Abstract
Background:
Discharge instructions are vital in postemergency patient care to help the caregiver understand the diagnosis and identify symptoms which require prompt readmission. In general, oral or written instructions are provided on discharge. However, there is a dearth of information on the efficacy of discharge instructions provided by physicians in KSA.
Objectives:
To evaluate the efficacy of discharge instructions for postpediatrics emergency visit.
Materials and Methods:
This observational cross-sectional survey conducted in the Department of Paediatric Emergency at King Abdul Aziz Medical City, Riyadh, KSA, included 173 literate adult caregivers who had given their consent. Those who had been on admission earlier and been discharged from the emergency department were excluded. Demographic data and variables like knowledge of medicine and treatment follow-up were collected using a structured questionnaire and analyzed using SPSS version 16.
Results:
Verbal only, written only, or both verbal and written discharge instructions were provided. Written and verbal instructions, when provided together, were the most effective modes of communication with caregivers. The majority of the respondents were unaware of the follow-up plan (64.16%), unable to identify problems that would necessitate a follow-up (58.96%), and unable to identify the signs and symptoms that would require a revisit (62.43%) irrespective of the mode of instruction. However, more attention is necessary because of the 34.68% of the subjects who left the hospital without discharge instructions.
Conclusions:
Instructions given both verbally and in writing were observed to be more effective than verbal only or written only. The effectiveness of discharge instructions was highly influenced by the level of education of the caregivers. Improved caregiver friendly methods of communication from the pediatric emergency health-care team are necessary for the delivery of discharge instructions.
Key words: Caregiver, knowledge of medication and follow-up, patient discharge instructions, pediatric emergency
INTRODUCTION
Discharge instructions are guidelines that patients have to follow after discharge to deal with any remaining illnesses that need to be taken care of personally by the patient, home care attendants, and other clinicians on an outpatient basis. For emergency pediatric patients, discharge instructions are given to the parents and/or the caregivers usually by a nurse or clinician in simple language. In this regard, it is important to deliver detailed discharge instructions to the caregivers who present to the emergency department (ED) with their children in order to reduce hospital readmission and to improve patient care and safety. Preferably, caregivers should leave the ED with the necessary knowledge and skills to effectively manage their child's care at home.
Earlier studies found that 87% of the children visiting the ED are discharged to their residence.[1] However, it is a challenge for the patients and family members to memorize and understand hospital discharge instructions because of the physical and emotional discomfort at the time of discharge and/or they may be in a hurry to leave and are therefore not much interested in the instructions. Low literacy and/or health literacy further affect their compliance to the discharge instructions.[2]
Poor understanding of discharge instructions is influenced by many factors[3] such as the language barrier between the caregiver and the patients[4] and emotional disturbances as a result of anxiety about the outcome of the disease.[5] Other vital factors that may influence the quality of discharge instructions in the ED are overcrowding, waiting time, and limited time allocated for issuing discharge instructions.[6]
Discharge instructions can be classified as verbal and written or as handwritten instruction notes, preformatted instruction sheet, and information sheet.[7] Usually, clinicians depend on oral/verbal and/or written discharge instructions. Standardized written instructions given to parents upon ED discharge can improve knowledge and satisfaction with care.[8] However, verbal discharge instructions cannot be replaced by written instructions. Verbal discharge instructions is a critical component of patient care and provides a good opportunity for health-care professionals to communicate and interact with patients and their families.[1] Communication between the ED providers and parents should effectively complete three tasks during the discharge process: Communicate important information, verify comprehension, and adapt the discharge instruction to address areas of misunderstanding.[9] For many caregivers, this is not the experience.
Emergency care often depends on the coordination and interaction between a number of professionals inside and outside the ED, and generally takes place in a compressed timeframe. The chaotic nature of the ED setting is also characterized by frequent interruptions of work-flow and the time intended for discharge communication can sometimes be appropriated or compressed to take care of more urgent activities[10,11] and the understanding of the discharge information is rarely considered.[12] The lack of standards and considerable variation in practice regarding the discharge instruction in EDs poses a quality and safety risk for children and parents/caregivers.
Globally, efforts focus on optimizing discharge instructions from the emergency room by using innovative methods such as online videos and mobile discharge instructions.[13,14] However, there is little in the literature on this, and further research is needed to evaluate the best means of delivering discharge instructions at the local level. This study was conducted in King Abdulaziz Medical City, a tertiary care teaching hospital in Riyadh, KSA, where 60,000 patients per year seek medical care in different specialties. Usually, the caregivers are provided with verbal and written discharge instructions. The hospital records indicate a very high percentage (20%) of readmissions because of low compliance of instructions for home care. The present study was, therefore, conducted to find out the efficacy of postemergency discharge instructions for patients from the Pediatric ED.
