Abstract
Background:
Although radiological features of pneumocystis pneumonia (PCP) in non-Acquired Immune Deficiency Syndrome (AIDS) immunocompromised patients have been reported by other authors, there were no studies on the radiological stages of PCP previously. This study aimed to elucidate the radiological stages and prognoses of PCP in non-AIDS immunocompromised patients.
Methods:
Retrospective analysis of radiological manifestations and prognoses of 105 non-AIDS PCP immunocompromised patients from August 2009 to April 2016 was conducted. Chest radiograph was divided into three stages: early stage (normal or nearly normal chest radiograph), mid stage (bilateral pulmonary infiltrates), and late stage (bilateral pulmonary consolidations); chest high-resolution computed tomography (HRCT) was also divided into three stages: early stage (bilateral diffuse ground-glass opacity [GGO]), mid stage (bilateral diffuse GGO and patchy consolidations), and late stage (bilateral diffuse consolidations).
Results:
The case fatality rate (CFR) of all patients was 34.3% (36/105), all of them took routine chest X-ray (CXR), and 84 underwent chest CT examinations. According to the CXR most near the beginning of anti-PCP therapy, 18 cases were at early stage and CFR was 0 (0/18, P < 0.01), 50 cases were at mid stage and CFR was 28.0% (14/50, P > 0.05), and 37 cases were at late stage and CFR was 59.5% (22/37, P < 0.01). According to the chest HRCT most near the beginning of anti-PCP therapy, 40 cases were at early stage and CFR was 20.0% (8/40, P > 0.05), 34 cases were at mid stage and CFR was 47.1% (16/34, P > 0.05), and 10 cases were at late stage and CFR was 80.0% (8/10, P < 0.05); barotrauma, including pneumothorax, pneumomediastinum, and pneumohypoderma, was found in 18 cases and the CFR was 77.8% (14/18, P < 0.01).
Conclusions:
Based on the radiological manifestations, the course of PCP in non-AIDS immunocompromised patients can be divided into three stages: early stage, mid stage, and late stage. The prognoses of patients treated at early stage are good, and those at late stage are poor. Furthermore, the CFR of patients with barotrauma is high.
Keywords: Immunocompromised Patients, Pneumocystis Pneumonia, Prognosis, Radiological Stages
INTRODUCTION
Pneumocystis pneumonia (PCP) is an important and opportunistic pulmonary infection in Acquired Immune Deficiency Syndrome (AIDS) patients, which is caused by an odd fungus called Pneumocystis jirovecii, especially in AIDS patients with CD4+ T-cell < 0.2 × 109/L.[1] With the development of organ transplantation, chemotherapy and radiotherapy of malignant tumors, increasing prescriptions of glucocorticoids and cytotoxic drugs, the morbidity of PCP in non-AIDS immunocompromised patients has increased obviously in recent years in China.[2,3] Furthermore, PCP in non-AIDS immunocompromised patients is much more critical than that in AIDS patients.[4,5]
The imaging of PCP is characteristic but not specific, and the past studies focused only on the features.[6,7,8] Nevertheless, there are no studies on the radiological stages of PCP, which may be associated with the patient's prognoses.[9] In this study, we retrospectively analyzed the radiological manifestations and their characteristics; in addition, we defined new concepts of radiological stages of PCP and then analyzed the relationship between radiological stages and prognoses in non-AIDS immunocompromised patients.
METHODS
Patients
We retrospectively reviewed the radiological manifestations of 105 hospitalized non-AIDS immunocompromised patients who had a proven diagnosis of PCP in the Peking University First Hospital between August 2009 and April 2016. Ethical approval was obtained from the local institutional review boards. Informed consent was not required for this study. All data were obtained through a retrospective review of the Case File System in Peking University First Hospital.
