Abstract
Background and Aims:
Long distance air travel for medical needs is on the increase worldwide. The condition of some patients necessitates specially modified aircraft, and monitoring and interventions during transport by trained medical personnel. This article presents our experience in domestic and international interhospital air medical transportation from January 2010 to January 2014.
Material and Methods:
Hospital records of all air medical transportation undertaken to the institute during the period were analyzed for demographics, primary etiology, and events during transport.
Results:
586 patients, 453 (77.3%) males and 133 (22.6%) females of ages 46.7 ± 12.6 years and 53.4 ± 9.7 years were transported by us to the institute. It took 3030 flying hours with an average of 474 ± 72 min for each mission. The most common indication for transport was cardiovascular diseases in 210 (35.8%) and central nervous system disease in 120 (20.4%) cases. The overall complication rate was 5.3% There was no transport related mortality.
Conclusion:
Cardiac and central nervous system ailments are the most common indication for air medical transportation. These patients may need attention and interventions as any critical patient in the hospital but in a difficult environment lacking space and help. Air medical transport carries no more risk than ground transportation.
Key words: Air ambulance, air medical transportation, critical care, interhospital transfer, patient transport
Introduction
The use of air medical transportation has risen over the past two decades.[1] Air medical transportation has evolved from balloons used during the First World War to the massive evacuation exercise undertaken by the Indian forces in Uttarakhand and Kashmir in recent times. Many more patients are transported daily in need of advanced medical attention to higher centers worldwide. These are interhospital transfers of critical patients using the available air infrastructure.
Most individuals with mild to moderate medical or surgical conditions are able to travel safely in a normal cabin seat with some assistance from the airline in the form of wheelchair and oxygen in case of emergency.[2] Some patients need either a stretcher in a commercial scheduled flight or a smaller dedicated chartered flight with all medical equipment and medical staff experienced to handle the situation. This may include continuous oxygen supply, airway management, cardiac monitoring, and interventions. Many countries where large areas are served by a few tertiary care centers have very efficient air medical transportation services, e.g., Australia, South Africa. This facility is poorly developed in India.
On case basis, the cost of air medical transportation may seem expensive when compared to ground transportation and even in comparison to the actual cost of treatment. On the contrary, studies show it is cost effective due to the decrease in time to treatment,[3] survival benefits,[4] and quality of life years added.[5] Over the past decade, wide availability of air ambulance services has brought a reduction in mortality and morbidity in India.[6]
Ours is the largest private multi super specialty hospital in India with patients transported from all over India and the world. Some of these patients are in serious medical condition and require urgent transportation and life-saving intervention by our dedicated air transportation team.
We present our experience based on 4 years of activity with the domestic and international interhospital air transport. This is the first of its kind audit in India and gives an insight into the profile, interventions and the present scenario of air medical transport in India.
Material and Methods
This is a retrospective analysis of all air medical transportations undertaken by the hospital from January 2010 to January 2014. Predetermined demographic and variable parameters were accessed from medical records of the hospital after due clearance from hospital authorities and fed into an Excel sheet for analysis. The primary underlying cause identified was recorded as the underlying indication for transportation. The causes were grouped together under the organ system for ease of interpretation.
Derived data are presented as mean ± standard deviation and percentage.
Evacuation time was defined as time from actual possession of the patient at the transferee hospital to handing over to primary admitting team at the transferred hospital.
It is important to note that all transportations were carried out by our team and subsequently admitted to our hospital, after a request for the same was received from the next of kin or legal guardian. Fixed wing aircraft were used in all transportations.
Aircraft
Fixed wing small aircraft available to us as air ambulance included 2 single propeller engine (Pilatus 12 NG, Pilatus Aircrafts Ltd., Switzerland) and 1 double propeller engine aircraft (King Air B 200, Beechcraft Corporation, USA) in a 4 seat and 1 stretcher configuration [Figure 1]. They can accommodate 2 doctors, 1 nurse, 1 accompanying person and the patient on a stretcher. These small unscheduled flights can be arranged on short notice, and can land and take off from small airstrips.
Figure 1.
