Abstract
Objective Through colonoscopy, polyps can be identified and removed to reduce colorectal cancer incidence and mortality. Appropriate use of surveillance colonoscopy, post polypectomy, is a focus of healthcare reform.
Materials and Methods The authors developed and implemented the first electronic medical record–based colonoscopy reporting system (CoRS) that matches endoscopic findings with guideline-consistent surveillance recommendations and generates tailored results and recommendation letters for patients and providers.
Results In its first year, CoRS was used in 98.6% of indicated cases. Via a survey, colonoscopists agreed/strongly agreed it is easy to use (83%), provides guideline-based recommendations (89%), improves quality of Spanish letters (94%), they would recommend it for other institutions (78%), and it made their work easier (61%), and led to improved practice (56%).
Discussion CoRS’ widespread adoption and acceptance likely resulted from stakeholder engagement throughout the development and implementation process.
Conclusion CoRS is well-accepted by clinicians and provides guideline-based recommendations and results communications to patients and providers.
Keywords: colonoscopy, decision support, tailored intervention, surveillance
INTRODUCTION
Colorectal cancer is the second leading cause of cancer death worldwide.1 Colonoscopy begins a process2 whereby adenomatous polyps can be identified early and removed to reduce incidence and mortality.3,4 Effectiveness of this process is limited by suboptimal rates of surveillance among patients with precancerous polyps; those with advanced adenomas often fail to receive follow-up colonoscopy within 5 years.5 There is evidence of both under and over-use (e.g., repeat colonoscopy sooner than recommended among those with low-risk findings, such as nonadenomatous polyps).5,6 Using Medicare claims data, Goodwin et al.7 found >30% of patients had repeat colonoscopy ≤5 years of a normal baseline although guidelines recommend 10 years. Many gastroenterologists lack knowledge about or ignore recommendations for surveillance colonoscopy intervals.8 Overuse is problematic because of safety risks (potential bleeding, perforation), costs of the procedure, lost work days9 and cause of potential delays among patients for whom the procedure would provide greater value.
BACKGROUND
A major focus of healthcare reform is appropriate use of medical procedures, including reduction of unneeded procedures. Appropriate colonoscopy surveillance intervals are included in the Centers for Medicare and Medicaid Services 2014 Physician Quality Reporting System measures and the American Gastroenterological Association’s Choosing Wisely campaign. Surveillance intervals will continue to be monitored, particularly as reimbursement becomes increasingly tied to quality measures.
Researchers have developed decision support tools to match findings with follow-up recommendations. Some are “designed to be embedded into electronic medical records (EMRs), to facilitate access at point of care”10 but none has gone to the next step of generating tailored reports of recommendations to patients and referring physicians. Primary providers may only get a copy of the post-procedure colonoscopy report with vague recommendations (“follow-up in 3–5 years”) or no advice (“follow-up pending pathology results”). Patients may not know their findings and follow-up recommendations because they do not receive timely reports or do not understand what they receive, especially if English is not their first language. Through our NCI-funded Parkland-UT Southwestern PROSPR Center,2 we developed and implemented a colonoscopy reporting system (CoRS) to address these needs.
MATERIALS AND METHODS
System Development
The novel, provider-friendly Parkland-UT Southwestern Colonoscopic Reporting System uses the NoteWriter feature in Epic Epic Systems Corporation, Verona, WI. CoRS is written in XML layout, hosted by a Visual Basic control that saves to a data base that runs in Massachusetts General Hospital Utility Multi-Programming System. The system provides: 1) decision facilitation, 2) follow-up recommendation documentation, and 3) generation of tailored recommendation reports for patients and referring providers. It is driven by cascading questions in pull-down menus (Figure 1). Data are recorded in the EMR and used by tailoring algorithms to create a letter for each patient and the referring provider that summarizes findings and corresponding recommendations.
Figure 1:
Parkland-UT Southwestern CoRS screen shot.
