Abstract
Evidence supports the potential for e-prescribing to reduce the incidence of adverse drug events (ADEs) in hospital-based studies, but studies in the ambulatory setting have not used occurrence of ADE as their outcome. Using the “prescription origin code” in 2011 Medicare Part D prescription drug events files, the authors investigate whether physicians who meet the meaningful use stage 2 threshold for e-prescribing (≥50% of prescriptions e-prescribed) have lower rates of ADEs among their diabetic patients. Risk of any patient with diabetes in the provider’s panel having an ADE from anti-diabetic medications was modeled adjusted for prescriber and patient panel characteristics. Physician e-prescribing to Medicare beneficiaries was associated with reduced risk of ADEs among their diabetes patients (Odds Ratio: 0.95; 95% CI, 0.94-0.96), as were several prescriber and panel characteristics. However, these physicians treated fewer patients from disadvantaged populations.
Keywords: electronic prescribing, adverse drug events, Medicare Part D
INTRODUCTION
Growth in electronic health record (EHR) adoption has the potential to lead to improved health care quality, efficiency, and outcomes.1–3 Electronic prescribing (e-prescribing) is one of the features of EHRs that has shown benefit by reducing adverse drug events (ADEs).1 The evidence suggests that e-prescribing can affect the incidence of ADEs either by helping providers send accurate, error-free, and legible prescriptions to pharmacies4 or by providing decision support to prevent drug–drug or drug–disease interactions. These studies, however, are predominantly hospital-based.5 The few prior studies done in the ambulatory setting have not studied the outcome of actual adverse events.6 We would expect to see a large impact of e-prescribing on ADEs in the ambulatory setting since e-prescribing can also help to increase patient medication adherence. In fact, in the ambulatory setting, 28% of paper prescriptions never make it to the pharmacy. A recent study found that e-prescribing increased the number of prescriptions that make it to the pharmacy by 12%, and increased the number of prescriptions picked up by the patients by 10%.7
After Meaningful Use (MU) objectives in 2010 made e-prescribing a requirement, the Centers for Medicare and Medicaid Services (CMS) began requiring that source of the original prescription (handwritten, e-prescribed, etc.) be reported on prescription drug events (PDEs) submitted to CMS. This new data element and the increase in proportion of physicians e-prescribing through an EHR, from 7% in 2008 to 50% in 2012,8 creates an opportunity to study whether e-prescribing is associated with fewer ADEs in the ambulatory setting.
ADEs are of particular concern among Medicare beneficiaries due to the high incidence of chronic disease and polypharmacy among beneficiaries, especially those with diabetes. Anti-diabetic agents, such as insulin and oral hypoglycemic agents, are the most common cause of ADEs9 and are in the top five causes of inpatient and treat-and-release emergency department (ED) visits for drug-related adverse events.10,11 The objective of this study is to investigate whether physicians who meet the MU stage 2 threshold for e-prescribing have lower rates of ADEs among their diabetic patients. We describe differences between prescribers who met MU Stage 2 e-prescribing threshold (50% of all prescriptions e-prescribed) in 2011 and report whether there was a lower likelihood of an ADE in patients of high e-prescribers.
METHODS
DATA SOURCE
We used claims from 2011 Medicare Parts A, B, and D for all fee-for-service Part D beneficiaries 65 years or older with any type of diabetes and at least 90-days supply of anti-diabetic medication. 100% Medicare 2011 Medicare Part A and B claims data, Part D PDE data, Medicare beneficiary enrollment data, and Part D Prescriber Characteristics data were used. Medicare Part A data includes inpatient hospital, skilled nursing facilities, hospice care, and home health claims. Part B data includes claims for ambulatory care visits and other medically-necessary services. Part D includes prescription claims information for data from nearly 28 million Medicare beneficiaries.12 The primary exposure variable is the percent of prescriptions e-prescribed based upon the “Prescription Origin Code,” which designates the origin of a prescription as written, telephone, electronic, or facsimile.