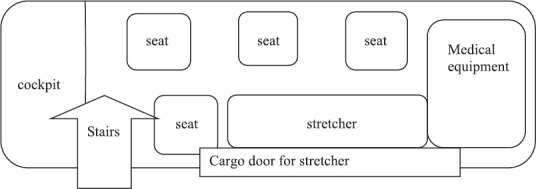
Customized arrangement of a 6 seater chartered aircraft for medical transport
Commercial flights are the routine scheduled operations of the airlines between airports. Most aircrafts can have seats customized to accommodate a stretcher on a prior request and approval by the airlines.
Equipment
Standard equipment for all medical transport includes airway management devices (laryngoscope, endotracheal tubes, tracheostomy tubes etc.), patient monitors, vascular access devices, and adequate number of oxygen cylinders. Vacuum stabilizing mattresses (Ferno (UK) Limited, West Yorkshire, UK) filled with small polyvinyl granules that adapt to shape of the supine patient to prevent undesirable and dangerous movement of the patient are used to transport critical patients, especially trauma victims. Intra-aortic balloon pump (IABP), cardiac pacing device, and fracture stabilizers (cervical collar, Thomas splint etc.) are included depending on the requirement. Spare dry nonspilling batteries are carried along as there may be no charging facility on aircraft.
As per aviation standards, all equipment are compact, portable, and noninterfering with radio communication. Equipment check for safety and integrity is done more frequently as they are more prone to wear and damage.
Staffing
Medical staff included 1 to 2 doctors and a nurse depending on the criticality of the case. Around 50 doctors from specialties including anesthesia and critical care, cardiology, cardiac surgery, emergency medicine, pediatrics have been trained to handle logistic and administrative issues related to air medical transport in addition to handling emergency situations. The choice of accompanying doctor depends on the specific case. The challenge in most air ambulances is constraint of space, constantly moving cabin and stressful working conditions. The main focus is thus to select highly motivated staff and training them to cope with stress in the small cabin of the aircraft with limited resources.
Procedure of air medical transport
All medical transports are under direct supervision of the Chairman, critical care and trauma of our institute. Request for transport of patients to the hospital is usually received by the hospital call center which is directed to the operations manager who acts as the coordinator between all concerned. He takes situation from the doctor where the patient is admitted, alerts the admitting specialty of our hospital, checks for availability of aircraft, applies for clearances from airport authorities and assembles the team of flight medical staff for preparations accordingly. The team is dispatched to the airport after affirmation from all concerned.
Stretcher in a routine scheduled commercial airline including international flights is available on request to the concerned airline and is subject to availability of required number of seats. The usual procedure is to get approval from the airline appointed doctor on the prescribed “Medif form” available with the airline office at least 2-3 days in advance.[2] Different aircraft need to assemble a fixed stretcher on 6-9 folded seats usually at the rear end of the aircraft with a curtain around it and an oxygen cylinder underneath. The accompanying staff is usually one doctor and one nurse. All equipment and patient responsibility have to be borne by the accompanying doctor. Visa for international transfers can be issued on an emergency basis by placing a request to the concerned embassy by the medical team.
The transport team, the patient's family and the operations manager remain in constant touch and appraise each other of the patient's condition and his/her further requirement all the time till the patient is handed over to the admitting team.
Patients are received at the transferee hospital where the first assessment is done, and any interventions necessary for safe transport are performed. Informed consent is taken, and family members are apprised of the condition.
The medical transport is complete only when the patient is handed over to admitting specialty and the family briefed.
Results
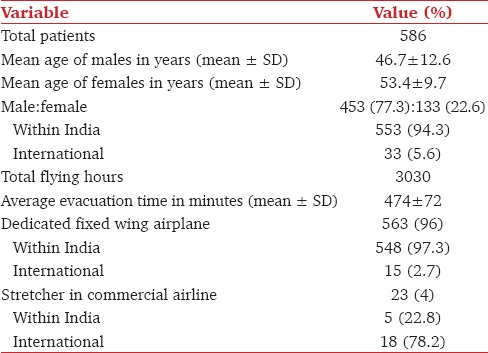
Over the 4-year period, 586 patients were air transported to our hospital with a total 3030 flying hours and a mean evacuation time of 474 ± 72 min.
