K, Tauras J, et al. Quit attempts and quit rates among menthol and nonmenthol smokers in the United States. Am J Public Health. 2011;101(7):1241–1247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. U.S. Department of Health and Human Services. Population Based Smoking Cessation: Proceedings of a Conference on What Works to Influence Cessation in the General Population. Bethesda, MD: U.S. Department of Health and Human Services, Public Health Service, National Institutes of Health, National Cancer Institute; 2000. http://cancercontrol.cancer.gov/Brp/tcrb/monographs/12/index.html Accessed September 14, 2015. [Google Scholar]
- 13. Holford TR, Levy DT, Meza R. Smoking history patterns among African American birth cohorts, 1965–2012. Nicotine Tob Res. 2016;18(S1):S16-S29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Fong GT, Cummings KM, Borland R, et al. The conceptual framework of the International Tobacco Control (ITC) Policy Evaluation Project. Tob Control. 2006;15(suppl 3):iii3–11. doi:10.1136/tc.2005.015438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Thompson ME, Fong GT, Hammond D, et al. Methods of the International Tobacco Control (ITC) Four Country Survey. Tob Control. 2006;15(suppl 3):iii12–18. doi:10.1136/tc.2005.013870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Heatherton TF, Kozlowski LT, Frecker RC, Rickert W, Robinson J. Measuring the heaviness of smoking: using self-reported time to the first cigarette of the day and number of cigarettes smoked per day. Br J Addict. 1989;84(7):791–799. http://eds.b.ebscohost.com/ehost/detail/detail?sid=2b9497c3-8f62-421e-8ff2-5afbdac56a29%40sessionmgr113&crlhashurl=login.aspx%253fdirect%253dtrue%2526scope%253dsite%2526db%253dmnh%2526AN%253d2758152%2526msid%253d-419430176&hid=111&vid=0&bdata=JnNpdGU9ZWhvc3QtbGl2ZSZzY29wZT1zaXRl#AN=2758152&db=mnh Accessed August 3, 2015. [DOI] [PubMed] [Google Scholar]
- 17. Trinidad DR, Pérez-Stable EJ, White MM, Emery SL, Messer K. A nationwide analysis of US racial/ethnic disparities in smoking behaviors, smoking cessation, and cessation-related factors. Am J Public Health. 2011;101(4):699–706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Malarcher A, Dube S, Shaw L, Babb S, Kaufmann R. Quitting smoking among adults--United States, 2001–2010. MMWR Morb Mortal Wkly Rep. 2011;60(44):1513–1519. www.cdc.gov/mmwr/preview/mmwrhtml/mm6044a2.htm Accessed August 3, 2015. [PubMed] [Google Scholar]
- 19. Cokkinides VE, Halpern MT, Barbeau EM, Ward E, Thun MJ. Racial and ethnic disparities in smoking-cessation interventions: analysis of the 2005 National Health Interview Survey. Am J Prev Med. 2008;34(5):404–412. doi:10.1016/j.MWPEW.2008.02.003. [DOI] [PubMed] [Google Scholar]
- 20. Davila EP, Zhao W, Byrne M, et al. Correlates of smoking quit attempts: Florida Tobacco Callback Survey, 2007. Tob Induc Dis. 2009;5(1):10. doi:10.1186/1617-9625-5-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Messer K, Trinidad DR, Al-Delaimy WK, Pierce JP. Smoking cessation rates in the United States: a comparison of young adult and older smokers. Am J Public Health. 2008;98(2):317–322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Stahre M, Okuyemi KS, Joseph AM, Fu SS. Racial/ethnic differences in menthol cigarette smoking, population quit ratios and utilization of evidence-based tobacco cessation treatments. Addiction. 2010;105(suppl 1):75–83. [DOI] [PubMed] [Google Scholar]
- 23. Fagan P, Augustson E, Backinger CL, et al. Quit attempts and intention to quit cigarette smoking among young adults in the United States. Am J Public Health. 2007;97(8):1412–1420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Hatziandreu EJ, Pierce JP, Lefkopoulou M, et al. Quitting smoking in the United States in 1986. J Natl Cancer Inst. 1990;82(17):1402–1406. http://jnci.oxfordjournals.org/content/82/17/1402.long Accessed August 3, 2015. [DOI] [PubMed] [Google Scholar]
