Abstract
Chronic excess salt intake increases the risk for hypertension and moderation of salt intake is an important strategy for prevention of cardiovascular and kidney disease, especially in salt-sensitive subjects. Although short-term blood pressure (BP) responses to high salt intake over several days are highly variable, chronic high salt intake worsens BP salt-sensitivity. Aging, diabetes, hypertension, and various acquired and genetic kidney disorders also exacerbate salt-sensitivity of BP. Kidney dysfunction, characterized by impaired pressure natriuresis, has been demonstrated in all forms of experimental and human genetic or acquired salt-sensitive hypertension studied thus far. Abnormalities of kidney function that directly or indirectly increase NaCl reabsorption, decrease glomerular capillary filtration coefficient, or cause nephron injury/loss exacerbate BP salt-sensitivity. In most cases, salt-sensitive hypertension is effectively treated with drugs that increase glomerular filtration rate or reduce renal NaCl reabsorption (e.g. diuretics, renin-angiotensin-aldosterone system blockers). Increased vascular resistance may occur concomitantly or secondarily to kidney dysfunction and increased BP in salt-sensitive hypertension. However, primary increases in non-renal vascular resistance have not been shown to cause salt-sensitive hypertension or long-term changes in BP in the absence of impaired renal-pressure natriuresis. The mechanisms responsible for increased total peripheral resistance (TPR) during high salt intake in salt-sensitive subjects are not fully understood but likely involve pressure-dependent and/or flow-dependent autoregulation in peripheral tissues as well as neurohormonal factors that occur concomitantly with kidney dysfunction. Physiological studies have demonstrated that increased BP almost invariably initiates secondary pressure-dependent functional and structural vascular changes that increase TPR.
Keywords: cardiac output, kidney, hemodynamics, hypertension, vasoconstriction, sodium
Chronic high salt intake increases the risk for hypertension and associated cardiovascular and kidney disease whereas modest reductions in salt intake significantly decrease BP in many hypertensive subjects.1-3 However, the mechanisms of salt-induced changes in BP continue to be the subject of considerable interest and controversy.
“Salt” in the context of this review refers to NaCl. In humans and experimental models, full expression of salt-sensitive hypertension depends on sodium and chloride.4-6 Although some studies suggest that sodium bicarbonate loading can raise BP and cause renal vasoconstriction in sensitive subjects, the BP effect is about half as great as with NaCl loading7 and plasma volume is expanded much less by non-chloride sodium salts than with NaCl.8
Hemodynamic events that initially accompany abrupt, large increases in salt intake in subjects who are considered to be “salt-resistant” include positive sodium balance and increased extracellular fluid volume (ECFV), transient increased cardiac output (CO), and minimal changes in BP.9 Total peripheral vascular resistance (TPR) may initially decrease, perhaps due to reflex/hormonal mechanisms that cause vasodilation in response to volume loading, but within a few days TPR returns to near normal as salt/volume balance is reestablished and CO and BP return to near normal levels. In “salt-sensitive” subjects high salt intake also causes sodium retention (which has been reported to be similar7 or greater10 than in salt-resistant subjects) as well as increases in ECFV and CO.9 In salt-sensitive subjects, however, high salt intake causes a gradual increase in BP followed by a rise in TPR.9
Because BP is, mathematically, the product of CO and TPR, the rise in BP in salt-sensitive subjects has been attributed to increased TPR, or “vasodysfunction”.9,11 The basic idea is that salt-resistant subjects vasodilate during high salt intake whereas salt-sensitive subjects vasoconstrict, thereby raising their BP.11 This simplistic view does not take into account the following: 1) overwhelming experimental evidence indicates that kidney dysfunction is required for increased salt intake to raise BP chronically in all experimental and human forms of genetic or acquired salt-sensitive hypertension studied thus far;12-14 2) there is little evidence of vasodilation in salt-resistant subjects after several days of increased salt intake since BP, CO, and TPR are not significantly different than at normal salt intake;9 3) vasoconstriction often follows, rather than precedes, increased BP in salt-sensitive hypertension;9,12,15 4) physiological studies show that increased BP almost invariably initiates pressure-dependent functional and structural vascular changes that increase TPR;12,15 5) vascular changes associated with hypertension regress with treatments that improve renal excretory function (e.g. diuretics) and reduce BP; and 6) vasoconstriction of non-renal blood vessels, induced experimentally or by genetic mutations, has not been shown to increase salt-sensitivity of BP.
In this review, I discuss evidence that kidney dysfunction is required for chronic increases in BP in subjects who are “salt-sensitive” and that vasoconstriction of non-renal blood vessels, although present in salt-induced hypertension, is insufficient to chronically increase BP in the absence of kidney dysfunction. Evidence that vasoconstriction during salt loading may be secondary to increased BP, serving to protect tissues from pressure or flow overload, is also reviewed.12,15
Heterogeneity of Blood Pressure Responses to Changes in Salt Intake: “Salt-Sensitivity” and “Salt Resistance”
There is considerable heterogeneity of BP responses to changes in salt intake in normotensive and hypertensive subjects. Kawasaki et al,10 in one of the first reports of BP salt-sensitivity, studied hypertensive subjects on “normal” (109 mmol/d), “low” (9 mmol/d), and “high” (249 mmol/d) sodium intakes for one week at each level (Figure 1). The 9 subjects who had at least a 10% increase in BP during high compared to low salt intake were identified as “salt-sensitive” and the other 10 subjects were classified as “non–salt sensitive”. The salt-sensitive subjects retained more sodium and gained more weight on high salt intake than those who were “non-salt-sensitive”.10 This and subsequent investigations in normotensive or hypertensive subjects indicate that “salt sensitivity” is a continuous phenotype, not bimodal as might be inferred from the terms “salt-sensitive” and “salt-resistant”.4,16
Figure 1.

Percent increase in mean blood pressure in salt-sensitive and salt-resistant patients with hypertension when their diet was changed from a low sodium (9 mEq/day) to a high sodium (240 mEq/day) for one week at each level. Data are from Kawasaki et al.10
Assessment of BP salt-sensitivity in clinical studies is challenging. Weinberger and colleagues have measured changes in BP after large amounts of salt/volume were infused or rapidly depleted from the body by salt restriction and administration of powerful diuretics.16 This method has provided mechanistic insights into BP salt-sensitivity and appears to be reproducible.16 The neurohormonal and vascular mechanisms activated by rapid changes in blood volume and BP, however, may differ from those involved in chronic responses to physiological changes in salt intake. Measuring BP during prolonged changes in dietary NaCl intake in outpatient protocols and clinical trials reliably assesses BP salt-sensitivity in the “real world”, but mechanistic studies in humans lasting more than a few days are rare. Moreover, this approach is laborious, expensive, dependent on patient compliance, and is influenced by various genetic and demographic factors.
The challenge of assessing BP salt-sensitivity in humans has led investigators to examine various surrogate biomarkers such as plasma renin activity, atrial natriuretic peptide, genetic screens, proteomics, and urine exosomes.16,17 Although some biomarkers have shown promise in predicting BP salt-sensitivity, most have not been widely adopted for clinical practice and their accuracy is still uncertain. Many of these issues related to assessment of BP salt-sensitivity have been previously reviewed.16,17
Salt-sensitivity, in addition to being heterogeneous, is not a fixed phenotype. With aging there is often an increase in salt-sensitivity16 associated with a gradual loss of functional nephrons after age 40, even in healthy persons.18 Thus, most of us are prone to become salt-sensitive, to some extent, if we live long enough. With various pathophysiological conditions that cause more rapid loss of kidney function (e.g. diabetes, hypertension), loss of functional nephrons is accelerated and salt-sensitivity is amplified.4,16 Thus, phenotypes that are often associated with salt-sensitive BP include older age, diabetes, hypertension, obesity, kidney disease, and African-American ethnicity.4,16
There is also evidence that salt-sensitivity worsens when high salt intake is maintained for long periods of time.1,19 This progressive increase in salt-sensitivity likely reflects target organ injury, especially renal injury, through the damaging effects of high BP or other effects of high NaCl intake.1,19 BP salt-sensitivity and the mechanisms involved therefore depend partly on how long changes in salt intake are maintained.
Although BP salt-sensitivity is heterogeneous, all individuals with salt-induced chronic increases in BP have a common characteristic - they maintain salt balance at the expense of increased renal perfusion pressure.12,13 This renal dysfunction can be caused by genetic or acquired intrarenal and extrarenal neurohormonal disorders that impair the kidneys’ ability to maintain NaCl balance at normal BP.14,20 In some cases kidney dysfunction causes sodium retention and transient increases in CO that are followed by elevated TPR as BP rises. In other instances, renal dysfunction occurs concomitantly with vasoconstriction and decreased vascular capacitance and minimal NaCl retention is required to raise BP sufficiently to restore salt balance.
The critical role of kidney dysfunction in salt-induced increases in BP in sensitive subjects is highlighted by the fact that the most reproducible and consistent forms of experimental salt-sensitive hypertension are induced by impairing kidney function in various ways that reduce glomerular filtration rate (GFR) or increase tubular reabsorption. Also, all known monogenic forms of salt-sensitive human hypertension are characterized by mutations that directly or indirectly increase renal NaCl reabsorption.21-23
The Renal-Body Fluid Feedback Mechanism for Long-Term BP Regulation
Figure 2 shows the basic conceptual framework for long-term control of BP by the renal-body fluid feedback proposed by Guyton and Coleman in the 1960’s and subsequently expanded to include a large number of cardiovascular, neural and hormonal mechanisms for BP regulation.12-14,24 ECFV is determined by the balance between intake and renal excretion of salt/water. Even temporary imbalances between intake and output will change ECFV and potentially BP if cardiac and vascular functions are adequate. Although sodium can be stored in tissues such as skin, independent of volume retention,25 intake and output must eventually be balanced; otherwise, continued fluid/salt accumulation or loss could eventually lead to circulatory failure.
Figure 2.