STUDY SAMPLE
Diabetes Patient Sample
Medicare beneficiaries with 12 months of full coverage with Medicare Part A, B, and D, aged 65 or older, alive for the entire study year, and with a Chronic Condition Warehouse flag for diabetes and at least a 90-day supply of an anti-hyperglycemic (diabetes) medication were included. The analysis did not include Medicare Advantage participants. The First Databank’s Generic Therapeutic Classification system was used to identify anti-hyperglycemics (value of ‘72’) and the subclasses of diabetes medications based on the most common use indicator.13
Prescriber Sample
The prescribers in this study were limited to those who prescribed diabetes medications to at least five beneficiaries with diabetes and excluded those above the 95th percentile in diabetic patient volume to exclude any groups billing under a single identifier. Prescriber panels were created by including any patient for whom the clinician prescribed an anti-diabetes medication. Thirteen percent of patients appeared in more than one prescriber’s panel. Prescriber’s e-prescribing status was defined based upon Part D claims from all of their Medicare Part D beneficiaries, which was highly correlated with their diabetes prescribing but more precise because it is based on a larger volume of prescriptions and is consistent with MU criteria. The percentages of prescriptions e-prescribed were skewed with many zeros and a small number of prescribers with a very high percentage. After testing several cutpoints, we opted to dichotomize prescribers into high e-prescribers (with 50% or more of their beneficiaries’ prescription claims e-prescribed) and low because the 50% cutpoint corresponds to the MU Stage 2 EHR Incentive Payment Program core requirement.14
OUTCOME VARIABLE
The primary ADE outcome variable is if any patient with diabetes in the provider’s panel had a hospital or ED visit with a diagnosis indicating a hypoglycemic event or an ADE from insulin or antidiabetic medications (e.g., poisoning, insulin pump failure, or unspecified adverse effect). These are based on a subset of ICD-9 codes used in an algorithm provided by the Agency for Healthcare Research and Quality for ADEs to identify hypoglycemic events and ADEs from antidiabetic medications: 24930–31, 24980–81, 2510–12, 25030–33, 25080–83, 9623, 99 523, 99 657, E9323.10
INDEPENDENT VARIABLES
In addition to high vs. low e-prescribing, we categorized prescribers according to age, gender, prescriber specialty (based on the Healthcare Provider Taxonomy Code Set),15 rurality of practice, and size of their diabetes patient panel. Each patient panel was characterized by average beneficiary age, average Hierarchical Condition Category (HCC) risk score, percentage female and percentage race/ethnicity (white, black, Hispanic, other),16 and percentage of panel that received low-income subsidy as a proxy for low income.
ANALYSIS
Risk of any patient with diabetes in the provider’s panel having a hospital or ED visit for an ADE from anti-diabetic medications or a hypoglycemic event was modeled using logistic regression weighted for panel size. Covariates included provider characteristics (age, gender, specialty, and rural/urban location) and patient panel characteristics (average age, gender, race/ethnicity, low-income subsidy status, and average HCC risk score).17 As a sensitivity analysis, the model was run excluding beneficiaries who appeared in more than one physician panel. We conducted analyses using SAS Enterprise Guide version 5.1 in SAS(R) 9.3. Tests of statistical significance in analyses were conducted at the 0.05 level.
RESULTS
Of the 129 507 providers included, 25% were high e-prescribers in 2011. Five percent of high e-prescribers had at least one patient with an ADE, compared to 6.5% of low e-prescribers (7.9% and 9.4% weighted for panel size). As shown in Table 1, high e-prescribers were younger, more likely to be female and work in metropolitan areas. Patient panels did not differ by patient gender, age, or type of medications taken (31% of beneficiaries took insulin and 48% took sulfonylureas). High e-prescriber panels were less likely to be majority low income (30% vs. 39%), had fewer Black (10% vs. 13%) and Hispanic (8% vs. 11%) patients, and had lower comorbidity (HCC score of 1.5 vs. 1.6). All differences had P < .01.
Table 1.
