Abstract
Context:
Jam injuries of the finger are frequently encountered in general orthopaedic and sports medicine practice. The finger joints in particular are very susceptible to traumatic injury, but in the absence of severe deformity, digital trauma is often downplayed in the hopes of a more rapid return to game play.
Evidence Acquisition:
Articles published from 1966 to 2015 were reviewed to capture historical and current views on the presentation, diagnosis, and treatment of jam injuries in athletes.
Study Design:
Clinical review.
Level of Evidence:
Level 5.
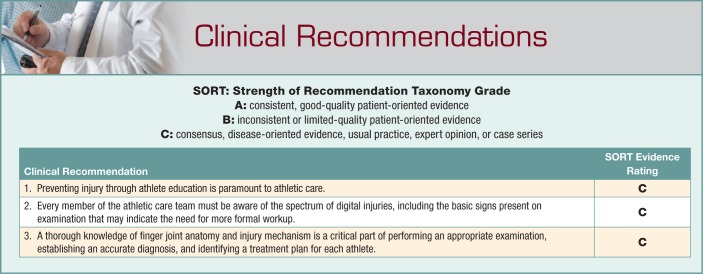
Results:
Although jam injuries are frequently grouped together, they represent a host of injuries that can be challenging to differentiate. A thorough knowledge of finger joint anatomy and injury mechanism is critical to perform an appropriate examination, establish an accurate diagnosis, and identify a treatment plan for each patient.
Conclusion:
Every member of the athletic care team must be aware of the spectrum of digital injuries, including the basic signs present on examination, which may indicate the need for more formal workup. Additionally, preventing injury through athlete education is paramount to athletic care.
Keywords: jam injury, finger injury, dislocation, distal interphalangeal joint, proximal interphalangeal joint
The upper extremity is a frequent site of sport-induced trauma and is often not properly evaluated or treated in the acute setting.9,12,33 The fingers are very susceptible to jam-type injuries, but digital trauma is often downplayed or dismissed by athletes in the hopes that any pain or deformity will resolve without formal intervention.7 Often, however, by delaying treatment the player is unknowingly slowing or jeopardizing his or her ability to regain full function.11,42,44 Athletic trainers and sports medicine physicians are tasked with encouraging athletes to seek medical attention for finger jam injuries and knowing the specifics of diagnosis and management of these common injuries.
This review aims to highlight the most commonly occurring athletic injuries of both the distal interphalangeal (DIP) and proximal interphalangeal (PIP) joints, the treatment options associated with each type of injury, and the evidence supporting any methods for future injury prevention.
Overview and Anatomy of the PIP and DIP Joints
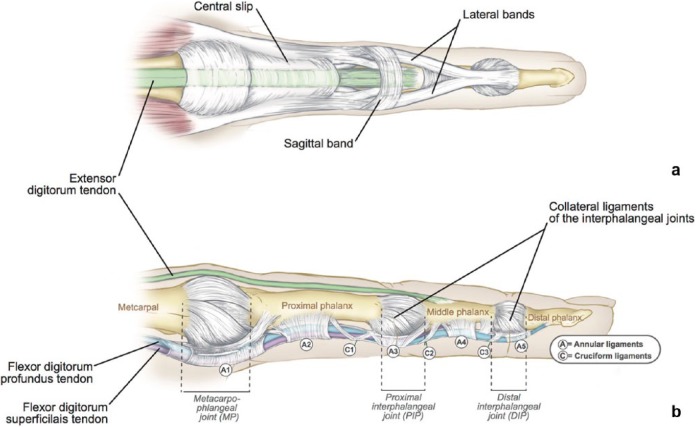
The PIP joint is the single most common location of digital injury in sports.5,43 The hinge motion of the PIP joint allows for flexion and extension from approximately 0° to 110°, and maintenance of this joint is critical to hand function.41,55 Loss of flexion at the PIP joint can decrease both pinch and grip strength and may impair sports performance as well as activities of daily living. The DIP joint functions in a manner similar to the PIP joint; however, the DIP joint has less motion, ranging from about 0° to 80° of flexion. It has yet to be proven whether this added stability is the etiology of the lower frequency of athletic injury to this joint.6,37 Figure 1 illustrates the basic anatomy of both the PIP and DIP joints and the surrounding structures.
Figure 1.
(a) Dorsal and (b) lateral view of the basic anatomic structures that comprise the finger. The proximal interphalangeal (PIP) joint is composed of the proximal and middle phalanges, the radial and ulnar collateral ligaments to provide lateral and medial joint stability to prevent dislocation, and the volar plate to provide stability in the anterior and posterior directions to prevent hyperextension. Each collateral ligament comprises a proper and accessory ligament that opposes each other’s actions. The proper collateral ligament (PCL) is the most important stabilizing structure of the PIP joint in flexion, and the volar portion of the PCL and the proximal portion of the accessory collateral ligament (ACL) stabilize the PIP joint in extension. The central slip reinforces the joint dorsally and helps to resist volar subluxation and dislocation. The DIP joint is made up of the middle and distal phalanges but functions in a manner similar to the PIP joint. The radial and ulnar collateral ligaments and volar plate remain present, but dorsal support is provided by the lateral bands and terminal insertion of the extensor mechanism.
