Abstract
Background and Aims:
Most vital aspect of Endoscopic Sinus Surgery (ESS) is an optimal visibility in the surgical field. This invariably requires controlled hypotension to facilitate surgical dissection and to decrease operative time. We used esmolol and magnesium sulfate to achieve controlled hypotension and assessed the quality of the surgical field in ESS.
Material and Methods:
A total of 30 patients undergoing ESS, were enrolled in three parallel groups of 10 patients each in a prospective randomized double-blind study. “Magnesium Sulfate group” received magnesium sulfate 40 mg/kg intravenously (i.v.) as a bolus over 10 min before induction of anesthesia, followed by 15-30 mg/kg/h through infusion. “Esmolol group” received 0.5 mg/kg i.v. bolus over 10 min after induction followed by 150-300 μg/kg/min infusion and “control group” received normal saline in same volume schedule. The primary aim was to assess the quality of surgical field, using Fromme scale. Category Scale values of all the three groups were compared using Kruskal-Wallis analysis of variance (ANOVA) test. Hemodynamic data was compared using ANOVA test.
Results:
Quality of the surgical field was better in both magnesium sulfate and esmolol groups as compared to the control group. Durations of anesthesia and surgery were significantly lower in esmolol group as compared to the control group. Blood loss was comparable in all the three groups.
Conclusion:
Quality of the surgical field was better in esmolol and magnesium sulfate groups as compared to control group. Duration of surgery was significantly less in esmolol group as compared to other two groups.
Key words: Controlled hypotension, esmolol, magnesium sulfate, paranasal sinus surgery
Introduction
Endoscopic Sinus Surgery (ESS) is a well-established procedure for a variety of sinonasal diseases. Even a small amount of bleeding can hinder the confined area of visibility in ESS.[1] Bleeding makes the surgery difficult and increases the risk of complications.[2] Controlled hypotension provides a relatively bloodless surgical field and facilitates surgical dissection.[3] Hypotensive techniques are associated with certain disadvantages. Hence, the anesthesiologists are still in search of the drugs with fewer side-effects.
Various drugs have been used to achieve controlled hypotension such as beta-blockers, nitroglycerine, sodium nitroprusside and magnesium sulfate.
Esmolol is a cardio-selective beta-1 receptor blocker with rapid onset as well as short duration. It has no significant membrane stabilizing activity at therapeutic dosages. Intravenous (i.v.) magnesium sulfate is a satisfactory agent to achieve controlled hypotension. The mechanism of action is through vasodilatation by inhibiting angiotensin converting enzyme activity as well as myocardial depression.
We conducted this study to evaluate the quality of the surgical field during esmolol or magnesium sulfate-induced controlled hypotension and compared it to normotensive (control) group in patients with sinus diseases.
Material and Methods
The study was conducted after due approval by the Institutional Ethics Committee (IEC Approval no. MS/258/MD/5068) and a written informed consent. Thirty patients, belonging to American Society of Anesthesiologists (ASA) physical status I-II, scheduled for ESS, were randomly allocated, using a computerized program, in one of the three parallel groups of 10 each (magnesium sulfate, esmolol, control). This study was conducted during a period from July 2007 to October 2008. The sample size was calculated by using a web-based power sample calculator as 10 patients in each group, based on previous studies to achieve a β-power of 80% with a sample of 30 patients. The quality of surgical field based on Formme scale was taken as endpoint for calculating the sample size.
Exclusion criteria included the patients on β-blockers and cardiovascular active drugs, major hepatic, renal or cardiac disease and hematological disorders. Furthermore, patients allergic to magnesium sulfate, history of neuromuscular disorder, diabetic neuropathy, pregnancy, and prior treatment with opioids or anticoagulants were excluded.
All the surgeries were performed by the same surgeon to minimize observer('s) bias. In this study, all the participants and the surgeon were blinded to the drug used for controlled hypotension.
All the patients were kept nil per os for 8 hrs. Premedication included oral alprazolam 0.25 mg a night before and 2 h prior to the surgery. In the operating room, i.v. line was secured and normal saline infusion was started. Standard monitoring included electrocardiogram, direct arterial blood pressure and pulse oximetry. All the patients received i.v. morphine 0.1 mg/kg for analgesia. Induction was achieved with propofol 1-2 mg/kg and tracheal intubation was facilitated with vecuronium, 0.1 mg/kg. Subsequently, anesthesia was maintained with 60% nitrous oxide in oxygen and propofol infusion, 50-150 µg/kg/min. Neuromuscular blockade was reversed with 0.05 mg/kg neostigmine and 0.01 mg/kg glycopyrrolate and trachea was extubated when the patient regained consciousness and was able to protect the airway.