Basic renal-body fluid feedback mechanism for long-term blood pressure regulation. A key component of this feedback is the effect of arterial pressure and urine sodium excretion, called renal-pressure natriuresis/diuresis. The dashed pressure natriuresis lines show increasingly impaired pressure natriuresis and increasing salt-sensitivity of arterial pressure. Increased arterial pressure may cause secondary increases in total peripheral resistance via pressure-dependent or flow dependent “autoregulation” in various tissues. Increased vascular capacity tends to reduce mean circulatory filling pressure.
A key element of this feedback is the effect of BP on salt/water excretion, often called “pressure natriuresis/diuresis”.20,26 This feedback was predicted to play a dominant role in long-term regulation of BP as well as salt/water balance.24 For example, if BP is increased above the renal-pressure natriuresis set-point because of increased TPR or increased cardiac pumping ability, NaCl/volume excretion would also increase and as long as excretion exceeds intake ECFV would decrease until BP returned to normal and fluid balance was reestablished.27 An important prediction of this concept is that chronic hypertension cannot be sustained unless pressure natriuresis is shifted to higher BP; otherwise, elevated BP would provoke increased sodium excretion which would reduce ECFV and CO until BP eventually returned to normal. Supporting this prediction is the finding that increases in vascular resistance that do not impair pressure natriuresis, such as closure of an A-V fistula or coarctation of the aorta below the kidneys (aortic coarctation above the kidneys causes hypertension), induce only transient increases in BP followed by natriuresis, decreased plasma volume, and rapid normalization of BP.12
Another key aspect of this conceptual framework for chronic BP regulation is the important role of neurohormonal systems in modulating pressure natriuresis.28,29 For example, during high salt intake decreased angiotensin II (AngII) and aldosterone formation enhance pressure natriuresis effectiveness, allowing sodium balance to be maintained with minimal changes in BP as long as the RAAS is functioning normally.13,28 Excessive RAAS activation, however, reduces the effectiveness of pressure natriuresis, thereby necessitating greater increases in BP to maintain sodium balance.29
In salt-resistant subjects, multiple intrarenal and neurohumoral adjustments permit salt balance with minimal changes in BP during increases in salt intake over several days. In salt-sensitive subjects elevated BP contributes to increased salt/water excretion during high salt intake through pressure natriuresis/diuresis.20,26,30 In addition to helping maintain salt/water balance, this mechanism also attenuates changes in BP during non-renal disturbances.
In all forms of human or experimental hypertension studied thus far, there is a shift of pressure natriuresis to higher BPs.12-14 This shift of pressure natriuresis can be caused by intrarenal disturbances that initially reduce GFR or increase tubular reabsorption or by extrarenal factors such as increased sympathetic nervous system (SNS) activity, excessive antinatriuretic hormones, or deficit of natriuretic hormones that reduce the kidney's ability to excrete NaCl and water.29 As BP rises, the initial kidney dysfunction is offset by natriuretic/diuretic effects of increased BP, thereby returning NaCl excretion to match intake.
Is abnormal renal-pressure natriuresis a cause or a consequence of hypertension?
The fact that hypertensive patients have normal NaCl excretion (equal to intake) despite increased BP indicates that pressure natriuresis is reset to higher BP. However, this resetting has been suggested to be secondary to increased BP rather than a major cause of hypertension.31,32 If BP truly has no long-term effect on NaCl/volume excretion, pressure natriuresis and the renal-body fluid feedback would be relatively unimportant in long-term BP regulation.
Therefore, a critical issue is whether BP has a long-term effect on NaCl/volume excretion or whether pressure natriuresis is mainly a short-term phenomenon with little role in chronic BP regulation. Although this issue has been difficult to test experimentally, several studies have confirmed that renal perfusion pressure has an important chronic effect on renal excretion and that pressure natriuresis plays a key role in maintaining salt balance in various experimental models of hypertension.13,20,33-39
Evidence that pressure natriuresis is a powerful long-term controller of salt excretion and BP
We tested whether pressure natriuresis has a long-term effect on sodium/water excretion by utilizing a split-bladder preparation to collect urine separately from each kidney and servo-controlling renal perfusion pressure in each of the two kidneys independently33 (Figure 3). Because the two kidneys in each animal were exposed to the same neurohormonal influences and blood composition, the chronic effects of small changes in renal perfusion pressure on electrolyte excretion and renal hemodynamics could be directly quantitated. These studies demonstrated that small changes in BP cause large alterations in NaCl/water excretion that persisted as long as pressure was altered (12 days). Thus, the kidneys did not adapt their excretory function during chronic changes in perfusion pressure. In fact, the long-term effects of BP on NaCl excretion are considerably greater than observed during acute pressure changes.27,29
Figure 3.
Renal artery pressure and urine sodium excretion, collected separately from each kidney using a split bladder method from kidneys of the same dogs in which pressure of one kidney was servo-controlled at a level about 10-12 mmHg below control (dashed lines) while pressure in the contralateral kidney increased about 4-5 mmHg above control (solid lines). Data are shown for 4 days of control measurements, 12 days of servo-controlling renal perfusion pressure, and 7 days of recovery. Redrawn from data in Mizelle et al.33
We also assessed the role of pressure natriuresis in maintaining NaCl/volume balance in several forms of experimental hypertension, including AngII, aldosterone, DOC-salt, norepinephrine, ACTH plus norepinephrine, and vasopressin hypertension.34-39 In each case, servo-controlling renal perfusion pressure at the normal level led to progressive sodium/water retention as well as continued increases in ECFV and systemic arterial pressure. In some cases, extreme salt/volume retention occurred when pressure natriuresis was prevented during development of hypertension, leading to circulatory congestion and pulmonary edema in a few days.
These observations highlight the powerful role of renal-pressure natriuresis in chronic regulation of NaCl balance and BP. They also strongly support the basic premise of the renal-body fluid feedback concept that chronic hypertension, including salt-sensitive hypertension, cannot be sustained in the absence of kidney dysfunction, characterized by impaired pressure natriuresis.
If kidney function is impaired in salt-sensitive hypertensive subjects, why do they sometimes excrete sodium as rapidly as normotensive subjects?
Previous studies have shown that salt-sensitive hypertensive subjects often retain more sodium than salt-resistant subjects during increased sodium intake.10,40 Some reports, however, suggest that salt-sensitive humans may excrete a sodium load almost as rapidly as salt-resistant subjects and are cited as evidence that salt-sensitive hypertension is not caused by renal dysfunction.9,11 An important, but often forgotten, consideration is that the kidneys of hypertensive subjects are perfused at elevated BP. Since increased BP tends to cause natriuresis, the finding that similar rates of excretion are observed in hypertensive and normotensive subjects implies that there is a defect in renal excretory capability. In the presence of high BP, the natriuretic handicap disappears and renal excretory function appears to be normal, except that pressure natriuresis is shifted to higher BP.
A common misconception: impaired renal-pressure natriuresis should always cause sodium retention, increased blood volume, and increased cardiac output
Although ECFV and blood volume are important components of long-term BP regulation, via the renal-body fluid feedback (Figure 2), BP is not a function of blood volume per se but of volume in relation to vascular capacity. This concept is sometimes referred to as “effective blood volume”.41 When vascular capacity increases (e.g. large varicose veins), greater blood volume is needed to maintain normal BP. Conversely, with vasoconstriction less volume is required to maintain normal BP. When high concentrations of strong vasoconstrictors such a norepinephrine and AngII are present, the kidneys may actually undergo pressure-induced natriuresis and ECFV may decrease even though the vasoconstrictors have antinatriuretic effects on the kidneys.29,37
Although norepinephrine and AngII promote sodium retention and shift pressure natriuresis to higher BPs by causing renal vasoconstriction and/or increased tubular reabsorption,13,29,37 they also rapidly increase BP because of peripheral vasoconstriction. If BP increases above the renal set-point, the elevated BP will initially cause natriuresis and decreased ECFV until BP stabilizes at the set-point dictated by the renal-pressure relationship. In parallel, decreased vascular capacitance permits maintenance of high BP with a reduced blood volume. This overfilling of the circulation, relative to vascular capacity, is reflected by increased mean circulatory filling pressure in various forms of salt-sensitive hypertension.12
Acquired Kidney Disorders That Cause Salt-Sensitive Hypertension
A challenge in determining mechanisms of salt-induced hypertension is that primary causes of increased BP are often obscured by compensatory neurohormonal, renal, and cardiovascular changes. Experimental and clinical studies, however, have shown that several types of kidney-specific disorders increase BP salt-sensitivity12,27,29,42-56 (Table 1). These include 1) various types of kidney injuries that cause loss of functional nephrons or decreased glomerular capillary filtration coefficient, 2) patchy (non-homogeneous) increases in preglomerular resistance, 3) inability to modulate the RAAS appropriately, and 4) acquired or genetic disorders that directly or indirectly increase renal NaCl reabsorption, especially in the distal and collecting tubules. The many conditions that can cause these disorders of kidney function have been reviewed previously and are distinct from those that cause salt-resistant hypertension.12,29
Table 1.
Examples of experimental kidney-specific disorders that cause salt-sensitive increases in blood pressure
| Collecting duct-specific deletion of NOS1 | Hyndman et al42 |
| Collecting duct-specific deletion of endothelin A and B receptors | Ge et al43 |
| Collecting duct-specific deletion of endothelin B receptors | Ge et al44 |
| Collecting duct-specific knockout of endothelin-1 | Ahn et al45 |
| Collecting duct-specific overexpression of renin | Ramkumar et al46 |
| Kidney intercalated cell-specific pendrin overexpression | Jacques et al47 |
| Increased renal medullary-specific oxidative stress | Cowley et al48 |
| Proximal tubule overexpression of angiotensinogen | Ying et al49 |
| Deficiency of renal cortical-specific EGF | Pavlov et al50 |
| Surgical reduction of kidney mass | Langston et al51 |
| Partial kidney infarction/nephron loss | Guyton (review)12 |
| 2-kidney, 1-clip Goldblatt hypertension | Hall, et al (review)29 |
| Hydronephrosis | Carlström et al52 |
| Uninephrectomy at a young age | Carlström et al53 |
| Kidney tubulointerstitial inflammation | Johnson et al (review)54 |
| Glomerlonephritis, IgA nephropathy | Konishi et al55 |
| Adenine-induced kidney injury | Nguy et al56 |
Note: This is only a partial list of the many kidney-specific disorders that have been shown to cause salt-sensitive blood pressure. Reviews listed in this table provide additional examples and discussion.
