Abstract
Introduction:
Chronic kidney disease (CKD) represents a serious public health problem due to the increase in incidence and prevalence of this disease worldwide. Given the significant morbidity and mortality from cardiovascular disease (CVD) in the population of patients with CKD, and the fact that dyslipidemia itself is a risk factor for CVD, increases the importance of lipid metabolism study in patients with CKD. Goal: Evaluate the lipid status of patients with chronic kidney disease.
Material and methods:
A one-year prospective study included 150 adult patients who were in various stages of chronic renal failure (stage I to IV). Estimate of creatinine clearance was performed using Cockroft-Goult formula. The classification of patients according to stages of chronic renal insufficiency was performed in accordance with the criteria of Kidney Disease Outcomes Quality Initiative (K/DOQI).
Results:
Of the total number of patients (N=150) there was 71 males and 79 females. The mean age of patients was 55.43 years. Average values of serum cholesterol were highest in patients with stage II renal disease and the lowest in patients classified as stage IV (5.76±1.60 mmol/L vs. 5.07±1.88 mmol/L). Analysis of the average value of triglycerides in blood show a slight increase through the stages of CKD in a manner that patients classified into stage I have low serum triglyceride levels (1.73±1.17 mmol/L (range 0.61 to 5.5 mmol/L), and patients classified in stage III the highest value 2.13±1.11 mmol/L (range 0.62 to 4.66 mmol/L).
Conclusion:
Average cholesterol levels does not statistically significantly change with progression of chronic renal disease. There is an almost linear increase in average triglyceride levels in chronic renal disease. Triglyceride levels in serum begins to increase in the early stage of chronic renal disease and reach the peak in stage IV.
Keywords: Chronic kidney disease (CKD), lipid status, cholesterol, triglycerides
1. INTRODUCTION
Chronic kidney disease represents a serious public health problem due to the increase in incidence and prevalence of this disease worldwide (1, 2). For chronic kidney disease (CKD) are also characteristic different lipid metabolic disorders that can worsen the progression of kidney disease (3). Also CKD is characterized both by quantitative and qualitative abnormalities of lipid status (4). Mechanisms of dyslipidemia occurrence are multiple and are associated with proteinuria and consequent disorder in lipoprotein transport as well as oxidative stress (5). Given the significant morbidity and mortality from cardiovascular disease (CVD) in the population of patients with CKD, and the fact that dyslipidemia itself is a risk factor for CVD, increases the importance of lipid metabolism study in patients with CKD.
2. MATERIAL AND METHODS
A one-year prospective clinical study was conducted at the University Clinical Center of Sarajevo, Bosnia and Herzegovina, and included 150 adult patients who were in various stages of chronic renal failure (stage I to IV) and healthy individuals. Each study group consisted of 30 patients, also with the control group of 30 healthy individuals. Patients who are excluded from the study were as follows: patients in the terminal stage of chronic renal insufficiency (stage V), patients with kidney transplant, patients with unstable renal function, patients with diagnosed diabetes, polycystic kidney disease, hydronephrosis, renal anomalies, renal tumors and accompanying decompensating disease.
We used the medical records of patients that contained the necessary clinical, laboratory and demographic data. At admission to each patient were taken demographic data (gender and age), values of total cholesterol and triglycerides as well as possible comorbidity. Estimate of creatinine clearance was performed using Cockroft-Goult formula (6). The classification of patients according to stages of chronic renal insufficiency was performed in accordance with the criteria of Kidney Disease Outcomes Quality Initiative (K/DOQI) (7).
The test results were analyzed using descriptive statistics, which included determining the mean value, standard deviation (SD) and standard error of mean (SEM). To test the normal distribution of variables Kolmogorov-Smirnov test (Z) was used. Statistical significance of differences in mean values between the samples was determined using the Student t-test (t) and ANOVA (F) methods for variables with normal distribution, and Mann-Whitney test for variables that do not have a normal distribution. Accepted statistical significance was p <0.05.
3. RESULTS
Of the total number of patients (N=150) there was 71 males and 79 females. The mean age of patients was 55.43 years. Table 1. present the average values of cholesterol in different stages of chronic kidney disease.
Table 1.
The average values of serum cholesterol in patients in different stages of CKD. U=1.305; df=3; p=0.276
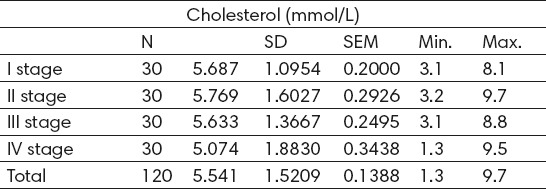
Average values of serum cholesterol were highest in patients with stage II renal disease and the lowest in patients classified as stage IV (5.76±1.60 mmol/L vs. 5.07±1.88 mmol/L). Statistical analysis showed no significant difference in the cholesterol level between study groups (p> 0.05). Table 2 present the average values of triglycerides in different stages of chronic kidney disease.