Presentation and Examination of the Jammed Finger
Dislocation events are often easily diagnosed by gross deformity, while other injuries are more subtle and may be missed, particularly in the context of severe edema. A finger that is maintained in a flexed posture may represent a fracture dislocation, pulley rupture injury, or damage to the extensor mechanism. Rarely, injured fingers are held in the extended position, which may signal flexor tendon injuries or dorsal dislocations. After observing the digit, the joint should be gently palpated along the joint line to assess the point of maximal tenderness to evaluate for possible fracture fragments or dislocations.16 The presence of a somewhat mobile mass or fullness along the joint may indicate a tendinous or ligamentous rupture.
Joint stability should then be assessed to determine injury severity. In most cases, if a joint is clinically stable and some range of motion is preserved at the time of injury, an athlete may be allowed to resume play with buddy taping until the completion of competition, when a more thorough workup can be performed. Unstable injuries should be protected to some degree with either a cast or rigid splint to prevent further injury before return to play is considered acceptable.
Radiologic evaluation is needed as early as possible to identify dislocation or fracture. The 3 standard radiographic views of the finger (anteroposterior [AP], lateral, and oblique) are typically obtained in all patients.18 Only occasionally is magnetic resonance imaging (MRI) or ultrasound necessary to evaluate ligamentous injury.40
Injuries of the PIP Joint
Collateral Ligament Injuries
Mechanism
Figure 2 describes the deforming forces that lead to an isolated collateral ligament injury at the PIP joint. A study by McCue et al28 reported that collateral ligament injury occurs most commonly in football players and that the right index finger radial collateral ligament (RCL) is the most common site of occurence. However, combined injury to both collateral ligaments of the PIP joint is more common than isolated injuries to either radial or ulnar collateral ligaments.
Figure 2.
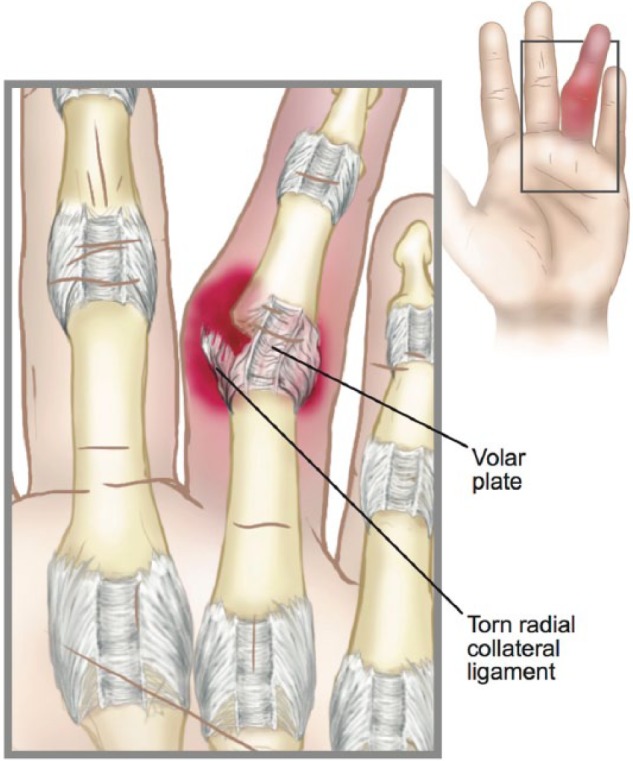
Injury to the collateral ligaments of the proximal interphalangeal (PIP) joint is the result of a radially or ulnarly directed force applied to the distal finger, causing rapid digital deviation at the PIP joint and subsequent rupture of the stabilizing ligaments on the contralateral side of the finger.
Physical Examination
Patients with injury of the collateral ligaments present with focal pain and tenderness at the radial or ulnar side of the joint and significant swelling and ecchymosis of the finger. Collateral ligament rupture can be assessed clinically based on the presence of lateral instability when the PIP joint is stressed. The proper collateral ligament is assessed by flexing the finger to 30° and applying an isolated radially or ulnarly directed stress. A similar maneuver in full joint extension will isolate the accessory collateral ligament. An opening of the joint space beyond 10° of medial or lateral angulation is indicative of ligament injury.43
Treatment
Provided the joint remains clinically stable, collateral ligament injuries are amenable to nonoperative management using a rigid protective splint worn full-time for 3 weeks.28 Most athletes are able to continue sports participation during treatment of collateral ligament tears, though glove wear and grip strength may be compromised. In very rare cases, interposed soft tissue within the articular space will preclude joint motion and require removal with primary ligamentous repair. In these cases, players can expect a longer recovery time and often a stiffer joint, which may require postoperative hand therapy.
Outcome
The functional results of ligamentous injury are related to the severity of the injury. In the event that no treatment is sought in the acute setting, long-term outcomes can include joint pain, deformity, recurrent instability, and, rarely, degenerative changes. Delayed primary repair of the collateral ligaments is undertaken occasionally with relative success, yet these repairs often result in a decreased range of motion at the affected joint and have not been tested in the setting of high-use athletes.32
Volar Plate Injuries
Mechanism
Hyperextension injuries to the PIP joint commonly threaten the integrity of the volar plate and can lead to volar plate sprains, tears, or avulsions. These types of injuries are commonly seen in athletes engaged in ball-handling sports and can present as an isolated injury or in combination with other bony or ligamentous pathology.6,51 An early study by Degroot and Mass7 demonstrated a high occurrence of isolated volar plate injuries in softball players. In this report, 38% of injuries led to avulsion of the volar plate from its insertion on the middle phalanx.