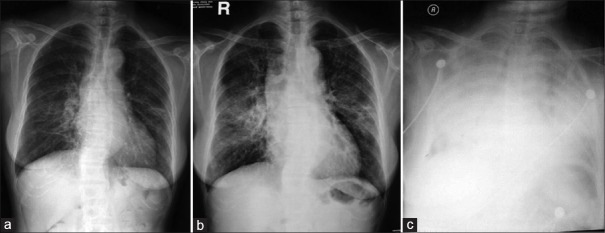
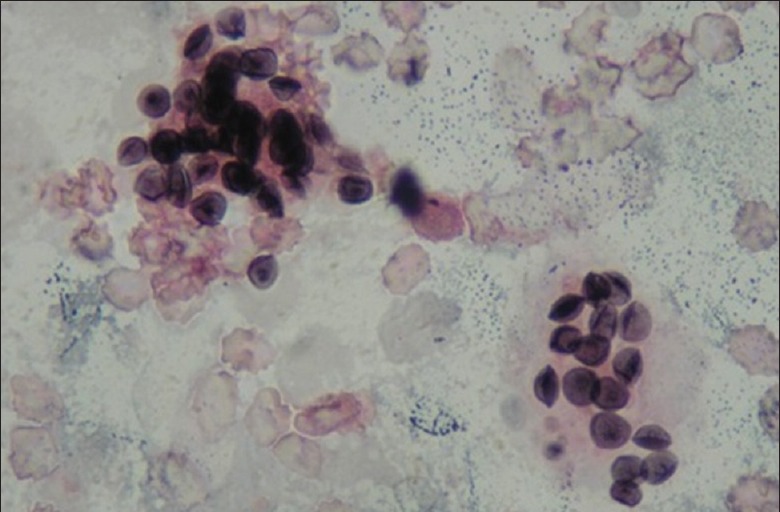
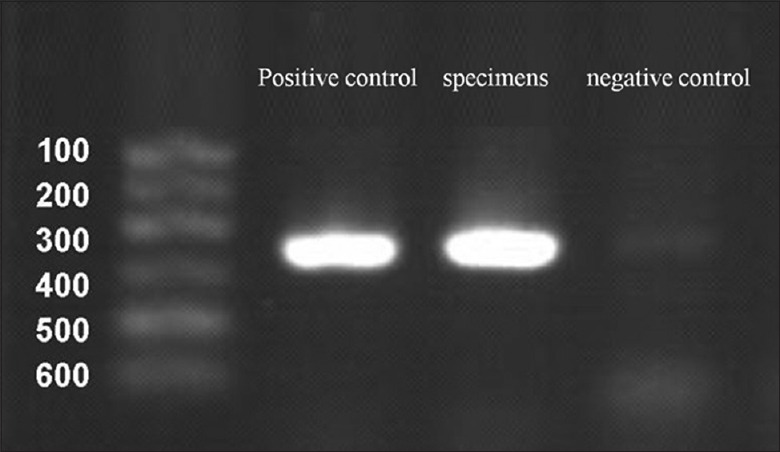
The 105 patients in our study fulfilled the gold standard diagnostic criteria of PCP.[1] Gomori methenamine silver (GMS) stains of bronchoalveolar lavage fluid (BALF) and/or sputum in all patients were positive for detecting cysts of P. jirovecii by high-power microscope [Figure 1]. Furthermore, polymerase chain reaction (PCR) assays of BALF and/or sputum were all positive [Figure 2].
Figure 1.
The cysts of Pneumocystis jirovecii were crowed in foamy alveolar casts in bronchoalveolar lavage fluid (GMS and eosin, ×1000).
Figure 2.
Agarose gel electrophoresis demonstrated typical polymerase chain reaction amplification findings of the mitochondrial large subunit ribosomal RNA gene of Pneumocystis jirovecii.
The mean age of the patients was 53 years (range, 13–81 years). Moreover, the group comprised 62 men and 43 women. All of them had some forms of immunosuppression, including immunosuppressive medications because of connective tissue diseases (n = 33), malignant tumors (n = 18), kidney transplantations (n = 14), primary renal disease (n = 16), and other diseases (n = 24). All patients had a fever or respiratory symptoms, but refractory to broad-spectrum antibiotics.
Trimethoprim-sulfamethoxazole was the first-line therapy of PCP for 21 days, and adjunctive corticosteroids were added in severe patients who had hypoxemia (the partial pressure of arterial oxygen while the patient breathing in room air is <70 mmHg or the alveolar–arterial gradient is above 35 mmHg).[1] Clindamycin combined with primaquine was used as second-line therapy; echinocandins were also administrated in some critically ill patients. If necessary, mechanical ventilations and/or other life supportive therapies were applied. All the clinical data were retrospectively reviewed by two independent physicians, and they reached a consensus decision.
Imaging examinations
In all the 105 patients, chest X-rays (CXRs) were taken and repeated; 84 patients underwent chest spiral computed tomography (CT) examinations and repeated in most of them. CT scans were performed with different scanner types, but with similar CT protocols. The CT scanners included a Somatom Plus 4 CT Scanner (Siemens, Erlangen, Germany), a GE Lightspeed Scanner (GE Medical Systems, Milwaukee, USA). Chest CT scans of the entire lungs were obtained while the patients were in a supine position at the end of inspiration. The scanning parameters included 120 kV, 150–350 mAs, 5 mm collimation, and a pitch of 1 or 1.5. All scans were viewed at standard lung window settings (level − 700 HU, width 1500 HU).
