Abstract
Aim:
There is growing evidence that non-communicable diseases (NCDs) are a major health problem in developing and transitional countries. The prevalence of NCDs and associated factors are under-researched in Albania. We aimed to assess the prevalence and socio-demographic and lifestyle correlates of NCDs in the Albanian adult population.
Methods:
The study was carried out in the framework of Albania Living Standard Measurement Survey (LSMS), a national population-based cross-sectional study conducted in 2012 including 12,554 men and women aged ≥35 years. All participants reported on the presence of at least one chronic condition, which in the analysis was dichotomized into “yes” vs. “no”. Information on socio-demographic characteristics (age, gender, education, employment status, residence) and lifestyle factors (smoking and alcohol consumption) was also collected. Logistic regression was used to assess socio-demographic and behavioral correlates of NCDs.
Results:
Overall, the prevalence of chronic diseases in this population-based sample of Albanian adults was 2864/12554=22.8%. Upon multivariable adjustment for all covariates, positive correlates of chronic conditions were older age (OR=6.0, 95%CI=5.3-6.8), female gender (OR=1.2, 95%CI=1.1-1.4), residence in coastal areas of Albania (OR=2.0, 95%CI=1.7-2.5), unemployment (OR=1.8, 95%CI=1.6-2.0), low education (OR=1.6, OR=1.3-1.9) and current smoking (OR=1.2, 95%CI=1.1-1.5). Conversely, there was an inverse association with poverty (OR=0.8, 95%CI=0.7-1.0).
Conclusions:
This study provides evidence on self-reported NCDs and its determinants in transitional Albania. These baseline data may be useful for assessment of future NCD trends in Albania and cross-comparisons with the neighboring countries.
Keywords: Albania, non-communicable diseases, risk factors
1. INTRODUCTION
Non-communicable diseases ((NCDs), such as coronary heart disease (CHD), stroke, chronic obstructive pulmonary disease (COPD), cancer, type 2 diabetes and chronic kidney disease are the leading cause of mortality and morbidity worldwide (1). Recent studies indicate that NCDs generate a large impact on healthcare spending, national income and macro-economic productivity in the WHO regions (2, 3). Also, there is growing evidence that NCDs are a major health problem in the developing and transitional countries (1, 4). Recently, a cluster of preventable and modifiable risk factors such as tobacco use, heavy alcohol consumption, physical inactivity and unhealthy diet was shown to be the major contributor to the observed increase of total burden of NCDs in South Eastern European (SEE) countries (5). This is attributed not only to the health-damaging behaviors, but also to the negative impact of globalization and rapid urbanization (6). However, risk factors vary across regions and countries (6, 7). Establishment of effective surveillance systems to determine the prevalence of national risk factors and NCDs is essential to build strategies for prevention and control of NCDs.
To date, the prevalence and predictors of NCDs in Albanian adults are under-researched. Yet, available evidence suggests that Albania, a former communist country in the SEE region, is currently undergoing a rapid epidemiological transition characterized by a significant increase of the NCD burden (5, 8, 9). In this framework, we aimed to assess the prevalence and socio-demographic and lifestyle correlates of NCDs in the Albanian adult population.
2. METHODS
The study was carried out in the framework of Albania Living Standard Measurement Survey (LSMS) which is a national population-based cross sectional survey. Its main objective is to collect information for measuring the Albanian households’ welfare and to identify factors that determine it. The survey was conducted in September 2012 comprising a sample of 6671 Albanian households. In our study, we included all individuals aged ≥35 years (6110 men and 6444 women). In order for the sample estimates from the Albania LSMS to be representative of the overall Albanian population, the data are multiplied by a sampling weight. The basic weight for each sample household is equal to the inverse of its probability of selection (calculated by multiplying the probabilities at each sampling stage). The geographic domain of analyses has included four geographic regions of Albania (Central, Coastal, Mountain and Tirana) by rural and urban strata.