Physical Examination
To assess possible volar plate injuries, gentle pressure is applied to the dorsal aspect of the digit. If injured, this will expose laxity in the volar translation, with no fixed endpoint in PIP extension.36 Joint hyperextension should be compared with the same digit on the opposite hand to rule out a nonpathologic cause for generalized joint laxity.
Imaging
Findings on plain-film radiographs are outlined in Figure 3.
Figure 3.

Lateral views of the proximal interphalangeal (PIP) joint are used in diagnosing volar plate avulsion injuries. Often the injury is demonstrated by the presence of a small, avulsed fragment of the base of the middle phalanx, which is displaced volarly (arrow).
Outcome
Isolated volar plate avulsion injuries that are not associated with joint instability are amenable to early mobilization of the PIP joint, with progressive range of motion exercises beginning 1 week after injury.43 This regimen is typically sufficient to prevent long-term complications, specifically flexion contractures leading to pseudo-boutonniere deformities, which may be encountered if the joint is not properly stretched. Surgical intervention is typically only considered when volar plate tear results in avulsion of a bony fragment constituting more than 40% of the articular surface, which renders the joint unstable. In these cases, open reduction and primary reattachment of the volar plate may be indicated.28 Most commonly, contact athletes require protection from hyperextension stress during the first 6 weeks of healing. All other athletes are allowed to return to unrestricted activities and would risk iatrogenic harm by prolonged immobilization.
Central Slip and Boutonniere Injuries
Mechanism
Trauma to the central slip is seen most often in basketball players, with the typical mechanism of injury being a rapid forced flexion of the PIP joint. Clinically evident injury to the central slip can range from tendon rupture to dorsal avulsion fractures of the middle phalanx with volar dislocations of the PIP joint.38
Physical Examination
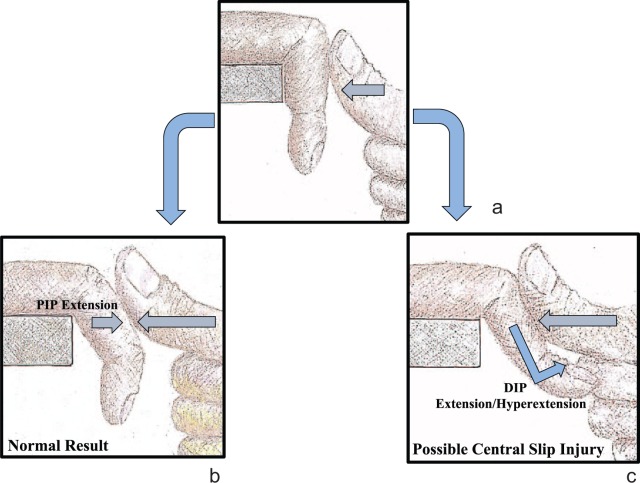
Central slip injuries may not be immediately apparent on cursory examination after trauma, so a complete history from the patient is of critical importance. Typically, the athlete will recall “jamming” his or her finger on a ball or opponent but cannot necessarily distinguish a flexion- or hyperextension-type injury.27 The Elson test can be useful in the identification of possible central slip injuries (Figure 4).21,26,28
Figure 4.
Schematic of the Elson test used to identify injury to the central slip. (a) The patient places his or her hand over the edge of a surface with the digits flexed at the proximal interphalangeal (PIP) joint and hanging freely. The examiner applies firm, constant pressure to the digit in question at the level of the middle phalanx. The patient then attempts to extend the finger at the PIP joint in opposition to the examiner’s applied force. (b) If the patient is able to extend the PIP joint while the distal interphalangeal (DIP) joint remains pliable, it can be concluded that the central slip is intact. (c) If there is an injury to the central slip, the patient will only be able to extend the PIP joint through the use of the lateral bands, which will lead to DIP joint rigidity and concomitant extension or even hyperextension through the DIP joint.
Imaging
Plain films are used to identify whether an avulsion injury or dislocation has occurred. In the absence of these findings, MRI may occasionally be utilized to characterize soft tissue pathology.43
Treatment
Nonsurgical treatment is successful for the majority of athletes presenting with a central slip tear. Typically, the conservative treatment includes 6 weeks of rigid extension splinting at the PIP joint using a clamshell-type splint, allowing for full range of motion at the DIP joint, followed by 3 weeks of soft sleeve splinting only during the night. Although it is preferable to have approximately 3 weeks of continuous rigid splinting before returning to gameplay, some elite athletes may be allowed to have immediate return to practice if proper precautions are taken. These precautions include pregame heat therapy, soft splinting during game play, and postgame icing with return to a rigid splint.23,54 Surgery is only considered for large avulsion injuries that are not easily reducible on examination and in cases where nonoperative management has failed.50
Outcome
The ultimate goal of treating a central slip injury is to prevent the progression to a boutonniere deformity. If left untreated, PIP flexion and DIP hyperextension can result in as little as 2 to 3 weeks postinjury.52 Once a boutonniere deformity is established, correction should be attempted with serial digital casting.52 While this technique has been shown to be moderately successful, surgical correction may be needed when the injury is long-standing or if the gross deformity is severe.28
Dislocations
Mechanism
There are 3 main types of dislocations that can occur at the PIP joint, which are classified based on the direction of displacement of the middle phalanx: dorsal dislocations, lateral dislocations, and volar dislocations. Dorsal dislocations are commonly associated with hyperextension injuries and can therefore be seen in conjunction with damage to the volar plate. Lateral dislocations are caused by laterally directed forces and result in damage to the collateral ligaments. Finally, pure volar dislocations are the most uncommon type of PIP dislocation seen in athletes and are frequently correlated with damage to the central slip.13,43
Physical Examination
Dislocation results in abnormal angulation of the PIP joint, which is easily identifiable on visual inspection.