The CXR and chest CT images were retrospectively reviewed by two independent diagnostic radiologists who were experienced in the interpretation of thoracic radiological images. They reached a consensus decision regarding the findings. We used a standard glossary of radiological images definitions to describe the pulmonary lesions.[10]
Definitions of imaging stages
According to our previous study,[9] we defined new concepts of radiological stages of PCP in non-AIDS immunocompromised patients [Table 1]. The manifestations of CXR and chest CT of PCP were both divided into 3 stages: early stage, mid stage, and late stage. In the early stage, CXR was normal or nearly normal while chest CT scan showed bilateral diffuse ground-glass opacities (GGOs); in the mid stage, CXR showed bilateral pulmonary infiltrates while chest CT scan showed bilateral diffuse GGO and patchy consolidations; and in the late stage, CXR showed bilateral pulmonary consolidations while chest CT scan showed bilateral predominant consolidations. However, the stages of CXR and chest CT are not certainly accordant with each other.
Table 1.
Radiological stages of PCP in non-AIDS immunocompromised patients
| Stages | Manifestations of CXR | Manifestations of chest CT |
|---|---|---|
| Early | Normal or nearly normal | Bilateral diffuse GGO |
| Mid | Bilateral infiltrates | Bilateral diffuse GGO and patchy consolidations |
| Late | Bilateral consolidations | Bilateral predominant consolidations |
PCP: Pneumocystis pneumonia; GGO: Ground-glass opacity; CXR: Chest X-ray; CT: Computed tomography.
Statistical analysis
SPSS 17.0 (SPSS Inc., Chicago, IL, USA) software was applied for statistical analysis; all continuous variables were expressed as mean with standard deviation (SD). The case fatality rates (CFRs) between different groups were compared using Pearson Chi-square test, and P < 0.05 considered statistically significant.
RESULTS
Clinical data
There were totally 105 non-AIDS immunocompromised patients diagnosed as PCP in our hospital between August 2009 and April 2016. Clinical manifestations included fever (97/105), cough (71/105), and dyspnea (83/105). The average CD4+ T lymphoid cell count was 332 ± 218/mm3; average arterial oxygen partial pressure (PaO2) on room air of all the patients was 52.1 ± 16.7 mmHg; and average level of plasma lactate dehydrogenase was 621 ± 367 U/L. All of the patients were administrated by anti-PCP medications. Thirty-five patients underwent noninvasive and/or invasive mechanical ventilation. Continuous renal replacement therapy was carried out in 14 patients. Eventually, 69 patients survived and 36 died, and the overall CFR was 34.3% (36/105).
Stages of chest X-ray and prognoses
CXRs were taken in all the 105 non-AIDS immunocompromised patients with PCP. At the early stage, CXR was normal or nearly normal [Figure 3a]; at the mid stage, CXR showed bilateral pulmonary infiltrates [Figure 3b]; and at the late stage, CXR showed bilateral pulmonary consolidations [Figure 3c].
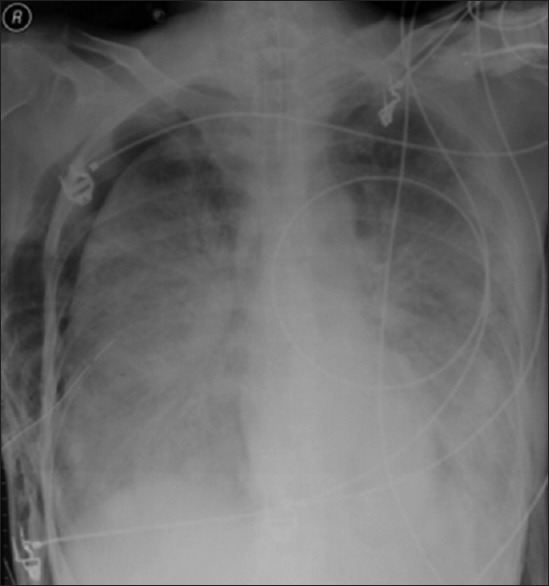
Figure 3.
Pneumocystis pneumonia in a 56-year-old female patient 3 months after renal transplantation. (a) In the 7th day of fever, chest X-ray was nearly normal. (b) In the 12th day of fever, chest X-ray showed bilateral pulmonary infiltrates (c) in the 16th day of fever, chest X-ray showed bilateral pulmonary consolidations (bilateral white lungs).
According to the CXR most near the beginning of anti-PCP therapy, CXR was at the early stage in 18 patients, and none of them was dead, the CRF was 0 (0/18, P < 0.05); CXR was at the mid stage in 50 patients, and 14 of them was dead, the CRF was 28.0% (14/50, P > 0.05); CXR was at the late stage in 37 patients, and 22 of them was dead, the CRF was 59.5% (22/37, P < 0.01) [Table 2].
Table 2.
