Abstract
Introduction:
In an aging population, new strategies are required to identify individuals at risk of adverse health outcomes. Frailty syndrome is related to negative health events. This increased risk may be used to identify individuals in which interventions can delay the onset of physical and functional complications. The aim of the study was to determine the relationship between the onset of frailty and the beginning of functional disability.
Materials and Methods:
This was a cross-sectional observational study with consecutive sampling to analyze 146 patients aged seventy and older who come to the primary care center. The level of frailty was registered according to fatigue, resistance, ambulation, illnesses, and loss of weight scale. Disability for Instrumental Activities of Daily Live dependency, comorbidity, and social risk factors was registered too.
Results:
The prevalence of frailty and prefrailty was 17.8% and 39%, respectively, and were associated with age, level of disability, and the presence of gastrointestinal disease. Prefrail patients had initial levels of dependency, while those who were not frail were mostly independent.
Conclusion:
Frailty syndrome is easily detectable. The intermediate stage known as prefrailty is related to the start of the functional disability. The syndrome screening identifies individuals at risk in whom we can potentially intervene to delay the onset of the syndrome and delay functional disability. Control of comorbidity in frail patients must be studied. Screening age could be set in patients between 75 and 81 years old.
Key words: Disability, elderly, frailty, primary care
INTRODUCTION
The aging of a population leads to a higher incidence and prevalence of various health and social problems related to age, as well as the increased rates of dependency, comorbidity, and economic and social costs associated to those entities.[1] It is necessary to identify individuals at risk in order to delay the onset of health problems and the economic problems related to aging.
Frailty appears as a clinical syndrome associated with greater vulnerability of the individual to adverse health outcomes, a higher level of disability, and increased mortality. It is characterized by reduced resistance, strength, and decreased physiological functions.[2] Sarcopenia is considered the factor that initiates the pathophysiological cycle of frailty, generating structural, and metabolic changes through insulin resistance, together with the tendency to inflammatory conditions and an increased cardiovascular risk.[3,4]
The lack of a definition of frailty common to different authors makes it difficult to calculate the real prevalence of the syndrome,[5] which is said to be around 10.7% of the elderly, with 41.6% in the prefrailty situation.[6]
Fatigue, resistance, ambulation, illnesses, and loss of weight (FRAIL) scale may be used to detect frailty. This scale is easily applicable within the comprehensive geriatric assessment in primary care.[2] It establishes three frailty levels according to the responses obtained to five questions on comorbidity, fatigue, resistance, aerobic capacity, and unintended weight loss. Each item is scored with one point. Patients with 0 points are considered nonfrail, with 1 or 2 points for prefrail, and frail are those with 3 or more points.[7]
Frail people have less capacity for daily living activities than nonfrail patients, but this relation is not well defined since it is not known if these entities are time-related.[8] The possibility of using frailty as a screening method to detect people at risk of being unable to cope with their daily life activities might be useful to establish interventions to prevent or delay this loss.[9]
The objective of this study was to describe the functional capacities of the elderly in each frailty state according to FRAIL scale. A time-related relationship between these entities may indicate when to start rehabilitation measures by detecting the frailty level.
MATERIALS AND METHODS
A descriptive observational study was accomplished, taking as target population 70-year-olds or older patients assigned to a single primary care center. The chosen Primary Care Center was located in an urban area of the Eastern part of the city of Madrid, of a low-medium socioeconomic status. Patients who did not sign the informed consent, were institutionalized and/or had language barriers or cognitive impairment and could not understand the information provided and required were excluded.
Based on an estimated prevalence of frailty of 10.7% in previous studies with similar tools, in a similar population, the calculated sample size was 145 subjects from a reference population of 3806 patients, (5% precision, confidence interval (CI) - 95%). These individuals were selected using consecutive not randomized sampling during the months of October and November 2014 until the sample was complete.
Subjects selected were verbally informed about the study features and were asked to complete the informed consent in writing by a letter. This enabled the investigators to consult their medical records and proceed with a personal interview.