Kidney injury and decreased functional nephrons causes salt-sensitivity
One of the most reliable experimental methods for creating salt-sensitivity is to induce renal injury and loss of functional nephrons.12,51,56 Although surgical removal of up to 70% of kidney mass does not, by itself, cause marked hypertension it does greatly enhance BP salt-sensitivity.51 Uninephrectomy or chronic high salt diet in young animals, after completed nephrogenesis, also causes salt-sensitive hypertension in adulthood.53 Hydronephrosis, partial kidney infarction, tubulointerstitial inflammation, immune cell infiltration of the kidneys, IgA nephropathy, and many other types of renal insults also cause BP salt-sensitivity.27,52,54,55,57 In patients with chronic kidney disease, BP salt-sensitivity increases exponentially as creatinine clearance decreases.58 Salt loading in patients with severe kidney disease causes much greater increases in BP and intravascular volume compared to patients with moderate kidney disease.58 Thus, acquired renal injuries due to aging, diabetes, hypertension and various types of acute and chronic kidney injury, even when they are subtle, usually increase BP salt-sensitivity.4,16,27,54
RAAS-mediated kidney dysfunction causes salt-sensitivity
Increased activity of the RAAS or fixed low activity of the RAAS causes BP salt-sensitivity28 (Figure 4). This is not surprising since the RAAS is the most powerful hormone system for regulating NaCl balance.59 When the RAAS is fully functional, the chronic renal-pressure natriuresis curve is steep and NaCl balance can be achieved over a wide range of intakes with minimal BP changes.28,29
Figure 4.
Changes in mean arterial pressure during chronic increases in sodium intake from 5 to 80, 240 and 480 mEq/day in normal control dogs, after angiotensin converting enzyme (ACE) inhibition, or after AngII infusion at a low, initially subpressor dose, to prevent AngII from being suppressed when sodium intake was increased. Note that BP salt-sensitivity is markedly increased when AngII levels cannot be suppressed because of high fixed AngII levels or because of low fixed AngII due to ACE inhibition. Redrawn from data in Hall et al.28
The mechanisms that mediate the potent effects of AngII on pressure natriuresis and salt-sensitive BP include direct and indirect effects that increase tubular reabsorption as well as renal hemodynamic effects.59 Although the BP effects of AngII have often been attributed to its actions on the brain, adrenal gland, and non-renal blood vessels, activation of kidney AT1 receptors is required for AngII to cause chronic hypertension.60,61 Crowley, Coffman and colleagues62 found that AngII infusion in wild-type (WT) mice increased BP and caused cardiac hypertrophy and fibrosis. However, in WT mice that received transplanted kidneys from AT1 receptor knock-out mice (i.e. AT1 receptors were present in the peripheral vasculature, brain, heart and other organs, but not in the kidneys), AngII infusion did not raise BP chronically or cause cardiac hypertrophy/fibrosis. In AT1 receptor knock-out mice that received transplanted kidneys from WT mice (i.e. AT1 receptors were present only in the kidneys and not in peripheral blood vessels, brain, heart or other organs), AngII infusion caused chronic hypertension as well as cardiac hypertrophy/fibrosis. These observations indicate that renal effects of AngII, instead of peripheral vascular or other non-renal effects, mediate chronic increases in BP and cardiac hypertrophy in this salt-sensitive model of hypertension.
Although the kidney cell lineages responsible for the chronic BP effects of AngII have not been completely elucidated, proximal tubule AT1 receptors play an important role by augmenting NHE3-dependent sodium reabsorption.63 Kidney vascular AT1 receptors contribute to the pathogenesis of AngII-induced hypertension by reducing renal blood flow which also enhances sodium retention.64 Thus, the long-term effects of AngII on BP and salt-sensitivity are closely coupled to renal tubular and hemodynamic actions that cause salt/water retention.
Excessive activation of the mineralocorticoid receptor (MR) also increases NaCl reabsorption in the distal nephron and BP salt-sensitivity while suppressing AngII formation. MR activation can occur as a result of increased circulating ligands, such as aldosterone, or because of other factors that activate MR even in the absence of increased levels of mineralocorticoids. For example, deficiency of 11β-hydroxysteroid dehydrogenase 2 (11β-HSD2) can lead to activation of MR by glucocorticoids, as discussed later. Additional factors in salt-sensitive hypertension that have been suggested to activate renal tubular MR in a ligand-independent manner include increased reactive oxygen species and Ras-related C3 botulinum toxin substrate (Rac1), a Rho family small GTPase.65 The molecular/cellular mechanisms linking these changes with increased renal tubular NaCl reabsorption and BP salt-sensitivity have been previously reviewed.65
Endothelin-mediated kidney dysfunction causes salt-sensitive BP
Although endothelin-1 (ET-1) is a potent vasoconstrictor its renal actions, especially in the collecting ducts (CDs), are of unique importance in long-term BP salt-sensitivity66 (Table 1). The CDs produce ET-1 which binds in an autocrine manner to endothelin A/B (ETA/B) receptors, causing inhibition of salt/water reabsorption.66 Salt/volume loading stimulates CD ET-1 production through local mechanisms that sense salt delivery and shear stress when flow rate increases. Locally released ET-1 activates ETB receptors and inhibits sodium reabsorption. The importance of these renal actions is demonstrated by the fact that CD-specific deletion of ETB receptors increases BP salt-sensitivity.44 CD-specific deletion of ET-1 production or deletion of ETA/B receptors in CDs produces even greater salt-dependent BP elevation than knockout of ETB receptors alone.43,45 Blockade of ET-1 receptors also attenuates or abolishes hypertension in Dahl-salt sensitive rats and DOCA-salt hypertension. 66,67
These observations do not necessarily negate a potential role for extrarenal ET-1 or its receptors in BP salt-sensitivity. Although ET-1 is a potent vasoconstrictor in many tissues, including the kidneys, and may stimulate SNS activity and regulate extravascular sodium storage,68 whether these extrarenal actions ultimately influence renal-pressure natriuresis and chronic BP regulation is unclear. What is clear is that the renal actions of ET-1, especially in the CD, play a major role in protecting against salt-sensitive hypertension.
Genetic Kidney Disorders That Cause Salt-Sensitive Hypertension
Kidney transplantation attenuates or abolishes genetic salt-sensitive hypertension in rodents
In Dahl salt-sensitive rats,69,70 Milan hypertensive rats,71 Prague hypertensive rats,72 and Okamoto spontaneously hypertensive rats (SHR),69,73 hypertension can be transferred with renal grafts from the hypertensive strain to normotensive histocompatible recipients. Conversely, renal grafts from normotensive control strains reduce or normalize BP in each of these genetically hypertensive rat strains. Thus, renal mechanisms have consistently been shown to play a key role in rodent models of genetic, salt-sensitive hypertension.
Although kidney dysfunction is clearly a major cause of increased BP in these rodent models of genetic hypertension, there is often little evidence of volume expansion or increased CO after hypertension is established. The most obvious abnormality is increased TPR. The mechanisms responsible for increased TPR have not been fully elucidated but, in some cases, may occur secondary to the rise in BP, via pressure- or flow-dependent autoregulatory vasoconstriction.14 In other instances neurohormonal or paracrine factors may contribute to increased TPR even though kidney dysfunction is required for hypertension to be sustained.
Volume expansion is required for increases in BP and TPR to be triggered in some forms of salt-sensitive hypertension. For example, servo-control of body weight to prevent volume expansion abolished increased BP when Dahl salt-sensitive or AngII-infused rats were placed on a high salt diet.74,75 Regardless of whether increased BP is associated with measureable volume expansion, kidney dysfunction plays a critical role in genetic as well as acquired forms of salt-sensitive hypertension.
Kidney dysfunction in monogenic, salt-sensitive human hypertension
Table 2 shows 7 monogenic disorders that share the common phenotypes of increased renal NaCl reabsorption and salt-sensitive hypertension.21-23 Although these disorders account for <1% of human hypertension, they provide additional examples of salt-sensitive BP associated with kidney dysfunction and impaired pressure natriuresis.
Table 2.
Monogenic forms of salt-sensitive hypertension and therapies that effectively reduce blood pressure in these disorders.
