Abstract
Objective Mobile health (mHealth) interventions may improve diabetes outcomes, but require engagement. Little is known about what factors impede engagement, so the authors examined the relationship between patient factors and engagement in an mHealth medication adherence promotion intervention for low-income adults with type 2 diabetes (T2DM).
Materials and Methods Eighty patients with T2DM participated in a 3-month mHealth intervention called MEssaging for Diabetes that leveraged a mobile communications platform. Participants received daily text messages addressing and assessing medication adherence, and weekly interactive automated calls with adherence feedback and questions for problem solving. Longitudinal repeated measures analyses assessed the relationship between participants’ baseline characteristics and the probability of engaging with texts and calls.
Results On average, participants responded to 84.0% of texts and participated in 57.1% of calls. Compared to Whites, non-Whites had a 63% decreased relative odds (adjusted odds ratio [AOR] = 0.37, 95% confidence interval [CI], 0.19-0.73) of participating in calls. In addition, lower health literacy was associated with a decreased odds of participating in calls (AOR = 0.67, 95% CI, 0.46-0.99, P = .04), whereas older age ( Pnonlinear = .01) and more depressive symptoms (AOR = 0.62, 95% CI, 0.38-1.02, P = .059) trended toward a decreased odds of responding to texts.
Conclusions Racial/ethnic minorities, older adults, and persons with lower health literacy or more depressive symptoms appeared to be the least engaged in a mHealth intervention. To facilitate equitable intervention impact, future research should identify and address factors interfering with mHealth engagement.
Keywords: mHealth, patient engagement, medication adherence, type 2 diabetes mellitus, disparities
BACKGROUND AND SIGNIFICANCE
Among adults with type 2 diabetes (T2DM), nonadherence to medications is common, 1,2 especially among lower-income racial/ethnic minorities. 3,4 Medication nonadherence is associated with having worse glycemic control, 5,6 an increased risk of hospitalizations, 2,7 premature death, 2,7 and higher healthcare costs. 8 Despite nonadherence being more prevalent among minorities and low socioeconomic status (SES) groups, research aimed at understanding and improving medication adherence for these individuals has been limited. 9,10
Cell phones can deliver medication adherence support to patients with diabetes. Approximately 90% of US adults use cell phones, 11 and find it essential for daily functioning. 12 In 2013, secure messaging service (SMS) text messaging was the most common cell phone activity among all cell phone users, 11 and was used equally across racial/ethnic and socioeconomic groups. 11,13 However, only 9% of all cell phone users have ever received SMS updates or alerts about their health or medical issues, 14 making SMS an untapped channel for supporting patients.
SMS and Interactive Voice Response (IVR; a telephone technology that automates interactions with callers) have the potential to improve a variety of health behaviors and outcomes. 15 While SMS/IVR interventions have helped hard-to-reach and vulnerable patients around the world, 16 less is known about the benefits of these interventions for low SES racial/ethnic minorities in the United States. 17 A 2014 meta-analysis of 10 SMS intervention studies for T2DM patients ( n = 960) reported glycemic control improved, with a 44% effect size. 17 However, only 2 of the 10 studies were conducted in the United States, 18,19 with just one involving low SES community health center patients that improved patients’ self-efficacy, but not their glycemic control. 19 Not included in that meta-analysis was a 12-month SMS intervention study that enrolled 32 African Americans with T2DM from a community health center, and found a reduction in hospitalizations and emergency room visits only among patients who engaged with the intervention for 12 months. 20
Patient engagement is critical to reaping an intervention’s potential benefits, and varied use and/or nonuse may compromise intervention efficacy. While patients with diabetes rate mobile health (mHealth) interventions favorably, 21 patients often respond to less than or near 50% of an intervention’s SMS texts or IVR calls. 20,22 Given that low SES minorities with T2DM are more likely to be both nonadherent to medications and experience suboptimal diabetes outcomes, there is significant value in addressing what factors both limit and increase the likelihood of mHealth engagement among this population.
OBJECTIVE
The MEssaging for Diabetes (MED) intervention leveraged the SuperEgo mobile communications platform 23 to deliver one- and two-way text messages, and weekly IVR calls to promote medication adherence among low SES, diverse adults with T2DM. In a sample from the target population, we examined the relationship between patients’ demographic characteristics, health literacy skills, depressive symptoms, and clinical characteristics and the probability of engaging with the intervention over 3 months.