Provider and panel characteristics of high and low e-prescribers in 2011 Medicare Part D who prescribe to beneficiaries with diabetes
| High E-Prescribers (n = 31 917) | Low E-Prescribers (n = 97 590) | ||
|---|---|---|---|
| Provider characteristics | Number (%)/mean ± SD | Number (%)/mean ± SD | P-value |
| Female | 13 783 (43%) | 32,894(34%) | < .0001 |
| Age (years) | 49 ± 10 | 52 ± 11 | < .0001 |
| Claims E-Prescribed (mean %) | 66 ± 15% | 16 ± 17% | < .0001 |
| Specialty Type | |||
| Internal Medicine/Family Medicine | 25 753 (81) | 78 482 (80) | |
| Emergency Medicine | 80 (<1) | 497 (1) | |
| Nurse Practitioner/Physician Assistant | 4775 (15) | 11 424 (12) | |
| Specialist | 375 (1) | 2286 (2) | |
| All Other | 934 (3) | 4901 (5) | < .0001 |
| Area Type | |||
| Rural | 1963 (6) | 8254 (9) | |
| Micropolitan | 3624 (11) | 11 142 (11) | |
| Metropolitan | 26 208 (82) | 77 312 (79) | |
| Unknown | 122 (<1) | 882 (1) | < .0001 |
| Patient panel characteristics | |||
|---|---|---|---|
| No. of panels (%)/panel mean ± SD | No. of panels (%) panel mean ± SD | ||
| Diabetic patient panel size | |||
| 5–7 patients | 7835(25) | 21 420 (22) | |
| 8–10 | 5456(17) | 15 153 (16) | |
| 11–15 | 6361(20) | 17 853 (18) | |
| 16–24 | 6510(20) | 20 267 (21) | |
| 25+ | 5779(18) | 22 873 (23) | < .0001 |
| Average percentage female (%) | 60% ± 18 | 60% ± 18 | <.0001 |
| Average panel age (years) | 75 ± 2.7 | 75 ± 3.0 | < .0001 |
| Comorbidity: (Average Panel HCC Score) | 1.5 ± 0.4 | 1.6 ± 0.5 | < .0001 |
| Average panel percentage race | |||
| White (%) | 75% ± 30 | 70% ± 33 | < .0001 |
| Black (%) | 10% ± 19 | 13% ± 22 | < .0001 |
| Other (%) | 6% ± 17 | 6% ± 15 | < .02 |
| Hispanic (%) | 8% ± 18 | 11% ± 23 | < .0001 |
| Panel income level (Average Percentage Receiving Low Income Subsidy) | |||
| 0–25% (highest average income) | 12 626 (40) | 32 374 (33) | |
| 25–50% | 9798 (31) | 27 224 (28) | |
| 50–75% | 4863 (15) | 17 254 (18) | |
| 75–100% (lowest average income) | 4641 (15) | 20 727 (21) | < .0001 |
| Adverse drug event in Panel | |||
|---|---|---|---|
| Total number of ADEs (count) | 1794 | 6669 | |
| ADE rate per 1000 | 3.45 ± 0.02 | 3.99 ± 0.02 | .0002 |
| At least one ADE in panel (unweighted %) | 5.3% ± 0.22 | 6.5% ± 0.25 | < .0001 |
| At least one ADE in panel (weighted by panel size %) | 7.9% ± 1.1 | 9.4% ± 1.2 | < .0001 |
HCC- Hierarchical Condition Category; LIS- Low Income Subsidy.
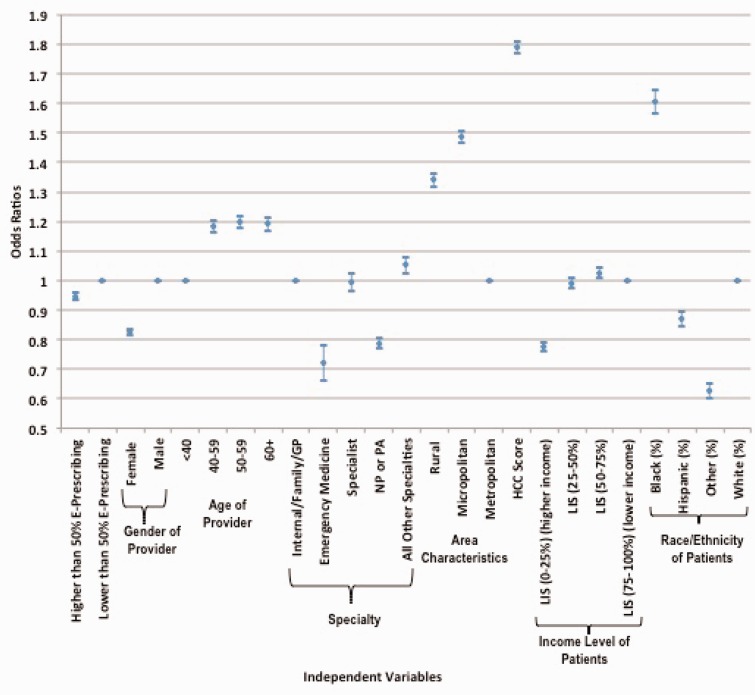
In the physician-level model controlling for provider and patient panel characteristics, high e-prescribers were significantly less likely to have any patient hospitalized or have an ED visit for an ADE (OR: 0.95; 95% CI, 0.94-0.96). Providers who were women, younger, or practiced in rural areas were less likely to have an ADE in their panel (see Figure 1), while providers with a sicker panel of patients or more low income patients had greater risk of ADEs. Having a panel with a higher proportion black patients was associated with greater likelihood of ADEs (OR: 1.61; 95% CI, 1.6-1.7), while proportion of Hispanics in the panel was associated with lower risk (OR: 0.87; 95% CI, 0.85-0.90). The results were not sensitive to exclusion of patients who were in more than one prescriber panel.
