Abstract
Background:
Though rehabilitation attempts to correct “stiff knee gait” and control for dynamic limb valgus after anterior cruciate ligament reconstruction (ACLR), impaired biomechanics often persist when an individual is cleared to return to sport (RTS). Reduced knee extension moments (KEMs) and knee flexion angles (KFAs) often continue. While at the hip, increased hip adduction angles (HADDAs) and hip internal rotation angles (HIRAs) often persist in spite of dynamic hip stabilization exercises. Sled towing and weighted vest tasks increase KEM and hip extension moments (HEMs) in healthy individuals, yet biomechanical profiles during these tasks after ACLR are unknown.
Hypothesis:
Weighted gait will increase KEM, HEM, hip abduction moments (HABDMs), and hip external rotation moments (HERMs) and will not increase unwanted biomechanics (limb asymmetries, HIRA, HADDA) compared with normal gait.
Study Design:
Controlled laboratory study.
Level of Evidence:
Level 4.
Methods:
Fourteen men and 24 women who were 5 to 12 months after ACLR, had no concomitant ligament injuries, and were cleared to RTS were recruited. Sexes were evaluated independently given the sex-specific incidence to ACL injury, reinjury, and gait responses to certain interventions. Joint moment impulses and peak angles over the first 25% of stance were compared between limbs and across tasks (eg, unweighted gait, sled 50% body weight [BW], and vest 50% BW).
Results:
Men showed that weighted gait increased KEM, HEM, HERM, HADBM (vest only), HADDA, HIRA (sled only), and KFA. Asymmetrical KEM and KFA existed across tasks. Women showed that weighted gait increased KEM, HEM, HERM, HADBM (vest only), HFA (sled only), HADDA, and KFA. Asymmetrical KEM, HEM, HIRA, and KFA (sled only) existed across tasks.
Conclusion:
Weighted gait generally increased joint moments. Unwanted biomechanics were unique for each weighted gait task.
Clinical Relevance:
Though joint moments increased, both tasks created unwanted biomechanics after ACLR. Persistent hip (women only) and KEM asymmetries across tasks when cleared to RTS are concerning given the relationship among these biomechanics and decreased functional performance.
Keywords: rehabilitation, gait mechanics, return to sport
Abnormal biomechanics are present in individuals after anterior cruciate ligament (ACL) rupture, even when ACL reconstruction (ACLR) is performed.3-5 During the early stance phase of gait, a “stiff knee gait pattern” is ubiquitous after ACL injury.20 This “stiff knee gait pattern” includes reduced knee flexion angle (KFA) and reduced knee extension torque (internal knee extension moment [KEM]) in the ACL-deficit limb.20 This pattern does not resolve in the ACLR limb and can persist for years even with rehabilitation.5,16,23 Furthermore, aberrant hip biomechanics, particularly a dynamic lower extremity valgus position (eg, knee position close to or crossing the body’s midline), can persist after rehabilitation and increases risk of rerupture.9,18 Continued use of aberrant biomechanics at the hip and knee after ACLR results in worse functional outcomes,5,18 increases the risk of sustaining a second ACL rupture on return to sports (RTS),18 and may contribute to the development of knee osteoarthritis.7,17,24 Identifying a task that reduces the “stiff knee gait” and dynamic limb valgus is needed for ACLR rehabilitation given the link between aberrant knee and hip biomechanics and poor function.5,18
There is strong evidence that KEM during gait, stepping, hopping, and jumping activities is related to quadriceps strength.16,21,23 However, neither progressive quadriceps strengthening or gait training correct a “stiff knee gait” pattern or restore normal mechanics during the weight acceptance phase of gait.3-6,19 Even when athletes achieve quadriceps strength symmetry after ACLR, reduced KEM in the ACLR limb can persist during gait.5
Evidence suggests that individuals with asymmetrical knee and hip biomechanics during gait are unable to pass RTS criteria; yet those with no hip asymmetries are able to pass RTS criteria.5 This is concerning as individuals who use asymmetrical hip mechanics in conjunction with reduced KEM have worse functional outcomes compared with those with reduced KEM only.4,5,18 Additionally, when an individual with reduced KEM and dynamic limb valgus position lands from a jump, they are at significantly increased risk of recurrent injury.18 Thus, interventions that correct aberrant knee and hip mechanics after ACLR may improve functional outcomes and decrease risk of reinjury.
Both towing a sled with 50% bodyweight (BW) and wearing a 55-kg vest increases knee and hip joint moments in healthy individuals.15,22 The effects of these weighted tasks on the biomechanics in individuals after ACLR are unknown. Identifying the biomechanical profiles of the acute effects of weighted gait is necessary to determine whether interventions that include weighted gait would be suitable to reduce incidence of undesirable biomechanics after ACLR. The biomechanical profile should include the most relevant measures related to “stiff knee gait” (KFA, KEM, hip flexion angles [HFA]), dynamic limb valgus (hip adduction [HADDA] and hip internal rotation angles [HIRA]), moments that have the potential to protect against dynamic limb valgus (eg, hip extension [HEM], abduction [HABDM], and external rotation moments [HERM]), and limb symmetry data.1,5,9,18 This biomechanical profile will drive future intervention studies that will allow clinicians to make a more informed decision about the potential impact of these tasks on individuals after ACLR.