METHODS
MEssaging for Diabetes (MED)
The MED intervention was designed to improve medication adherence among low SES, diverse adults with T2DM. The MED intervention includes three components: 1) a unique, daily, one-way text message addressing user-specific barriers to medication adherence; 2) a daily, two-way text message asking if the user took all of his/her diabetes medications for the day, requesting a “yes” or “no” response; and 3) an automated weekly IVR call. The call consists of user-specific adherence feedback based on a user’s weekly aggregated responses to the daily, two-way text message inquiring about daily adherence, an encouraging message, and a series of problem solving questions intended to promote future adherence successes. The text message content and feasibility of MED was previously tested in a usability study, resulting in refinements and improvements to the intervention. 25 We used the SuperEgo mobile communications platform to tailor text messages based on integrated patient self-report of barriers to medication adherence, and to tailor the timing of text and voice communications based on participant preferences, 23 communicate with Twilio © to send text messages and integrate voice communication for the IVR functionality, calculate users’ barriers to adherence for the focus of communications, calculate weekly adherence rates from text messages used in the IVR feedback, and collect all mobile text and voice responses. 24 Leveraging the voice and SMS text messaging capabilities shared by all cell phones has the ability to reach the broadest range of cell phone users and has been shown to be a feasible and reliable modality for intervention delivery and data collection. 24
Sample and Recruitment
We conducted this research as part of a pilot study evaluating initial efficacy of the MED intervention on improving medication adherence and glycemic control among adults with T2DM. Participants were recruited from a Federally Qualified Health Center (FQHC) in Nashville, Tennessee. Through advertisements and assistance from clinic staff members, 80 eligible adult patients were recruited to participate in the study and completed informed consent (see Figure 1 ). Eligible patients were at least 18 years of age, English-speaking, diagnosed with T2DM, prescribed diabetes medication(s), owned a cell phone with SMS capability, and had a Social Security number. Exclusion criteria included a pre-existing diagnosis of dementia, auditory limitations (a requirement for IVR engagement), and the inability to see and respond to text messages. The Vanderbilt University Institutional Review Board approved all study procedures prior to enrollment.
Figure 1:
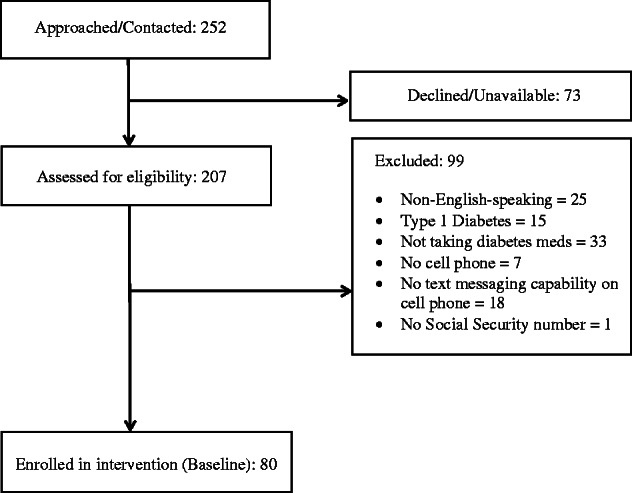
Flow chart of patient recruitment and enrollment.
Data and Procedures
At baseline, research assistants (RAs) administered informed consent to interested and eligible patients in a private clinic room. RAs verbally administered survey items and response options to collect patients’ self-reported demographic and health information (e.g., age, race/ethnicity, insulin status, years/months since a diabetes diagnosis), responses to widely used measures of health literacy and depressive symptoms, and responses to a barriers to medication adherence assessment. A clinic phlebotomist performed a blood drawn hemoglobin A1c (A1C) test to assess participants’ glycemic control. We included participants’ A1C results in our characterization of the sample.
Following the assessment, RAs entered participants’ responses to items assessing medication adherence barriers into SuperEgo’s web-based form, which identified each participant’s top 3 barriers to medication adherence out of 17 barriers based on response frequencies, and then delivered daily, one-way text messages to address each of these barriers. For the next three months, participants received daily and weekly MED intervention components (see intervention description above). During this time, RAs contacted participants monthly to reassess participants' barriers to adherence, input these data into SuperEgo’s web-based form, which would, in turn, update a participant's top 3 barriers to adherence as needed and change the intervention experience for that participant.
Over the course of three months, the SuperEgo platform tracked participants’ responses to daily, two-way adherence assessment text messages and participation in weekly IVR calls. For the latter, the system tracked whether participants answered each phone call and recorded their keypad and voice responses to the problem solving questions.
Measures
Demographic and clinical characteristics
We collected self-reported age, gender, race, ethnicity, income, education (i.e., years in school), insurance status, insulin status, and diabetes duration (i.e., years/months since a diabetes diagnosis).
Health literacy
The Brief Health Literacy Screen (BHLS) assessed health literacy, 26 and consists of three items. Two items ask, “How often do you have someone help you read hospital materials?” and, “How often do you have problems learning about your medical condition because of difficulty understanding written information?” Response options range from 1 = never to 5 = always. The third item asks, “How confident are you filling out medical forms by yourself?” Response options range from 1 = not at all to 5 = extremely. Responses to the first two items are reversed, and all three responses are summed to create a score ranging from 3 to 15, with higher scores indicating higher health literacy.