- 25. Kahende JW, Malarcher AM, Teplinskaya A, Asman KJ. Quit attempt correlates among smokers by race/ethnicity. Int J Environ Res Public Health. 2011;8(10):3871–3888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Trosclair A, Husten C, Pederson L, Dhillon I. Cigarette smoking among adults--United States, 2000. MMWR Morb Mortal Wkly Rep. 2002;51(29):642–645. www.cdc.gov/mmwr/preview/mmwrhtml/mm5129a3.htm Accessed August 3, 2015. [PubMed] [Google Scholar]
- 27. Yong LC, Luckhaupt SE, Li J, Calvert GM. Quit interest, quit attempt and recent cigarette smoking cessation in the US working population, 2010. Occup Environ Med. 2014;71(6):405–414. doi:10.1136/oemed-2013–101852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Rafful C, García-Rodríguez O, Wang S, Secades-Villa R, Martínez-Ortega JM, Blanco C. Predictors of quit attempts and successful quit attempts in a nationally representative sample of smokers. Addict Behav. 2013;38(4):1920–1923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Hymowitz N, Sexton M, Ockene J, Grandits G. Baseline factors associated with smoking cessation and relapse. MRFIT Research Group. Prev Med. 1991;20(5):590–601. [DOI] [PubMed] [Google Scholar]
- 30. Windsor RA, Lowe JB, Perkins LL, et al. Health education for pregnant smokers: its behavioral impact and cost benefit. Am J Public Health. 1993;83(2):201–206. www.ncbi.nlm.nih.gov/pmc/articles/PMC1694576/ Accessed August 3, 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Kendrick JS, Zahniser SC, Miller N, et al. Integrating smoking cessation into routine public prenatal care: the Smoking Cessation in Pregnancy project. Am J Public Health. 1995;85(2):217–222. www.ncbi.nlm.nih.gov/pmc/articles/PMC1615299/ Accessed August 3, 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Murray RP, Connett JE, Buist AS, Gerald LB, Eichenhorn MS. Experience of black participants in the Lung Health Study smoking cessation intervention program. Nicotine Tob Res. 2001;3(4):375–382. [DOI] [PubMed] [Google Scholar]
- 33. Lando H, Hennrikus D, McCarty M, Vessey J. Predictors of quitting in hospitalized smokers. Nicotine Tob Res. 2003;5(2):215–222. [DOI] [PubMed] [Google Scholar]
- 34. Daza P, Cofta-Woerpel L, Mazas C, et al. Racial and ethnic differences in predictors of smoking cessation. Subst Use Misuse. 2006;41(3):317–339. [DOI] [PubMed] [Google Scholar]
- 35. Fu SS, Burgess DJ, Hatsukami DK, et al. Race and nicotine replacement treatment outcomes among low-income smokers. Am J Prev Med. 2008;35(suppl 6):S442–S448. [DOI] [PubMed] [Google Scholar]
- 36. Smith SS, Fiore MC, Baker TB. Smoking cessation in smokers who smoke menthol and non-menthol cigarettes. Addiction. 2014;109(12):2107–2117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Burgess DJ, van Ryn M, Noorbaloochi S, et al. Smoking cessation among African American and white smokers in the Veterans Affairs health care system. Am J Public Health. 2014;104(suppl 4):S580–587. doi:10.2105/AJPH.2014.302023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Stevens VJ Solberg LI Bailey SR, . et al Assessing trends in tobacco cessation in diverse patient populations [published online ahead of print April 28, 2015]. Nicotine Tob Res. 2015. doi:10.1093/ntr/ntv092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. McWhorter WP, Boyd GM, Mattson ME. Predictors of quitting smoking: the NHANES I followup experience. J Clin Epidemiol. 1990;43(12):1399–1405. [DOI] [PubMed] [Google Scholar]