Patient demographics and mission details are presented in Table 1. Maximum evacuation time within India was 430 min (Imphal, Manipur) and from an international location to our hospital was 1560 min (San Francisco, USA). International transfers included USA, Europe, Africa, Middle East Asia, Afghanistan, Pakistan, Nepal and South East Asia.
Table 1.
Demographics
The primary cause most commonly identified or diagnosed in 210 (35.8%) patients at initial admission center was of cardiovascular origin. These included angina and myocardial infarction, cardiac failure, valvular and congenital heart disease. Central nervous system disease including head injury and stroke in 120 (20.4%) was the second most common indication [Table 2].
Table 2.
Primary identified etiology

Five patients were intubated on board by the anesthetist/critical care physician. The indication for tracheal intubation was cardiorespiratory arrest in 2 and inability to maintain oxygen saturation with noninvasive ventilation in 4 patients. One endotracheal tube change for cuff malfunction and 5 tube depth change were needed for optimal ventilation. 156 patients (26.6%) were already intubated at the hospital of origin.
Four patients needed cardio pulmonary resuscitation (CPR) during transportation out of which 2 died. One of the patients was a 72-year-old male with recent myocardial infarction on mechanical ventilation and nitroglycerine infusion. The other was a 56 year old male with multiorgan failure involving cardiovascular, respiratory and renal system on ventilator and vasopressor support and history of 10 days in hospital.
Inotropic and vasopressor infusion was used in 109 (18.6%) patients for a total of 1133 h. This included 50 (45.8%) patients on a single drug. Most commonly used single agent was noradrenaline infusion in 32 patients. 59 (54.2%) patients were on more than 2 inotropes. The most common inotropic combination used at the receiving hospital was dopamine and noradrenaline in 25 patients.
Intra-aortic balloon pump was used in 7 patients, all of which were inserted prior to transport by the cardiac surgeon from our team. 14 invasive monitoring lines were placed during transport including 8 central venous catheters and 6 arterial lines. 96 (16.4%) patients already had invasive lines in place (78 CVCs and 36 arterial catheters) at receiving hospitals.
Overall complication rate including minor event was 31 (5.3%). All handovers to the admitting team were reported to be in satisfactory condition.
Discussion
Prehospital and transportation data analysis has been done earlier, and it gives an insight into the demographics and travel patterns of the particular countries.[7,8] There are a few commentaries on the uniqueness of air medical transport scenario in India.[9]
Cardiovascular diseases remain the most common cause for the need of transfer to a tertiary center. This may be partly due to uneven distribution of tertiary cardiac centers in India and mainly due to an increase in incidence as well as a decrease in age of cardiac diseases in India.[10] Essebag and Halabi also observed an increased frequency of medical transportation of cardiac patients due to medical, economical, and social patterns in Canada.[1] The same holds true for India.
More males are transported for treatment to another facility. This may be attributed to the cultural, social, and economical dominance of males in the Indian society. Khera et al. pointed out that there is a gender bias in medical care in India.[11]
The main patient-related concerns when air transporting a critical patient are the low atmospheric pressure and gas expansion effects of altitude, patient and family anxiety; and movement related complications. Fixed wing propeller aircrafts fly at an altitude of 15,000-30,000 feet. Barometric pressure decreases from 760 mm Hg at sea level to 226 mm Hg at 30,000 feet. The aircraft cabin is pressurized to an equivalent pressures of 5000-8000 feet which corresponds to a PO2(inspired) of 107 mm Hg.[12] This PiO2 is easily tolerated by normal individuals but in critical patients with limited reserves, it causes hyperventilation and tachycardia with an increase in cardiac output. This may also alter the need of vasopressors and inotropes and can be particularly detrimental to patients with underlying respiratory or cardiac diseases.[13] In our experience, there was a need for CPR in 4 patients and 2 mortalities due to cardiac arrest. It is important to note that these were all previously sick patients in need of advanced care. The changes in the environment, however small could not be ignored and need further investigation.
Another effect of decreased atmospheric pressure is on gas expansion. All potential body spaces, especially middle ear, bowel and pathological body spaces like pneumoperitoneum, pneumocranium, pneumothorax are at risk of expansion at high altitudes and especially during rapid changes during rapid ascend and descent. Though we did not find any complication to any body cavity, there was an incidence of endotracheal tube cuff rupture which needed tube change by the accompanying anesthetist. This was reported just after take off and could be attributed to the gaseous expansion in the cuff.