Depressive symptoms
The two-item Patient Health Questionnaire (PHQ-2) assessed depressive symptoms 27 by asking how often over the past two weeks, on a scale from 0 = not at all to 3 = nearly every day, a respondent has been bothered by, (1) “little interest or pleasure in doing things,” and (2) “feeling down, depressed, or hopeless.” Responses are summed to create a score ranging from 0 to 6, with higher scores indicating more depressive symptoms.
Engagement.
We assessed participants’ engagement with the intervention in two ways: responses to daily, two-way text messages, and participation in weekly IVR calls. Over the course of the intervention, participants were sent a total of ∼84 daily, two-way text messages (one text per day for 12 weeks) requesting a response of “yes” or “no” if all diabetes medications had been taken on a given day. We defined text message engagement as any participant response, including “yes,” “no,” or a different, unsolicited response. If a participant did not respond, it was coded as non-engagement for that day. The primary goal of sending the two-way text messages was to get an accurate assessment of participants’ daily adherence. Because of within- and between participant variability in the time of day they took their medications, we allowed participants to respond to the two-way text message at any time. All sent messages were time-stamped and each response was linked to the original sent message through a message thread. Participants could identify when the text message was sent through the message content (e.g., “On Mon, Feb. 25, did you take all your diabetes meds?”). Because the messages did not expire, participants could have responded to texts sent on a previous day. This allowed the possibility of participants responding to multiple messages at one time. However, 87.3% of sent text messages were responded to within 24 h and 8.7% were responded to within 48 h.
Additionally, participants received a total of ∼11 weekly IVR calls (one call per week for 11 weeks). If a participant missed the call, the system called back, one time, 1 h later. Additionally, a participant could call the system back before midnight to listen to his/her individualized adherence feedback and answer the call’s three problem solving questions (i.e., why were you successful taking your medications last week? and unsuccessful? and did you experience any technical issues receiving text messages?). After midnight of the day an IVR call was made, a participant could no longer listen to or respond to that week’s IVR call. We defined IVR engagement as answering (or returning) the call and providing a response to at least one of the three problem solving questions. If a participant did not both answer/return a given IVR call and provide a response to at least one question, it was coded as non-engagement for that week.
Analysis
Sample demographics and clinical characteristics were described using means and standard deviations ( ± SD), medians and interquartile ranges (IQR), or frequencies and percents as appropriate. Text responses were recorded daily and call participation was recorded weekly. The range of possible text responses was 0–84 (days) and the range of call participation was 0–11 (weeks). In univariate analyses, we calculated the rate of text responses and call participation by dividing each participant’s number of responses by the total number of calls/texts that he/she was sent throughout the course of the intervention. We applied two separate multivariable longitudinal binary response regression models to assess the association between observed patient characteristics and two outcomes: text responses and call participation. Predictors for the repeated measures logistic multivariable regression models included demographics (age, gender, race, and income), health literacy skills, depressive symptoms, duration of diabetes, and time (number of days for the text response model and number of weeks for the call participation model). Education was not included in the model because of potential collinearity with health literacy (Spearman’s rho correlation = 0.48). Robust covariance standard error estimates (i.e., Huber-White sandwich estimator) were applied to account for clustering of data (repeated measures). 28 We modeled age as a flexible smooth parameter using restricted cubic splines and graphically displayed the relationship with probability of text response after adjustment for covariates. All statistical analyses were performed using R version 3.1 (R Core Team, R Foundation for Statistical Computing, Vienna, Austria).
RESULTS
We enrolled 80 adults diagnosed with T2DM (see Table 1 ). The sociodemographics of the sample was comparable to the sociodemographics of the sample of patients from our prior work at this FQHC that was representative of the clinic population. 29 The current sample was on average 50.1 ± 10.5 years old; 54% were female, 69% were non-White (90.9% African American; 7.5% Hispanic.). Nearly two-thirds (70.1%) had annual household incomes less than $20 K; 56.3% had less than a high school degree or equivalent; and 82.5% were either uninsured or had public insurance. The sample’s average A1C was 8.2% (67 mmol/mol) ± 2.0%; 62.5% had suboptimal glycemic control (A1C ≥ 7.0%); and over half (63.8%) were prescribed insulin. Of those enrolled, 3 participants dropped out of the study during the 3-month intervention; 2 participants said they were annoyed with the text messages, and 1 participant passed away from reasons unrelated to the intervention.