MATERIALS AND METHODS
This observational cross-sectional study was conducted in Paediatric ED of King Abdulaziz Medical City from July 25 to August 22, 2015. The respondents of the study included parents/caregivers of patients discharged from pediatric emergency.
During the period of study, about four hundred patients sought help from the Paediatric ED of King Abdulaziz Medical City. After fixing a margin of error of 5% at 95% level of confidence level, a sample of size 197 was arrived at by using Raosoft online sample size calculator. Respondents for the study were selected according to the selection criterion: Literate adults who had no earlier admission and discharge from the ED. Caregivers who were not willing to give consent were excluded from the study during sampling. Accordingly, 173 caregivers who fell within the selection criterion were chosen as the subjects for the study by using convenient sampling technique.
Efficacy of discharge instructions required qualitative data with respect to the demography of the respondents as well as the data on variables which might have an influence on the objectives of providing discharge instructions by the emergency health-care team. With this in mind, a structured questionnaire was formulated, reviewed, and edited after discussions with all the researchers. The final structured questionnaire with closed-ended questions was translated into Arabic. The questionnaire in Arabic and English were administered to the caregivers of the pediatric patients during their postemergency visit for follow-up. The collected data included demographic information of the caregiver as well as the details of discharge instructions with respect to the mode of instruction, and knowledge of the caregiver about medicines, signs and symptoms, and follow-up plan.
The data were scored and entered in Microsoft Excel (Microsoft Corp., Redmond, WA, USA). Incompatible data were recognized and edited. Simple descriptive statistics such as percentages and frequencies were used to describe demographic information, educational status of the caregiver and the caregiver's knowledge about medicines, signs and symptoms requiring medical assistance, and follow-up plan. Data analyses were performed by using SPSS version 16 (For windows, IBM SPSS statistics, IBM Corporation, Armonk, NY).
The study was approved by the Institutional Review Board of King Abdullah International Medical Research Centre, Riyadh, KSA.
RESULTS
Table 1 shows the age of the caregivers by gender. About 98% of the caregivers were 20-60 years of age. For female caregivers, the most common age group was 21-40 whereas more male caregivers were in 31-50 age group. More than half (53.74%) of the caregivers were females.
Table 1.
Demographic characteristic of the caregivers
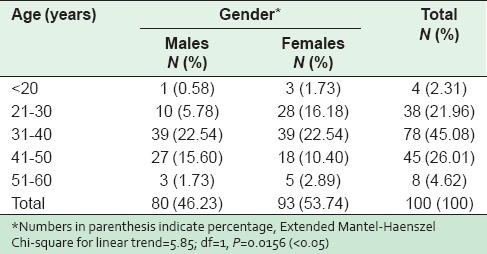
Of the female respondents, 49.13% were the mothers of the pediatric patients, while 4.61% were either relatives or informal caregivers as shown in Figure 1. The male caregivers were as follows: Fathers of the patients (43.35%) and male relatives (2.88%). Statistical analyses indicated a significant linear relationship between the age and gender of the caregiver (p = 0.0156). Majority (64.7%) of the caregivers had basic school education, whereas, 35.26% were university graduates or had higher degree; only 4.6% caregivers were literate.
Figure 1.
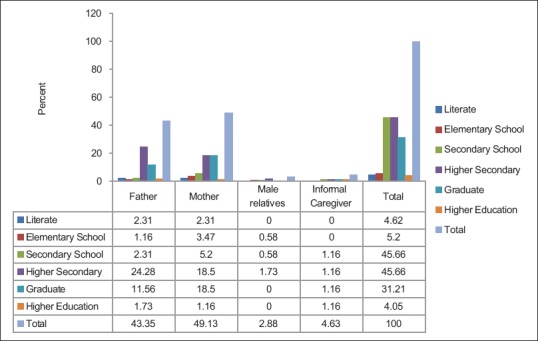
Frequency distribution of caregivers’ educational status and relationship to the patient
Yates Chi-square analysis indicated that there was no association between the educational level of the caregiver and his/her relationship with the patient (p = 0.9453).