The 6 endotracheal tube adjustments to optimize ventilation were needed due to the endobronchial migration of tube probably during patient transfers between beds. This was despite precautions including head stabilizers and vacuum body stabilizing stretchers.
The overall complication rate of 5.3% in our study is similar to 5-6% reported by Szem et al. in 1994.[14] This paper however evaluated interhospital road transport of patients. A review article by Waydhas reported a complication rate in the range of 6-70% during transfers rather than during actual transport.[15] Most common complications were disconnections of leads, intravenous tubing, and ventilator circuits. We can safely say that air transportation carries no more risk than ground transportation.
Ground transportation may seem cheaper than air transportation. Some emergencies are potentially life or limb threatening and require urgent care and speedy transport to an advanced care center. This has been made possible only by air medical transportation with proven benefits in survival.[3,4,5] Bruhn et al. created an economical model to compare the cost of air ambulance services and ground ambulance services. The annual budgetary cost of ground network was estimated at $3,804,000, and helicopter ambulance cost was estimated at $16,865,000. Per patient cost worked out to be $4,475 and $2,811, respectively. They concluded that the commonly held notion that condemns helicopters as an excessively expensive technology as incorrect.[16] Only two clinical situations justify the choice of air over ground interhospital transportation of sick patients. First, nonavailability of the required diagnostic and therapeutic facility at the present facility and second when factors such as time and distance render ground transportation nonfeasible.[17]
Over the past decade, many factors have contributed to the increase in interhospital air medical transport in India. There is an easier availability of small aircraft for civil use that can be customized as ambulances. Almost all districts in India have access to either a civilian or military airstrip which can be used for air ambulance services on request to competent authorities.[18] There is an inequitable distribution of tertiary care hospitals in India.[19] Further, access to internet has made it easy to locate and communicate with specialty centers worldwide.
Even after all the above catalysts, the limiting factor in the speedy air transport of critical patients has been the time required for the customization of the aircraft and shortage of specialized equipment like IABP and extra corporeal membrane oxygenation and trained personnel.
The condition of the air transported patients is the same as in any other critical area of the hospital and thus necessitates the same monitoring and interventions in a totally different environment.[20] This requires specialized equipment and trained staff. At present, there is no air medical training facility for civilians in India.[21] Norton pointed that there is a need for air medical transport curriculum for emergency medical residents.[22] We feel there is a need of a structured accreditation policy and training program to bring accountability to the mushrooming air ambulance business in India. There is a need for trained medical staff, equipment, and dedicated aircraft to fill in the gap created by the inequitable distribution of hospitals in India.
Conclusion
Patients who are transported with a medical escort may need invasive and advanced monitoring and interventions as in any critical care area of the hospital. Cardiovascular diseases remain the most common reason for interhospital air medical transport. Complication rate during interhospital air transportation of critical patients is similar to ground transportation.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Essebag V, Halabi AR, Churchill-Smith M, Lutchmedial S. Air medical transport of cardiac patients. Chest. 2003;124:1937–45. doi: 10.1378/chest.124.5.1937. [DOI] [PubMed] [Google Scholar]
- 2.International Air Transport Association. Medical Manual. c2013. [Last accessed on 2014 Feb 02]. www.iata.org . Available from: http://www.iata.org/whatwedo/safety/health/Documents/medical-manual-2013.pdf .