- 40. Hymowitz N, Cummings KM, Hyland A, Lynn WR, Pechacek TF, Hartwell TD. Predictors of smoking cessation in a cohort of adult smokers followed for five years. Tob Control. 1997;6(suppl 2):S57–62. www.ncbi.nlm.nih.gov/pmc/articles/PMC1766209/ Accessed August 3, 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Kiefe CI, Williams OD, Lewis CE, Allison JJ, Sekar P, Wagenknecht LE. Ten-year changes in smoking among young adults: are racial differences explained by socioeconomic factors in the CARDIA study? Am J Public Health. 2001;91(2):213–218. www.ncbi.nlm.nih.gov/pmc/articles/PMC1446547/ Accessed August 3, 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Hyland A, Li Q, Bauer JE, Giovino GA, Steger C, Cummings KM. Predictors of cessation in a cohort of current and former smokers followed over 13 years. Nicotine Tob Res. 2004;6(suppl 3):S363–369. http://ntr.oxfordjournals.org/content/6/Suppl_3/S363.long Accessed August 3, 2015. [DOI] [PubMed] [Google Scholar]
- 43. Messer K, Mills AL, White MM, Pierce JP. The effect of smoke-free homes on smoking behavior in the U.S. Am J Prev Med. 2008;35(3):210–216. [DOI] [PubMed] [Google Scholar]
- 44. Caraballo RS, Kruger J, Asman K, et al. Relapse among cigarette smokers: the CARDIA longitudinal study - 1985–2011. Addict Behav. 2014;39(1):101–106. doi:10.1016/j.addbeh.2013.08.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Gandhi KK, Foulds J, Steinberg MB, Lu SE, Williams JM. Lower quit rates among African American and Latino menthol cigarette smokers at a tobacco treatment clinic. Int J Clin Pract. 2009;63(3):360–367. [DOI] [PubMed] [Google Scholar]
- 46. Haas JS, Kaplan CP. The divide between breast density notification laws and evidence-based guidelines for breast cancer screening: legislating practice. JAMA Intern Med. 2015;175(2):1439–1440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Pletcher MJ, Hulley BJ, Houston T, Kiefe CI, Benowitz N, Sidney S. Menthol cigarettes, smoking cessation, atherosclerosis, and pulmonary function: the Coronary Artery Risk Development in Young Adults (CARDIA) Study. Arch Intern Med. 2006;166(17):1915–1922. [DOI] [PubMed] [Google Scholar]
- 48. Coambs RB, Li S, Kozlowski LT. Age interacts with heaviness of smoking in predicting success in cessation of smoking. Am J Epidemiol. 1992;135(3):240–246. http://aje.oxfordjournals.org/content/135/3/240.long Accessed August 3, 2015. [DOI] [PubMed] [Google Scholar]
- 49. Delnevo CD, Gundersen DA, Hrywna M, Echeverria SE, Steinberg MB. Smoking-cessation prevalence among U.S. smokers of menthol versus non-menthol cigarettes. Am J Prev Med. 2011;41(4):357–365. [DOI] [PubMed] [Google Scholar]
- 50. Mdodo R, Frazier EL, Dube SR, et al. Cigarette smoking prevalence among adults with HIV compared with the general adult population in the United States: cross-sectional surveys. Ann Intern Med. 2015;162(5):335–344. [DOI] [PubMed] [Google Scholar]
- 51. Novotny TE, Warner KE, Kendrick JS, Remington PL. Smoking by blacks and whites: socioeconomic and demographic differences. Am J Public Health. 1988;78(9):1187–1189. www.ncbi.nlm.nih.gov/pmc/articles/PMC1349391/ Accessed August 3, 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Sakuma KL, Felicitas J, Fagan P, et al. Smoking trends and disparities among Black and non-hispanic Whites in California [published online ahead of print February 8, 2015]. Nicotine Tob Res. 2015. doi:10.1093/ntr/ntv032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Trinidad DR, Pérez-Stable EJ, Messer K, White MM, Pierce JP. Menthol cigarettes and smoking cessation among racial/ethnic groups in the United States. Addiction. 2010;105(suppl 1):84–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Burns DM, Lee L, Shen LZ, et al. Cigarette Smoking Behavior in the United States. Monograph 8: Changes in Cigarette-Related Disease Risks and Their Implications for Prevention and Control: National Cancer Institute 1997:13–112. http://cancercontrol.cancer.gov/brp/tcrb/monographs/8/index.html Accessed August 3, 2015.