On discharge, 54.91% of the subjects received verbal instructions, 3.47% received written instructions, and 6.36% were given both verbal and written instructions. About 34.68% of the patients and caregivers left the hospital without receiving any type of discharge instructions [Figure 2].
Figure 2.
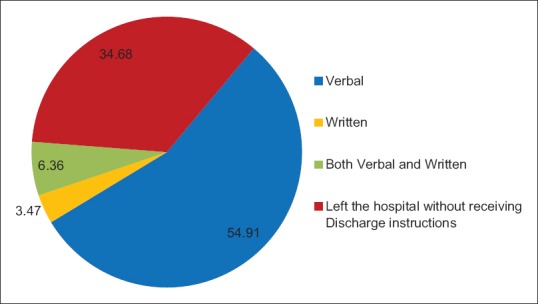
Distribution of mode of discharge instruction
Table 2 shows the effect that various types of discharge instructions had on the knowledge of medicines. A high percentage of caregivers who got both verbal and written discharge instructions exhibited a good knowledge of medications in terms of the name of the medication (91.67%), dose (100%), the frequency of medication (91.67%), and possible side effects (83.33%). It was observed that the respondents who got written discharge (83.33%) instructions were more aware of the duration of medication than other variables.
Table 2.
Effect of mode of instruction on the knowledge about medicines

On the whole, 55.49% of respondents knew the name of medication, 69.64% were aware of the dose, 68.20 knew about the frequency of administering the medication, 64.74% knew the duration for which the medication was to be given, and 46.56% recognized possible side effects. A mild statistical association was observed between the mode of discharge instructions and the knowledge of the caregiver about possible side effects of the prescribed medicine.
Written instruction was found to be more effective in communicating the plan of follow-up, identification of problems that would need a follow-up, and signs and symptoms for revisiting the pediatric emergency [Table 3]. On comparing verbal only versus written and verbal instructions, a better understanding of patient follow-up and revisit signs and symptoms details was displayed by those who got the latter.
Table 3.
Efficacy of mode of instruction on knowledge of treatment follow-up plan
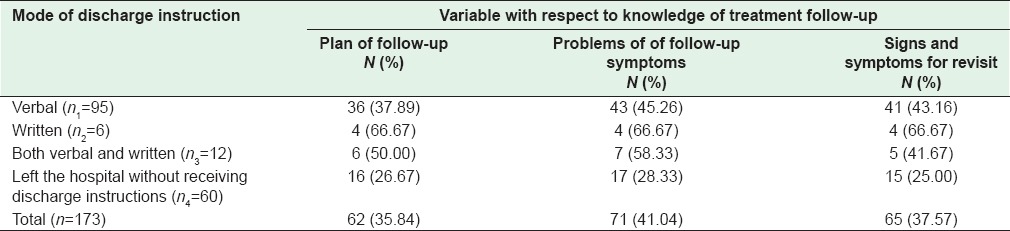
Figure 3 represents the proportion of caregivers who were unaware of the treatment regime. From Figure 3, it was observed that giving written and verbal instructions together were more effective in communicating the treatment regime to the caregivers than either verbal or written instructions alone. The percentage of respondents who were unaware of after-care ranged from 0 (knowledge of dose of medicine) to 56.84 (unaware about signs and symptoms for a revisit). About 66.67% of the respondents who got written instructions did not know the name of the medicine. This is at par with those who left the hospital without receiving any discharge instructions. The caregivers who did not receive discharge instructions were unaware of the medicine and the follow-up plan.
Figure 3.
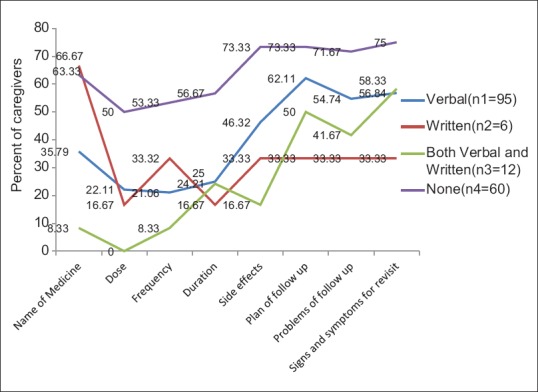
Proportion of caregivers who were unaware about treatment regime
DISCUSSION
A total of 173 caregivers of pediatric patients were surveyed during the first follow-up postdischarge from the Paediatric ED at King Abdul Aziz Medical City, Riyadh, KSA.