Relationship between stages of CXR and prognoses of PCP in non-AIDS immunocompromised patients
| Stages | Case (n) | Death (n) | CFR (%) | χ2 | P |
|---|---|---|---|---|---|
| Early | 18 | 0 | 0 | 8.725 | 0.003 |
| Mid | 50 | 14 | 28.0 | 0.612 | 0.434 |
| Late | 37 | 22 | 59.5 | 7.176 | 0.007 |
| Total | 105 | 36 | 34.3 | ||
n: Number of patients; CFR: Case fatality rate; PCP: Pneumocystis pneumonia; CXR: Chest X-ray; CFR: Case fatality rate.
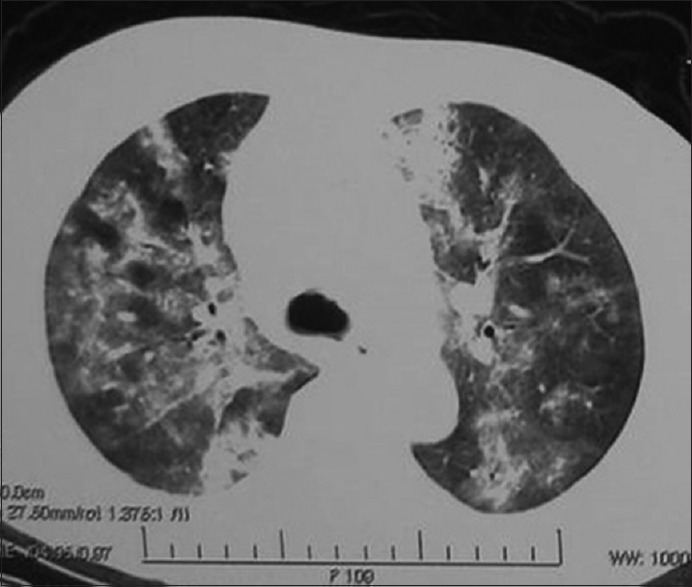
Stages of chest computed tomography and prognoses
Chest CT scans were performed in 84 non-AIDS immunocompromised patients with PCP. At the early stage, chest CT showed bilateral diffuse ground-glass opacity (GGO) [Figure 4]; at the mid stage, chest CT showed bilateral diffuse GGO and patchy consolidations [Figure 5]; and at the late stage, chest CT showed bilateral diffuse consolidations [Figure 6].
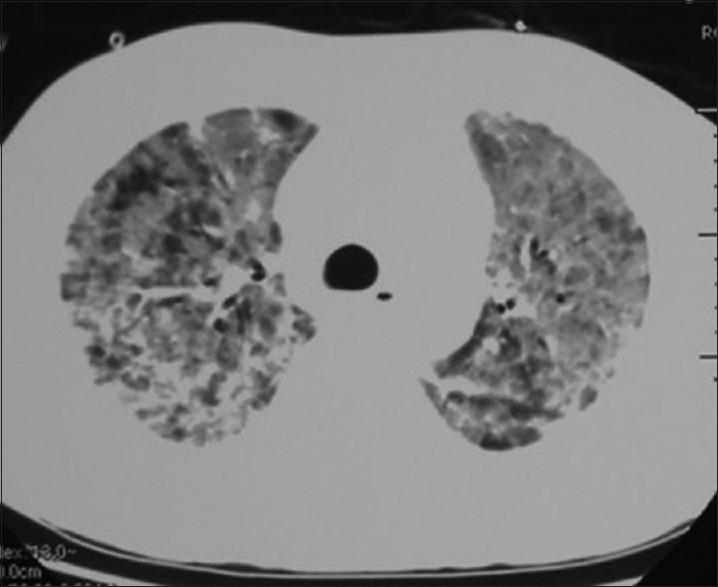
Figure 4.

Chest computed tomography showed bilateral diffuse ground-glass opacity in a 31-year-old male patient 14 months after renal transplantation.
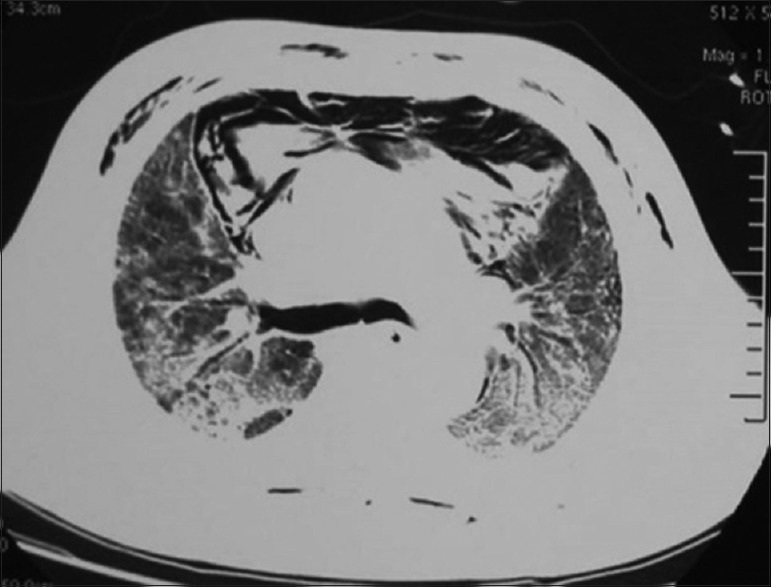
Figure 5.