Figure 1:
Logistic regression showing association of prescribing provider and patient panel characteristics with occurrence of a hospitalization or ED visit for an ADE among Medicare Part D beneficiaries with diabetes.
DISCUSSION
Ambulatory EHR adoption in the United States has surged in recent years, concurrent with implementation of the Health Information Technology for Economic and Clinical Health Act that is designed to support adoption and MU of EHRs; and ensuring that the benefits EHRs accrue to all patient populations is a national priority.18 We found that the occurrence of ADEs among patients with diabetes is lower in association with clinicians doing the majority of their prescriptions electronically, but not all groups of patients are equally served by high e-prescribing clinicians. In addition, other physician and patient panel characteristics were independently associated with risk of diabetes-related ADE.
The importance of patient factors, such as comorbidity and low income, highlights that e-prescribing will not address all the factors leading to ADEs. The mechanisms by which e-prescribing may influence ADE stem largely from the provider side of ADE prevention. At a minimum, e-prescribing helps providers to send error-free and legible prescriptions to pharmacies.4 E-prescribing capability is accompanied by varying degrees of decision support and drug interaction alerts. In a meta-analysis of studies prior to 2006,6 even with many e-prescribers (up to 50% of prescribers) not having any decision support, e-prescribing was associated with fewer prescription errors, and fewer potential and actual ADEs. Only three of the included studies were in the ambulatory setting, and none reported ADEs as an outcome. A fourth, more recent study, found that e-prescribing reduced prescription errors in community-based practices nearly sevenfold and eliminated prescription errors due to illegibility but also did not study outcomes.19 Our report suggests that there is a statistically significant although small association of e-prescribing in the ambulatory setting with lower risk of ADEs significant enough to result in a visit to the hospital or ED. The findings of this study support previous hospital-based findings that MU measures are associated with a reduction of ADEs.20
This study provides a first look at e-prescribing under MU and has several limitations. First, there may be residual confounding in the relationship between e-prescribing and ADE events based on potential unmeasured differences between the earlier adopters of e-prescribing and those not yet taking up this practice change. Follow-up studies in subsequent years will reveal whether the lower risk of ADEs remains associated with e-prescribing as more diverse clinicians uptake the behavior. Second, we focus the association of physician prescribing behavior with outcomes for a panel of patients, rather than the impact on individual patients who may be seeing multiple providers. Further studies will use hierarchical modeling to estimate effects for individuals and be able to account for multiple prescribers per individual and the independent effect of fragmentation of prescribing across providers. The last limitation is that the mechanism of the effect (error-free prescriptions versus decision-support or other mechanism) cannot be assessed with this data source alone.
In summary, e-prescribing to Medicare beneficiaries with diabetes is associated with reduced risk of hospital or ED visits for hypoglycemia or ADEs related to antidiabetic medications but many traditionally disadvantaged populations are less likely to receive prescriptions from a clinician who frequently e-prescribes. As more clinicians shift toward e-prescribing in the ambulatory environment, further evaluation should explore whether there are disparities by patient race and income in both access to e-prescribing providers and risk of ADEs.
FUNDING
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
COMPETING INTERESTS
None of the authors have any competing interests to declare.
CONTRIBUTORS
All five authors made substantial contributions to the conception or design of the work, acquisition, analysis, or interpretation of data for the work; and wrote or critically revised and approved the manuscript for publication.
ACKNOWLEDGEMENTS
All authors made substantial contribution to the manuscript (planning, analysis, writing, and editing). Christopher Powers had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis and he conducted and is responsible for the data analysis. No direct funding was provided for this study although investigators where either employees (Powers, Gabriel, Encinosa, Mostashari) of the Department for Health and Human Services or on an intergovernmental personnel agreement with the CMS (Bynum). The design and conduct of the study; collection, management, analysis, interpretation of the data, manuscript preparation, and the decision to submit the manuscript for publication were conducted by authors without input from HHS or CMS; the manuscript had to be cleared for submission by CMS prior to submission.