- 3.Phillips M, Arthur AO, Chandwaney R, Hatfield J, Brown B, Pogue K, et al. Helicopter transport effectiveness of patients for primary percutaneous coronary intervention. Air Med J. 2013;32:144–52. doi: 10.1016/j.amj.2012.08.007. [DOI] [PubMed] [Google Scholar]
- 4.Gearhart PA, Wuerz R, Localio AR. Cost-effectiveness analysis of helicopter EMS for trauma patients. Ann Emerg Med. 1997;30:500–6. doi: 10.1016/s0196-0644(97)70010-6. [DOI] [PubMed] [Google Scholar]
- 5.Silbergleit R, Scott PA, Lowell MJ, Silbergleit R. Cost-effectiveness of helicopter transport of stroke patients for thrombolysis. Acad Emerg Med. 2003;10:966–72. doi: 10.1197/s1069-6563(03)00316-6. [DOI] [PubMed] [Google Scholar]
- 6.Mehra A. Air ambulance services in India. J Postgrad Med. 2000;46:314–7. [PubMed] [Google Scholar]
- 7.Judi C, Frank T. A 10-year analysis of 214 HEMS backcountry hoist rescues. Air Med J. 2012;32:64–5. doi: 10.1016/j.amj.2012.10.012. [DOI] [PubMed] [Google Scholar]
- 8.Wegmann F, Kromann-Andersen B, Staehr Johansen T, Jessen K. Sixteen years with the Danish search and rescue helicopter service. Aviat Space Environ Med. 1990;61:436–9. [PubMed] [Google Scholar]
- 9.Chawla NP, Chawla K. Against all odds: Air medical transport in India. Air Med J. 1998;17:146–8. doi: 10.1016/s1067-991x(98)90038-4. [DOI] [PubMed] [Google Scholar]
- 10.Ajay VS, Prabhakaran D. Coronary heart disease in Indians: Implications of the INTERHEART study. Indian J Med Res. 2010;132:561–6. doi: 10.4103/0971-5916.73396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Khera R, Jain S, Lodha R, Ramakrishnan S. Gender bias in child care and child health: Global patterns. Arch Dis Child. 2014;99:369–74. doi: 10.1136/archdischild-2013-303889. [DOI] [PubMed] [Google Scholar]
- 12.American Medical Association. Medical aspects of transportation aboard commertial aircraft. J Am Med Assoc. 1982;247:1007–11. [Google Scholar]
- 13.Cong H. Air travel and oxygen therapy in cardiopulmonary disorders. Chest. 1992;101:463–76. doi: 10.1378/chest.101.4.1104. [DOI] [PubMed] [Google Scholar]
- 14.Szem J, Hydro LJ, Fisher E, Kapur S, Klemperer J, John B, et al. High risk interhospital transport of critically ill patients: Safety and outcome of necessary “road trip”. Crit Care Med. 1995;23:1660–6. doi: 10.1097/00003246-199510000-00009. [DOI] [PubMed] [Google Scholar]
- 15.Waydhas C. Equipment review: Interhospital transport of critical ill patients. Crit Care. 1999;3:83–9. [Google Scholar]
- 16.Bruhn JD, Williams KA, Aghababian R. True costs of air medical vs. ground ambulance systems. Air Med J. 1993;12:262–8. doi: 10.1016/S1067-991X(05)80311-6. [DOI] [PubMed] [Google Scholar]
- 17.American College of Emergency Physicians [www.acep.org. ]. American College of Emergency Physicians and National Association of EMS Physicians. Guidelines for Air Medical Dispatch, Policy Resource and Education Paper. c2006. [Last accessed on 2014 Dec 25]. Available from: https://www.acep.org/uploadedfiles/ACEP/Practice_Resources/issues_by_category/Emergency_Medical_GuidelinesForAirMedDisp.pdf .
- 18.Airports Authority of India [www.aai.aero. ] New Delhi List of Airports. [Last accessed on 2014 Feb 02]. Available from: http://www.aai.aero/public_notices/aaisite_test/policy.jsp#4 .
- 19.Lackner CK, Stolpe E. New order of things: An international overview of air medical transport. Air Med J. 1998;17:142–5. doi: 10.1016/s1067-991x(98)90037-2. [DOI] [PubMed] [Google Scholar]
- 20.Fromm RE, Jr, Varon J. Critical care transport. Crit Care Clin. 2000;16:695–705. doi: 10.1016/s0749-0704(05)70141-x. [DOI] [PubMed] [Google Scholar]
- 21.Aggarwal NN, Aggarwal S. Transfer of sick children by air. Indian Pediatr. 2000;37:853–71. [PubMed] [Google Scholar]
- 22.Norton EG. Model curriculum in air medical transport for emergency medicine residencies. Ann Emerg Med. 1991;20:431–2. doi: 10.1016/s0196-0644(05)81671-3. [DOI] [PubMed] [Google Scholar]