| Genetic Disorder | Treatment |
|---|---|
| Liddle syndrome | amiloride, triamterene |
| Activating MR mutation exacerbated by pregnancy | delivery of fetus amiloride, triamterene, |
| Apparent mineralocorticoid excess (AME) | MR antagonist, amiloride, triamterene |
| Gordon syndrome | thiazide diuretic |
| Glucocorticoid remediable aldosteronism (FH-I, GRA) | glucocorticoids, MR antagonist, amiloride, triamterene |
| Congenital adrenal hyperplasia (CAH) | adrenalectomy or MR antagonist |
| Familial hyperaldosteronism not remediable by glucocorticoids (FH-III and FH-IV) |
adrenalectomy or MR antagonist |
Note: Vasodilators are generally ineffective in treating these disorders that are associated with increased renal tubular NaCl reabsorption
That these human monogenic forms of hypertension are effectively treated with appropriate diuretics that reduce renal NaCl reabsorption reinforces the importance of excessive renal salt/water reabsorption in the pathogenesis of increased BP. For example, pseudohypoaldosteronism type 2 (Gordon syndrome) is caused by mutations of genes that encode WNK1 and WNK4, two members of the WNK family of serine-threonine kinases expressed in the distal nephron.76 Mutations of WNK1 are large intronic deletions that increase WNK1 expression whereas WNK4 mutations are missense and cause loss of function. Both mutations increase activity of thiazide-sensitive NaCl transporters in the distal nephron, and patients with these mutations are effectively treated with thiazide diuretics which lower BP chronically by inhibiting NaCl renal reabsorption.76
Liddle syndrome is caused by gain of function mutations of the β or γ subunits of the epithelial sodium channel (ENaC).21-23 This disorder causes increased sodium reabsorption, hypoaldosteronism and low plasma renin activity, and is effectively treated with amiloride or triamterene which block ENaC and inhibit CD reabsorption.21,22
Glucocorticoid-remediable aldosteronism (GRA), apparent mineralocorticoid excess (AME), congenital adrenal hyperplasia, familial hyperaldosteronism not remedial by glucocorticoids, and hypertension exacerbated by pregnancy are all monogenic forms of salt-sensitive hypertension associated with excessive activation of MR. All are effectively treated by drugs that block renal tubular ENaC, MR, or aldosterone secretion. In each case, there is evidence of kidney dysfunction,21 including studies showing reversal of hypertension when patients received normal kidneys without the mutation.77-81
Kurtz, Morris and colleagues have11 questioned whether increased renal NaCl reabsorption can account for increased BP in monogenic salt-sensitive hypertension and have opined that “vasodysfunction” may underpin hypertension. Their main argument is based on the observation that salt-induced BP increases are often associated with increased TPR whereas non-hypertensive salt-resistant subjects may have normal or reduced TPR.11 It should be noted, however, that changes in CO and TPR have not actually been measured during salt-induced BP increases in these forms of monogenic hypertension. Also, primary vascular dysfunction has not been shown to play a causal role in initiating the hypertension and may occur secondarily to increased BP and pressure- or flow-dependent autoregulatory responses.14,15,82
A common misconception, illustrated in a review by Kurtz et al, is that “autoregulatory” increases in TPR require increased CO to be activated.11 However, increased BP almost invariably evokes vasoconstriction, even in isolated blood vessels or tissues, with or without increases in CO or blood flow, and may also result from pressure-dependent structural changes during chronic increased BP.14,15,82 Neurohormonal-mediated vasoconstriction may also occur concomitantly with kidney dysfunction and, if severe, may actually reduce plasma volume and CO even though kidney dysfunction is required for salt-induced BP increases to be sustained.
Kidney transplantation attenuates or abolishes salt-sensitive hypertension in AME or Liddle syndrome
AME, a monogenic form of salt-sensitive hypertension, is caused by deficiency of 11β-HSD2 which causes glucocorticoid activation of MR.83 Although cortisol can bind to MR with high affinity, renal epithelial cells are normally “protected” by 11β-HSD2 which locally converts cortisol to cortisone which does not avidly bind MR. Therefore, 11β-HSD2 deficiency causes excessive MR stimulation which activates ENaC in aldosterone-sensitive distal nephrons, leading to impaired renal-pressure natriuresis and hypertension with characteristics similar to that caused by primary aldosteronism.83 After hypertension is established, most indices of kidney function appear normal, except for hypokalemia and impaired renal-pressure natriuresis, and multiple vascular abnormalities begin to appear as a consequence of increased BP.
Unambiguous evidence for kidney dysfunction in mediating this form of salt-sensitive hypertension comes from the finding that transplantation of normal kidneys into patients with AME caused complete remission of hypertension and electrolyte abnormalities.77,78 These observations indicate that hypertension in AME has a renal origin.
Similar results were obtained in a patient with Liddle syndrome whose hypertension resolved after receiving a kidney transplant.79 The finding that BP remained normal for at least 5 years after kidney transplantation, even though potential extrarenal effects associated with this syndrome were still present, indicates that the kidney abnormalities played a critical role in the pathogenesis of hypertension.
Kidney dysfunction also occurs in salt-sensitive hypertension caused by excess MR activity in primary aldosteronism or glucocorticoid-remediable aldosteronism.83 Although vasodysfunction may occur in rodent and human genetic salt-sensitive hypertension, there are no studies, to my knowledge, demonstrating that non-renal vasoconstriction induced by MR activation causes salt-sensitive hypertension. Also, it is unclear whether increased TPR is directly related to vascular/endothelial MR activation or is secondary to NaCl/volume retention and pressure-dependent vasoconstriction in these forms of hypertension. On the other hand, there is substantial evidence that kidney dysfunction is necessary for increased BP in human and rodent genetic salt-sensitive hypertension.
Human primary hypertension
Curtis et al.80 demonstrated in patients with primary hypertension that transplantation of kidneys from normotensive donors completely resolved their hypertension. After an average follow-up of 4.5 years, the patients were normotensive, without antihypertensive medication.80 BP normalization was associated with regression of vascular injury and left ventricular hypertrophy, indicating that these abnormalities occurred as a consequence of hypertension. If vascular dysfunction or non-renal neurohumoral mechanisms were major causes of hypertension in these patients then increased BP should have reappeared. However, all patients remained normotensive and had normal renal sodium handling in response to wide variations in sodium intake (between 9 and 300 mmol/day) even after several years of follow-up, indicating that kidney abnormalities underpinned their hypertension.80
Guidi et al81 followed 85 patients with hypertension and ESRD of different origin for an average of 8 years after renal transplantation. Recipients who were transplanted with kidneys from donors with a positive family history of hypertension needed more antihypertensive treatment to reach target BP than when transplanted with a kidney from a donor with a negative family history of hypertension.
Although limited human data are available, current evidence suggests that non-renal vascular dysfunction often follows the hypertension rather than causing increased BP. As shown in Table 3, kidney specific interventions attenuate or prevent salt-induced increases in BP in many models of salt-sensitive hypertension.62,63,70-73,78-80,84-88 These observations do not negate the importance of neurohormonal mechanisms in mediating vasoconstriction or hypertension by altering kidney function but they do provide another proof-of-principle test of the concept that kidney dysfunction is a key cause of salt-sensitive hypertension.
Table 3.
Examples of kidney-specific interventions that prevent or attenuate salt-sensitive increases in blood pressure (BP)
| Transplantation of kidney from normotensive human donors normalizes BP in | |
| Patients with apparent mineralocorticoid excess | Kattab et al78 |
| Patients with Liddle’s syndrome | Botero-Velez et al79 |
| Patients with essential hypertension | Curtis et al,80 |
| Transplantation of kidneys from normotensive donor rats reduces/normalizes BP in | |
| Dahl salt-sensitive rats | Dahl et al70 |
| Prague Hypertensive rats | Heller et al72 |
| Milan Hypertensive rats | Bianchi et al71 |
| Spontaneously hypertensive rats | Kawabe et al73 |
| Collecting duct-specific renin deletion attenuates AngII hypertension | |
| Ramkumar et al84 | |
| Distal convoluted tubule-specific deletion of NCC transporter reverses hypertension caused by WNK4 mutations (pseudohypoaldosteronism type II) | |
| Lalioti et al85 | |
| Kidney-specific deletion of TNF-α attenuates AngII hypertension | Zhang et al86 |
| Kidney-specific deletion of AT1 receptors blocks chronic AngII hypertension | |
| Crowley et al62 | |
| Proximal tubule-specific deletion of AT1 receptors attenuates AngII hypertension | |
| Gurley et al63 | |
| Renal denervation lowers blood pressure in | |
| Obese hypertensive humans | DiBona and Esler87 |
| Obese hypertensive experimental animals | Henegar et al88 |
Diuretics lower BP in salt-sensitive hypertension by reducing renal tubular reabsorption
Responses to diuretics provide additional insights into the mechanisms by which salt/volume changes influence BP regulation in salt-sensitive subjects. Although diuretics initially reduce renal NaCl and water reabsorption, balance between NaCl intake and output eventually occurs, BP decreases, CO is usually normal or slightly reduced, and TPR decreases.89 These responses, the reverse of what happens when salt intake is increased in salt-sensitive subjects, have led to speculation that diuretics lower BP by causing peripheral vasodilation.90 However, diuretics have little chronic effect on BP unless they are able to increase renal NaCl/volume excretion; for example, thiazide diuretics do not significantly lower BP in patients with ESRD who cannot respond to their natriuretic and volume depleting effects.91 The hypotensive effects of furosemide also depend on natriuresis and diuresis.92
If direct vascular actions of diuretics cannot account for their chronic BP lowering effects, why do diuretics lower TPR? Frohlich and colleagues89 showed that chlorothiazide administration initially reduced plasma volume and CO. With prolonged diuretic administration, TPR decreased in parallel with the fall in BP. This sequence suggests that decreased TPR is secondary to volume depletion and decreased BP, and again highlights the key role of kidney dysfunction in mediating salt-induced BP increases in salt-sensitive subjects.
Kidney Disorders That Cause Salt-Resistant Hypertension
Although kidney dysfunction is necessary for hypertension to be sustained chronically, not all kidney disorders cause salt-sensitive hypertension. Generalized increases in preglomerular resistance caused by suprarenal aortic coarctation or constriction of one renal artery and removal of the contralateral kidney (1-kidney, 1-clip Goldblatt hypertension) cause salt-resistant hypertension.12,93 Immediately after constriction of the renal artery or aorta, GFR and sodium excretion decrease and renin secretion increases. As BP rises most indices of renal function return to nearly normal, including sodium excretion and pressure distal to the stenosis, if the constriction is not too severe.12,93
A major reason that high salt intake does not greatly exacerbate hypertension caused by increased preglomerular resistance is that after BP increases sufficiently to restore renal perfusion pressure and renin secretion to normal, the RAAS is fully capable of appropriate suppression during high salt intake.29 As discussed previously, the ability to effectively modulate RAAS activity is a key mechanism for preventing salt-sensitivity of BP.
Phosphodiesterase 3A mutations cause increased vascular resistance and salt-resistant hypertension
Autosomal-dominant hypertension with brachydactyly is caused by gain-of-function mutations in the gene encoding phosphodiesterase 3A (PDE3A) which catalyzes hydrolysis of intracellular second messengers, cAMP and cGMP.94 The mutated PDE3A causes vascular smooth muscle cell proliferation and vasoconstriction, leading to increased TPR and presumably increased renal vascular resistance. Sympathetic blockade and hydrochlorothiazide treatment were ineffective in reducing BP whereas nitroprusside caused acute decreases in BP, consistent with an intrinsic vascular abnormality.95,96 Despite marked vasoconstriction and increased TPR, these patients are not salt-sensitive and have normal renin, aldosterone and norepinephrine.96
Thus, generalized vasoconstriction does not appear to increase BP salt-sensitivity in the absence of kidney abnormalities that increase tubular reabsorption, decrease glomerular filtration coefficient, and/or reduce responsiveness of the RAAS. Renal preglomerular vasoconstriction can increase BP but the hypertension is usually not salt-sensitive.