Workflow
Colonoscopists access pathology through Epic’s In Basket, then click buttons to answer questions about these variables that determine appropriate recommendations (Figure 1): (a) indication (screening, surveillance, diagnostic), (b) intubation of cecum, (c) bowel prep quality, (d) family history, (e) number of polyps, and (f) “worst” finding on pathology. For a hyperplastic polyp and a large tubular adenoma, the worst finding is “1 cm or larger adenoma.” If adenomas are present, colonoscopists specify whether high-grade dysplasia and/or villous/tubulovillous histology is present. For large adenomas, users specify whether the polyp was removed piecemeal.
Computerized Decision Support
A tailoring algorithm in the NoteWriter function uses collected data to generate a report of findings and colonoscopy recommendation based on guidelines from Winawer et al.11and Lieberman et al.12 It selects “repeat colonoscopy in 5 years” for patients whose worst pathologic finding is a single small adenomatous polyp and “repeat colonoscopy in 3–6 months” for patients with piecemeal resection of a large polyp or without cecal intubation. When there is flexibility in recommendations, a choice of guideline-based intervals is displayed. For example, because US Multi-Society Task Force on Colorectal Cancer guidelines recommend repeat colonoscopy any time within 3 years among patients with 10 or more adenomatous polyps, colonoscopists choose colonoscopy in 3–6 months, 1, 2, or 3 years (but not 5 or 10). To avoid overuse, users can override surveillance recommendations if they believe repeat colonoscopy is not indicated due to age or comorbid conditions. Once completed, CoRS generates a progress note documenting colonoscopy findings and recommendations in the EMR. This information is then available to all specialty providers, the primary care physician, and colonoscopist.
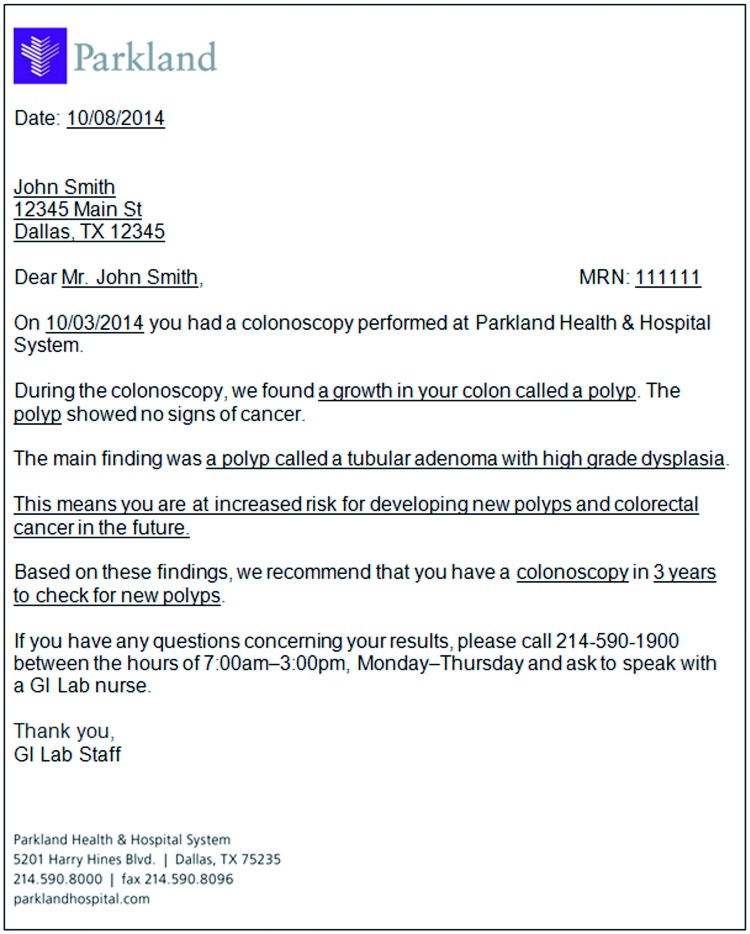
To generate the tailored letter, users click on a letter template. Findings and recommendations automatically generate a simple-language English and Spanish letter for the referring provider and patient (Figure 2). Patient letters are printed by administrative staff and sent via US mail. Providers’ versions are routed to electronic inboxes.