Chest computed tomography showed bilateral diffuse ground-glass opacity and patchy consolidations in a 78-year-old female patient 2 months after immunosuppressive medications for retroperitoneal fibrosis.
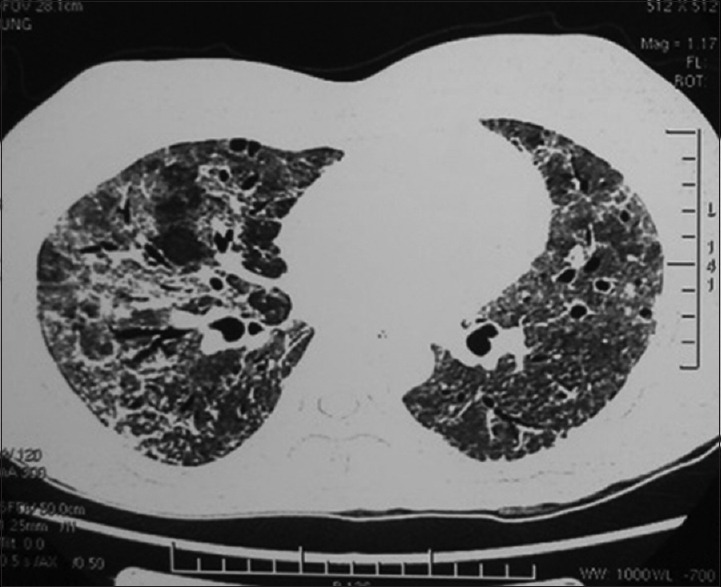
Figure 6.
Chest computed tomography showed bilateral pulmonary consolidations in a 50-year-old male patient 3 months after immunosuppressive medications for pemphigoid.
According to the chest high-resolution computed tomography (HRCT) most near the beginning of anti-PCP therapy, 40 cases were at early stage and CFR was 20.0% (8/40, P > 0.05), 34 cases were at mid stage and CFR was 47.1% (16/34, P > 0.05), and 10 cases were at late stage and CFR was 80.0% (8/10, P < 0.05); barotrauma, including pneumothorax, pneumomediastinum, and pneumohypoderma, was found in 18 cases and the CFR was 77.8% (14/18, P < 0.05).
According to the chest CT scans most near the beginning of anti-PCP therapy, chest CT was at the early stage in 40 patients, and 8 of them was dead, the CRF was 20.0% (8/40, P > 0.05); chest CT was at the mid stage in 34 patients, and 16 of them was dead, the CRF was 47.1% (16/34, P > 0.05); chest CT was at the mid stage in 10 patients, and 8 of them was dead, the CRF was 80.0% (8/10, P < 0.05) [Table 3].
Table 3.
Relationship between stages of chest CT and prognoses of PCP in non-AIDS immunocompromised patients
| Stages | Case (n) | Death (n) | CFR (%) | χ2 | P |
|---|---|---|---|---|---|
| Early | 40 | 8 | 20.0 | 4.060 | 0.054 |
| Mid | 34 | 16 | 47.1 | 0.806 | 0.369 |
| Late | 10 | 8 | 80.0 | 6.419 | 0.011 |
| Total | 84 | 32 | 38.1 | ||
n: Number of patients; CFR: Case fatality rate; CT: Computed tomography; PCP: Pneumocystis pneumonia.
Radiological features and prognoses
In the whole course of PCP in non-AIDS immunocompromised patients, radiological manifestations including GGO in 84 patients and 26 deaths (26/84, P > 0.05), mosaic sign in 64 patients and 20 deaths (20/64, P > 0.05), consolidations in 44 patients and 24 deaths (24/44, P > 0.05), pleural effusions in 20 patients and 8 deaths (8/20, P > 0.05), small nodules in 16 patients and 4 deaths (4/16, P > 0.05), barotrauma [Figures 7 and 8], including pneumothorax, pneumomediastinum and pneumohypoderma, in 18 patients and 14 deaths (14/18, P < 0.01), cystic lesions [Figure 9] in 14 patients and 6 deaths (6/14, P > 0.05), and thickened lobular septa in 14 patients and 6 deaths (6/14, P > 0.05) [Table 4].
Figure 7.
Chest X-ray showed right pneumothorax, pneumohypoderma and bilateral pulmonary consolidations in a 59-year-old male patient after immunosuppressive medications for nephrotic syndrome.
Figure 8.