Is Increased TPR (“Vasodysfunction”) a Consequence Rather Than a Cause of Salt-Sensitive Hypertension?
Although kidney dysfunction clearly plays a causal role in salt-induced hypertension (Tables 1, 3), sodium balance, plasma volume, and CO may not be markedly different than in normotensive subjects after hypertension is established. The most obvious abnormality is often increased TPR; even in hypertension that is clearly initiated by kidney dysfunction and salt loading, CO is usually normal and TPR is increased after a few days. What causes increased TPR in salt-loading hypertension?
It is important to remember that TPR is a recondite number, derived from measurements of BP and CO. If BP increases and CO returns to normal, as occurs even when kidney dysfunction and salt/volume retention initiate the hypertension, increased TPR will be calculated. Unless the heart is weakened or metabolic rate of the tissues is altered, CO is chronically regulated at a level that is near normal and TPR increases in proportion to BP.
Why does CO return to nearly normal following transient increases during salt loading? This is easier to understand if one remembers that CO represents the total blood flow of the organs/tissues. The proper level of tissue blood flow is one of the highest priorities for homeostasis and is achieved by multiple short-term and long-term mechanisms, including local tissue controls. Short-term studies show that active vasoconstriction occurs in most tissues when BP or blood flow is increased.12,15,82 When BP increases are sustained, gradual vascular remodeling and thickening of blood vessel walls occur. Blood flows in most tissues, and therefore CO, are ultimately maintained at a level appropriate for the tissue metabolic needs even with high salt/volume intake and increased BP. This process has often been called “autoregulation” and involves pressure-dependent as well as flow-dependent factors and almost invariably leads to increased TPR when BP increases.12,15,82 Moreover, when renal excretory function is improved (e.g. by kidney transplantation or treatment with diuretics) and BP is reduced, TPR also decreases and vascular changes usually regress.
Is increased TPR required for development of salt-sensitive hypertension?
In contrast to multiple studies showing that kidney dysfunction is required for salt-sensitive BP increases, there have been no studies, to my knowledge, demonstrating that increased TPR is required for salt-induced increases in BP, or that primary increases in non-renal vascular resistance can cause salt-sensitive hypertension. In fact, multiple studies have shown that increases in non-renal vascular resistance are unable to make BP salt-sensitive in the absence of kidney dysfunction.12-15,26,27,62
Additional observations that question whether primary vascular dysfunction is required for salt-sensitive hypertension are 1) increased salt intake in various forms of salt-sensitive hypertension (e.g. AngII hypertension) causes hypertension even after genetic deletion of non-renal vascular effects, and 2) decreasing TPR to normal by infusion of vasodilators or by opening an AV fistula, did not prevent DOCA-salt hypertension.97,98
Technical and conceptual challenges in determining mechanisms of salt-induced hypertension from measurements of CO and BP
In most clinical and experimental studies, BP and CO are measured for only a few minutes under resting conditions during a control period before an experimental manipulation such as increasing salt intake, and then during the experimental period. TPR is calculated from BP and CO measurements and inferences are made regarding whether changes in BP are due to changes in CO or TPR9,99 (Figure 5). A major limitation of this approach is that BP and CO are rapidly changing throughout the day with various activities and it is unlikely that casual measurements of these variable can adequately represent the average changes throughout the day or small, dynamic differences, especially when changes are transient such as during increased salt intake.
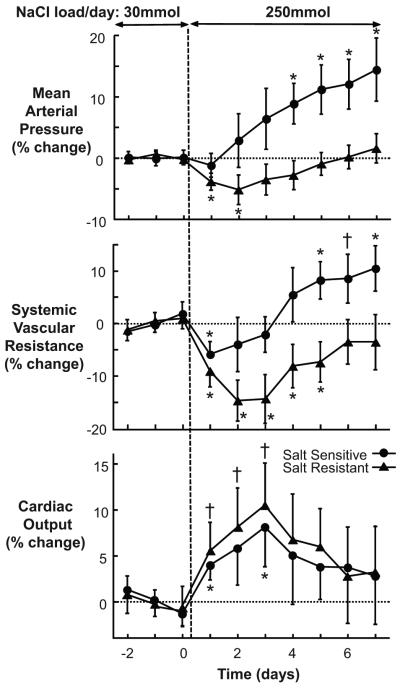
Figure 5.
Time course of changes in mean arterial pressure (MAP), systemic vascular resistance (SVR), and cardiac output when NaCl intake was raised from 30 to 250 mmol/day in salt-resistant (SR, ▴) and salt-sensitive (SS, •) subjects. Values are shown as percent change from baseline (average of day 5 through 7 of 30 mmol/day NaCl intake). *P<0.01 and †P<0.05, respectively, compared with low-salt period. Responses of MAP and SVR to NaCl loading differ significantly in SS versus SR subjects from day 2. Responses of CO did not differ between groups and CO was not significantly different than baseline values after 4 days. Note that SVR increased significantly in salt-sensitive, compared to baseline, only after MAP increased. Also note that SVR was not significantly different, compared to baseline values, in SR subjects after 6 days. Baseline values for SS and SR subjects were not provided in the paper. Data are from Schmidlin et al.9
Another limitation is the accuracy of CO measurements when CO is assessed with methods such as impedance cardiography which may have a variability of 9-11% when compared to more direct methods such an electromagnetic flowmeter.100 Studies that have assessed CO by impedance cardiography during salt loading in humans, including those by Morris and colleagues, have generally found only transient increases in CO that are 10% or less9,99 (Figure 5). Moreover, increased TPR in these studies generally follows, rather than precedes, increased BP after a few days of salt loading. Unless CO is measured continuously and with great accuracy, small transient changes that occur with salt loading are difficult to discern.
More important, although CO or TPR may be elevated at various stages of salt-induced increases in BP, neither of these variables is a primary long-term controller of BP. Instead, CO and TPR are the effectors of a complex system in which the set-point is determined by intrarenal and extrarenal factors that ultimately influence renal-pressure natriuresis and insure that salt and water balances are maintained. Unless the heart is weakened or metabolic needs of the tissues are altered, CO is maintained relatively constant, despite kidney dysfunction or salt loading, and TPR usually follows BP. Hypertensive disorders associated with primary increases in vascular resistance (e.g. PDE3A mutations) have not been shown to be salt-sensitive.
Changes in vascular resistance certainly play a crucial role in moment-to-moment BP regulation, especially in emergency circumstances such as severe hemorrhage. A minimal level of vascular resistance and adequate cardiac function are required for normal long-term BP regulation. However, primary changes in TPR that are not accompanied by changes in the relationship between BP and renal salt/water excretion (renal-pressure natriuresis/diuresis) have not been shown to cause salt-sensitivity or to change the long-term level of BP.
Summary and Conclusions
Chronic high salt intake increases the risk for hypertension and moderation of salt intake is an important strategy for preventing cardiovascular and kidney disease, especially in salt-sensitive subjects. BP salt-sensitivity is a highly variable, continuous phenotype and may worsen with aging and kidney injury if high salt intake is maintained chronically.
Kidney dysfunction, characterized by impaired pressure natriuresis, has been demonstrated in all forms of experimental and human genetic or acquired salt-sensitive hypertension studied thus far. Experimental models and monogenic forms of salt–sensitive hypertension have abnormalities of kidney function that directly or indirectly increase NaCl reabsorption, decrease glomerular capillary filtration coefficient, or cause nephron injury/loss.
Vascular dysfunction may occur concomitantly or secondarily to increased BP in salt-sensitive hypertension, but increases in non-renal vascular resistance have not been shown to increase BP salt-sensitivity unless renal-pressure natriuresis is impaired. The mechanisms by which high salt intake increases TPR are not fully understood but may involve multiple factors including pressure-dependent and flow-dependent autoregulation, and neurohormonal factors that occur concomitantly with kidney dysfunction. The fact that hypertension-associated vascular changes usually regress when renal excretory function is improved and BP is reduced also suggests that increased TPR and vascular dysfunction are often secondary to hypertension. Although CO or TPR may be elevated in salt-sensitive hypertension, neither of these variables is a primary long-term controller of BP. Instead, CO and TPR are the effectors of a complex system in which the set-point is determined by intrarenal and extrarenal factors that ultimately influence kidney function and insure that salt/water balance is maintained.
Supplementary Material
Acknowledgments
I gratefully acknowledge Arthur Guyton as well as current and former colleagues at the University of Mississippi Medical Center for their many contributions to the concepts discussed in this review, and for their collaborations with our experimental studies.
FUNDING SOURCES: The author’s research was supported by grants from the National Heart, Lung, and Blood Institute (P01 HL51971) and the National Institute of General Medical Sciences (P20 GM104357) of the National Institutes of Health.
Footnotes
DISCLOSURES: None.