Table 1:
Patient characteristics (N = 80)
| Variable | M ± SD or n (%) or IQR |
|---|---|
| Age, years | 50.08 ± 10.53 |
| Gender | |
| Male | 26 (32.5) |
| Female | 54 (67.5) |
| Race | |
| Caucasian/White | 25 (31.3) |
| Non-Caucasian/Non-White | 55 (68.75) |
| Education, years | 12.94 ± 2.29 |
| <High school graduate | 16 (20) |
| High school graduate | 29 (36.3) |
| >High school graduate | 35 (43.8) |
| Annual household income (in US$) | |
| <10,000 | 29 (36.3) |
| 10,000–20,000 | 27 (33.8) |
| >20,000 | 24 (30) |
| Insurance status | |
| Private | 14 (17.5) |
| Public | 38 (47.5) |
| None | 28 (35) |
| Diabetes duration, years | 9.6 ± 6.4 |
| Insulin status, taking insulin | 51 (63.8) |
| Glycemic control (HbA1c, %) | 8.25 ± 1.99 |
| Optimal (<7.0%) | 26 (32.5) |
| Suboptimal (≥7.0%) | 54 (67.5) |
| Health literacy (BHLS) | 9.36 ± 2.87 |
| Limited (≤9) | 37 (46.3) |
| Adequate (>9) | 43 (53.8) |
| Depressive symptoms (PHQ-2) | 1 (0–2.0) |
| Severe (≥3) | 14 (17.6) |
| Non-severe (<3) | 66 (82.5) |
Note. Non-Caucasian/Non-White participants were the majority (90.9%) African American; 7.5% identified as Hispanic. HbA1c, hemoglobin A1c; BHLS, Brief Health Literacy Screen; PHQ-2, Patient Health Questionnaire-2.
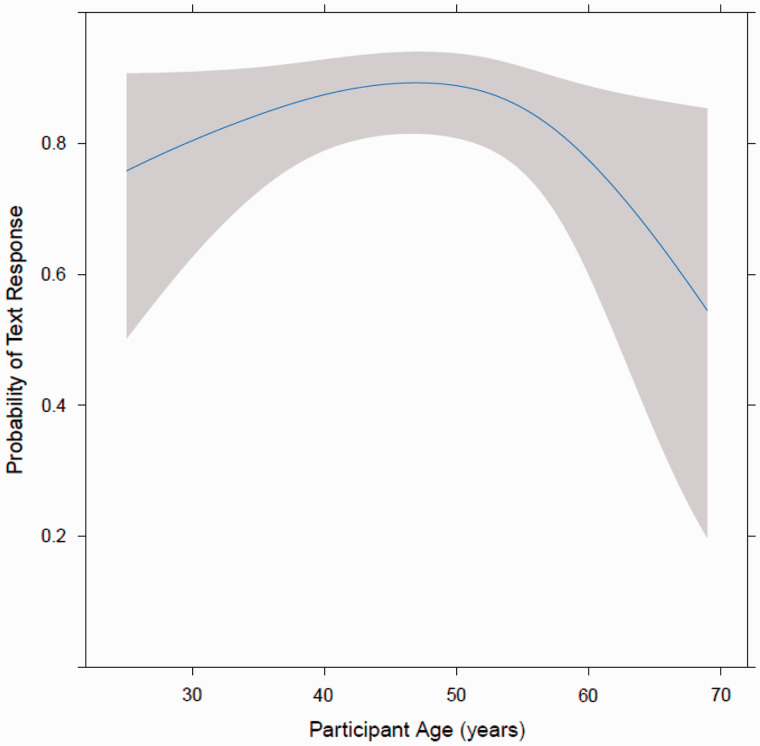
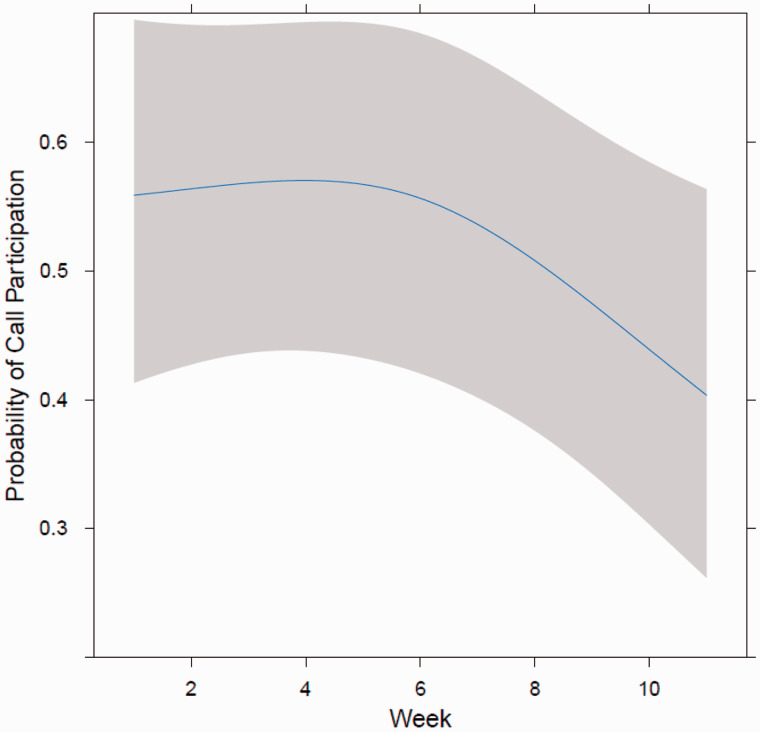
On average, participants responded to 84.0% (IQR: 80.8–96.3%) of the two-way text messages and participated in 57.1% (IQR: 32.1–86.2%) of the IVR calls. In multivariate analysis, participants’ gender, race, income, health literacy, diabetes duration, and time exposed to the intervention were not associated with responding to text messages. Additionally, participants’ age, gender, income, depressive symptoms, and diabetes duration were not associated with IVR call participation. Age had a non-monotonic relationship with text responses ( Pnonlinear = .01) such that the probability of responding to texts tended to increase from about age 25 until roughly age 50 years, and then appeared to decrease as age increased (see Figure 2 ). Participants’ race was significantly associated with IVR call participation ( P < .01). Compared to White participants, non-White participants had a 63% decreased relative odds (AOR: 0.37, 95% CI, 0.19-0.73) of participating in IVR calls. Health literacy was another predictor of IVR call participation ( P = .04). For an IQR (15–11) of four points difference on the BHLS, participants had a 33% decreased odds (AOR: 0.67, 95% CI, 0.46-0.99) of participating in the IVR calls. Depressive symptoms were marginally associated with the probability of text responses. For an interquartile range difference on the PHQ-2 of two points (IQR: 0–2), participants had a 38% decreased odds of responding to texts (AOR = 0.62, 95% CI, 0.38-1.02) ( P = .0594). Time exposed to the intervention was significantly associated with IVR call participation ( P = .01), such that participation appeared to decrease following the fifth week of using the intervention (see Figure 3 ).
Figure 2:
The association between participants age and the probability of responding to two-way text messages
Note: We used repeated measures logistic regression to assess the association between age and probability of text response with adjustment for covariates and clustering. Age was included as a non-linear term using restricted cubic splines.
Figure 3:
The association between time exposed to the intervention (in weeks) and the probability of participating in IVR calls
Note: We used repeated measures logistic regression to assess the association between time and probability of call participation with adjustment for covariates and clustering.
DISCUSSION
We designed an SMS- and IVR-delivered mHealth intervention to improve medication adherence among low SES, diverse adults with T2DM, called the MED intervention. Patients used this intervention for three months, and we measured and assessed the relationship between patient factors and responses to daily two-way text messages, and participation in weekly IVR calls. The relationship between patients’ age and text responses was nonmonotonic, such that the likelihood of responding to texts appeared to increase from age 25 until roughly age 50 years and then decreased beyond age 50 years. Non-White participants had a lower likelihood of participating in IVR calls relative to Whites. Participants with lower health literacy also had a lower likelihood of participating in IVR calls than participants with higher health literacy, and participants with more depressive symptoms had a lower likelihood of responding to text messages compared to participants with fewer depressive symptoms.
There is a small, but growing literature reporting on patient factors associated with engagement in technology-delivered diabetes interventions. For example, among adults with Type 1 diabetes and T2DM, being older, 30 having more education, 31 and being diagnosed with diabetes longer 30 has been associated with more engagement in Internet- and SMS-delivered interventions for blood glucose monitoring and diabetes self-management. Moreover, in a recent 3-month IVR-delivered intervention to promote self-management of chronic conditions, including diabetes, participants aged 18–65 had a roughly constant (∼50%) probability of participating in IVR calls, but after age 65 this probability declined sharply. 22
Older age has been associated with more engagement in health information technologies; 30,31 however, this relationship is not always monotonic. 22 In our study, the probability of engagement indicated by responses to texts appeared to increase with age from about 25 years to ∼50 years. After age 50, the relationship reversed, with a lower probability of responding to texts with increasing age. This finding aligns closely with recent research reporting mobile phone usage wanes after age 50, with individuals 50–64 years of age engaging in half as many mobile phone activities as those 30–49 years of age. 11
While there appears to no longer be a digital divide in owning a cell phone with SMS and voice communication capabilities and using SMS, 11,13 non-Whites were less likely than Whites to use voice communications as part of our diabetes mHealth intervention. Different factors impact the engagement of minorities with T2DM in diabetes interventions, including culturally competent approaches. 32 A recent review suggests cultural adaptations of interventions (e.g., tailoring content to cultural attitudes/beliefs) may be an effective strategy for increasing minority engagement. 33 Although the MED intervention included tailored content addressing patient-specific barriers to adherence, it did not address population-specific barriers to adherence that may include cultural nuances. Not accounting for such nuances might have diminished the engagement of minorities.