Chest computed tomography showed bilateral diffuse ground-glass opacity, patchy consolidations, pneumomediastinum, and pneumohypoderma in a 56-year-old male patient after immunosuppressive medications for microscopic polyangiitis.
Figure 9.
Chest computed tomography demonstrated bilateral diffuse ground-glass opacity and multiple aerocysts in a 32-year-old female patient after chemotherapy for non-Hodgkin's lymphoma.
Table 4.
Relationship between radiological features and prognoses of PCP in non-AIDS immunocompromised patients
| Radiological features | Case (n) | Death (n) | CFR (%) | χ2 | P |
|---|---|---|---|---|---|
| GGO | 84 | 26 | 30.9 | 0.003 | 0.958 |
| Mosaic sign | 64 | 20 | 31.2 | 0.000 | 0.994 |
| Consolidations | 44 | 24 | 54.5 | 4.316 | 0.070 |
| Pleural effusions | 20 | 8 | 40.0 | 0.586 | 0.444 |
| Small nodules | 16 | 4 | 25.0 | 0.263 | 0.608 |
| Barotrauma | 18 | 14 | 77.8 | 14.328 | 0.000 |
| Cystic lesions | 14 | 6 | 42.8 | 0.759 | 0.384 |
| Thickened lobular septa | 14 | 6 | 42.8 | 0.759 | 0.384 |
| Total | 105 | 36 | 34.3 | ||
Barotrauma included aerothorax, pneumomediastinum, and pneumohypoderma. n: Number of patients; CFR: Case fatality rate; GGO: Ground-glass opacity; PCP: Pneumocystis pneumonia.
DISCUSSION
Although the radiological appearances of PCP have been reported by many authors, they have been noted only radiological features such as diffuse infiltrates on CXR and GGO on CT, and there was no further analysis of the dynamic evolution of radiological imaging in patients with PCP.[6,7,8] In the natural course of PCP, radiological imaging continuously progresses and reflects the severity of the disease.[8] Furthermore, PCP in non-AIDS immunocompromised patients is much more critical than that in AIDS patient, and without treatment, their mortality approaches 100%; if it is treated timely, most of them will be cured.[4] Therefore, radiological stages and manifestations should be closely correlated with prognosis. However, there was no concept of radiological stages of PCP in the previous literature, and let alone studies on the relationship between them and prognoses. According to our previous study,[9] we defined radiological stages of PCP in non-AIDS immunocompromised patients in this article, which included early stage, mid stage, and late stage of both CXR and chest CT, although the stages between them are not completely coincident.
In the early stage, CXR of PCP in non-AIDS immunocompromised patients is normal or nearly normal, and the patients usually present with mild fever and/or dyspnea and without any abnormal sign on auscultation of chest. Our study showed that all the patients were cured if they began specific anti-PCP therapy in the early stage of CXR. Nevertheless, the diagnosis of PCP in this stage is difficult to be confirmed, and HRCT has proved to be more sensitive than CXR for the detection and characterization of PCP.[6] In the early stage, when CXR is normal, chest HRCT has shown bilateral diffuse GGO.[10] If clinicians can recognize early radiological features of PCP, GMS stains and PCR assay of BALF or sputum should be carried out to confirm the diagnosis in the early stage.[1,2] The early stage of PCP in AIDS patients last longer than that in non-AIDS immunosuppressed hosts.[4,5] Because of the more rapid progressions of PCP in non-AIDS immunosuppressed hosts, it is important to confirm the diagnosis of PCP in the early stage and begin specific anti-PCP therapy as early as possible, which can sharply reduce the mortality and improve prognosis.[11]
In the mid stage, CXR of PCP in non-AIDS immunocompromised patients showed bilateral pulmonary infiltrates, while chest CT scans are mixed with bilateral diffuse GGO and patchy Consolidations, which are the radiological characteristics of PCP.[12] However, the stages of CXR and chest CT are not certainly accordant with each other. When CXR is at the mid stage, chest CT may be at the early- or mid-stage. In the mid stage, the patients usually present with obvious dyspnea and hypoxemia,[13] and then clinicians just recognize the diagnosis of PCP, although PCP in patients without AIDS was diagnosed after a shorter time interval from symptom onset.[8] Our study showed that the CFR of PCP is significantly higher when specific anti-PCP treatments begin in the mid stage rather than early stage.