Treatment
Dorsal dislocations are most amenable to reduction in the acute setting, while volar dislocations may be complicated by soft tissue entrapment, which could require operative treatment. Simple traction applied to the affected digit can frequently pull the displaced phalanges back into alignment, especially if this is attempted prior to the onset of significant edema. However, an apparent reduction does not eliminate the need for postgame evaluation and splint placement to prevent redislocation in the acute setting.1,13,43
Volar dislocations can be further complicated by rotary displacement with an associated collateral ligament injury, which is the result of both lateral and dorsal forces simultaneously applied to the joint.2,15 Typically, the middle phalanx rotates along the intact collateral ligament, causing the lateral condyle to become entrapped between the lateral band and the collaterals. This ultimately leads to distention of the collaterals, which may have become entrapped, causing collateral ligament rupture. The reduction maneuver for volar rotatory dislocations of the PIP joint is important to know (Figure 5). However, occasionally, closed reduction attempts are unsuccessful and it is necessary to perform an operative open reduction and Kirschner wire (K-wire) fixation.10
Figure 5.
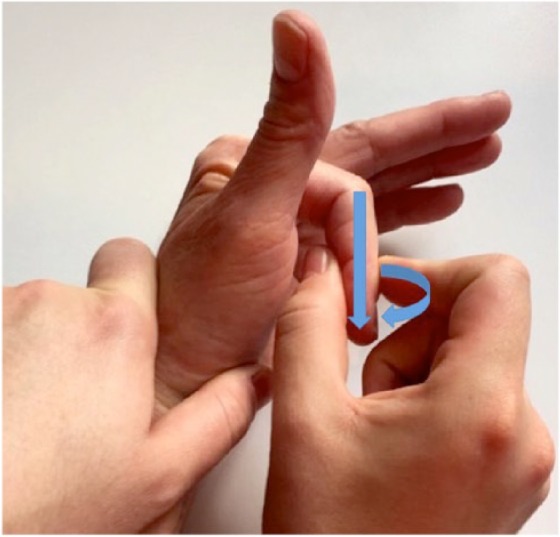
Reduction maneuver required to correct a volar rotary dislocation. The patient’s hand is held with his or her wrist in slight extension and the digit in flexion at both the metacarpophalangeal (MCP) and proximal interphalangeal (PIP) joints. The physician then applies constant traction to the distal portion of the finger, followed by a gradual rotation through the PIP joint leading to reduction of the dislocation.
Although radiographs are typically not necessary to diagnose simple PIP joint dislocations, imaging can be helpful to determine the success of a closed reduction attempt and identification of fracture-dislocation injuries. A minimum of 2 orthogonal views should always be obtained, but it is the lateral view that is most helpful when assessing the congruity of the articular surfaces.
Outcome
The goals of treatment are to maintain a congruent joint long term and to promote early mobilization to prevent joint stiffness and pain. For injuries that are stable after reduction, buddy taping is a reasonable option, and early return to play may be allowed. For athletes involved in contact sports, however, temporarily wearing a soft, slip-on splint combined with buddy taping is a preferred option. In the context of gross instability after reduction in a contact-sport athlete, a rigid splint should be applied. This form of protective fixation should not be left in place for longer than 3 weeks, as prolonged wear often results in joint stiffness.40
Fracture-Dislocations
PIP dislocations that occur under a high level of force can result in a concomitant fracture of the middle phalanx. PIP fracture-dislocations are complex injuries that necessitate recognition by sports trainers and general orthopaedists but may warrant evaluation by a hand surgeon for appropriate surgical intervention.8,22,53
Injuries of the DIP Joint
Collateral Ligament Injuries
Injury of the collateral ligaments at the DIP joint is a rare occurrence, even in an active athlete. This low rate of occurrence may be due to the relative stability of the DIP joint compared with that of the PIP joint. The stability of the DIP joint is primarily imparted by the extensive adherent soft tissues. Additionally, the distal phalanx, being shorter than the middle and distal phalanges combined, provides a shorter lever arm and therefore less torque for inducing injury. Finally, collateral ligament injury at the DIP joint may be more difficult to diagnose than more obvious proximal injuries, leading to fewer reported cases and even fewer management options.56
Mallet Fingers and Associated Swan Neck Deformities
Mechanism
Mallet finger injuries are often encountered in baseball, softball, and basketball, but can occur in almost any sport (Figure 6). Mallet injuries most commonly occur in the ulnar 3 digits, though the reason for this remains unclear.21 Despite the frequency of mallet injuries, these injuries are often underestimated and undertreated.
Figure 6.