Based on ours and others’ previous research, 13,31,34 adults with T2DM and lower health literacy tend to be less engaged in Internet- and mHealth-delivered interventions. Mayberry et al. 35 found that leveraging family members may help overcome barriers to using technology for adults with T2DM and lower health literacy. In our study, we did not examine the influence of family members on patients’ mobile phone use, but it is possible family members’ support for bridging the digital divide may act as a moderator of the relationship between health literacy and engagement with a technology-based intervention. In other words, in the presence of instrumental support for using technologies, health literacy might not be associated with technology use.
In the MED intervention, depressive symptoms were associated with a lower likelihood of responding to text messages over three months. In a review examining engagement with Internet-delivered interventions for depression, higher rates of baseline depression were associated with less intervention engagement. 36 Additionally, research suggests diabetes patients with more depressive symptoms are less likely to adhere to self-care regimens in general. 37 The sense of hopelessness associated with depressive symptoms 27 may contribute to suboptimal engagement with a variety of health-related behaviors.
In order to develop a stronger understanding of subgroup-specific barriers and challenges to using mHealth interventions, future research may benefit from using more qualitative methods to probe populations identified as having low engagement. For instance, focus groups can shed light on why older adults may be less inclined to respond to text messages than middle-aged adults and the reasons for this. After identifying the reasons for less engagement, mHealth interventions can be customized to different user groups. This may involve sending text messages less frequently (if certain groups express annoyance with texts), including more personalized content (if expressing boredom or lack of interest), or supplying more resources and assistance (if technical issues are an issue). Through additional user-centered design approaches, such as participatory design, 38 user groups can be involved in the intervention design process. Actively involving users in decision-making may reveal group-specific preferences for the type of content they desire and the schedule for when and how its received. Using participatory design methods with racial/ethnic minorities could also generate population-specific content that may help facilitate engagement. 33
Once an initial intervention design and build is in place, usability testing can further elucidate patient perceptions. Using mixed methods in usability testing, such as questionnaires and interviews, can provide a deeper understanding of how and why patients choose to engage with a technology-based intervention. 39 Such an approach could be used to further explore why individuals with lower health literacy are less engaged. If the issue is directly related to one’s health literacy status, content can be modified to an appropriate level of understanding, or family members can be leveraged to close the health literacy digital divide. 35 Lastly, future research should explore whether providing motivational and inspirational content may encourage engagement from individuals with depressive symptoms.
There are several study limitations to acknowledge. With any technology-delivered intervention, there is the potential for technical issues (e.g., system delays in sending text messages) and glitches. We experienced some technical issues, which might have limited the opportunities for engagement. In spite of this, we found significant associations between patient factors and engagement within the opportunities given. In addition, our IVR content might not have been appropriate for all levels of health literacy. We ensured our text message content was written at a fifth-grade reading level, but the IVR questions might have been more complex and difficult to understand for persons with lower health literacy. It was a challenge to sustain IVR engagement regardless of patient characteristics, as evidenced by the decrease in IVR participation after five weeks. Studies that engage participants for a longer period of time may find a different pattern of associations. Additionally, it is unclear why participants did not always respond to the two-way text message within 24 h. Future research might conduct a review in order to examine how engagement with mHealth technology changes across the course of an intervention and explore possible reasons for this. Our relatively small sample size might also be considered a limitation; however, we were able to detect significant associations between a priori defined patient factors and SMS or IVR engagement that contribute to our understanding of intervention engagement even with this small sample size. Finally, we recruited low-SES, diverse adults with T2DM from a single FQHC in Nashville, TN, potentially limiting the generalizability of our findings to other patient populations.
CONCLUSION
There are significant gaps to address in understanding the impact of mHealth interventions. Despite their potential to improve patients’ health in diabetes and other chronic disease contexts, 17,21 the average rate of engagement in mHealth interventions is often ≤50%. 20,22 While mHealth intervention research often reports the engagement rate for the studied sample, studies rarely report the relationship between patient factors and the probability of engaging with an intervention or any of its components. Our study addressed the latter by identifying patient characteristics associated with SMS and IVR engagement in a medication adherence promotion mHealth intervention. Furthermore, the groups who were less engaged are groups who are also less adherent to diabetes medications and have suboptimal glycemic control. 3,4 mHealth-delivered interventions have the potential to benefit traditionally hard-to-reach populations. However, it is difficult to promote their value if persons most in need of their support are not engaging with the intervention . Because they elicit rich and descriptive data, focus groups and participatory design are potential avenues for understanding and addressing the low engagement in these at-risk groups. Leveraging mobile phones may not be the best method for delivering interventions to certain groups, or there may need to be modifications to the way these interventions are delivered. Our research highlights the need to ensure high rates of engagement across patient groups, so all patients have an equal opportunity to receive an intervention’s potential benefits.
FUNDING
This research was supported by a McKesson Foundation mHealth Award to Drs Osborn and Mulvaney. Dr Osborn was also supported by a career development award K01DK087894 and the Vanderbilt Center for Diabetes Translational Research P30DK092986. Drs Osborn and Nelson were both supported by R01DK100694-01A1.