Controlled hypotension was defined as mean arterial pressure (MAP) of 55-65 mmHg. Magnesium sulfate group received 10% i.v. magnesium sulfate, 40 mg/kg as bolus over a period of 10 min before the induction of anesthesia a followed by 15-30 mg/kg/h as infusion to achieve MAP of 55-65 mmHg. Esmolol group received i.v. esmolol 500 µg/kg/min as a bolus over 10 min after induction followed by infusion at the rate of 100-300 µg/kg/min. Control group received normal saline in the same volume-schedule and MAP was maintained ±10% of baseline value. In this group, tachycardia and hypertension were treated by increasing the depth of anesthesia, hyperventilation and bolus dose of fentanyl. Bradycardia and hypotension were managed by correcting the underlying cause and by administration of fluids.
Any intraoperative or postoperative complications, such as excessive hypotension (MAP <50 mmHg), hypertension (MAP >10% of baseline), need of additional hypotensive agents or vasopressors, tachycardia, bradycardia, bronchospasm, arrhythmias or delayed recovery were noted. Rescue antihypertensive agent was nitroglycerine and the patients requiring it were excluded from the study. Bradycardia was generally self-limiting and was corrected spontaneously after stopping infusion of esmolol if required. Excessive hypotension in any group was managed by stopping the infusion of hypotensive agent and by fluid boluses.
Subjective assessment of the surgical field for bleeding was carried out by the surgeon according to category scale adapted from Fromme et al.[4] Category scale values of 2 and 3 for the surgical field were considered as ideal.
The blood was sucked in a preheparinized suction canister. The amount of blood loss was calculated from the fluid volume of the suction canister (V), the Hb concentration of the suction canister, and the patient's mean Hb concentration at the beginning and end of surgery (Hbm) using the following equation:
Blood loss (mL) = Hb (gdL/1) × V (mL)/Hbm (g/dL).
Data was analyzed by using Statistical Package for Social Sciences (SPSS version 17 for Windows, Chicago, Illinois, USA), and expressed as mean ± standard error, medians and range. Continuous Scale values of all the three groups were compared using Kruskal-Wallis analysis of variance (ANOVA) test. That was followed by Mann-Whitney U-test to assess the significance of various groups. For categorical data, Chi-square test was applied. Hemodynamic data was compared with one-way ANOVA test. P < 0.05 was considered as statistically significant.
Results
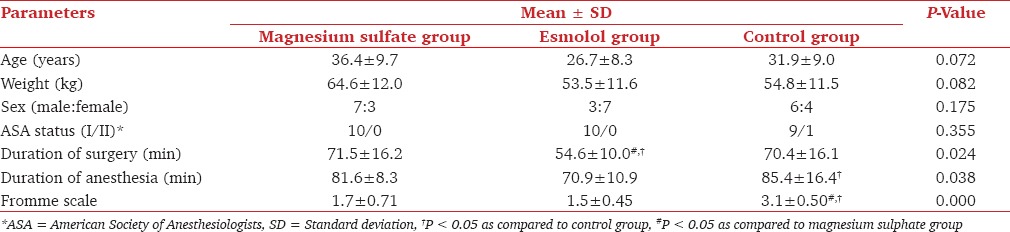
All the groups were comparable with respect to age, sex, weight and ASA status [Table 1]. The durations of surgery and anesthesia were significantly less in esmolol group as compared to control and magnesium sulfate group [Table 1].
Table 1.
Demographic characteristics and Fromme scale values
The preanesthetic MAP and heart rate (HR) were comparable between the groups. MAP was significantly lower at 5-60 min in both magnesium sulfate and esmolol group [Figures 1 and 2] as compared to the control group. There were no episodes of excessive hypotension (MAP <50 mm Hg), arrhythmias or reflex tachycardia and rebound hypertension in esmolol or magnesium sulfate groups. Hemodynamic parameters were kept within 10% of baseline value in the control group.
Figure 1.