Figure 2:
Tailored results reporting and recommendation letter.
Tailored Recommendation Letters
Prior to CoRS, reporting letters had varied in wording and thoroughness. Spanish versions were often generated by a computer translation program without checks for accuracy or clarity. For CoRS letters, health communications experts generated a tailored message library13 of low-literacy English versions of tailored text for every potential finding and ensured the messages flowed seamlessly, regardless of which messages preceded or followed. We used a language validation iterative process11 of forward/backward translation, evaluation by a committee of Spanish speakers from different countries, and cognitive testing with low-literacy English and Spanish speakers.14
Figure 2 shows a sample tailored letter, with standard content in plain text and content from the tailored message library underlined. Figure 3 shows the corresponding tailoring algorithm flow diagram illustrating how each piece of text was selected from the message library for this one scenario. In this there was ≥ polyp, size of the largest was ≥ 1 cm, and the resection was piecemeal, indicating need for repeat colonoscopy in 3–6 months.
Figure 3:
CoRS algorithm.
A table of all tailoring algorithms, illustrating how responses to each CoRS question were linked to guidelines and how each piece of text was selected from the tailored letter message library, can be found in an online Appendix.
Stakeholder Engagement
As recommended by Fisher15 and others, CoRS was developed with stakeholder engagement of gastroenterology (GI) faculty, fellows, and laboratory staff; institutional leadership; primary-care providers; and information technology (IT) staff. GI faculty and fellows provided input about question content and order, response options, algorithms that link these responses to re-screening and surveillance guidelines, and wording for tailored message text. GI laboratory staff and primary-care providers suggested how reports should be transferred to In Baskets. IT staff advised about feasible methods for using responses to generate tailored reporting letters and developed the system over an 18-month period. Patients pre-tested the tailored messages via cognitive interviews to ensure understandability and conceptual equivalence in English and Spanish.16
Implementation and Evaluation
In December 2013, the system was implemented for all colonoscopies performed at Parkland involving polyp removal or biopsy. Because GI faculty and fellows were initially skeptical about whether using CoRS would disrupt work flow and whether they could trust accuracy of the algorithms, we wondered whether they would use and come to trust it. An anonymous survey used a 5-point Likert scale to assess extent of agreement the system: 1) is easy to use, 2) disrupts work flow, 3) has led to improvement in screening practice, 4) produces guideline-based recommendations, 5) makes your work easier, 6) improves quality of Spanish-language letters, and 7) is something you would recommend for other institutions? To determine rate of adoption and whether it improved over time, we compared total colonoscopies involving polyp removal (denominator) with the number for which CoRS was used (numerator) at 6 and 12 months post implementation. To assess whether CoRS was adopted by providers and if adoption increased over time, we calculated usage rates at 6 and 12 months post implementation.
RESULTS
Patient Characteristics and Colonoscopic Findings
Most patients for whom CoRS was used were female (55.9%) and minority (38.9% Hispanic, 35.5% African American; Table 1).
Table 2:
Physician reactions to CoRS
| To what extent do you agree that the NoteWriter… | Strongly Agree/Agree, n (%) | Neutral, n (%) | Disagree/Strongly Disagree, n (%) |
|---|---|---|---|
| Is easy to use? | 15 (83.3) | 1 (5.6) | 2 (11.1) |
| Disrupts your work flow? | 2 (11.1) | 4 (22.2) | 12 (66.7) |
| Has led to improvement in the colorectal Cancer screening practice? | 10 (55.6) | 8 (44.4) | 0 (0.0) |
| Produces guideline-based follow-up recommendations? | 16 (88.9) | 1 (5.6) | 1 (5.6) |
| Makes your work easier?a | 11 (61.1) | 5 (27.8) | 1 (5.6) |
| Improves quality of Spanish-language letters to patients? | 17 (94.4) | 1 (5.6) | 0 (0.0) |
| Is something you would recommend for adoption at other institutions? | 14 (77.8) | 4 (22.2) | 0 (0.0) |
aOne participant did not respond.