The following variables were recorded: Sex, age (grouped into 5-year groups), frailty level according to FRAIL scale,[7] comorbidities, and pluripathology following the instructions for development of clinical guidelines of the Spanish Primary Care Societies (illnesses are classified in eight groups, depending on the organ or system affected),[10] instrumental daily life activities capacity through Lawton-Brody scale,[11] and the social risk following the GijÓn social risk scale adapted to the Spanish population.[11]
A dissociated database was created, ensuring that the processing of data was anonymous. Frequencies and 95% CI were calculated for qualitative variables. Age was also measured as a continuous quantitative variable, calculating the median and standard deviation. Bivariate analysis was performed with Chi-square test for measuring the association between variables, taking frailty as the dependent variable, and using the Pearson's regression ratio to quantify the association power if any. A logistic regression was performed in order to reject those variables that worked as confounding factors. SPSS 22.0 (SPSS 22.0, copyright by IBM, USA) program was used for the statistical analysis.
Ethical issues were considered, respecting personal privacy, obtaining patients consent for the recruitment and the use of the data only for the purpose of this study. This investigation was approved by the Investigation Committee of the East Health Assistance Area of Madrid.
RESULTS
Classified as frail was 17.81% (CI 12–24%) of the population and 39.72% (CI 32–48%) as prefrail. There were no differences in the proportion of frailty by sex. Frailty was more common in the older subgroup as shown in Figure 1. The median age of frail individuals was 84 years with a standard deviation of 1-year. The median age of prefrail individuals was 81, with a standard deviation of 1-year. The youngest prefrail person was 75 years old.
Figure 1.
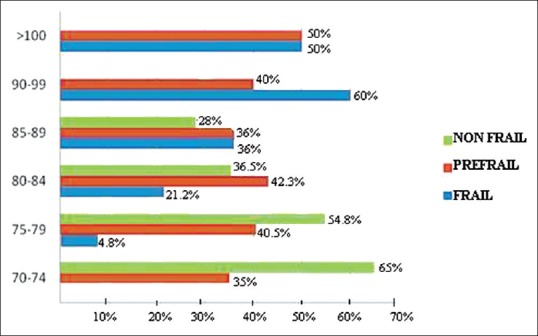
Prevalence of frailty by age group
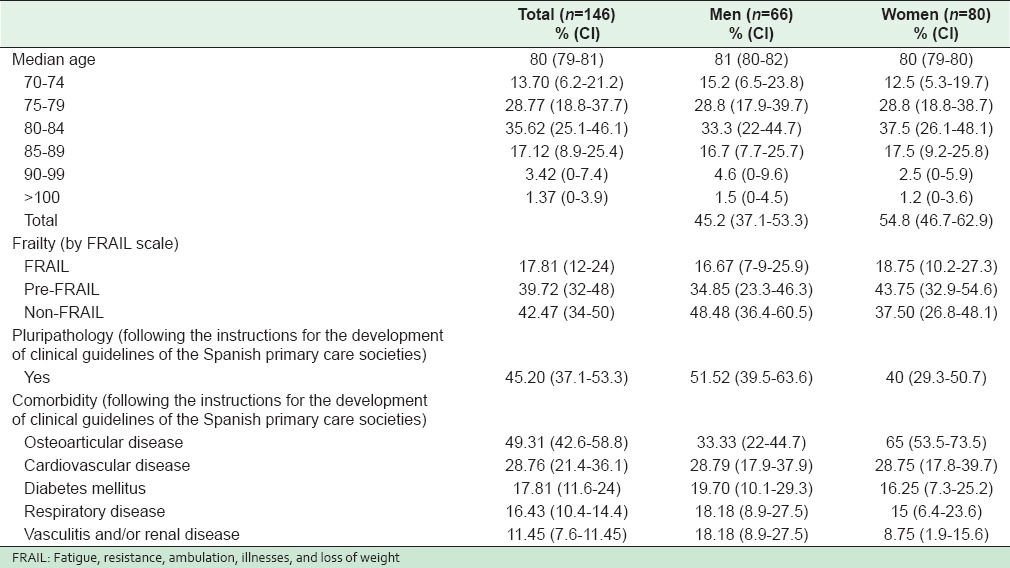
Of the population, 45.20% were male and 54.8% were female. The distribution of age groups and variable frequencies by sex is shown in Table 1.