References
- 1.Appel LJ, Frohlich ED, Hall JE, Pearson TA, Sacco RL, Seals DR, Sacks FM, Smith SC, Jr., Vafiadis DK, Van Horn LV. The importance of population-wide sodium reduction as a means to prevent cardiovascular disease and stroke: a call to action from the American Heart Association. Circulation. 2011;123:1138–1143. doi: 10.1161/CIR.0b013e31820d0793. [DOI] [PubMed] [Google Scholar]
- 2.Whelton PK, Appel LJ, Sacco RL, Anderson CA, Antman EM, Campbell N, Dunbar SB, Frohlich ED, Hall JE, Jessup M, Labarthe DR, MacGregor GA, Sacks FM, Stamler J, Vafiadis DK, Van Horn LV. Sodium, blood pressure, and cardiovascular disease: further evidence supporting the American Heart Association sodium reduction recommendations. Circulation. 2012;126:2880–2889. doi: 10.1161/CIR.0b013e318279acbf. [DOI] [PubMed] [Google Scholar]
- 3.He FJ, MacGregor GA. Effect of modest salt reduction on blood pressure: a meta-analysis of randomized trials. Implications for public health. J Hum Hypertens. 2002;16:761–770. doi: 10.1038/sj.jhh.1001459. [DOI] [PubMed] [Google Scholar]
- 4.Kotchen TA, Cowley AW, Jr., Frohlich ED. Salt in health and disease--a delicate balance. N Engl J Med. 2013;368:1229–1237. doi: 10.1056/NEJMra1212606. [DOI] [PubMed] [Google Scholar]
- 5.Kotchen TA, Luke RG, Ott CE, Galla JH, Whitescarver S. Effect of chloride on renin and blood pressure responses to sodium chloride. Ann Intern Med. 1983;98:817–822. doi: 10.7326/0003-4819-98-5-817. [DOI] [PubMed] [Google Scholar]
- 6.Whitescarver SA, Ott CE, Jackson BA, Guthrie GP, Jr., Kotchen TA. Salt-sensitive hypertension: contribution of chloride. Science. 1984;223:1430–1432. doi: 10.1126/science.6322303. [DOI] [PubMed] [Google Scholar]
- 7.Schmidlin O, Forman A, Sebastian A, Morris RC., Jr. Sodium-selective salt sensitivity: its occurrence in blacks. Hypertension. 2007;50:1085–1092. doi: 10.1161/HYPERTENSIONAHA.107.091694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kurtz TW, Al-Bander HA, Morris RC., Jr. "Salt-sensitive" essential hypertension in men. Is the sodium ion alone important? N Engl J Med. 1987;317:1043–1048. doi: 10.1056/NEJM198710223171702. [DOI] [PubMed] [Google Scholar]
- 9.Schmidlin O, Sebastian AF, Morris RC., Jr. What initiates the pressor effect of salt in salt-sensitive humans? Observations in normotensive blacks. Hypertension. 2007;49:1032–1039. doi: 10.1161/HYPERTENSIONAHA.106.084640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kawasaki T, Delea CS, Bartter FC, Smith H. The effect of high-sodium and low-sodium intakes on blood pressure and other related variables in human subjects with idiopathic hypertension. Am J Med. 1978;64:193–198. doi: 10.1016/0002-9343(78)90045-1. [DOI] [PubMed] [Google Scholar]
- 11.Kurtz TW, Dominiczak AF, DiCarlo SE, Pravenec M, Morris RC., Jr. Molecular-based mechanisms of Mendelian forms of salt-dependent hypertension: questioning the prevailing theory. Hypertension. 2015;65:932–941. doi: 10.1161/HYPERTENSIONAHA.114.05092. [DOI] [PubMed] [Google Scholar]
- 12.Guyton AC. Circulatory Physiology III. WB Saunders; Philadelphia: 1980. Arterial pressure and hypertension; pp. 1–564. [Google Scholar]
- 13.Hall JE. The kidney, hypertension, and obesity. Hypertension. 2003;41:625–633. doi: 10.1161/01.HYP.0000052314.95497.78. [DOI] [PubMed] [Google Scholar]
- 14.Cowley AW., Jr. Long-term control of arterial blood pressure. Physiol Rev. 1992;72:231–300. doi: 10.1152/physrev.1992.72.1.231. [DOI] [PubMed] [Google Scholar]
- 15.Cowley AW., Jr. The concept of autoregulation of total blood flow and its role in hypertension. Am J Med. 1980;68:906–916. doi: 10.1016/0002-9343(80)90225-9. [DOI] [PubMed] [Google Scholar]
- 16.Weinberger MH. Salt sensitivity of blood pressure in humans. Hypertension. 1996;27:481–490. doi: 10.1161/01.hyp.27.3.481. [DOI] [PubMed] [Google Scholar]
- 17.Felder RA, White MJ, Williams SM, Jose PA. Diagnostic tools for hypertension and salt sensitivity testing. Curr Opin Nephrol Hypertens. 2013;22:65–76. doi: 10.1097/MNH.0b013e32835b3693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bertram JF, Douglas-Denton RN, Diouf B, Hughson MD, Hoy WE. Human nephron number: implications for health and disease. Pediatr Nephrol. 2011;26:1529–1533. doi: 10.1007/s00467-011-1843-8. [DOI] [PubMed] [Google Scholar]
- 19.Frohlich ED. The salt conundrum: a hypothesis. Hypertension. 2007;50:161–166. doi: 10.1161/HYPERTENSIONAHA.107.088328. [DOI] [PubMed] [Google Scholar]
- 20.Hall JE, Mizelle HL, Hildebrandt DA, Brands MW. Abnormal pressure natriuresis. A cause or a consequence of hypertension? Hypertension. 1990;15:547–559. doi: 10.1161/01.hyp.15.6.547. [DOI] [PubMed] [Google Scholar]
- 21.Rossier BC, Staub O, Hummler E. Genetic dissection of sodium and potassium transport along the aldosterone-sensitive distal nephron: importance in the control of blood pressure and hypertension. FEBS Lett. 2013;587:1929–1941. doi: 10.1016/j.febslet.2013.05.013. [DOI] [PubMed] [Google Scholar]
- 22.Lifton RP, Gharavi AG, Geller DS. Molecular mechanisms of human hypertension. Cell. 2001;104:545–556. doi: 10.1016/s0092-8674(01)00241-0. [DOI] [PubMed] [Google Scholar]
- 23.O'Shaughnessy KM, Karet FE. Salt handling and hypertension. J Clin Invest. 2004;113:1075–1081. doi: 10.1172/JCI21560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Guyton AC, Coleman TG, Granger HJ. Circulation: overall regulation. Annu Rev Physiol. 1972;34:13–46. doi: 10.1146/annurev.ph.34.030172.000305. [DOI] [PubMed] [Google Scholar]
- 25.Linz P, Santoro D, Renz W, Rieger J, Ruehle A, Ruff J, Deimling M, Rakova N, Muller DN, Luft FC, Titze J, Niendorf T. Skin sodium measured with 23Na MRI at 7.0 T. NMR Biomed. 2015;28:54–62. doi: 10.1002/nbm.3224. [DOI] [PubMed] [Google Scholar]
- 26.Guyton AC. The surprising kidney-fluid mechanism for pressure control--its infinite gain! Hypertension. 1990;16:725–730. doi: 10.1161/01.hyp.16.6.725. [DOI] [PubMed] [Google Scholar]
- 27.Hall JE, Guyton AC, Brands MW. Pressure-volume regulation in hypertension. Kidney Int Suppl. 1996;55:S35–S41. [PubMed] [Google Scholar]
- 28.Hall JE, Guyton AC, Smith MJ, Jr., Coleman TG. Blood pressure and renal function during chronic changes in sodium intake: role of angiotensin. Am J Physiol. 1980;239:F271–F280. doi: 10.1152/ajprenal.1980.239.3.F271. [DOI] [PubMed] [Google Scholar]
- 29.Hall JE, Granger JP, do Carmo JM, da Silva AA, Dubinion J, George E, Hamza S, Speed J, Hall ME. Hypertension: physiology and pathophysiology. Compr Physiol. 2012;2:2393–2442. doi: 10.1002/cphy.c110058. [DOI] [PubMed] [Google Scholar]
- 30.Hall JE, Mizelle HL, Brands MW, Hildebrandt DA. Pressure natriuresis and angiotensin II in reduced kidney mass, salt-induced hypertension. Am J Physiol. 1992;262:R61–R71. doi: 10.1152/ajpregu.1992.262.1.R61. [DOI] [PubMed] [Google Scholar]
- 31.Omvik P, Tarazi RC, Bravo EL. Regulation of sodium balance in hypertension. Hypertension. 1980;2:515–523. doi: 10.1161/01.hyp.2.4.515. [DOI] [PubMed] [Google Scholar]
- 32.Averina VA, Othmer HG, Fink GD, Osborn JW. A mathematical model of salt-sensitive hypertension: the neurogenic hypothesis. J Physiol. 2015;593:3065–3075. doi: 10.1113/jphysiol.2014.278317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Mizelle HL, Montani JP, Hester RL, Didlake RH, Hall JE. Role of pressure natriuresis in long-term control of renal electrolyte excretion. Hypertension. 1993;22:102–110. doi: 10.1161/01.hyp.22.1.102. [DOI] [PubMed] [Google Scholar]
- 34.Hall JE, Granger JP, Smith MJ, Jr., Premen AJ. Role of renal hemodynamics and arterial pressure in aldosterone "escape". Hypertension. 1984;6:I183–I192. doi: 10.1161/01.hyp.6.2_pt_2.i183. [DOI] [PubMed] [Google Scholar]
- 35.Hall JE, Granger JP, Hester RL, Coleman TG, Smith MJ, Jr., Cross RB. Mechanisms of escape from sodium retention during angiotensin II hypertension. Am J Physiol. 1984;246:F627–F634. doi: 10.1152/ajprenal.1984.246.5.F627. [DOI] [PubMed] [Google Scholar]
- 36.Hall JE, Montani JP, Woods LL, Mizelle HL. Renal escape from vasopressin: role of pressure diuresis. Am J Physiol. 1986;250:F907–F916. doi: 10.1152/ajprenal.1986.250.5.F907. [DOI] [PubMed] [Google Scholar]
- 37.Hall JE, Mizelle HL, Woods LL, Montani JP. Pressure natriuresis and control of arterial pressure during chronic norepinephrine infusion. J Hypertens. 1988;6:723–731. doi: 10.1097/00004872-198809000-00006. [DOI] [PubMed] [Google Scholar]
- 38.Woods LL, Mizelle HL, Hall JE. Control of sodium excretion in NE-ACTH hypertension: role of pressure natriuresis. Am J Physiol. 1988;255:R894–R900. doi: 10.1152/ajpregu.1988.255.6.R894. [DOI] [PubMed] [Google Scholar]