Mallet finger injuries occur after forced flexion of the distal interphalangeal (DIP) joint during active joint extension. The “mallet” appearance of the finger results from the avulsion of the terminal extensor tendon and the resultant loss of continuity of the extensor mechanism, leading to the loss of active DIP extension and (a) the classic flexed posture at the DIP joint due to the unopposed pull of the flexor digitorum profundus (FDP) tendon. (B) Lateral view plain-film radiograph of a swan-neck deformity, as demonstrated by DIP flexion and proximal interphalangeal (PIP) hyperextension, secondary to a chronic mallet injury.
Physical Examination
Mallet injuries present with loss of active DIP extension, along with a flexed posture at that same joint, due to the unopposed pull of the flexor digitorum profundus (FDP) tendon (Figure 6a) and dorsal edema at the middle phalanx, where the extensor tendon sits retracted. Soft tissue mallet injuries may not be painful when they occur, but pain or tenderness at the DIP joint should increase suspicion for an avulsion fracture.27
Imaging
Lateral radiographs are critical to differentiate soft tissue and bony mallets from isolated DIP dislocations and can also be useful to determine the presence of volar subluxation.6
Treatment
Isolated soft tissue mallet injuries and mallet injuries with small bony avulsions are amenable to splinting in the acute setting.49 Fractures associated with volar subluxation of the DIP joint or fractures involving more than 40% of the articular surface of the distal phalanx are associated with predictable instability and require surgical fixation for optimal outcomes.7
For closed, stable injuries, a rigid splint is utilized for 6 to 12 weeks, typically until the extension lag disappears. Generally, athletes are weaned from full-time splinting at 8 weeks, with careful return to gameplay in a protective splint for an additional 4 weeks.30 Clinical results of nonoperative treatment are correlated with compliance with splint wear.39 It is important to emphasize to the patient that splint use must be continuous.
The goal of surgical intervention is the reduction of the DIP joint, and multiple surgical options have been described. Regardless of tendon repair technique, most surgical treatments are reinforced with a K-wire to stabilize and protect the joint repair for 6 to 8 weeks. Multiple rehabilitation protocols have been suggested but limited data exist at this time to suggest that 1 protocol is superior to another.27
Outcome
The long-term complications of mallet injuries include interphalangeal (IP) joint stiffness, loss of reduction, and development of PIP joint hyperextension leading to the formation of a swan neck deformity (Figure 6b).20 Multiple studies have shown that a slight extensor lag is frequently present after nonoperative treatment of uncomplicated mallet injuries. However, as long as the patient has full flexion, there is rarely a loss of grip strength, and some degree of extensor lag is typically acceptable for daily activities and most athletic endeavors.21
Correction of a swan-neck deformity is exceptionally difficult and may not improve patient function.4
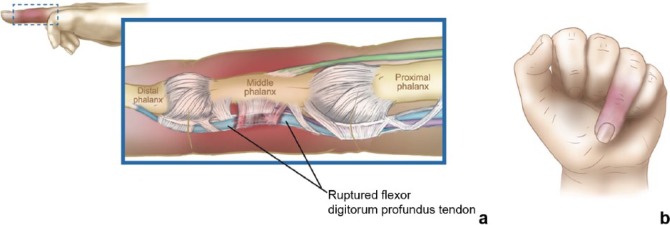
Jersey Fingers
Mechanism
Jersey finger injuries are reasonably common, especially in athletes.11,19 The mechanism of injury is outlined in Figure 7a. Sporting activities most commonly associated with jersey fingers are those with frequent physical contact between players, such as football, rugby, or soccer.3 The ring finger is the most common site of injury, accounting for nearly 75% of injuries. This may be due to the relative length of the ring finger during fist or gripping motions.14
Figure 7.
The name “jersey finger” is derived from the common cause of injury, which is when a player’s finger is caught in an opponent’s jersey and forcibly extended during resisted flexion. (a) This results in rupture of the flexor digitorum profundus (FDP) tendon and, occasionally, an avulsion injury at the FDP insertion point on the distal phalanx. (b) As a result, active flexion of the distal interphalangeal (DIP) joint is no longer possible.
Physical Examination
On examination, jersey fingers are identified by an inability to actively flex the DIP joint (Figure 7b) and point tenderness and/or swelling at the palmar aspect of the digit where the retracted, avulsed FDP tendon can be palpated within or just proximal to the tendon sheath.
Treatment
Avulsion of the FDP can occur as an isolated tendinous injury or a bony avulsion, so radiographs are necessary to characterize the injury and for surgical planning. When necessary, augmenting the physical examination with ultrasound and MRI can be useful in determining the degree of proximal tendon retraction.38
Almost all cases of jersey finger in athletes will be treated surgically, and most surgeons advocate for surgical repair as soon as possible to ensure that primary repair is possible.14 If the tendon has retracted to a point that it cannot be stretched back to its original insertion point, tendon grafting should be considered.
Outcome
Postoperative rehabilitation after flexor tendon repair is a complex topic, but nearly all hand surgeons employ some early motion protocol to minimize the chance of flexor tendon adhesions and to improve the strength of the repair. Athletes who sustain jersey fingers should expect full return to sport within 4 months. In select cases where athletes are not heavily dependent on a complete grip for their sport, they may be allowed to have an earlier return to play with the use of a protective splint.35
Pulley Ruptures
Mechanism
While ruptures of the digital pulley system are relatively uncommon injuries, they are somewhat common in athletes who utilize a “crimping” grip, such as rock climbers and baseball pitchers.31 The “crimped” position places high forces on the pulleys, making them more susceptible to rupture.48 The most common sites of pulley rupture are at the A2 and A4 pulleys in the middle and ring fingers due to the combination of biomechanical factors that come into play when force is applied to the “crimping” grip hand position.23 Multiple sequential pulley ruptures are discussed in Figure 8.