In the late stage, CXRs show bilateral diffuse pulmonary consolidations, which are known as “while lungs.”[9] Moreover, predominant consolidations were also found in bilateral lung fields of chest CT scans. Pulmonary consolidations are more likely to occur in patients without AIDS rather than those with AIDS.[7] Most of the patients in this stage present with severe dyspnea and hypoxemia and some of them manifest as acute respiratory distress syndrome.[14] Consequently, intubation and mechanical ventilation are usually unavoidable because of respiratory distress and failure.[15] In the late stage of severe PCP, without treatment, all of them are doomed to die;[4] begin specific anti-PCP therapy immediately, many of them still cannot survive.[3,15] Our study revealed the similar endings. Other studies showed that echinocandins and extracorporeal membrane oxygenation might be helpful in such critical situations.[16,17]
In addition, our study showed that primary radiological features of PCP in non-AIDS immunocompromised patients comprised bilateral diffuse GGO with mosaic signs and consolidations; other manifestations included pleural effusions, small nodules, aerothorax, pneumomediastinum, pneumohypoderma, cystic lesions, and thickened lobular septa, which were consistent with previous studies.[6,7,8] Aerothorax, pneumomediastinum, and pneumohypoderma are often associated with barotrauma because of mechanical ventilation, and patients with barotrauma have extremely poor prognosis.[18,19] PCP prone to barotrauma might also have a relationship with cystic lesions.[20] However, cystic lesions are rare in non-AIDS immunocompromised patients.[6,8] In our study, no other radiological manifestations had a significant relationship with prognoses.
There are several limitations in our study. First, CXRs were taken in the supine position in some severe patients, which might result in different manifestations of CXR. Second, in most patients, CXR was the first imaging examination rather than chest CT scans and the repeat examinations of CXR were more often than that of CT scans. Third, mixed pulmonary infections affected the clinical and radiological manifestations of patients. Finally, this article was a retrospective monocentric study and the number of patients was small, and hence, larger prospective multicenter researches are needed in the future.
In conclusion, based on radiological manifestations, the course of PCP in non-AIDS immunocompromised patients can be divided into three stages: early stage, mid stage, and late stage. The prognoses of patients treated at early stage are good, and those at late stage are poor. Furthermore, the CFR of patients with barotrauma is high.
Financial support and sponsorship
This study was supported by a grant from the Special Foundation of Capital Health Research and Development (No. 2014-4-4072).
Conflicts of interest
There are no conflicts of interest.
Footnotes
Edited by: Li-Shao Guo
REFERENCES
- 1.Bienvenu AL, Traore K, Plekhanova I, Bouchrik M, Bossard C, Picot S. Pneumocystis pneumonia suspected cases in 604 non-HIV and HIV patients. Int J Infect Dis. 2016;46:11–7. doi: 10.1016/j.ijid.2016.03.018. doi: 10.1016/j.ijid.2016.03.018. [DOI] [PubMed] [Google Scholar]
- 2.Ling C, Qian S, Wang Q, Zeng J, Jia X, Liu J, et al. Pneumocystis pneumonia in non-HIV children: A 10-year Retrospective Study. Clin Respir J. 2016 doi: 10.1111/crj.12467. Epub ahead of print. doi: 10.1111/crj.12467. [DOI] [PubMed] [Google Scholar]
- 3.Mu XD, Wang GF, Su L. A clinical comparative study of polymerase chain reaction assay for diagnosis of pneumocystis pneumonia in non-AIDS patients. Chin Med J. 2011;124:2683–6. doi: 10.3760/cma.j.issn.0366-6999.2011.17.021. [PubMed] [Google Scholar]
- 4.Rouyer M, Stoclin A, Blanc FX. Pneumocystis pneumonia in HIV-negative adults. Rev Mal Respir. 2015;32:985–90. doi: 10.1016/j.rmr.2015.06.007. doi: 10.1016/j.rmr.2015.06.007. [DOI] [PubMed] [Google Scholar]
- 5.Roux A, Gonzalez F, Roux M, Mehrad M, Menotti J, Zahar JR, et al. Update on pulmonary Pneumocystis jirovecii infection in non-HIV patients. Med Mal Infect. 2014;44:185–98. doi: 10.1016/j.medmal.2014.01.007. doi: 10.1016/j.medmal.2014.01.007. [DOI] [PubMed] [Google Scholar]