- 55. Burns D. Chapter 1: The Scientific Rationale for Comprehensive, Community-Based, Smoking Control Strategies. In: Shopland DR, Burns DM, Samet JM, Gritz ER, eds. Strategies to Control Tobacco Use in the United States: A Blueprint for Public Health Action in the 1990’s; NIH Publication No. 92–3316. Bethesda, MD: U.S. Department of Health and Human Services, Public Health Service, National Institutes of Health, National Cancer Institute; 1991. http://cancercontrol.cancer.gov/brp/tcrb/monographs/1/index.html Accessed August 3, 2015. [Google Scholar]
- 56. Husten CG, McCarty MC, Giovino GA, Chrismon JH, Zhu B. Intermittent smokers: a descriptive analysis of persons who have never smoked daily. Am J Public Health. 1998;88(1):86–89. www.ncbi.nlm.nih.gov/pmc/articles/PMC1508393/ Accessed August 3, 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Trinidad DR, Pérez-Stable EJ, Emery SL, White MM, Grana RA, Messer KS. Intermittent and light daily smoking across racial/ethnic groups in the United States. Nicotine Tob Res. 2009;11(2):203–210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Webb Hooper M, Kolar SK. Distress, race/ethnicity and smoking cessation in treatment-seekers: implications for disparity elimination. Addiction. 2015;110(9):1495–1504. [DOI] [PubMed] [Google Scholar]
- 59. DeNavas-Walt C, Proctor BD, Smith JC. Income, Poverty, and Health Insurance Coverage in the United States: 2009. Washington, DC: U.S. Government Printing Office; 2010. www.google.com/url?sa=t&rct=j&q=&esrc=s&source=web&cd=2&ved=0CCUQFjABahUKEwjt1cPD7vbHAhWGej4KHUJPAsc&url=https%3A%2F%2Fwww.census.gov%2Fprod%2F2010pubs%2Fp60-238.pdf&usg=AFQjCNG-z9nBg2REAX_ScqnQirEapne0IQ&cad=rja Accessed September 14, 2015. [Google Scholar]
- 60. Carroll ME, Anker JJ, Perry JL. Modeling risk factors for nicotine and other drug abuse in the preclinical laboratory. Drug Alcohol Depend. 2009;104(suppl 1):S70–78. doi:10.1016/j.drugalcdep.2008.11.011. [DOI] [PubMed] [Google Scholar]
- 61. Walker RE, Keane CR, Burke JG. Disparities and access to healthy food in the United States: a review of food deserts literature. Health Place. 2010;16(5):876–884. [DOI] [PubMed] [Google Scholar]
- 62. Haibach JP, Homish GG, Giovino GA. A longitudinal evaluation of fruit and vegetable consumption and cigarette smoking. Nicotine Tob Res. 2013;15(2):355–363. [DOI] [PubMed] [Google Scholar]
- 63. Hatch SL, Dohrenwend BP. Distribution of traumatic and other stressful life events by race/ethnicity, gender, SES and age: a review of the research. Am J Community Psychol. 2007;40(3):313–332. [DOI] [PubMed] [Google Scholar]
- 64. Gundersen DA, Delnevo CD, Wackowski O. Exploring the relationship between race/ethnicity, menthol smoking, and cessation, in a nationally representative sample of adults. Prev Med. 2009;49(6):553–557. [DOI] [PubMed] [Google Scholar]
- 65. Hyland A, Garten S, Giovino GA, Cummings KM. Mentholated cigarettes and smoking cessation: findings from COMMIT. Community Intervention Trial for Smoking Cessation. Tob Control. 2002;11(2):135–139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Fu SS, Okuyemi KS, Partin MR, et al. Menthol cigarettes and smoking cessation during an aided quit attempt. Nicotine Tob Res. 2008;10(3):457–462. [DOI] [PubMed] [Google Scholar]