Table 1.
Percentage distribution and 95% CI for sociodemographic characteristics of the study population by gender
Total disability for instrumental daily living activities comprised 3.42% (CI 0.5-6.4%) of the population, severe 8.22% (CI 3.9-12.7%), moderate 15.07% (CI 9.8-20.9%), and mild 27.4% (CI 20.3-34.6%). There was no limitation in those activities for 45.20% (37.1-53.3%) of the population.
There were no differences in levels of dependency by sex. The level of disability was greater in the higher age subgroups. A marked increase in the level of dependence occurred when the nonfrail and prefrail groups were compared as shown in Figure 2.
Figure 2.
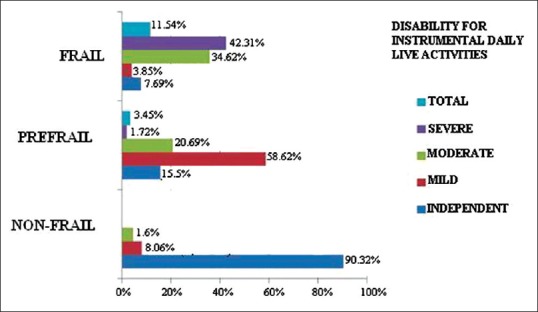
Distribution of dissability for Instrumental Activities of Daily Live by different levels of frailty
Of the total sample, 0.68% (CI 0.2-2.02%) presented a high social risk, 23.29% (CI 16.4-30.1%) moderate, and for 76.03% (CI 69.1-82.9%) there was no risk at all. There were no significant differences in social risk by sex.
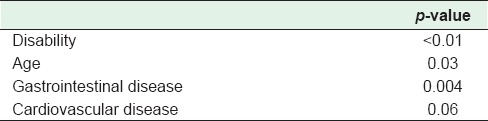
The bivariate analysis between frailty and the different variables showed p values [Table 2] which allowed the establishment of a possible association between the frailty and the level of dependence in instrumental activities of daily living, the presence of comorbidity such as cardiovascular, musculoskeletal and digestive diseases, and age. All these variables besides sex were tested to a logistic regression. The only association found was between frailty and disability, age dependency and diseases of the digestive system [Table 3].
Table 2.
P-values for association between frailty (dependent variable) and the rest of the study variables in a bivariate analysis
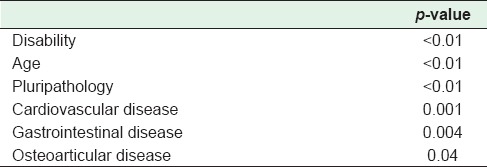
Table 3.
P-values for association between frailty (dependent variable) and variables previously associated in the bivariate analysis within a multivariate model
DISCUSSION
The prevalence of frailty similar to the previous studies with similar scales and population (5.8–27.3%) was found although the criteria for the diagnosis of this entity are not the same in all of the literature. Further research in this field must be done to establish common criteria so that the real impact of this syndrome can be described. Prefrailty prevalence was also within the limits of previous publications (34.6–50.9%).[12] Although we have used a different methodology in sampling, the use of the same scales makes the comparison with other studies plausible. The results are applied to the population studied, but further research will help us to compare the differences with the general population. It is important to attend primary care to detect frailty properly as certain studies have demonstrated differences in the way family physicians and geriatricians detect this entity.[13]
In a descriptive analysis, frailty has been more frequent in relative terms in men than in women although they have presented greater relative frequency of prefrailty. No objective statistical association between the presence of frailty and sex was found.[14] Our findings are in agreement with those studies that indicate that frailty is more common in women and that they persist in this condition longer than men. This may be due to the attendance of frail women at a different health-care center from the rest of population, delegating some activities to other family members.