Of all the caregivers surveyed, the majority was aged 31 to 50 years (71%) and more than half were females (53.74%). According to the estimates of the family caregiver alliance (2012), the majority of caregivers was also female and the percentage of family or informal caregivers who were women ranged from 53% to 68%. While men also provide assistance, female caregivers tend to spend more time providing care than male caregivers (21.9 vs. 17.4 h per week). Besides, women were likely to assist with more difficult caregiving tasks, such as seeing to the toilet of the patient, while men were more likely to assist with finance or arrange for other care.[15]
Parents (92.48%) of the pediatric patients, both father and mother, were the primary caregivers as they play a crucial role in the care and safety of their children. The rest were relatives/informal caregivers.
Of the 173 caregivers surveyed, most had only basic school education, while only 35.25% were graduates or had higher degrees. Higher literacy levels make it easier for caregivers to comprehend written/verbal instructions provided by health-care professionals who often use medical terminology during communication.
An earlier study on ED patients’ understanding of common medical terms used by health-care providers revealed a significant positive independent relationship between knowledge test score and the level of education (P < 0.001).[16] Hence, it is imperative for emergency health-care providers to understand that even commonly used medical terms should be carefully explained to their patients.
The study demonstrates that providing verbal and written discharge instructions together are more effective in imparting information on medications and care to be followed at home than either verbal only or written instructions only. This is consistent with the findings from a study[17] on otitis media patients whose knowledge scores were recorded in three areas-medication data, signs of improvement, and worrying signs. In terms of the knowledge of the medication data, parents in the intervention group (written information in addition to verbal information) scored significantly higher than the control group (verbal information) during the exit interview (p < 0.05). A similar outcome was reported in a burns trial[18] where the intervention group (written information in addition to verbal information) had significantly higher knowledge scores overall than those in the control group (verbal information) (p = 0.029).
Caregivers provided with written instructions displayed a better understanding of the treatment follow-up plan and identifying signs and symptoms for a revisit, while those provided with both verbal and written instructions had better knowledge about the name of the medication, dosage, dose frequency, and the duration for which the medications were to be used. Hence, providing clear instructions to caregivers verbally at the time of discharge along with written instructions is necessary to improve their understanding of the specifics of patient care.
Despite being provided with both written and verbal instructions, nearly half of the caregivers reported to be unaware of the plan and problem of follow-up and signs and symptoms of a revisit. This lacuna underlines the emphasis that needs to be given to these parameters at the time of delivering discharge instructions. Research has suggested the use of pictographs to communicate discharge instructions to patients.[19]
The study also reveals the importance of providing instructions to those who leave the hospital in a hurry without receiving the discharge instructions. Such caregivers call for more consideration as this might cause hospital readmissions. Mobile technology may be suggested to make it easier for caregivers to transition back to their home environment. The cell phone number provided during patient registration can be used to deliver and confirm the receipt of electronic discharge instructions so that patients can see the instructions with respect to prescribed medications, diet, activity, and recommended follow-up appointments.
Recommendations
From the results of the study, it is recommended that both verbal and written instructions should be given to caregivers of pediatric patients at the time of the patient's discharge. This combination reinforces what caregivers need to do at home to care for the patient and also acts as proof of information exchanged between the health-care provider and caregiver. Pictographs that are easily understood by both caregivers and older children can be supplementary to written instructions and verbal communication for better comprehension. The study calls for the possibility of delivering discharge instructions through friendly communication with the caregiver or through mobile phone applications so that no caregiver or patient misses the instructions or is denied the benefit of discharge instructions.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
The authors would like to thank Dr. Abdulla Al-Mutrafy, Deputy Executive Director, Medical Services for King Abdullah Specialist Children Hospital, King Abdulaziz Medical City, Riyadh, Formerly Dean, College of Applied Medical Sciences, King Saud bin Abdulaziz University for Health Sciences, Riyadh, for providing support for the conduct of the study.