Data were collected by structured questionnaires through two methods of interviewing: a face to face interview during interviews to subject’s home and self-completion diary filled in by the household member. Detailed information about the research method and questionnaires used can be found at: http://microdata.worldbank.org/index.php/catalog/1970/get_microdata/.
Briefly, the outcome variable was the self-reported presence of chronic NCDs upon the following question: “Has a doctor ever told you that you have a chronic condition?”
The independent variables included socio-demographic characteristics: age (categorized into: 35-50 years, 51-65 years and ≥66 years), gender, education (categorized into: primary, high school and university), poverty level (dichotomized into: poor vs. nor poor), employment status (categorized into: employed vs. unemployed) and place of residence (urban vs. rural areas). Two health behavioral variables were used: smoking (trichotomized into: never, past smoker and current smoker) and alcohol intake (dichotomized into: yes vs. no).
Statistical analysis
Sample estimates of self-reported NCDs by socio-demographic characteristics and lifestyle factors were standardized with the respective strata of the overall Albanian population aged 35 years and above. Absolute numbers and their respective percentages from the study sample, and standardized (population-weighted) percentages were reported.
Binary logistic regression was used to assess the association of self-reported NCDs with socio-demographic characteristics and behavioral factors. Initially, crude (unadjusted) odds ratios (OR: “NCD: yes” vs. “NCD: no”), their respective 95% confidence intervals (95%CIs) and p-values were calculated. Next, age-adjusted models were conducted. Subsequently, all variables were included into a backward stepwise elimination procedure with a p-value to exit set at >0.10. Multivariable-adjusted ORs, their respective 95% CIs and p-values were calculated. Hosmer-Lemeshow test was used to assess the overall goodness-of-fit of the logistic regression models (all the reported models met the goodness-of-fit criterion). SPSS (Statistical Package for Social Sciences, version 19.0), was used for all the statistical analyses.
3. RESULTS
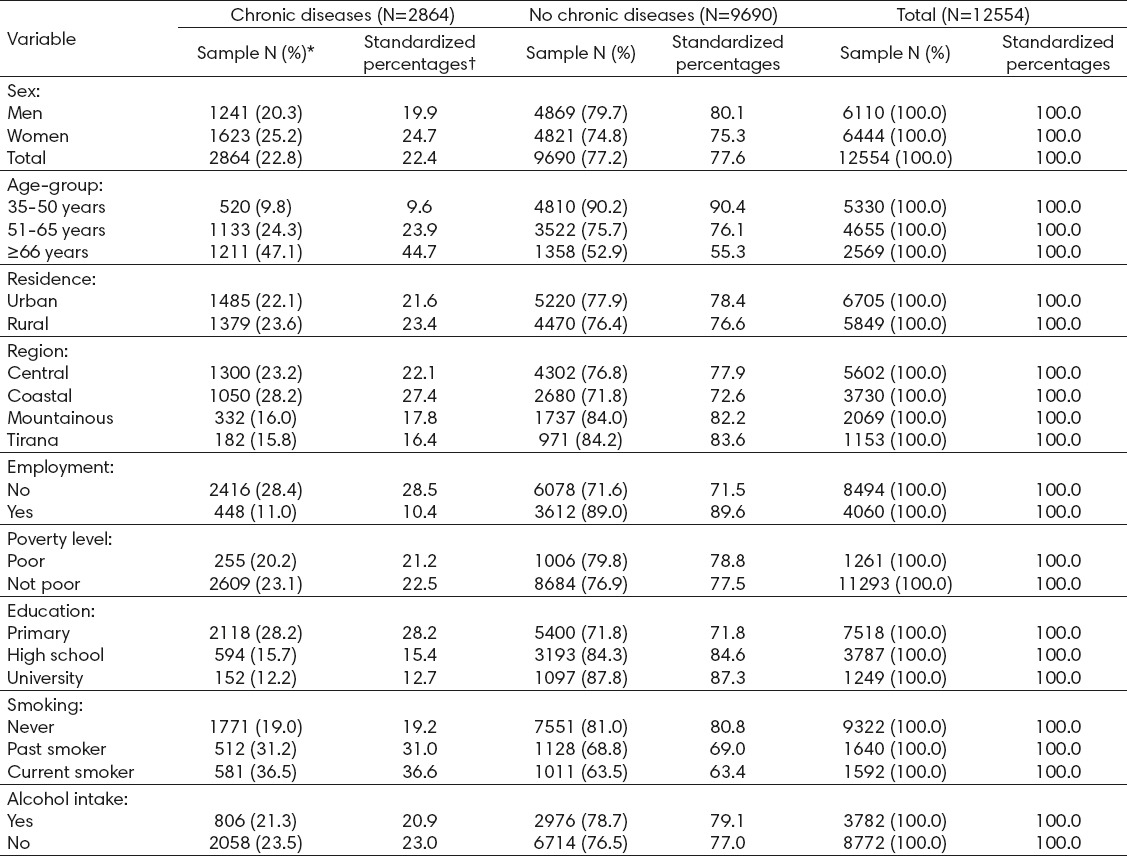
Overall, the prevalence of chronic diseases in this population-based sample of Albanian men and women aged 35 years and above was 2864/12554=22.8% (Table 1).. The prevalence of chronic conditions was higher in women compared to men (25.2% vs. 20.3%, respectively). As expected, the youngest participants (individuals aged 35-50 years) had the lowest prevalence of chronic conditions (about 10%), whereas their oldest counterparts (individuals aged 66 years and above) exhibited the highest