- 39.Brands MW, Hall JE. Renal perfusion pressure is an important determinant of sodium and calcium excretion in DOC-salt hypertension. Am J Hypertens. 1998;11:1199–1207. doi: 10.1016/s0895-7061(98)00031-4. [DOI] [PubMed] [Google Scholar]
- 40.Passmore JC, Whitescarver SA, Ott CE, Kotchen TA. Importance of chloride for deoxycorticosterone acetate-salt hypertension in the rat. Hypertension. 1985;7:I115–I120. doi: 10.1161/01.hyp.7.3_pt_2.i115. [DOI] [PubMed] [Google Scholar]
- 41.Schrier RW, Howard RL. Unifying hypothesis of sodium and water regulation in health and disease. Hypertension. 1991;18:III164–III168. doi: 10.1161/01.hyp.18.5_suppl.iii164. [DOI] [PubMed] [Google Scholar]
- 42.Hyndman KA, Boesen EI, Elmarakby AA, Brands MW, Huang P, Kohan DE, Pollock DM, Pollock JS. Renal collecting duct NOS1 maintains fluid-electrolyte homeostasis and blood pressure. Hypertension. 2013;62:91–98. doi: 10.1161/HYPERTENSIONAHA.113.01291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ge Y, Bagnall A, Stricklett PK, Webb D, Kotelevtsev Y, Kohan DE. Combined knockout of collecting duct endothelin A and B receptors causes hypertension and sodium retention. Am J Physiol Renal Physiol. 2008;295:F1635–F1640. doi: 10.1152/ajprenal.90279.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ge Y, Bagnall A, Stricklett PK, Strait K, Webb DJ, Kotelevtsev Y, Kohan DE. Collecting duct-specific knockout of the endothelin B receptor causes hypertension and sodium retention. Am J Physiol Renal Physiol. 2006;291:F1274–F1280. doi: 10.1152/ajprenal.00190.2006. [DOI] [PubMed] [Google Scholar]
- 45.Ahn D, Ge Y, Stricklett PK, Gill P, Taylor D, Hughes AK, Yanagisawa M, Miller L, Nelson RD, Kohan DE. Collecting duct-specific knockout of endothelin-1 causes hypertension and sodium retention. J Clin Invest. 2004;114:504–511. doi: 10.1172/JCI21064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Ramkumar N, Ying J, Stuart D, Kohan DE. Overexpression of Renin in the collecting duct causes elevated blood pressure. Am J Hypertens. 2013;26:965–972. doi: 10.1093/ajh/hpt071. [DOI] [PubMed] [Google Scholar]
- 47.Jacques T, Picard N, Miller RL, Riemondy KA, Houillier P, Sohet F, Ramakrishnan SK, Busst CJ, Jayat M, Corniere N, Hassan H, Aronson PS, Hennings JC, Hubner CA, Nelson RD, Chambrey R, Eladari D. Overexpression of pendrin in intercalated cells produces chloride-sensitive hypertension. J Am Soc Nephrol. 2013;24:1104–1113. doi: 10.1681/ASN.2012080787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Cowley AW, Jr., Abe M, Mori T, O'Connor PM, Ohsaki Y, Zheleznova NN. Reactive oxygen species as important determinants of medullary flow, sodium excretion, and hypertension. Am J Physiol Renal Physiol. 2015;308:F179–F197. doi: 10.1152/ajprenal.00455.2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Ying J, Stuart D, Hillas E, Gociman BR, Ramkumar N, Lalouel JM, Kohan DE. Overexpression of mouse angiotensinogen in renal proximal tubule causes salt-sensitive hypertension in mice. Am J Hypertens. 2012;25:684–689. doi: 10.1038/ajh.2012.16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Pavlov TS, Levchenko V, O'Connor PM, Ilatovskaya DV, Palygin O, Mori T, Mattson DL, Sorokin A, Lombard JH, Cowley AW, Jr., Staruschenko A. Deficiency of renal cortical EGF increases ENaC activity and contributes to salt-sensitive hypertension. J Am Soc Nephrol. 2013;24:1053–1062. doi: 10.1681/ASN.2012080839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Langston JB, Guyton AC, Douglas BH, Dorsett PE. Effect of changes in salt intake on arterial pressure and renal function in partially nephrectomized dogs. Circ Res. 1963;12:508–512. [Google Scholar]
- 52.Carlström M, Wahlin N, Sallstrom J, Skott O, Brown R, Persson AE. Hydronephrosis causes salt-sensitive hypertension in rats. J Hypertens. 2006;24:1437–1443. doi: 10.1097/01.hjh.0000234126.78766.00. [DOI] [PubMed] [Google Scholar]
- 53.Carlström M, Sallstrom J, Skott O, Larsson E, Persson AE. Uninephrectomy in young age or chronic salt loading causes salt-sensitive hypertension in adult rats. Hypertension. 2007;49:1342–1350. doi: 10.1161/HYPERTENSIONAHA.107.087213. [DOI] [PubMed] [Google Scholar]
- 54.Johnson RJ, Lanaspa MA, Gabriela Sanchez-Lozada L, Rodriguez-Iturbe B. The discovery of hypertension: evolving views on the role of the kidneys, and current hot topics. Am J Physiol Renal Physiol. 2015;308:F167–F178. doi: 10.1152/ajprenal.00503.2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Konishi Y, Nishiyama A, Morikawa T, Kitabayashi C, Shibata M, Hamada M, Kishida M, Hitomi H, Kiyomoto H, Miyashita T, Mori N, Urushihara M, Kobori H, Imanishi M. Relationship between urinary angiotensinogen and salt sensitivity of blood pressure in patients with IgA nephropathy. Hypertension. 2011;58:205–211. doi: 10.1161/HYPERTENSIONAHA.110.166843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Nguy L, Johansson ME, Grimberg E, Lundgren J, Teerlink T, Carlstrom M, Lundberg JO, Nilsson H, Guron G. Rats with adenine-induced chronic renal failure develop low-renin, salt-sensitive hypertension and increased aortic stiffness. Am J Physiol Regul Integr Comp Physiol. 2013;304:R744–R752. doi: 10.1152/ajpregu.00562.2012. [DOI] [PubMed] [Google Scholar]
- 57.Franco M, Tapia E, Bautista R, Pacheco U, Santamaria J, Quiroz Y, Johnson RJ, Rodriguez-Iturbe B. Impaired pressure natriuresis resulting in salt-sensitive hypertension is caused by tubulointerstitial immune cell infiltration in the kidney. Am J Physiol Renal Physiol. 2013;304:F982–F990. doi: 10.1152/ajprenal.00463.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Koomans HA, Roos JC, Boer P, Geyskes GG, Mees EJ. Salt sensitivity of blood pressure in chronic renal failure. Evidence for renal control of body fluid distribution in man. Hypertension. 1982;4:190–197. doi: 10.1161/01.hyp.4.2.190. [DOI] [PubMed] [Google Scholar]
- 59.Hall JE. Control of sodium excretion by angiotensin II: intrarenal mechanisms and blood pressure regulation. Am J Physiol. 1986;250:R960–R972. doi: 10.1152/ajpregu.1986.250.6.R960. [DOI] [PubMed] [Google Scholar]
- 60.Coffman TM, Crowley SD. Kidney in hypertension: Guyton redux. Hypertension. 2008;51:811–816. doi: 10.1161/HYPERTENSIONAHA.105.063636. [DOI] [PubMed] [Google Scholar]
- 61.Crowley SD, Coffman TM. The inextricable role of the kidney in hypertension. J Clin Invest. 2014;124:2341–2347. doi: 10.1172/JCI72274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Crowley SD, Gurley SB, Herrera MJ, Ruiz P, Griffiths R, Kumar AP, Kim HS, Smithies O, Le TH, Coffman TM. Angiotensin II causes hypertension and cardiac hypertrophy through its receptors in the kidney. Proc Natl Acad Sci U S A. 2006;103:17985–17990. doi: 10.1073/pnas.0605545103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Gurley SB, Riquier-Brison AD, Schnermann J, Sparks MA, Allen AM, Haase VH, Snouwaert JN, Le TH, McDonough AA, Koller BH, Coffman TM. AT1A angiotensin receptors in the renal proximal tubule regulate blood pressure. Cell Metab. 2011;13:469–475. doi: 10.1016/j.cmet.2011.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Sparks MA, Stegbauer J, Chen D, Gomez JA, Griffiths RC, Azad HA, Herrera M, Gurley SB, Coffman TM. Vascular Type 1A Angiotensin II Receptors Control BP by Regulating Renal Blood Flow and Urinary Sodium Excretion. J Am Soc Nephrol. 2015 Apr;:8. doi: 10.1681/ASN.2014080816. doi: ASN. 2014080816 [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Nishimoto M, Fujita T. Renal mechanisms of salt-sensitive hypertension: contribution of two steroid receptor-associated pathways. Am J Physiol Renal Physiol. 2015;308:F377–F387. doi: 10.1152/ajprenal.00477.2013. [DOI] [PubMed] [Google Scholar]
- 66.Kohan DE. Role of collecting duct endothelin in control of renal function and blood pressure. Am J Physiol Regul Integr Comp Physiol. 2013;305:R659–R668. doi: 10.1152/ajpregu.00345.2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Kohan DE, Rossi NF, Inscho EW, Pollock DM. Regulation of blood pressure and salt homeostasis by endothelin. Physiol Rev. 2011;91:1–77. doi: 10.1152/physrev.00060.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Speed JS, Heimlich JB, Hyndman KA, Fox BM, Patel V, Yanagisawa M, Pollock JS, Titze JM, Pollock DM. Endothelin-1 as a master regulator of whole-body Na+ homeostasis. FASEB J. 2015 Aug;:12. doi: 10.1096/fj.15-276584. pii: fj.15-276584 [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Rettig R, Grisk O. The kidney as a determinant of genetic hypertension: evidence from renal transplantation studies. Hypertension. 2005;46:463–468. doi: 10.1161/01.HYP.0000178189.68229.8a. [DOI] [PubMed] [Google Scholar]