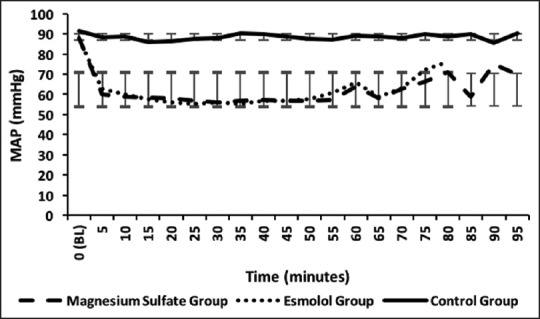
Comparison of mean arterial pressure between three groups. MAP, Mean Arterial Pressure; BL, Baseline
Figure 2.
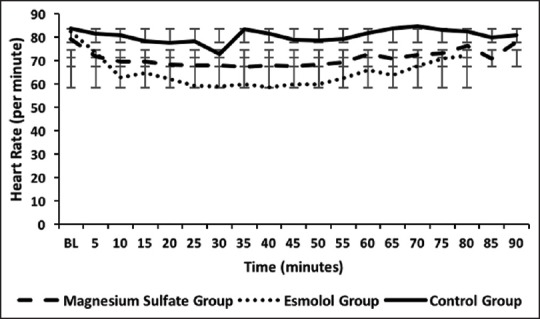
Comparison of heart rate between three groups. BL, Baseline
The quality of the operative field was significantly better in esmolol and magnesium sulfate groups at 5-60 min as compared to the control group [Table 1].
Intraoperative blood loss was comparable in all the three groups. Mean blood loss was 138 ± 26, 140 ± 30, and 142 ± 42 mL in, esmolol, magnesium sulfate and control groups respectively.
Discussion
Magnesium sulfate was included in the study as it is a vasodilator with minimal myocardial depression.[5] Neuroprotective effects of magnesium sulfate and its effect on cerebral blood flow[6,7] can be advantageous during controlled hypotension. However, there are the potential risks of magnesium such as, potentiation of opioids and neuromuscular blockers leading to delayed emergence.[8,9] Elsharnouby and Elsharnouby[10] concluded that magnesium sulfate leads to a reduction in arterial pressure, HR, blood loss and duration of sinus surgery.
In our study, the duration of anesthesia was prolonged in magnesium sulfate group. This prolongation can be explained by the potentiation of neuromuscular blocking drugs as well as more bleeding in the surgical field than esmolol group. In control group, total duration of anesthesia and surgery was increased because of excessive bleeding as compared to other groups.
Improved surgical field during ESS with β-blockers is probably attributable to vasoconstriction of the mucous membrane arterioles and the precapillary sphincters that results from unopposed α-adrenergic effects of endogenous catecholamine and the increased sympathetic tone.[11] The β-blockers slow the HR, reduce the myocardial contractility increase the diastolic time, resulting in decreased venous tone and greater venous capacitance. This results in reduced venous oozing in the surgical field. The patients who maintain a tachycardia during surgery were benefited with β-blocker therapy.
Guney et al.[12] found that esmolol provides hemodynamic stability and good surgical field visibility and should be considered as an alternative to nitroglycerin. Sieskiewicz et al.,[13] concluded that if HR is around 60 beats/min there is no need to decrease the MAP to dangerously low levels to achieve good operative field conditions. Other studies[14,15] comparing propofol and isoflurane also showed decreasing heart rate with fentanyl boluses provides a better operative field.