Table 2.
The average values of serum triglycerides in patients in different stages of CKD. F=0.897; df=3; p=0.445
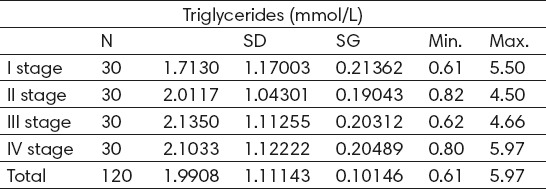
Analysis of the average value of triglycerides in blood show a slight increase through the stages of CKD in a manner that patients classified into stage I have low serum triglyceride levels 1.73±1.17 mmol/L (range 0.61 to 5.5 mmol/L), and patients classified in stage III the highest value 2.13±1.11 mmol/L (range 0.62 to 4.66 mmol/L). The patient of control group had the lowest values of triglycerides in blood 1.52±1.15 mmol/L (range 0.60 to 4.50mmol/L). There was no statistically significant difference in serum triglycerides levels between study groups (p>0.05).
4. DISCUSSION
Chronic kidney disease represents a serious public health problem due to the increase in its incidence and prevalence, both in the world and our country.
Analysis of the average values of cholesterol in patients with a defined stage of chronic renal disease showed no statistically significant differences between groups, while the analysis of the average values of blood triglycerides showed an almost linear increase, so that the patients classified into control group had lowest values and the patients classified in stage III the highest value of triglyceride level in the blood. Kaysen and colleagues studied the abnormal blood fat levels in patients with chronic renal disease and concluded that in this population we can speak of dyslipidemia rather than the hyperlipidemia. For chronic renal disease is characterized moderate increase in triglycerides levels in the blood, while the value of total cholesterol tends to remain in the reference values (8). Triglyceride levels in serum begins to increase in the early stages of chronic kidney disease, and the highest value are achieved in stages IV and V. Patients with chronic renal disease generally have lower HDL cholesterol levels, while elevated LDL cholesterol levels can be found in the initial, but is not typical for the advanced stages of chronic kidney disease (3).
5. CONCLUSION
Average cholesterol levels does not statistically significantly change with progression of chronic renal disease. There is an almost linear increase in average triglyceride levels in chronic renal disease. Triglyceride levels in serum begins to increase in the early stage of chronic renal disease and reach the peak in stage IV.
Footnotes
• Conflict of interest: None declared.
REFERENCES
- 1.National Kidney Foundation. K/DOQI clinical practice guidelines for chronic kidney disease:evaluation, classification, and stratification. Am J Kidney Dis. 2002;39(2 Suppl 1):S1–266. [PubMed] [Google Scholar]
- 2.Zoccali C, Kramer A, Jager KJ. Epidemiology of CKD in Europe:an uncertain scenario. Nephrol Dial Transplant. 2010;25:1731–3. doi: 10.1093/ndt/gfq250. [DOI] [PubMed] [Google Scholar]
- 3.Kwan BCH, Kronenberg F, Beddhu S, Cheung AK. Lipoprotein Metabolism and Lipid Management in Chronic Kidney Disease. JASN. 2007;18:1246–61. doi: 10.1681/ASN.2006091006. [DOI] [PubMed] [Google Scholar]
- 4.Pandya V, Rao A, Chaudhary K. Lipid abnormalities in kidney disease and management strategies. World Journal of Nephrology. 2015;4(1):83–91. doi: 10.5527/wjn.v4.i1.83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Trevisan R, Dodesini AR, Lepore G. Proceedings of the Fourth Genoa Meeting on Hypertension, Diabetes, and Renal Diseases:Lipids and Renal Disease. JASN. 2006;17:S145–S147. doi: 10.1681/ASN.2005121320. [DOI] [PubMed] [Google Scholar]
- 6.Cockcroft D, Gault M. Prediction of creatinine clearance from serum creatinine. Nephron. 1976;16:31–41. doi: 10.1159/000180580. [DOI] [PubMed] [Google Scholar]
- 7.National Kidney Foundation. K/DOQI clinical practice guidelines for chronic kidney disease:evaluation, classification and stratification. Am J Kidney Dis. 2002;39(2 Suppl 1):S1–266. [PubMed] [Google Scholar]
- 8.Kaysen GA. Dyslipidemia in chronic kidney disease:Causes and consequences. Kidney International. 2006;70:S55–S58. [Google Scholar]