- 70.Dahl LK, Heine M. Primary role of renal homografts in setting chronic blood pressure levels in rats. Circ Res. 1975;36:692–696. doi: 10.1161/01.res.36.6.692. [DOI] [PubMed] [Google Scholar]
- 71.Bianchi G, Fox U, Di Francesco GF, Giovanetti AM, Pagetti D. Blood pressure changes produced by kidney cross-transplantation between spontaneously hypertensive rats and normotensive rats. Clin Sci Mol Med. 1974;47:435–448. doi: 10.1042/cs0470435. [DOI] [PubMed] [Google Scholar]
- 72.Heller J, Schubert G, Havlickova J, Thurau K. The role of the kidney in the development of hypertension: a transplantation study in the Prague hypertensive rat. Pflugers Arch. 1993;425:208–212. doi: 10.1007/BF00374168. [DOI] [PubMed] [Google Scholar]
- 73.Kawabe K, Watanabe TX, Shiono K, Sokabe H. Influence on blood pressure of renal isografts between spontaneously hypertensive and normotensive rats, utilizing the F1 hybrids. Jpn Heart J. 1978;19:886–894. doi: 10.1536/ihj.19.886. [DOI] [PubMed] [Google Scholar]
- 74.Greene AS, Yu ZY, Roman RJ, Cowley AW., Jr. Role of blood volume expansion in Dahl rat model of hypertension. Am J Physiol. 1990;258:H508–H514. doi: 10.1152/ajpheart.1990.258.2.H508. [DOI] [PubMed] [Google Scholar]
- 75.Krieger JE, Cowley AW., Jr. Prevention of salt angiotensin II hypertension by servo control of body water. Am J Physiol. 1990;258:H994–1003. doi: 10.1152/ajpheart.1990.258.4.H994. [DOI] [PubMed] [Google Scholar]
- 76.Hoorn EJ, Nelson JH, McCormick JA, Ellison DH. The WNK kinase network regulating sodium, potassium, and blood pressure. J Am Soc Nephrol. 2011;22:605–614. doi: 10.1681/ASN.2010080827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Palermo M, Cossu M, Shackleton CH. Cure of apparent mineralocorticoid excess by kidney transplantation. N Engl J Med. 1998;339:1787–1788. doi: 10.1056/NEJM199812103392414. [DOI] [PubMed] [Google Scholar]
- 78.Khattab AM, Shackleton CH, Hughes BA, Bodalia JB, New MI. Remission of hypertension and electrolyte abnormalities following renal transplantation in a patient with apparent mineralocorticoid excess well documented throughout childhood. J Pediatr Endocrinol Metab. 2014;27:17–21. doi: 10.1515/jpem-2013-0235. [DOI] [PubMed] [Google Scholar]
- 79.Botero-Velez M, Curtis JJ, Warnock DG. Brief report: Liddle's syndrome revisited--a disorder of sodium reabsorption in the distal tubule. N Engl J Med. 1994;330:178–181. doi: 10.1056/NEJM199401203300305. [DOI] [PubMed] [Google Scholar]
- 80.Curtis JJ, Luke RG, Dustan HP, Kashgarian M, Whelchel JD, Jones P, Diethelm AG. Remission of essential hypertension after renal transplantation. N Engl J Med. 1983;309:1009–1015. doi: 10.1056/NEJM198310273091702. [DOI] [PubMed] [Google Scholar]
- 81.Guidi E, Menghetti D, Milani S, Montagnino G, Palazzi P, Bianchi G. Hypertension may be transplanted with the kidney in humans: a long-term historical prospective follow-up of recipients grafted with kidneys coming from donors with or without hypertension in their families. J Am Soc Nephrol. 1996;7:1131–1138. doi: 10.1681/ASN.V781131. [DOI] [PubMed] [Google Scholar]
- 82.Carlström M, Wilcox CS, Arendshorst WJ. Renal autoregulation in health and disease. Physiol Rev. 2015;95:405–511. doi: 10.1152/physrev.00042.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Chapman K, Holmes M, Seckl J. 11beta-hydroxysteroid dehydrogenases: intracellular gate-keepers of tissue glucocorticoid action. Physiol Rev. 2013;93:1139–1206. doi: 10.1152/physrev.00020.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Ramkumar N, Stuart D, Rees S, Hoek AV, Sigmund CD, Kohan DE. Collecting duct-specific knockout of renin attenuates angiotensin II-induced hypertension. Am J Physiol Renal Physiol. 2014;307:F931–F938. doi: 10.1152/ajprenal.00367.2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Lalioti MD, Zhang J, Volkman HM, Kahle KT, Hoffmann KE, Toka HR, Nelson-Williams C, Ellison DH, Flavell R, Booth CJ, Lu Y, Geller DS, Lifton RP. Wnk4 controls blood pressure and potassium homeostasis via regulation of mass and activity of the distal convoluted tubule. Nat Genet. 2006;38:1124–1132. doi: 10.1038/ng1877. [DOI] [PubMed] [Google Scholar]
- 86.Zhang J, Patel MB, Griffiths R, Mao A, Song YS, Karlovich NS, Sparks MA, Jin H, Wu M, Lin EE, Crowley SD. Tumor necrosis factor-alpha produced in the kidney contributes to angiotensin II-dependent hypertension. Hypertension. 2014;64:1275–1281. doi: 10.1161/HYPERTENSIONAHA.114.03863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.DiBona GF, Esler M. Translational medicine: the antihypertensive effect of renal denervation. Am J Physiol Regul Integr Comp Physiol. 2010;298:R245–R253. doi: 10.1152/ajpregu.00647.2009. [DOI] [PubMed] [Google Scholar]
- 88.Henegar JR, Zhang Y, Rama RD, Hata C, Hall ME, Hall JE. Catheter-based radiorefrequency renal denervation lowers blood pressure in obese hypertensive dogs. Am J Hypertens. 2014;27:1285–1292. doi: 10.1093/ajh/hpu048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Frohlich ED, Schnaper HW, Wilson IM, Freis ED. Hemodynamic alterations in hypertensive patients due to chlorothiazide. N Engl J Med. 1960;262:1261–1263. doi: 10.1056/NEJM196006232622502. [DOI] [PubMed] [Google Scholar]
- 90.Pickkers P, Hughes AD, Russel FG, Thien T, Smits P. Thiazide-induced vasodilation in humans is mediated by potassium channel activation. Hypertension. 1998;32:1071–1076. doi: 10.1161/01.hyp.32.6.1071. [DOI] [PubMed] [Google Scholar]
- 91.Bennett WM, McDonald WJ, Kuehnel E, Hartnett MN, Porter GA. Do diuretics have antihypertensive properties independent of natriuresis? Clin Pharmacol Ther. 1977;22:499–504. [PubMed] [Google Scholar]
- 92.Mukherjee SK, Katz MA, Michael UF, Ogden DA. Mechanisms of hemodynamic actions of furosemide: differentiation of vascular and renal effects on blood pressure in functionally anephric hypertensive patients. Am Heart J. 1981;101:313–318. doi: 10.1016/0002-8703(81)90196-4. [DOI] [PubMed] [Google Scholar]
- 93.Hall JE. Renal function in one-kidney, one-clip hypertension and low renin essential hypertension. Am J Hypertens. 1991;4:523S–533S. doi: 10.1093/ajh/4.10.523s. [DOI] [PubMed] [Google Scholar]
- 94.Toka O, Tank J, Schachterle C, Aydin A, Maass PG, Elitok S, Bartels-Klein E, Hollfinger I, Lindschau C, Mai K, Boschmann M, Rahn G, Movsesian MA, Muller T, Doescher A, Gnoth S, Muhl A, Toka HR, Wefeld-Neuenfeld Y, Utz W, Topper A, Jordan J, Schulz-Menger J, Klussmann E, Bahring S, Luft FC. Clinical Effects of Phosphodiesterase 3A Mutations in Inherited Hypertension With Brachydactyly. Hypertension. 2015;66:800–808. doi: 10.1161/HYPERTENSIONAHA.115.06000. [DOI] [PubMed] [Google Scholar]
- 95.Jordan J, Toka HR, Heusser K, Toka O, Shannon JR, Tank J, Diedrich A, Stabroth C, Stoffels M, Naraghi R, Oelkers W, Schuster H, Schobel HP, Haller H, Luft FC. Severely impaired baroreflex-buffering in patients with monogenic hypertension and neurovascular contact. Circulation. 2000;102:2611–2618. doi: 10.1161/01.cir.102.21.2611. [DOI] [PubMed] [Google Scholar]
- 96.Schuster H, Toka O, Toka HR, Busjahn A, Oztekin O, Wienker TF, Bilginturan N, Bahring S, Skrabal F, Haller H, Luft FC. A cross-over medication trial for patients with autosomal-dominant hypertension with brachydactyly. Kidney Int. 1998;53:167–172. doi: 10.1046/j.1523-1755.1998.00732.x. [DOI] [PubMed] [Google Scholar]
- 97.Huang M, Hester RL, Coleman TG, Smith MJ, Guyton AC. Development of hypertension in animals with reduced total peripheral resistance. Hypertension. 1992;20:828–833. doi: 10.1161/01.hyp.20.6.828. [DOI] [PubMed] [Google Scholar]
- 98.Huang M, Hester RL, Guyton AC, Norman RA., Jr. Hemodynamic studies in DOCA-salt hypertensive rats after opening of an arteriovenous fistula. Am J Physiol. 1992;262:H1802–H1808. doi: 10.1152/ajpheart.1992.262.6.H1802. [DOI] [PubMed] [Google Scholar]
- 99.Schmidlin O, Forman A, Leone A, Sebastian A, Morris RC., Jr. Salt sensitivity in blacks: evidence that the initial pressor effect of NaCl involves inhibition of vasodilatation by asymmetrical dimethylarginine. Hypertension. 2011;58:380–385. doi: 10.1161/HYPERTENSIONAHA.111.170175. [DOI] [PubMed] [Google Scholar]
- 100.White SW, Quail AW, de Leeuw PW, Traugott FM, Brown WJ, Porges WL, Cottee DB. Impedance cardiography for cardiac output measurement: an evaluation of accuracy and limitations. Eur Heart J. 1990;11(Suppl I):79–92. doi: 10.1093/eurheartj/11.suppl_i.79. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.