Figure 8.
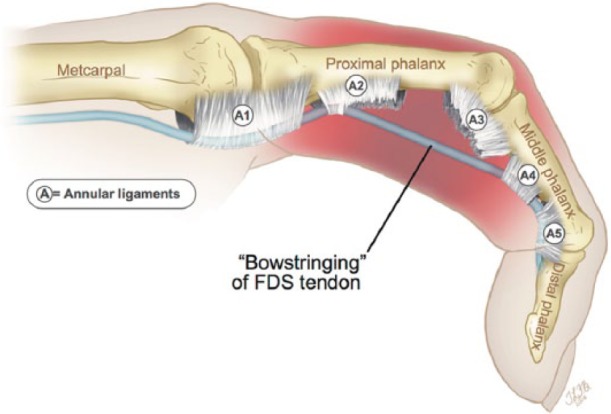
Pulley ruptures can be complete or partial and can occur at 1 or multiple sites in any single digit. Injury to multiple sequential pulley structures may lead to a bowstringing deformity on resting flexion that is evident on physical examination. FDS, flexor digitorum superficialis.
Physical Examination
With acute pulley ruptures, athletes typically describe a popping sound at the time of injury, which occurs when a load is applied to a flexed finger. Typically, athletes will present with mild to moderate pain and swelling of the tendon in the sheath. Flexion and extension lags are common, either due to swelling or bowstringing of the tendons.24,57
Imaging
MRI or ultrasound can be used to confirm rupture of the pulley system. Images should be inspected to identify an increased distance between the phalanges and tendon sheath, which can be indicative of a pulley rupture. Occasionally, sequential imaging is done in a flexed and extended position to demonstrate bowstringing.47
Treatment
Most isolated pulley ruptures can be treated nonsurgically. Pulley reconstruction is considered when multiple sequential pulleys are ruptured to prevent flexion contractures and loss of terminal flexion.46 Nonoperative treatment includes rest, pulley ring splinting, and oral anti-inflammatory medications. Steroid injections are generally discouraged as they may delay healing.
Outcome
After about 1 week of rest, sports may slowly be reintroduced along with active and passive tendon gliding exercises to prevent stiffness. With return to sport, protective taping is frequently employed. Full return to sports is typically not possible until 2 to 3 months after injury, and some advocate for protective digital taping for up to 6 months.35 Some athletes, specifically climbers, may choose to continue taping indefinitely as it provides a sense of security and strength to the digit. However, studies have not shown this to be beneficial in preventing reinjury of the pulley system.45
Summary
Jam injuries are an extremely common occurrence in almost all areas and levels of athletics. However, athletes often attempt to minimize pain and deformity in an effort to prevent loss of practice or game time in their sport of choice.9,25 The term “jam injury” encompasses a wide range of very specific bony and soft tissue injuries, some with relatively benign treatment plans and outcomes and others that result in serious, long-term ramifications, even with the appropriate treatment. It is often the responsibility of the trainer or team physician to identify whether a serious digital injury has occurred and when to refer their athlete to a hand surgeon for definitive treatment. It is therefore crucial that every member of the athletic team be aware of the spectrum of injuries, as well as some of the basic signs present on examination that may indicate the need for more formal workup, as a missed diagnosis could ultimately lead to a prolonged absence from sport or worse long-term functional result.34
Preventing injury through athlete education is paramount to athletic care. In addition to a thorough history and physical examination, radiographic evaluation is often needed.17,29 A thorough knowledge of finger joint anatomy and injury mechanism will always be a critical part of performing an appropriate examination, establishing an accurate diagnosis, and identifying a proven treatment plan for each athlete.
Footnotes
The authors report no potential conflicts of interest in the development and publication of this article.