REFERENCES
- 1.Buntin MB, Burke MF, Hoaglin MC, et al. The benefits of health information technology: a review of the recent literature shows predominantly positive results. Health Aff. 2011;30(3):464-471. [DOI] [PubMed] [Google Scholar]
- 2.Goldzweig CL, Towfigh A, Maglione M, et al. Costs and benefits of health information technology: new trends from the literature. Health Aff. 2009;28(2):w282-w293. [DOI] [PubMed] [Google Scholar]
- 3.Chaudhry B, Wang J, Wu S, et al. Systematic review: impact of health information technology on quality, efficiency, and costs of medical care. Ann Int Med. 2006;144(10):742-752. [DOI] [PubMed] [Google Scholar]
- 4.Ryan J. Nuts and bolts of e-prescribing. Secondary Nuts and bolts of e-prescribing 2008. American Academy of Orthopaedic Surgeons. http://www.aaos.org/news/aaosnow/oct08/managing6.asp. Accessed April 15, 2015. [Google Scholar]
- 5.Tache SV, Sonnichsen A, Ashcroft DM. Prevalence of adverse drug events in ambulatory care: a systematic review. Ann Pharmacother 2011;45(7-8):977-989. [DOI] [PubMed] [Google Scholar]
- 6.Ammenwerth E, Schnell-Inderst P, Machan C, et al. The effect of electronic prescribing on medication errors and adverse drug events: a systematic review. J Am Med Inform Assoc 2008;15(5):585-600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Surescripts. E-Prescribing Shown to Improve Outcomes and Save Healthcare System Billions of Dollars. 2012. http://surescripts.com/news-center/press-releases/!content/212_eprescribing. Accessed April 15, 2015.
- 8.Hufstader M, Swain M, Furukawa MF. State Variation in E-Prescribing Trends in the United States. ONC Data Brief, no. 4 Washington, DC: Office of the National Coordinator for Health Information Technology, 2012. [Google Scholar]
- 9.Budnitz DS, Pollock DA, Weidenbach KN, et al. National surveillance of emergency department visits for outpatient adverse drug events. J Am Med Assoc. 2006;296(15):1858-1866. [DOI] [PubMed] [Google Scholar]
- 10.Lucado J, Paez K, Elixhauser A. Medication-related adverse outcomes in U.S. hospitals and emergency departments, 2008. Secondary Medication-Related Adverse Outcomes in U.S. Hospitals and Emergency Departments, 2008. http://www.hcup-us.ahrq.gov/reports/statbriefs/sb109.jsp. Accessed April 15, 2015. [Google Scholar]
- 11.Weiss A, Elixhauser A, Bae J, et al. Origin of Adverse Drug Events in U.S. Hospitals, 2011. Secondary Origin of Adverse Drug Events in U.S. Hospitals, 2011. http://www.hcup-us.ahrq.gov/reports/statbriefs/sb158.jsp. Accessed April 15, 2015. [Google Scholar]
- 12. The Medicare and Medicaid Statistical Supplement, 2011. Secondary The Medicare and Medicaid Statistical Supplement, 2011. http://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/MedicareMedicaidStatSupp/2011.html. Accessed April 15, 2015.
- 13.FDB MedKnowledge Database. Secondary FDB MedKnowledge Database 2013. http://www.fdbhealth.com/solutions. Accessed April 15, 2015.
- 14.Eligible Professionals Meaningful Use Core Measures. Secondary Eligible Professionals Meaningful Use Core Measures 2010. http://www.cms.gov/Regulations-and-Guidance/Legislation/EHRIncentivePrograms/downloads/4_e-prescribing.pdf. Accessed April 15, 2015.
- 15.Healthcare Provider Taxonomy Code Set. Secondary Healthcare Provider Taxonomy Code Set 2013. http://www.cms.gov/Medicare/Provider-Enrollment-and-Certification/MedicareProviderSupEnroll/Taxonomy.html. Accessed April 15, 2015.
- 16.Eicheldinger C, Bonito A. More accurate racial and ethnic codes for Medicare administrative data. Health care Financ Rev. 2008;29(3):27-42. [PMC free article] [PubMed] [Google Scholar]
- 17.Medicare Managed Care Manual Chapter 7 – Risk Adjustment. Secondary Medicare Managed Care Manual Chapter 7 – Risk Adjustment 2013. http://www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/downloads/mc86c07.pdf. Accessed April 15, 2015.
- 18.Federal Health Information Technology Strategic Plan, 2015-2020. http://www.healthit.gov/sites/default/files/federal-healthIT-strategic-plan-2014.pdf. Accessed April 15, 2015.
- 19.Kaushal R, Kern LM, Barron Y, et al. Electronic prescribing improves medication safety in community-based office practices. J Gen Intern Med 2010;25(6):530-536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Encinosa WE, Bae J. Meaningful Use IT reduces hospital-caused adverse drug events even at challenged hospitals. Healthcare. 2014;3(1):12-17. [DOI] [PubMed] [Google Scholar]