prevalence of chronic diseases (45%). Individuals residing in rural areas had a slightly higher prevalence of chronic conditions compared to their urban counterparts (24% vs. 22%, respectively). Furthermore, Tirana residents had the lowest prevalence of chronic diseases (16%), whereas individuals residing in the coastal part of Albania had the highest prevalence (27%). The unemployed has a much higher prevalence of chronic diseases than individuals who were employed (28% vs. 11%, respectively). Similarly, the low educated individuals had a considerably higher prevalence of chronic diseases compared to highly educated participants (28% vs. 12%, respectively). Current smokers had the highest prevalence (36%), whereas never smokers had the lowest prevalence of chronic conditions (19%). Finally, alcohol abstainers had a slightly higher prevalence of chronic conditions than individuals who consumed alcohol (23% vs. 21%, respectively) (Table 1).
Table 1.
Distribution of socio-demographic characteristics and behavioral factors in a population-based sample of Albanian adults by presence of chronic diseases. * Absolute numbers and their respective row percentages (in parentheses) in the actual study sample. † Population standardized (weighted) percentages.
In crude (unadjusted) logistic regression models (Table 2– left panel), there was a strong graded positive association of age with chronic conditions [OR(51-65 years vs. 35-50 years)=3.0, 95%CI=2.7-3.3 and OR(≥66 years vs. 35-50 years)=8.2, 95%CI=7.3-9.3]. In addition, there was a positive relationship with female gender (OR=1.3, 95%CI=1.2-1.4). There was a weak association with place of residence (urban vs. rural areas), whereas Tirana residents had the lowest odds of chronic conditions. Furthermore, there was evidence of a strong relationship with unemployment (OR=3.2, 95%CI=2.9-3.6) and a low education attainment (OR=2.8, 95%CI=2.4-3.4). Conversely, there was an inverse relationship with self-perceived poverty (OR=0.8, 95%CI=0.7-1.0). There was a graded relationship of chronic conditions with smoking status [OR(past smokers vs. never smokers)=1.4, 95%CI=1.3-1.7 and OR(current smokers vs. never smokers)=1.6, 95%CI=1.3-1.9]. On the other hand, alcohol abstainers had higher odds of chronic conditions (OR=1.1, 95%=1.0-1.2) (Table 3 – left panel).
Table 2.
Association of self-reported chronic diseases with socio-demographic characteristics and behavioral factors; odds ratios from binary logistic regression. * Odds ratios (OR: chronic diseases vs. no chronic diseases) and 95% confidence intervals (95%CI) from binary logistic regression. † All variables were included in a backward stepwise elimination procedure with a p-value to exit set at >0.10. Empty cells refer to the variables excluded from the model.