As already shown in the literature, the presence of frailty increases with age.[15] The ideal time for screening frailty can be set between 75 and 81 although the sample size limits the interpretation of results, and other studies have shown that there may be younger frail individuals.[16]
The transition from a normal situation to prefrailty status entails deterioration in instrumental activities of daily living. This relationship has been described in other articles, but the temporal association between the onset of prefrailty and the start of the loss of functional capacities has not been recounted in the consulted literature. For example, Woo et al. indicate that frailty can be used as a method that allows targeted interventions to retard disability.[17] Mijnarends et al. reflected on the relationship between frailty and sarcopenia, recognizing the similarities between the Frail scale and Fried's frailty phenotype, and encouraged the study of the relationship of these entities with a disability.[18]
Frailty syndrome is related to dependence, age, and digestive illnesses. Malnutrition may be behind this latest relationship, influencing pathophysiological changes associated with frailty. Cardiovascular diseases showed no significant relationship with frailty, but this result may change with further research, in accordance with previous literature and remove the limitations of this investigation.
Detection of frailty syndrome, especially its intermediate stage or prefrailty status, identifies individuals with greater risk of disease and negative prognosis. This condition can assist in making clinical decisions based on the timing of benefits of the different diagnostic and therapeutic procedures. Establishment of the relationship between frailty and functional dependency as well as the identification of those individuals more likely to require the use of social resources later[19] are vital so that social and health policies[9] can be determined.
It is necessary to establish the temporal relationship of the events associated with the onset of frailty, such as the time of evolution from the prefrail status to frailty, or the prognosis of frail and prefrail patients. Studying the relationship between frailty and different pathology groups can strengthen the understanding of the pathophysiology of the syndrome in order to find the possible ways of prevention and treatment. It is possible that intervention in the gastrointestinal or cardiovascular field can delay the development of the syndrome, relying in each case on their pathophysiology.
This study has some limitations. It obtained the association between variables but not a cause-effect relationship. However, the results may be used to develop scenarios and proposals for improvement. Patients included in the study did not cover the entire population spectrum because of the sampling. Using charts and data collection in a medical environment can produce biases that have to be borne in mind when the results are interpreted.
CONCLUSION
Detecting frailty in the early stage called prefrailty may be useful to identify patients at risk of losing their functional capacities. This relationship is important not only to maintain the best health level in the population, but also for the organizational implications that can be developed from it. The identification of prefrail individuals may be useful in the implementation of health and social programs that prevent the development of frailty and disability, and its economic and social costs. Further research might be done to describe the effects of different interventions on prefrail patients.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
This study has not received any funding support. The authors declare that they have no financial or personal relationship which may have inappropriately influenced me in writing this paper. Thanks to all the doctors and nurses that work in the Alpes Primary Care Centre, Madrid, where this study took place.
REFERENCES