References
- 1. Bach AW. Finger joint injuries in active patients: pointers for acute and late-phase management. Phys Sportsmed. 1999;27:89-104. [DOI] [PubMed] [Google Scholar]
- 2. Bindra RR, Foster BJ. Management of proximal interphalangeal joint dislocations in athletes. Hand Clin. 2009;25:423-435. [DOI] [PubMed] [Google Scholar]
- 3. Blazina ME, Lane C. Rupture of the insertion of the flexor digitorum profundus tendon in student athletes. J Am Coll Health Assoc. 1966;14:248-249. [PubMed] [Google Scholar]
- 4. Chauhan A, Jacobs B, Andoga A, Baratz ME. Extensor tendon injuries in athletes. Sports Med Arthrosc. 2014;22:45-55. [DOI] [PubMed] [Google Scholar]
- 5. Chen J, Tan J, Zhang AX. In vivo length changes of the proximal interphalangeal joint proper and accessory collateral ligaments during flexion. J Hand Surg Am. 2015;40:1130-1137. [DOI] [PubMed] [Google Scholar]
- 6. Dawson WJ. The spectrum of sports-related interphalangeal joint injuries. Hand Clin. 1994;10:315-326. [PubMed] [Google Scholar]
- 7. Degroot H, Mass DP. Hand injury patterns in softball players using a 16 inch ball. Am J Sports Med. 1988;16:260-265. [DOI] [PubMed] [Google Scholar]
- 8. Deitch MA, Kiefhaber TR, Comisar BR, Stern PJ. Dorsal fracture dislocations of the proximal interphalangeal joint: surgical complications and long-term results. J Hand Surg Am. 1999;24:914-923. [DOI] [PubMed] [Google Scholar]
- 9. Dobyns JH, Sim FH, Linscheid RL. Sports stress syndromes of the hand and wrist. Am J Sports Med. 1978;6:236-254. [DOI] [PubMed] [Google Scholar]
- 10. Ellsasser JC, Stein AH. Management of hand injuries in a professional football team. Review of 15 years of experience with one team. Am J Sports Med. 1979;7:178-182. [DOI] [PubMed] [Google Scholar]
- 11. Freilich AM. Evaluation and treatment of jersey finger and pulley injuries in athletes. Clin Sports Med. 2015;34:151-166. [DOI] [PubMed] [Google Scholar]
- 12. Gaston RG, Loeffler BJ. Sports-specific injuries of the hand and wrist. Clin Sports Med. 2015;34:1-10. [DOI] [PubMed] [Google Scholar]
- 13. Geissler WB, Burkett JL. Ligamentous sports injuries of the hand and wrist. Sports Med Arthrosc. 2014;22:39-44. [DOI] [PubMed] [Google Scholar]
- 14. Goodson A, Morgan M, Rajeswaran G, Lee J, Katsarma E. Current management of jersey finger in rugby players: case series and literature review. Hand Surg. 2010;15:103-107. [DOI] [PubMed] [Google Scholar]
- 15. Green D, Hotchkiss R, Pederson W. Green’s Operative Hand Surgery. 4th ed. Philadelphia, PA: Churchill Livingstone; 1999. [Google Scholar]
- 16. Hankin FM, Peel SM. Sport-related fractures and dislocations in the hand. Hand Clin. 1990;6:429-453. [PubMed] [Google Scholar]
- 17. Isani A. Prevention and treatment of ligamentous sports injuries to the hand. Sports Med. 1990;9:48-61. [DOI] [PubMed] [Google Scholar]
- 18. Kenney RJ, Hammert WC. Physical examination of the hand. J Hand Surg Am. 2014;39:2324-2334. [DOI] [PubMed] [Google Scholar]
- 19. Leddy JP, Packer JW. Avulsion of the profundus tendon insertion in athletes. J Hand Surg Am. 1977;2:66-69. [DOI] [PubMed] [Google Scholar]
- 20. Leinberry C. Mallet finger injuries. J Hand Surg Am. 2009;34:1715-1717. [DOI] [PubMed] [Google Scholar]
- 21. Lin JD, Strauch RJ. Closed soft tissue extensor mechanism injuries (mallet, boutonniere, and sagittal band). J Hand Surg Am. 2014;39:1005-1011. [DOI] [PubMed] [Google Scholar]
- 22. London PS. Sprains and fractures involving the interphalangeal joints. Hand. 1971;3:155-158. [DOI] [PubMed] [Google Scholar]
- 23. Lourie GM, Marino JT. Boutonnière and pulley rupture in elite athletes. Hand Clin. 2012;28:437-445. [DOI] [PubMed] [Google Scholar]
- 24. Lourie GM, Hamby Z, Raasch WG, Chandler JB, Porter JL. Annular flexor pulley injuries in professional baseball pitchers: a case series. Am J Sports Med. 2011;39:421-424. [DOI] [PubMed] [Google Scholar]
- 25. Mall NA, Carlisle JC, Matava MJ, Powell JW, Goldfarb CA. Upper extremity injuries in the National Football League: part I: hand and digital injuries. Am J Sports Med. 2008;36:1938-1944. [DOI] [PubMed] [Google Scholar]
- 26. Marino JT, Lourie GM. Boutonnière and pulley rupture in elite athletes. Hand Clin. 2012;28:437-445. [DOI] [PubMed] [Google Scholar]
- 27. Matzon JL, Bozentka DJ. Extensor tendon injuries. J Hand Surg Am. 2010;35:854-861. [DOI] [PubMed] [Google Scholar]
- 28. McCue FC, Honner R, Johnson MC, Gieck JH. Athletic injuries of the proximal interphalangeal joint requiring surgical treatment. J Bone Joint Surg Am. 1970;52:937-956. [PubMed] [Google Scholar]
- 29. McCue FC, Meister K. Common sports hand injuries. An overview of etiology, management and prevention. Sports Med. 1993;15:281-289. [DOI] [PubMed] [Google Scholar]