Table 1:
Patient Characteristics
| Overall N = 673 | |
|---|---|
| Sex, n (%) | |
| Female | 376 (55.9) |
| Male | 297 (44.1) |
| Race, n (%) | |
| White | 388 (57.7) |
| Black | 239 (35.5) |
| Asian | 38 (5.6) |
| American Indian | 1 (0.1) |
| Other Pacific Islander | 3 (0.4) |
| Unknown | 4 (0.6) |
| Ethnicity, n (%) | |
| Hispanic | 262 (38.9) |
| Non-Hispanic | 405 (60.2) |
| Unknown | 6 (0.9) |
Recorded indication for colonoscopy was: 44.5% diagnostic; 24.3% screening; 21.3% surveillance. Nearly all (97.5%) were complete to the cecum; 84.1% had good/excellent prep. Polyps were found in 626 patients. Most common worst finding (43.8%) was 1–2 tubular adenoma(s) <1 cm.
Colonoscopists’ Reactions to the System
We achieved a 6-month survey response rate of 100% among the 18 providers who used CoRS.
As shown in Table 2, more than three quarters of these colonoscopists indicated the system is easy-to-use (83.3%), provides guideline-based follow-up recommendations (88.9%), improves quality of Spanish letters (94.4%), and they would recommend adoption at other institutions (77.8%). Most (55.6%) agreed it improved screening practice and made work easier.
Adoption of CoRS at 6 and 12 months
During the first 6 months of implementation, 1775 colonoscopies were performed, of which 804 (45.3%) had polyp removal. CoRS was used for 673 (83.7%) of these cases. Utilization rose from 83.7% during the first 6-month period to 98.6% during the latter 6 months.
DISCUSSION
During a time when appropriate use of colorectal cancer surveillance is increasingly scrutinized, Parkland-UT Southwestern CoRS is an EMR-based module facilitating reporting and guideline-based recommendations for patients undergoing polypectomy. Despite complex risk assessment and surveillance recommendations, CoRS minimized user burden by including only a few questions and eliminating the need for dictating or typing free text. CoRS uniquely extends beyond decision support to include tailored communication with providers and patients regarding results and guideline-based recommendations. Although previous colorectal cancer screening communications interventions have provided tailored content for individual recipients,17–20 ours is the first to use EMR information as tailoring data.
In addition to guideline-based recommendations, CoRS tracks cecal intubation rates, which are associated with colonoscopy quality and interval cancer risk. Previously these data existed as “free text” that required chart review or natural language processing (NLP) for extraction. Similarly, the system captures colonoscopy indication—important for clinical care, reimbursement, healthcare quality reporting, and research.
Early and extensive stakeholder engagement of primary-care providers, GI faculty and fellows, the IT team, and patients was critical to the program’s successful implementation and helped ensure providers’ uptake and positive reactions.
Our evaluation of CoRS implementation has several limitations. First, it occurred within a single center. Although results may not be generalized to other practice settings, we believe it would be equally successful given the high agreement for acceptance among providers who used the program. Second, CoRS is only used for reporting polyp pathology to date; providers continue to use nontailored letters for normal findings, nonpolyp colonoscopy pathology, and any upper endoscopy pathology results. However, we are expanding its use to patients without polyps and/or biopsies to help facilitate tracking of adenoma detection rates. Third, although CoRS has potential to reduce disparities in cancer outcomes by generating tailored, simple-language letters to patients with low literacy and those whose primary language is Spanish—those historically less likely to complete the screening process4,21–23 and are at elevated risk for adverse outcomes24–27—studies are needed to characterize impact of improved communication on outcomes such as patient adherence with recommendations.