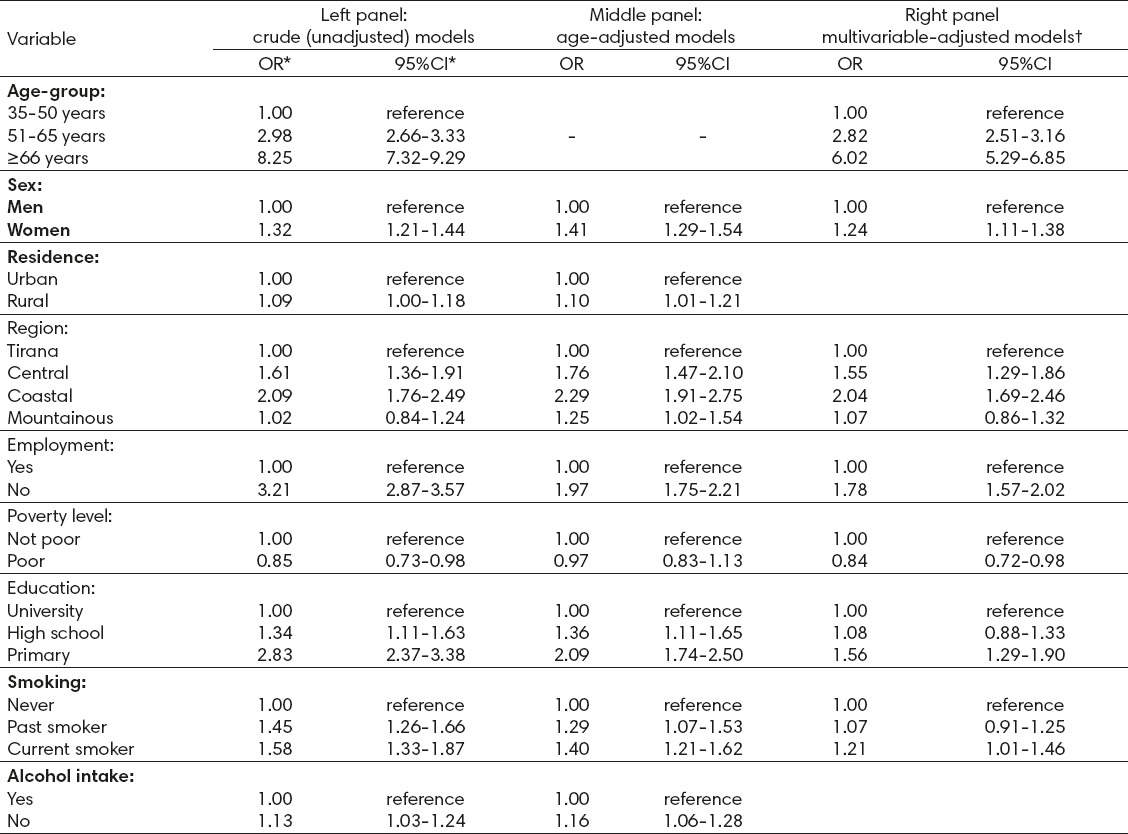
Adjustment for age (Table 3– middle panel) slightly accentuated the positive association with female gender and residence in regions other than Tirana, but it attenuated the relationship with employment, educational level and smoking status.
Upon multivariable adjustment for all covariates in a backward stepwise elimination procedure (Table 3 – right panel), positive correlates of chronic conditions remained older age (OR(≥66 years vs. 35-50 years)=6.0, 95%CI=5.3-6.8), female gender (OR=1.2, 95%CI=1.1-1.4), residence in coastal areas of Albania (OR=2.0, 95%CI=1.7-2.5), unemployment (OR=1.8, 95%CI=1.6-2.0), low education (OR=1.6, OR=1.3-1.9) and current smoking (OR=1.2, 95%CI=1.1-1.5). On the other hand, the inverse association with poverty persisted in multivariable-adjusted logistic regression models (OR=0.8, 95%CI=0.7-1.0) (Table 3 – right panel).