REFERENCES
- 1.Curran JA, Murphy A, Newton M, Zemek R, Hartling L, Plint A, et al. Discharge instructions for caregivers in the context of pediatric emergency care: A narrative synthesis protocol. Syst Rev. 2014;3:26. doi: 10.1186/2046-4053-3-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Geboers B, Brainard JS, Loke YK, Jansen CJ, Salter C, Reijneveld SA, et al. The association of health literacy with adherence in older adults, and its role in interventions: A systematic meta-review. BMC Public Health. 2015;15:903. doi: 10.1186/s12889-015-2251-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Maloney LR, Weiss ME. Patients’ perceptions of hospital discharge informational content. Clin Nurs Res. 2008;17:200–19. doi: 10.1177/1054773808320406. [DOI] [PubMed] [Google Scholar]
- 4.Karliner LS, Auerbach A, Nápoles A, Schillinger D, Nickleach D, Pérez-Stable EJ. Language barriers and understanding of hospital discharge instructions. Med Care. 2012;50:283–9. doi: 10.1097/MLR.0b013e318249c949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Strunin L, Stone M, Jack B. Understanding rehospitalization risk: Can hospital discharge be modified to reduce recurrent hospitalization? J Hosp Med. 2007;2:297–304. doi: 10.1002/jhm.206. [DOI] [PubMed] [Google Scholar]
- 6.Atwal A. Nurses’ perceptions of discharge planning in acute health care: A case study in one British teaching hospital. J Adv Nurs. 2002;39:450–8. doi: 10.1046/j.1365-2648.2002.02310.x. [DOI] [PubMed] [Google Scholar]
- 7.Taylor DM, Cameron PA. Discharge instructions for emergency department patients: What should we provide? J Accid Emerg Med. 2000;17:86–90. doi: 10.1136/emj.17.2.86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Johnson A, Sandford J. Written and verbal information versus verbal information only for patients being discharged from acute hospital settings to home: Systematic review. Health Educ Res. 2005;20:423–9. doi: 10.1093/her/cyg141. [DOI] [PubMed] [Google Scholar]
- 9.Samuels-Kalow ME, Stack AM, Porter SC. Effective discharge communication in the emergency department. Ann Emerg Med. 2012;60:152–9. doi: 10.1016/j.annemergmed.2011.10.023. [DOI] [PubMed] [Google Scholar]
- 10.Chisholm CD, Collison EK, Nelson DR, Cordell WH. Emergency department workplace interruptions: Are emergency physicians “interrupt-driven” and “multitasking”? Acad Emerg Med. 2000;7:1239–43. doi: 10.1111/j.1553-2712.2000.tb00469.x. [DOI] [PubMed] [Google Scholar]
- 11.Jeanmonod R, Boyd M, Loewenthal M, Triner W. The nature of emergency department interruptions and their impact on patient satisfaction. Emerg Med J. 2010;27:376–9. doi: 10.1136/emj.2008.071134. [DOI] [PubMed] [Google Scholar]
- 12.Logan PD, Schwab RA, Salomone JA, 3rd, Watson WA. Patient understanding of emergency department discharge instructions. South Med J. 1996;89:770–4. doi: 10.1097/00007611-199608000-00003. [DOI] [PubMed] [Google Scholar]
- 13.Meeusen AJ, Porter R. Patient-reported use of personalized video recordings to improve neurosurgical patient-provider communication. Cureus. 2015;7:e273. doi: 10.7759/cureus.273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Free C, Phillips G, Galli L, Watson L, Felix L, Edwards P, et al. The effectiveness of mobile-health technology-based health behaviour change or disease management interventions for health care consumers: A systematic review. PLoS Med. 2013;10:e1001362. doi: 10.1371/journal.pmed.1001362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Family Caregiver Alliance (2012, November) Selected Caregiver Statistics (Fact Sheet) 2012. [Last accessed on 2015 Dec 12]. Available from: https://www.caregiver.org/selected-caregiver-statistics .
- 16.Lerner EB, Jehle DV, Janicke DM, Moscati RM. Medical communication: Do our patients understand? Am J Emerg Med. 2000;18:764–6. doi: 10.1053/ajem.2000.18040. [DOI] [PubMed] [Google Scholar]
- 17.Isaacman DJ, Purvis K, Gyuro J, Anderson Y, Smith D. Standardized instructions: Do they improve communication of discharge information from the emergency department? Pediatrics. 1992;89(6 Pt 2):1204–8. [PubMed] [Google Scholar]
- 18.Jenkins HM, Blank V, Miller K, Turner J, Stanwick RS. A randomized single-blind evaluation of a discharge teaching book for pediatric patients with burns. J Burn Care Rehabil. 1996;17:49–61. [PubMed] [Google Scholar]
- 19.Zeng-Treitler Q, Kim H, Hunter M. Improving Patient Comprehension and Recall of Discharge Instructions by Supplementing Free Texts with Pictographs, AMIA 2008 Symposium Proceedings. 2008:849–53. [PMC free article] [PubMed] [Google Scholar]