A final potential limitation of CoRS is that the system is not fully automated. Generation of tailored letters and guideline-based recommendations requires manual input from providers rather than employing NLP to read directly from pathology reports and other data sources. Our current NLP capabilities are not sophisticated enough to capture information within and outside of the patient record with high enough specificity to ensure accurate capture of essential elements. Future improvements in standardization of reports, including obtaining them through Health Level 7 International interfaces rather than blobs of text, might remedy this situation. However, with or without NLP to generate recommendations, responsible clinicians must review colonoscopy and pathology findings and “sign off” on recommendations; our approach takes advantage of this required professional responsibility with minimal additional burden.
Overall, the Parkland-UT Southwestern CoRS is novel and addresses an important issue in the colorectal cancer screening process. Given its success at Parkland, we are adapting it for implementation at the University of Texas Southwestern Medical Center. We believe CoRS could be easily implemented at many other EMR-based systems in the future.
FUNDING
This work was supported by the National Institutes of Health, grant number UL1TR001105; Cancer Center Support Grant, grant number P30 CA142543; and National Institutes of Health/National Cancer Institute, grant number U54 CA163308.
COMPETING INTEREST
The authors have no competing interests to declare.
CONTRIBUTORS
Drs Skinner, Mayorga, Gupta, Agrawal, Moran, and Singal and Ms. Bishop, Mr. Wright and Ms. McCallister contributed to the conception and design.
Drs Skinner, Gupta, Halm, and Singal, and Ms. McCallister, Bishop, and Sanders contributed to the analysis and interpretation of the data.
Drs Skinner, Gupta, Halm, and Singal, and Ms. McCallister and Mr. Wright contributed to the drafting of the article.
Drs Santini, Mayorga, Agrawal, and Moran, and Ms. Bishop contributed critical revision of the article for important intellectual content.
All authors submitted final approval of the article.
SUPPLEMENTARY MATERIAL
Supplementary material is available online at http://jamia.oxfordjournals.org/.
REFERENCES
- 1.American Cancer Society. Cancer Facts & Figures 2013. Atlanta, GA: American Cancer Society; 2013. [Google Scholar]
- 2.Tiro JA, Kamineni A, Levin TR, et al. The colorectal cancer screening process in community settings: a conceptual model for the population-based research optimizing screening through personalized regimens consortium. Cancer Epidemiol Biomarkers Prev. 2014;23(7):1147–1158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Shapiro JA, Klabunde CN, Thompson TD, Nadel MR, Seeff LC, White A. Patterns of colorectal cancer test use, including CT colonography, in the 2010 National Health Interview Survey. Cancer Epidemiol Biomarkers Prev. 2012;21(6):895–904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Klabunde CN, Cronin KA, Breen N, Waldron WR, Ambs AH, Nadel MR. Trends in colorectal cancer test use among vulnerable populations in the United States. Cancer Epidemiol Biomarkers Prev. 2011;20(8):1611–1621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Schoen RE, Pinsky PF, Weissfeld JL, et al. Utilization of surveillance colonoscopy in community practice. Gastroenterology. 2010;138(1):73–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Shah TU, Voils CI, McNeil R, Wu R, Fisher DA. Understanding gastroenterologist adherence to polyp surveillance guidelines. Am J Gastroenterol. 2012;107(9):1283–1287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Goodwin JS, Singh A, Reddy N, Riall TS, Kuo YF. Overuse of screening colonoscopy in the Medicare population. Arch Intern Med. 2011;171(15):1335–1343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Saini SD, Nayak RS, Kuhn L, Schoenfeld P. Why don't gastroenterologists follow colon polyp surveillance guidelines?: results of a national survey. J Clin Gastroenterol. 2009;43(6):554–558. [DOI] [PubMed] [Google Scholar]