- 6.Vogel MN, Vatlach M, Weissgerber P, Goeppert B, Claussen CD, Hetzel J, et al. HRCT-features of Pneumocystis jiroveci pneumonia and their evolution before and after treatment in non-HIV immunocompromised patients. Eur J Radiol. 2012;81:1315–20. doi: 10.1016/j.ejrad.2011.02.052. doi: 10.1016/j.ejrad.2011.02.052. [DOI] [PubMed] [Google Scholar]
- 7.Pitcher RD, Daya R, Beningfield SJ, Zar HJ. Chest radiographic presenting features and radiographic progression of pneumocystis pneumonia in South African children. Pediatr Pulmonol. 2011;46:1015–22. doi: 10.1002/ppul.21465. doi: 10.1002/ppul.21465. [DOI] [PubMed] [Google Scholar]
- 8.Hardak E, Brook O, Yigla M. Radiological features of Pneumocystis jirovecii Pneumonia in immunocompromised patients with and without AIDS. Lung. 2010;188:159–63. doi: 10.1007/s00408-009-9214-y. doi: 10.1007/s00408-009-9214-y. [DOI] [PubMed] [Google Scholar]
- 9.Mu XD, Gao L, Wang RG, Su L, Zhang C, Que CL, et al. Retrospective analysis of relationship between radiological features and prognoses of pneumocystis pneumonia in non-AIDS immunocompromised patients (in Chinese) Nat Med J Chin. 2012;92:2703–6. doi: 10.3760/cma.j.issn.0376-24912012.38.011. [PubMed] [Google Scholar]
- 10.Richards PJ, Riddell L, Reznek RH, Armstrong P, Pinching AJ, Parkin JM. High resolution computed tomography in HIV patients with suspected Pneumocystis carinii pneumonia and a normal chest radiograph. Clin Radiol. 1996;51:689–93. doi: 10.1016/s0009-9260(96)80239-x. [DOI] [PubMed] [Google Scholar]
- 11.Asai N, Motojima S, Ohkuni Y, Matsunuma R, Nakashima K, Iwasaki T, et al. Early diagnosis and treatment are crucial for the survival of Pneumocystis pneumonia patients without human immunodeficiency virus infection. J Infect Chemother. 2012;18:898–905. doi: 10.1007/s10156-012-0441-4. doi: 10.1007/s10156-012-0441-4. [DOI] [PubMed] [Google Scholar]
- 12.Song T, Wei LP, Chen WJ, Liu P, Mai WW, Li ZZ. Imaging characteristics of pneumocystis pneumonia after renal transplantation. Ren Fail. 2010;32:78–84. doi: 10.3109/08860220903367510. doi: 10.3109/088602;20903367510. [DOI] [PubMed] [Google Scholar]
- 13.Wang HW, Lin CC, Kuo CF, Liu CP, Lee CM. Mortality predictors of Pneumocystis jirovecii pneumonia in human immunodeficiency virus-infected patients at presentation: Experience in a tertiary care hospital of northern Taiwan. J Microbiol Immunol Infect. 2011;44:274–81. doi: 10.1016/j.jmii.2010.08.006. doi: 10.1016/j.jmii.2010.08.006. [DOI] [PubMed] [Google Scholar]
- 14.Ainoda Y, Hirai Y, Fujita T, Isoda N, Totsuka K. Analysis of clinical features of non-HIV Pneumocystis jirovecii pneumonia. J Infect Chemother. 2012;18:722–8. doi: 10.1007/s10156-012-0408-5. doi: 10.1007/s10156-012-0408-5. [DOI] [PubMed] [Google Scholar]
- 15.Ko Y, Jeong BH, Park HY, Koh WJ, Suh GY, Chung MP, et al. Outcomes of Pneumocystis pneumonia with respiratory failure in HIV-negative patients. J Crit Care. 2014;29:356–61. doi: 10.1016/j.jcrc.2013.12.005. doi: 10.1016/j.jcrc.2013.12.005. [DOI] [PubMed] [Google Scholar]
- 16.Mu XD, Que CL, He B, Wang GF, Li HC. Caspofungin in salvage treatment of severe pneumocystis pneumonia: Case report and literature review. Chin Med J. 2009;122:996–9. doi: 10.3760/cma.j.issn.0366-6999.2009.08.023. [PubMed] [Google Scholar]
- 17.Cawcutt K, Gallo De Moraes A, Lee SJ, Park JG, Schears GJ, Nemergut ME. The use of ECMO in HIV/AIDS with Pneumocystis jirovecii Pneumonia: A case report and review of the literature. ASAIO J. 2014;60:606–8. doi: 10.1097/MAT.0000000000000112. doi: 10.1097/MAT.0000000000000112. [DOI] [PubMed] [Google Scholar]
- 18.Pastores SM, Garay SM, Naidich DP, Rom WN. Review: Pneumothorax in patients with AIDS-related Pneumocystis carinii pneumonia. Am J Med Sci. 1996;312:229–34. doi: 10.1097/00000441-199611000-00008. doi: 10.4103/2320-8775;.158834. [DOI] [PubMed] [Google Scholar]
- 19.Safe IP, Oliveira VC, Marinho PM, Lacerda MV, Damian MM. Spontaneous pneumothorax: A fatal complication in HIV-infected patients. Braz J Infect Dis. 2014;18:466. doi: 10.1016/j.bjid.2014.04.004. doi: 10.1016/j.bjid.2014.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cho JY, Kim DM, Kwon YE, Yoon SH, Lee SI. Newly formed cystic lesions for the development of pneumomediastinum in Pneumocystis jirovecii pneumonia. BMC Infect Dis. 2009;9:171. doi: 10.1186/1471-2334-9-171. doi: 10.1186/1471. [DOI] [PMC free article] [PubMed] [Google Scholar]