4. DISCUSSION
About 23% of men and women included in this nationwide representative sample of Albanian adults reported at least one chronic condition. Similar to other studies (7, 10-15), older age, female gender, residence in coastal areas of Albania, unemployment status and low education were associated with the presence of self-reported NCDs. These findings confirm that NCDs risk among Albanian adults vary by socio-demographic factors and have implications for preventive measures and intervention programs, health care services and health expenditure according to different socio-demographic subgroups. Our findings concur with previous reports that older females are more likely than older males to suffer from NCDs (10, 11, 16). On the other hand, unemployment and low educated men and women were more likely to report NCDs than the employed, or individuals with higher education. Conversely, two studies have shown a positive association of NCDs with higher education (14) or employment status (15).
Results of the current study show also that living in the coastal areas of Albania is associated with a twofold increase in the risk of NCDs. In the past 25 years, presumably, these areas have been undergoing a more rapid process of “modernization” including health damaging behaviours (smoking, heavy alcohol consumption, sedentary lifestyle and poor dietary habits) (5).
Interestingly, our findings show an inverse relationship between poverty and the presence of self-reported NCDs. In fact, previous studies have shown that lower socioeconomic groups tend to engage later in health-damaging behaviours in the course of a country’s multidimensional transition (economic, demographic and geographic) (7, 17).
Few studies in Albania have reported the prevalence of lifestyle risk factors for NCDs in urban and rural areas (18-23). However, as indicated in a national health report, the overall lifestyle factors in 2010 accounted for about 72% of the total burden of disease in Albania (24).
Cigarette smoking is one of the major risk factors for NCDs in Albania (24). The proportion of the burden of disease attributable to smoking increased from 9.9% in 1990 to 12.1% in 2010 (24). Albanian data indicate that cigarette smoking is a major modifiable risk factor for type 2 diabetes (18), hypertension (19), coronary heart diseases (21) and bone diseases (20). Previous studies in Albania have shown that current cigarette smoking is a risk factor for pancreatic cancer (OR=6.8, 95%CI=2.1-18.5) (22), esophageal squamous-cell carcinoma (OR=3.90, 95%CI=2.9-5.4) and esophageal adenocarcinoma (OR=2.60, 95%CI=2.2-3.2) (23). Furthermore, another study from Albania has reported that partner’s current smoking status was positively associated with a greater acute coronary syndrome risk in men, but not in women (25). Also, it should be pointed out that, in 2010, the age-standardized Disability-Adjusted Life Years (DALYs) attributable to smoking in Albania was above the mean value in the SEE countries (24). Nevertheless, Albania has currently implemented a comprehensive tobacco control program, but further surveys should be conducted to monitor the effectiveness of the program.
Regarding the alcohol consumption, our findings that alcohol abstainers had higher odds of chronic conditions are consistent with the previous evidence obtained from the Albanian population (22, 23, 26). Furthermore, compared with the other countries in the SEE region, the age-standardized burden of disease attributable to alcohol use in Albania was one of the lowest in the region but with an increasing trend during the last decade (24). The current rising trend of smoking and alcohol intake reinforce the importance of prevention and detection of these modifiable risk factors in reducing the burden of NCDs in the Albania population.
This study has some limitations including its cross-sectional design, use of self-reported vs. clinical examination of NCDs, and the absence of other key behavioral determinants of NCDs such as dietary habits and physical exercise.
In conclusion, regardless of its potential limitations, this study provides important evidence on the self-reported prevalence of NCDs and its socio-demographic and behavioural risk factors in post-communist Albania. These baseline data may be useful for assessment of future NCD trends in Albania and cross-comparisons with the neighboring countries. However, further studies are needed to monitor the prevalence and risk factors of NCDs in this transitional population.