COMPETING INTERESTS
None declared.
CONTRIBUTORS
L.A.N. coded data and wrote the manuscript. S.A.M. co-designed the parent study, oversaw data collection, administered the intervention platform, and edited the manuscript. T.G. conducted analyses and edited the manuscript. Y.H. managed data, coded and analyzed data analyses and edited the manuscript. K.J. edited the manuscript. C.Y.O. co-designed the parent study, oversaw data collection and analyses, and co-wrote and edited the manuscript.
ACKNOWLEDGEMENTS
The authors thank Cecilia C. Quintero and Dr Lindsay S. Mayberry for their role in data collection, and the Vine Hill Community Clinic personnel and the participants for their contributions to this research. The contents of this manuscript are solely the responsibility of the authors and do not necessarily represent official views of the funding entities.
REFERENCES
- 1. Cramer JA . A systematic review of adherence with medications for diabetes . Diabetes Care. 2004. ; 27 : 1218 – 1224 . [DOI] [PubMed] [Google Scholar]
- 2. Ho PM, Rumsfeld JS, Masoudi FA, et al. . Effect of medication nonadherence on hospitalization and mortality among patients with diabetes mellitus . Arch Intern Med. 2006. ; 166 : 1836 – 1841 . [DOI] [PubMed] [Google Scholar]
- 3. Egede LE, Gebregziabher M, Hunt KJ, et al. . Regional, geographic, and racial/ethnic variation in glycemic control in a national sample of veterans with diabetes . Diabetes Care. 2011. ; 34 : 938 – 943 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Osborn CY, Cavanaugh K, Wallston KA, et al. . Health literacy explains racial disparities in diabetes medication adherence . J Health Commun. 2011. ; 16 : 268 – 278 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Kim N, Agostini JV, Justice AC . Refill adherence to oral hypoglycemic agents and glycemic control in veterans . Ann Pharmacother. 2010. ; 44 : 800 – 808 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Heisler M, Faul JD, Hayward RA, et al. . Mechanisms for racial and ethnic disparities in glycemic control in middle-aged and older Americans in the health and retirement study . Arch Intern Med. 2007. ; 167 : 1853 – 1860 . [DOI] [PubMed] [Google Scholar]
- 7. Hong JS, Kang HC . Relationship between oral antihyperglycemic medication adherence and hospitalization, mortality, and healthcare costs in adult ambulatory care patients with type 2 diabetes in South Korea . Med Care. 2011. ; 49 : 378 – 384 . [DOI] [PubMed] [Google Scholar]
- 8. Salas M, Hughes D, Zuluaga A, et al. . Costs of medication nonadherence in patients with diabetes mellitus: A systematic review and critical analysis of the literature . Value Health. 2009. ; 12 : 915 – 922 . [DOI] [PubMed] [Google Scholar]
- 9. McDonald HP, Garg AX, Haynes RB . Interventions to enhance patient adherence to medication prescriptions: scientific review . JAMA. 2002. ; 288 : 2868 – 2879 . [DOI] [PubMed] [Google Scholar]
- 10. Kripalani S, Yao X, Haynes RB . Interventions to enhance medication adherence in chronic medical conditions: A systematic review . Arch Intern Med. 2007. ; 167 : 540 – 550 . [DOI] [PubMed] [Google Scholar]
- 11. Duggan M . Cell Phone Activities 2013 . Washington, DC: : Pew Research Center; ; 2013. . [Google Scholar]
- 12. Smith A . The Best (and worst) of Mobile Technology . Washington, DC: : Pew Research Center; ; 2012. . [Google Scholar]
- 13. Chakkalakal RJ, Kripalani S, Schlundt DG, et al. . Disparities in using technology to access health information: race versus health literacy . Diabetes Care. 2014. ; 37 : e53 – e54 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Fox S, Duggan M . Mobile Health 2012 . Washington, DC: : Pew Research Center; ; 2012. . [Google Scholar]
- 15. Free C, Phillips G, Galli L, et al. . The effectiveness of mobile-health technology-based health behaviour change or disease management interventions for health care consumers: a systematic review . PLoS Med. 2013. ; 10 : e1001362 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Beratarrechea A, Lee AG, Willner JM, et al. . The impact of mobile health interventions on chronic disease outcomes in developing countries: A systematic review . Telemed J E-Health. 2014. ; 20 : 75 – 82 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Saffari M, Ghanizadeh G, Koenig HG . Health education via mobile text messaging for glycemic control in adults with type 2 diabetes: a systematic review and meta-analysis . Prim Care Diab. 2014. ; 29 : 275 – 285 . [DOI] [PubMed] [Google Scholar]