- 67. Alexander L, Trinidad DR, KSakuma K, et al. Why we must continue to investigate menthol’s role in the African American smoking paradox. Nicotine Tob Res. 2016;18(S1):S94–S104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Brody AL, Mukhin AG, La Charite J, et al. Up-regulation of nicotinic acetylcholine receptors in menthol cigarette smokers. Int J Neuropsychopharmacol. 2013;16(5):957–966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Foulds J, Hooper MW, Pletcher MJ, Okuyemi KS. Do smokers of menthol cigarettes find it harder to quit smoking? Nicotine Tob Res. 2010;12(suppl 2):S102–109. doi:10.1093/ntr/ntq166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Anderson SJ. Marketing of menthol cigarettes and consumer perceptions: a review of tobacco industry documents. Tob Control. 2011;20(suppl 2):ii20–28. doi:10.1136/tc.2010.041939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Richter P, Beistle D, Pederson L, O’Hegarty M. Small-group discussions on menthol cigarettes: listening to adult African American smokers in Atlanta, Georgia. Ethn Health. 2008;13(2):171–182. [DOI] [PubMed] [Google Scholar]
- 72. Unger JB, Allen B, Jr, Leonard E, Wenten M, Cruz TB. Menthol and non-menthol cigarette use among Black smokers in Southern California. Nicotine Tob Res. 2010;12(4):398–407. [DOI] [PubMed] [Google Scholar]
- 73. Lacey LP, Manfredi C, Balch G, Warnecke RB, Allen K, Edwards C. Social support in smoking cessation among black women in Chicago public housing. Public Health Rep. 1993;108(3):387–394. [PMC free article] [PubMed] [Google Scholar]
- 74. Andrews JO, Mueller M, Newman SD, et al. The association of individual and neighborhood social cohesion, stressors, and crime on smoking status among African-American women in southeastern US subsidized housing neighborhoods. J Urban Health. 2014;91(6):1158–1174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Echeverría S, Diez-Roux AV, Shea S, Borrell LN, Jackson S. Associations of neighborhood problems and neighborhood social cohesion with mental health and health behaviors: the Multi-Ethnic Study of Atherosclerosis. Health Place. 2008;14(4):853–865. [DOI] [PubMed] [Google Scholar]
- 76. Lee JG, Henriksen L, Rose SW, Moreland-Russell S, Ribisl KM. A systematic review of neighborhood disparities in point-of-sale tobacco marketing. Am J Public Health. 2015;105(9):e8–e18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. National Institutes of Health. PATH: Population Assessment of Tobacco and Health 2015. https://pathstudyinfo.nih.gov/UI/HomeMobile.aspx Accessed July 6, 2015.
- 78. Sheffer CE, Stitzer M, Landes R, Brackman SL, Munn T, Moore P. Socioeconomic disparities in community-based treatment of tobacco dependence. Am J Public Health. 2012;102(3):e8–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Licht AS, King BA, Travers MJ, Rivard C, Hyland AJ. Attitudes, experiences, and acceptance of smoke-free policies among US multiunit housing residents. Am J Public Health. 2012;102(10):1868–1871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. Centers for Disease Control and Prevention. Response to increases in cigarette prices by race/ethnicity, income, and age groups--United States, 1976–1993. MMWR Morb Mortal Wkly Rep. 1998;47(29):605–609. www.cdc.gov/mmwr/preview/mmwrhtml/00054047.htm Accessed August 3, 2015. [PubMed] [Google Scholar]
- 81. Purnell JQ, Peppone LJ, Alcaraz K, et al. Perceived discrimination, psychological distress, and current smoking status: results from the Behavioral Risk Factor Surveillance System Reactions to Race module, 2004–2008. Am J Public Health. 2012;102(5):844–851. doi:10.2105/ajph.2012. 300694. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.