Footnotes
Author’s contribution: Fatjona Kraja, Bledar Kraja, Adriana Babameto and Genc Burazer made substantial contribution to conception, design, drafting the article and critical revision for important intellectual content. Fatjona Kraja, Bledar Kraja, Iris Mone and Ilda Harizi made substantial contribution to acquisition of data, analysis and interpretation of data and critical revision for important intellectual content. Fatjona Kraja, Bledar Kraja and Genc Burazeri made substantial contribution to conception and design. All the authors approved the final version to be published.
• Conflict of interest: None declared.
REFERENCES
- 1.Global Burden of Disease Study 2013 Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries. 1990–2013:a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2015 Aug 22;386(9995):743–800. doi: 10.1016/S0140-6736(15)60692-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Muka T, Imo D, Jaspers L, Colpani V, Chaker L, van der Lee SJ, et al. The global impact of non-communicable diseases on healthcare spending and national income:a systematic review. Eur J Epidemiol. 2015;30(4):251–77. doi: 10.1007/s10654-014-9984-2. [DOI] [PubMed] [Google Scholar]
- 3.Chaker L, Falla A, van der Lee SJ, Muka T, Imo D, Jaspers L, et al. The global impact of non-communicable diseases on macro-economic productivity:a systematic review. Eur J Epidemiol. 2015;30(5):357–95. doi: 10.1007/s10654-015-0026-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.World Health Organization. Global status report on noncommunicable diseases. Geneva, Switzerland: WHO; 2011. [Google Scholar]
- 5.Burazeri G, Achterberg P. Health status in the transitional countries of South Eastern Europe (Editorial) SEEJPH. 2015 doi:10.12908/SEEJPH-2014-43. [Google Scholar]
- 6.David J, Hunter K, Srinath Reddy. Noncommunicable Diseases. N Engl J Med. 2013;14(369):1336–43. doi: 10.1056/NEJMra1109345. [DOI] [PubMed] [Google Scholar]
- 7.Hosseinpoor RA, Bergen N, Kunst A, Harper S, Guthold R, Rekve D, et al. Socioeconomic inequalities in risk factors for non-communicable diseases in low-income and middle-income countries:results from the World Health Survey. BMC Public Health. 2012;12:912. doi: 10.1186/1471-2458-12-912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bjegovic V, Vukovic D, Terzic Z, Milicevic MS, Laaser UT. Strategic orientation of public health in transition:an overview of south eastern Europe. J Public Health Policy. 2007;28:94–101. doi: 10.1057/palgrave.jphp.3200121. [DOI] [PubMed] [Google Scholar]
- 9.Mackenbach JP, Stirbu I, Roskam AJ, Schaap MM, Menvielle G, Leinslau M, et al. Socioeconomic inequalities in health in 22 European countries. N Engl J Med. 2008;358:2468–81. doi: 10.1056/NEJMsa0707519. [DOI] [PubMed] [Google Scholar]
- 10.Phaswana-Mafuya N, Peltzer K, Chirinda W, Musekiwa A, Kose Z, Hoosain E, et al. Self-reported prevalence of chronic non-communicable diseases and associated factors among older adults in South Africa. Glob Health Action. 2013;6:20936. doi: 10.3402/gha.v6i0.20936. http://dx.doi.org/10.3402/gha.v6i0.20936 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jerliu N, Toçi E, Burazeri G, Ramadani N, Brand H. Prevalence and socioeconomic correlates of chronic morbidity among elderly people in Kosovo:a population-based survey. BMC Geriatrics. 2013;13:22. doi: 10.1186/1471-2318-13-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Marengoni A, Winblad B, Karp A, Fratiglioni L. Prevalence of chronic diseases and multimorbidity among the elderly population in Sweden. Am J Public Health. 