Both hypotensive groups had better quality of the surgical field than the control group. Previous studies have demonstrated that MAP and total blood loss are not necessarily correlated.[4,16] Use of inhalational agents such as isoflurane to decrease MAP to <70 mmHg may increase bleeding and worsen surgical field because of peripheral vasodilation and tachycardia.[17]
We conclude that magnesium sulfate and esmolol, by achieving controlled hypotension, significantly improve the surgical field during endoscopic sinus surgery.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Nair S, Collins M, Hung P, Refes G, Close D, Wormald PJ. The effect of beta-blocker premedication on the surgical field during endoscopic sinus surgery. Laryngoscope. 2004;114:1042–6. doi: 10.1097/00005537-200406000-00016. [DOI] [PubMed] [Google Scholar]
- 2.Baker AR, Baker AB. Anaesthesia for endoscopic sinus surgery. Acta Anaesthesiol Scand. 2010;54:795–803. doi: 10.1111/j.1399-6576.2010.02259.x. [DOI] [PubMed] [Google Scholar]
- 3.Carifi M. Perioperative bleeding control in functional endoscopic sinus surgery. Eur Arch Otorhinolaryngol. 2014;271:845–6. doi: 10.1007/s00405-013-2716-5. [DOI] [PubMed] [Google Scholar]
- 4.Fromme GA, MacKenzie RA, Gould AB, Jr, Lund BA, Offord KP. Controlled hypotension for orthognathic surgery. Anesth Analg. 1986;65:683–6. [PubMed] [Google Scholar]
- 5.Ghodraty MR, Homaee MM, Farazmehr K, Nikzad-Jamnani AR, Soleymani-Dodaran M, Pournajafian AR, et al. Comparative induction of controlled circulation by magnesium and remifentanil in spine surgery. World J Orthop. 2014;5:51–6. doi: 10.5312/wjo.v5.i1.51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wong GK, Kwok R, Tang K, Yeung D, Ahuja A, King AD, et al. Effects of magnesium sulfate infusion on cerebral perfusion in patients after aneurysmal SAH. Acta Neurochir Suppl. 2010;106:133–5. doi: 10.1007/978-3-211-98811-4_23. [DOI] [PubMed] [Google Scholar]
- 7.Mori K, Yamamoto T, Miyazaki M, Hara Y, Aiko Y, Koike N, et al. Effect of intrathecal magnesium sulfate solution injection via a microcatheter in the cisterna magna on cerebral vasospasm in the canine subarachnoid haemorrhage model. Br J Neurosurg. 2012;26:64–8. doi: 10.3109/02688697.2011.591948. [DOI] [PubMed] [Google Scholar]
- 8.Gupta K, Vohra V, Sood J. The role of magnesium as an adjuvant during general anaesthesia. Anaesthesia. 2006;61:1058–63. doi: 10.1111/j.1365-2044.2006.04801.x. [DOI] [PubMed] [Google Scholar]
- 9.Ray M, Bhattacharjee DP, Hajra B, Pal R, Chatterjee N. Effect of clonidine and magnesium sulphate on anaesthetic consumption, haemodynamics and postoperative recovery: A comparative study. Indian J Anaesth. 2010;54:137–41. doi: 10.4103/0019-5049.63659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Elsharnouby NM, Elsharnouby MM. Magnesium sulphate as a technique of hypotensive anaesthesia. Br J Anaesth. 2006;96:727–31. doi: 10.1093/bja/ael085. [DOI] [PubMed] [Google Scholar]
- 11.Jacob SM, Chandy TT, Cherian VT. Oral bisoprolol improves surgical field during functional endoscopic sinus surgery. J Anaesthesiol Clin Pharmacol. 2014;30:59–64. doi: 10.4103/0970-9185.125705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Guney A, Kaya FN, Yavascaoglu B, Gurbet A, Selmi NH, Kaya S, et al. Comparison of esmolol to nitroglycerine in controlling hypotension during nasal surgery. Eurasian J Med. 2012;44:99–105. doi: 10.5152/eajm.2012.23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sieskiewicz A, Drozdowski A, Rogowski M. The assessment of correlation between mean arterial pressure and intraoperative bleeding during endoscopic sinus surgery in patients with low heart rate. Otolaryngol Pol. 2010;64:225–8. doi: 10.1016/S0030-6657(10)70020-2. [DOI] [PubMed] [Google Scholar]
- 14.Tirelli G, Bigarini S, Russolo M, Lucangelo U, Gullo A. Total intravenous anaesthesia in endoscopic sinus-nasal surgery. Acta Otorhinolaryngol Ital. 2004;24:137–44. [PubMed] [Google Scholar]
- 15.Ankichetty SP, Ponniah M, Cherian V, Thomas S, Kumar K, Jeslin L, et al. Comparison of total intravenous anesthesia using propofol and inhalational anesthesia using isoflurane for controlled hypotension in functional endoscopic sinus surgery. J Anaesthesiol Clin Pharmacol. 2011;27:328–32. doi: 10.4103/0970-9185.83675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kerr AR. Anaesthesia with profound hypotension for middle ear surgery. Br J Anaesth. 1977;49:447–52. doi: 10.1093/bja/49.5.447. [DOI] [PubMed] [Google Scholar]
- 17.Van Aken H, Cottrell JE. Hypotensive anesthesia and its effects on cardiovascular system. In: Altura BM, Halevey S, editors. Cardiovascular Actions of Anaesthetics and Drugs Used in Anesthesia. 5th ed. Basel: Kerger Publishers; 1986. pp. 46–50. [Google Scholar]