- 9.Saini SD, Schoenfeld P, Vijan S. Surveillance colonoscopy is cost-effective for patients with adenomas who are at high risk of colorectal cancer. Gastroenterology. 2010;138(7):2292–2299. [DOI] [PubMed] [Google Scholar]
- 10.Lieberman DA. Colon polyp surveillance: clinical decision tool. Gastroenterology. 2014;146(1):305–306. [DOI] [PubMed] [Google Scholar]
- 11.Winawer SJ, Zauber AG, Fletcher RH, et al. Guidelines for colonoscopy surveillance after polypectomy: a consensus update by the US Multi-Society Task Force on Colorectal Cancer and the American Cancer Society. CA: A Cancer J Clin. 2006;56(3):143–159. [DOI] [PubMed] [Google Scholar]
- 12.Lieberman DA, Rex DK, Winawer SJ, Giardiello FM, Johnson DA, Levin TR. Guidelines for colonoscopy surveillance after screening and polypectomy: a consensus update by the US Multi-Society Task Force on Colorectal Cancer. Gastroenterology. 2012;143(3):844–857. [DOI] [PubMed] [Google Scholar]
- 13.Kreuter MW, Farrell D. Tailoring Health Messages: Customizing Communication with Computer Technology. Mahwah, NJ: L. Erlbaum; 2000. [Google Scholar]
- 14.Bishop WP, Tiro JA, Melhado TV, Stevens C, Lee SC, Skinner CS. Evaluating the validity of health literacy items in English- and Spanish-speaking Hispanics from a community registry. Am J Public Health. 2012;2012. [Google Scholar]
- 15.Fisher DA. Electronic medical records and improving the quality of the screening process. J Gen Intern Med. 2011;26(7):683–684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Willis GB. Cognitive Interviewing: A Tool for Improving Questionnaire Design. Thousand Oaks, CA: Sage Publications; 2004. [Google Scholar]
- 17.Lipkus I. Increasing colorectal cancer screening among individuals in the carpentry trade: test of risk communication intervention. Prev Med. 2004;37(5):513–519. [DOI] [PubMed] [Google Scholar]
- 18.Skinner CS, Rawl SM, Moser BK, et al. Impact of the cancer risk intake system on patient-clinician discussions of tamoxifen, genetic counseling, and colonoscopy. J Gen Intern Med. 2005;20(4):360–365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rawl SM, Skinner CS, Perkins SM, et al. Computer-delivered tailored intervention improves colon cancer screening knowledge and health beliefs of African-Americans. Health Educ Res. 2012;27(5):868–885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lowery JT, Horick N, Kinney AY, et al. A randomized trial to increase colonoscopy screening in members of high-risk families in the colorectal cancer family registry and cancer genetics network. Cancer Epidemiol Biomarkers Prev. 2014;23(4):601–610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.James TM, Greiner KA, Ellerbeck EF, Feng C, Ahluwalia JS. Disparities in colorectal cancer screening: a guideline-based analysis of adherence. Ethn Dis. 2007;16(1):228–233. [PubMed] [Google Scholar]
- 22.Centers for Disease Control and Prevention. Vital Signs: Colorectal Cancer Screening Test Use – United States, 2012. MMWR Morb Mortal Wkly Rep. 2013;62(44):881–888. [PMC free article] [PubMed] [Google Scholar]
- 23.Gupta S, Sussman DA, Doubeni CA, et al. Challenges and possible solutions to colorectal cancer screening for the underserved. J Natl Cancer Inst. 2014;106(4):dju032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chien C, Morimoto LM, Tom J, Li CI. Differences in colorectal carcinoma stage and survival by race and ethnicity. Cancer. 2005;104(3):629–639. [DOI] [PubMed] [Google Scholar]
- 25.Kauh J, Brawley OW, Berger M. Racial disparities in colorectal cancer. Curr Probl Cancer. 2007;31(3):123–133. [DOI] [PubMed] [Google Scholar]
- 26.Siegel R, Naishadham D, Jemal A. Cancer statistics, 2012. CA: A Cancer J Clin. 2012;62(1):10–29. [DOI] [PubMed] [Google Scholar]
- 27.Aizer AA, Wilhite TJ, Chen MH, et al. Lack of reduction in racial disparities in cancer-specific mortality over a 20-year period. Cancer. 2014;120(10):1532–1539. [DOI] [PubMed] [Google Scholar]