2008;98:1198–1200. doi: 10.2105/AJPH.2007.121137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Boutayeb A, Boutayeb S, Boutayeb W. Multi-morbidity of non-communicable diseases and equity in WHO Eastern Mediterranean countries. International Journal for Equity in Health. 2013;12:60. doi: 10.1186/1475-9276-12-60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bener A, Ghulom S, Abou-Saleh MT. Prevalence, symptom patterns and comorbidity of anxiety and depressive disorders in primary care in Qatar. Soc Psychiatry Psychiatr Epidemiol. 2012;47(3):439–46. doi: 10.1007/s00127-011-0349-9. [DOI] [PubMed] [Google Scholar]
- 15.Almawi W, Amim H, Al-Sayed N, Arekat MR, Al-Khateeb GM, Baqer A, et al. Association of comorbid depression, anxiety, and stress disorders with type 2 diabetes in Bahrain, a country with a very high prevalence of type 2 diabetes. J Endocrinol Invest. 2008;31(11):1020–24. doi: 10.1007/BF03345642. [DOI] [PubMed] [Google Scholar]
- 16.Rueda S, Artazcoz L, Navarro V. Health inequalities among the elderly in Western Europe. Journal of Epidemiology and Community Health. 2008;62:492–8. doi: 10.1136/jech.2006.059279. [DOI] [PubMed] [Google Scholar]
- 17.Blakely T, Hales S, Kieft C, Wilson N, Woodward A. The global distribution of risk factors by poverty level. Bull World Health Organ. 2005;83:118–26. [PMC free article] [PubMed] [Google Scholar]
- 18.Shapo L, McKee M, Coker R, Ylli A. Type 2 diabetes in Tirana City, Albania:a rapid increase in a country in transition. Diabet Med. 2004;21(1):77–83. doi: 10.1046/j.1464-5491.2003.01093.x. [DOI] [PubMed] [Google Scholar]
- 19.Petrela E, Burazeri G, Pupuleku F, Zaimi E, Rahman M. Prevalence and correlates of hypertension in a transitional southeastern European population:results from the Albanian Demographic and Health Survey. Arh Hig Rada Toksikol. 2013;64(4):479–87. doi: 10.2478/10004-1254-64-2013-2362. [DOI] [PubMed] [Google Scholar]
- 20.Hoxha F, Tafaj A, Roshi E, Burazeri G. Distribution of Risk Factors in Male and Female Primary Health Care Patients with Osteoarthritis in Albania. Med Arch. 2015;69(3):145–8. doi: 10.5455/medarh.2015.69.145-148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Burazeri G, Goda A, Sulo G, Stefa J, Roshi E, Kark JD. Conventional risk factors and acute coronary syndrome during a period of socioeconomic transition:population-based case-control study in Tirana, Albania. Croat Med J. 2007;48(2):225–33. [PMC free article] [PubMed] [Google Scholar]
- 22.Kraja F, Harizaj I, Kraja B, Babameto A, Kullolli S, Prifti S. Pancreatic cancer and lifestyle characteristics:a population-based study in Albania. Annals of Oncology. 2013;24(Suppl.4):iv41. P-0051. [Google Scholar]
- 23.Kraja B, Kreka B, Pupuleku F, Burazeri G, Prifti S. Smoking and alcohol consumption as risk factors for esophageal cancer. European Journal of Cancer. 2011;47(Suppl.1):S251. [Google Scholar]
- 24.Burazeri G, Bregu A, Qirjako G, Roshi E, Petrela K, Bukli M, et al. National Health Report:Health Status of the Albanian Population. 2014. http://www.ishp.gov.al/wp-content/uploads/2015/01/Health-report-English-version.pdf .
- 25.Sulo G, Burazeri G, Dehghan A, Kark JD. Partner’s smoking status and acute coronary syndrome:population-based case-control study in Tirana, Albania. Croat Med J. 2008;49(6):751–6. doi: 10.3325/cmj.2008.49.751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Burazeri G, Kark JD. Moderate alcohol intake, though not regular heavy drinking, is protective for acute coronary syndrome:a population-based, case-control study in Southeast Europe. Ann Epidemiol. 2011;21(8):564–71. doi: 10.1016/j.annepidem.2011.02.006. [DOI] [PubMed] [Google Scholar]