- 30. McMurtry JT, Isaacs J. Extensor tendons injuries. Clin Sports Med. 2015;34:167-180. [DOI] [PubMed] [Google Scholar]
- 31. Merritt AL, Huang JI. Hand injuries in rock climbing. J Hand Surg Am. 2011;36:1859-1861. [DOI] [PubMed] [Google Scholar]
- 32. Miyake J, Masatomi T, Murase T, Takahi K, Moritomo H, Yoshikawa H. Corrective osteotomy and ligament repair for longstanding radial collateral ligament tear of the proximal interphalangeal joint: case series. J Hand Surg Am. 2012;37:440-445. [DOI] [PubMed] [Google Scholar]
- 33. Morgan WJ, Slowman LS. Acute hand and wrist injuries in athletes: evaluation and management. J Am Acad Orthop Surg. 2001;9:389-400. [DOI] [PubMed] [Google Scholar]
- 34. Mosher JF. Current concepts in the diagnosis and treatment of hand and wrist injuries in sports. Med Sci Sports Exerc. 1985;17:48-55. [PubMed] [Google Scholar]
- 35. Neumann JA, Leversedge FJ. Flexor tendon injuries in athletes. Sports Med Arthrosc. 2014;22:56-65. [DOI] [PubMed] [Google Scholar]
- 36. Paschos NK, Abuhemoud K, Gantsos A, Mitsionis GI, Georgoulis AD. Management of proximal interphalangeal joint hyperextension injuries: a randomized controlled trial. J Hand Surg Am. 2014;39:449-454. [DOI] [PubMed] [Google Scholar]
- 37. Patel D, Dean C, Baker RJ. The hand in sports: an update on the clinical anatomy and physical examination. Prim Care. 2005;32:71-89. [DOI] [PubMed] [Google Scholar]
- 38. Peterson JJ, Bancroft LW. Injuries of the fingers and thumb in the athlete. Clin Sports Med. 2006;25:527-542. [DOI] [PubMed] [Google Scholar]
- 39. Pike J, Mulpuri K, Metzger M, Ng G, Wells N, Goetz T. Blinded, prospective, randomized clinical trial comparing volar, dorsal, and custom thermoplastic splinting in treatment of acute mallet finger. J Hand Surg Am. 2010;35:580-588. [DOI] [PubMed] [Google Scholar]
- 40. Prucz RB, Friedrich JB. Finger joint injuries. Clin Sports Med. 2015;34:99-116. [DOI] [PubMed] [Google Scholar]
- 41. Rettig AC. Epidemiology of hand and wrist injuries in sports. Clin Sports Med. 1998;17:401-406. [DOI] [PubMed] [Google Scholar]
- 42. Rettig AC. Athletic injuries of the wrist and hand: part II: overuse injuries of the wrist and traumatic injuries to the hand. Am J Sports Med. 2004;32:262-273. [DOI] [PubMed] [Google Scholar]
- 43. Rosner JL, Zlatkin MB, Clifford P, Ouellette EA, Awh MH. Imaging of athletic wrist and hand injuries. Semin Musculoskelet Radiol. 2004;8:57-79. [DOI] [PubMed] [Google Scholar]
- 44. Scalcione LR, Pathria MN, Chung CB. The athlete’s hand: ligament and tendon injury. Semin Musculoskelet Radiol. 2012;16:338-349. [DOI] [PubMed] [Google Scholar]
- 45. Schoffl I, Einwag F, Strecker W, Hennig F, Schoffl V. Impact of taping after finger flexor tendon pulley ruptures in rock climbers. J Appl Biomech. 2007;23:52-62. [DOI] [PubMed] [Google Scholar]
- 46. Schöffl V, Küpper T, Hartmann J, Schöffl I. Surgical repair of multiple pulley injuries—evaluation of a new combined pulley repair. J Hand Surg Am. 2012;37:224-230. [DOI] [PubMed] [Google Scholar]
- 47. Schöffl VR, Jüngert J. Closed flexor pulley injuries in nonclimbing activities. J Hand Surg Am. 2006;31:806-810. [DOI] [PubMed] [Google Scholar]
- 48. Schöffl VR, Schöffl I. Injuries to the finger flexor pulley system in rock climbers: current concepts. J Hand Surg Am. 2006;31:647-654. [DOI] [PubMed] [Google Scholar]
- 49. Segmueller HE. Mallet finger injuries. J Hand Surg Am. 2010;35:693. [DOI] [PubMed] [Google Scholar]
- 50. Smith DW. Boutonnière and pulley rupture in elite basketball. Hand Clin. 2012;28:449-450. [DOI] [PubMed] [Google Scholar]
- 51. Sundaram N, Bosley J, Stacy GS. Conventional radiographic evaluation of athletic injuries to the hand. Radiol Clin North Am. 2013;51:239-255. [DOI] [PubMed] [Google Scholar]
- 52. To P, Watson JT. Boutonniere deformity. J Hand Surg Am. 2011;36:139-142. [DOI] [PubMed] [Google Scholar]
- 53. Waris E, Alanen V. Percutaneous, intramedullary fracture reduction and extension block pinning for dorsal proximal interphalangeal fracture-dislocations. J Hand Surg Am. 2010;35:2046-2052. [DOI] [PubMed] [Google Scholar]
- 54. Weiland AJ. Boutonnière and pulley rupture in elite baseball players. Hand Clin. 2012;28:447. [DOI] [PubMed] [Google Scholar]
- 55. Williams CS. Football commentary: PIP fracture. Hand Clin. 2012;28:423-424. [DOI] [PubMed] [Google Scholar]
- 56. Yasuda M, Masada K, Takeuchi E. Isolated rupture of radial collateral ligament of the small finger DIP joint repaired with a bone suture anchor: a case report. Hand Surg. 2004;9:121-124. [DOI] [PubMed] [Google Scholar]
- 57. Zafonte B, Rendulic D, Szabo RM. Flexor pulley system: anatomy, injury, and management. J Hand Surg Am. 2014;39:2525-2532. [DOI] [PubMed] [Google Scholar]