- 18. Arora S, Peters AL, Burner E, et al. . Trial to examine text message-based mHealth in emergency department patients with diabetes (TExT-MED): a randomized controlled trial . Ann Emerg Med. 2014. ; 63 : 745 – 754e6 . [DOI] [PubMed] [Google Scholar]
- 19. Faridi Z, Liberti L, Shuval K, et al. . Evaluating the impact of mobile telephone technology on type 2 diabetic patients' self-management: The NICHE pilot study . J Eval Clin Pract. 2008. ; 14 : 465 – 469 . [DOI] [PubMed] [Google Scholar]
- 20. Katz R, Mesfin T, Barr K . Lessons from a community-based mHealth diabetes self-management program: “It's not just about the cell phone" . J Health Commun. 2012. ; 17 : 67 – 72 . [Google Scholar]
- 21. Liang X, Wang Q, Yang X, et al. . Effect of mobile phone intervention for diabetes on glycaemic control: A meta-analysis . Diabet Med. 2011. ; 28 : 455 – 463 . [DOI] [PubMed] [Google Scholar]
- 22. Piette JD, Valverde H, Marinec N, et al. . Establishing an independent mobile health program for chronic disease self-management support in Bolivia . Front Public Health. 2014. ; 2 : 1 – 10 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Mulvaney SA, Anders S, Smith AK, et al. . A pilot test of a tailored mobile and web-based diabetes messaging system for adolescents . J Telemed Telecare. 2012. ; 18 : 115 – 118 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Piette JD . Interactive voice response systems in the diagnosis and management of chronic disease . Am J Manag Care. 2000. ; 6 : 817 – 827 . [PubMed] [Google Scholar]
- 25. Osborn CY, Mulvaney SA . Development and feasibility of a text messaging and interactive voice response intervention for low-income, diverse adults with type 2 diabetes mellitus . J Diabetes Sci Technol. 2013. ; 7 : 612 – 622 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Wallston KA, Cawthon C, McNaughton CD, et al. . Psychometric properties of the brief health literacy screen in clinical practice . J Gen Intern Med. 2014. ; 29 : 119 – 126 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Kroenke K, Spitzer RL, Williams JBW . The Patient Health Questionnaire-2: validity of a two-item depression screener . Med Care. 2003. ; 41 : 1284 – 1292 . [DOI] [PubMed] [Google Scholar]
- 28. Freedman DA . On the so-called “Huber sandwich estimator” and “robust standard errors” . Am Stat. 2006. ; 60 : 299 – 302 . [Google Scholar]
- 29. Mayberry LS, Gonzalez JS, Wallston KA, Kripalani S, Osborn CY . The ARMS-D out performs the SDSCA, but both are reliable, valid, and predict glycemic control . Diabetes Res Clin Pract. 2013. ; 102 : 96 – 104 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Kwon H-S, Cho J-H, Kim H-S, et al. . Development of web-based diabetic patient management system using short message service (SMS) . Diabetes Res Clin Pract. 2004. ; 66 : S133 – S137 . [DOI] [PubMed] [Google Scholar]
- 31. Wangberg SC, Bergmo TS, Johnsen J-AK . Adherence in Internet-based interventions . Patient Pref Adherence. 2008. ; 2 : 57 . [PMC free article] [PubMed] [Google Scholar]
- 32. Loftin WA, Barnett SK, Bunn PS, et al. . Recruitment and retention of rural African Americans in diabetes research lessons learned . Diabetes Educ. 2005. ; 31 : 251 – 259 . [DOI] [PubMed] [Google Scholar]
- 33. Yancey AK, Ortega AN, Kumanyika SK . Effective recruitment and retention of minority research participants . Annu Rev Public Health. 2006. ; 27 : 1 – 28 . [DOI] [PubMed] [Google Scholar]
- 34. Osborn CY, Mayberry LS, Wallston KA, Johnson KB, Elasy TA . Understanding patient portal use: implications for medication management . J Med Internet Res. 2013. ; 15 : e133 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Mayberry LS, Kripalani S, Rothman RL, Osborn CY . Bridging the digital divide in diabetes: family support and implications for health literacy . Diabetes Technol Ther. 2011. ; 13 : 1005 – 1012 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Christensen H, Griffiths KM, Farrer L . Adherence in Internet interventions for anxiety and depression: systematic review . J Med Internet Res. 2009. ; 11 : e13 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Ciechanowski PS, Katon WJ, Russo JE . Depression and diabetes: impact of depressive symptoms on adherence, function, and costs . Arch Intern Med. 2000. ; 160 : 3278 – 3285 . [DOI] [PubMed] [Google Scholar]
- 38. Sanders EB-N . From user-centered to participatory design approaches . Design and the Social Sciences: Making Connections . 2002. : 1 – 8 . [Google Scholar]
- 39. Lyles CR, Sarkar U, Osborn CY . Getting a technology-based diabetes intervention ready for prime time: a review of usability testing studies . Curr Diab Rep. 2014. ; 14 : 1 – 12 . [DOI] [PMC free article] [PubMed] [Google Scholar]