- 1.De Lepeleire J, Iliffe S, Mann E, Degryse JM. Frailty: An emerging concept for general practice. Br J Gen Pract. 2009;59:e177–82. doi: 10.3399/bjgp09X420653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Morley JE, Vellas B, van Kan GA, Anker SD, Bauer JM, Bernabei R, et al. Frailty consensus: A call to action. J Am Med Dir Assoc. 2013;14:392–7. doi: 10.1016/j.jamda.2013.03.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Yao X, Li H, Leng SX. Inflammation and immune system alterations in frailty. Clin Geriatr Med. 2011;27:79–87. doi: 10.1016/j.cger.2010.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Krentz AJ, Viljoen A, Sinclair A. Insulin resistance: A risk marker for disease and disability in the older person. Diabet Med. 2013;30:535–48. doi: 10.1111/dme.12063. [DOI] [PubMed] [Google Scholar]
- 5.Romero-Ortuno R, Walsh CD, Lawlor BA, Kenny RA. A frailty instrument for primary care: Findings from the Survey of Health, Ageing and Retirement in Europe (SHARE) BMC Geriatr. 2010;10:57. doi: 10.1186/1471-2318-10-57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Collard RM, Boter H, Schoevers RA, Oude Voshaar RC. Prevalence of frailty in community-dwelling older persons: A systematic review. J Am Geriatr Soc. 2012;60:1487–92. doi: 10.1111/j.1532-5415.2012.04054.x. [DOI] [PubMed] [Google Scholar]
- 7.Morley JE, Malmstrom TK, Miller DK. A simple frailty questionnaire (FRAIL) predicts outcomes in middle aged African Americans. J Nutr Health Aging. 2012;16:601–8. doi: 10.1007/s12603-012-0084-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Roppolo M, Mulasso A, Gobbens RJ, Mosso CO, Rabaglietti E. A comparison between uni- and multidimensional frailty measures: Prevalence, functional status, and relationships with disability. Clin Interv Aging. 2015;10:1669–78. doi: 10.2147/CIA.S92328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Acosta Benito MÁ. Failty in the elderly: From the síndrome to the social, health and legal plannification. Rev Esp Med Legal. 2015;41:58–64. [Google Scholar]
- 10.Alonso Coello P, Bernabeu WiĴ el M, Casariego Vales E, Rico Blázquez M, Rotaeche del Campo R, Sánchez Gómez S. Development of clinical practice guidelines in patients with comorbidity and pluripathology. SEMFYC/SEMI/FAECAP. 2013 Apr [Google Scholar]
- 11.Sanjoaquín Romero AC, Fernández Arín E, Mesa Lampré MP, García-Arilla Calvo E. Comprehensive geriatric assessment. Treaty of Geriatrics for Residents. Spanish Society of Geriatrics and Gerontology. 2006 [Google Scholar]
- 12.Papiol M, Serra-Prat M, Vico J, Jerez N, Salvador N, Garcia M, et al. Poor muscle strength and low physical activity are the most prevalent frailty components in community-dwelling older adults. J Aging Phys Act. 2015 doi: 10.1123/japa.2015-0114. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 13.van Kempen JA, Melis RJ, Perry M, Schers HJ, Rikkert MG. Diagnosis of frailty after a comprehensive geriatric assessment: Differences between family physicians and geriatricians. J Am Board Fam Med. 2015;28:240–8. doi: 10.3122/jabfm.2015.02.130081. [DOI] [PubMed] [Google Scholar]
- 14.Gobbens RJ, Luijkx KG, Wijnen-Sponselee MT, Schols JM. Toward a conceptual definition of frail community dwelling older people. Nurs Outlook. 2010;58:76–86. doi: 10.1016/j.outlook.2009.09.005. [DOI] [PubMed] [Google Scholar]
- 15.Al-Kuwaiti SJ, Aziz F, Blair I. Frailty in community-dwelling older people in Abu Dhabi, United Arab Emirates: A cross-sectional study. Front Public Health. 2015;3:248. doi: 10.3389/fpubh.2015.00248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Alcalá MV. Prevalence of frailty in an urban population of over 65 years and their relationship with comorbidity and disability. Aten Primaria. 2010;42:520–7. doi: 10.1016/j.aprim.2009.09.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Woo J, Yu R, Wong M, Yeung F, Wong M, Lum C. Frailty screening in the community using the FRAIL scale. J Am Med Dir Assoc. 2015;16:412–9. doi: 10.1016/j.jamda.2015.01.087. [DOI] [PubMed] [Google Scholar]
- 18.Mijnarends DM, Schols JM, Meijers JM, Tan FE, Verlaan S, Luiking YC, et al. Instruments to assess sarcopenia and physical frailty in older people living in a community (care) setting: Similarities and discrepancies. J Am Med Dir Assoc. 2015;16:301–8. doi: 10.1016/j.jamda.2014.11.011. [DOI] [PubMed] [Google Scholar]
- 19.Abizanda P, Romero L, Sánchez-Jurado PM, Martínez-Reig M, Alfonso-Silguero SA, Rodríguez-Mañas L. Age, frailty, disability, institutionalization, multimorbidity or comorbidity. Which are the main targets in older adults? J Nutr Health Aging. 2014;18:622–7. doi: 10.1007/s12603-014-0033-3. [DOI] [PubMed] [Google Scholar]