The purpose of this investigation is to report biomechanical profiles during weighted gait in individuals after ACLR who have been cleared to RTS. We hypothesized that weighted gait will (1) increase joint moments (KEM, HEM, HABDM, and HERM) and joint angles (KFA, HFA) and (2) not create unwanted movement patterns (increase HIRA, HADDA, and limb asymmetries).11
Methods
This study was approved by the Institutional Review Board (20120709HARTE) at the University of New England. Two studies were performed: one with male participants and the other with female participants. We analyzed men and women separately to remove the potential influence of sex on gait mechanics.1,4,9
Fourteen men and 24 women were recruited using a sample of convenience. Emails and flyers were used to recruit individuals from the university’s community list and from local orthopaedic and physical therapy practices. Eligible individuals were 14 to 55 years old, 5 to 12 months postsurgery, discharged from physical therapy, and cleared by their physician to RTS. While achieving RTS status at 5 months is atypical, we chose this time to capture individuals who were cleared to RTS early. Individuals were excluded if they had a concomitant knee ligament injury during ACL rupture, surgery within the past 12 months excluding ACLR, knee pain with activity, current use of pain medications, any known cardiac or neurologic pathology, or ACL revisions. This study did not control for type of ACLR, surgeon, or type and length of physical therapy.
Demographic data were collected (Table 1) after the individuals gave written informed consent. Retroreflective markers were placed on the pelvis and lower legs to track limb motion. The method to create a mathematical model of each individual is described in detail elsewhere.15 Motion of the lower extremities was collected for 5 trials during each of the 3 gait tasks: normal walking, walking while pulling a weighted sled, and walking while wearing a weighted vest (Figure 1). Walking speed (1.3 m/s ± 5%) was controlled for using the Brower Timing Gate System (Brower). Weights were placed in the front and back of the vest to ensure equal distribution.22 The nonweighted sled had a weight of 12.33 kg, and plates were added to the sled to reach 50% BW for each individual. Of note, unpublished data from our laboratory indicated that the sled task with 20% BW only significantly increased HEM and did not significantly increase KEM compared with normal gait, thus the impetus for 50% BW. The individual pulled the sled with a shoulder attachment, as this attachment has been shown to increase KEMs.15
Table 1.
Mean (SD) demographics
| Women (n = 24) | Men (n = 14) | |
|---|---|---|
| Age, y | 25.0 (10.8) | 23.9 (12.1) |
| Body mass index, kg/m2 | 23.7 (3.9) | 24.9 (4.1) |
| Time since ACLR, mo | 7.2 (1.8) | 7.9 (1.9) |
| Mechanism of injury | 18 noncontact, 6 contact | 6 noncontact, 8 contact |
| Meniscal involvement | 13 no involvement, 3 tears resected, 8 repaired | 5 no involvement, 6 tears resected, 3 repaired |
ACLR, anterior cruciate ligament reconstruction.
Figure 1.
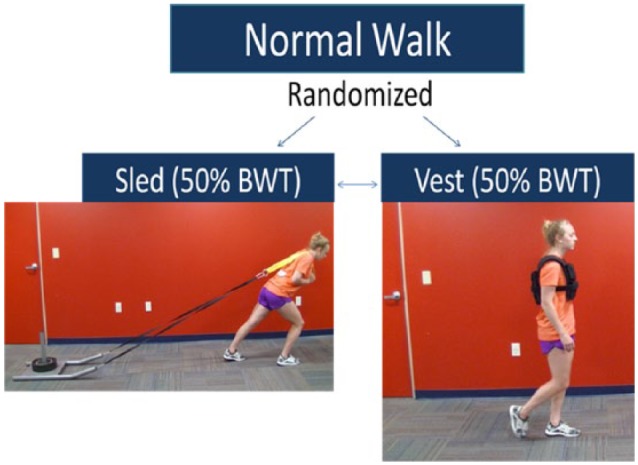
Once normal gait trials were completed, the order of the sled (EliteFTS) and vest (V-Max) tasks were randomized. BWT, body weight.
Each limb was tracked during the stance phase of gait using 8 Oqus Series 3 cameras (Qualisys) set at 120 Hz. Kinetic data were collected using 2 force plates (AMTI) at 1200 Hz. Visual 3D (C-Motion) was used to calculate peak joint angles and internal joint moment impulses for the hip and knee during the first 25% of stance phase.26 Joint moment impulses were chosen over a specific instant in the gait cycle for 2 reasons. First, peak joint angles and moments did not correspond in the time sequence among the 3 tasks (Figure 2), and moment impulses incorporate both time and magnitude components, which are more indicative of joint effort.25 Additional kinematic and kinetic data plotted during the first 25% of stance for all variables of interest are included in the Appendix, available online at sph.sagepub.com/supplemental.
Figure 2.
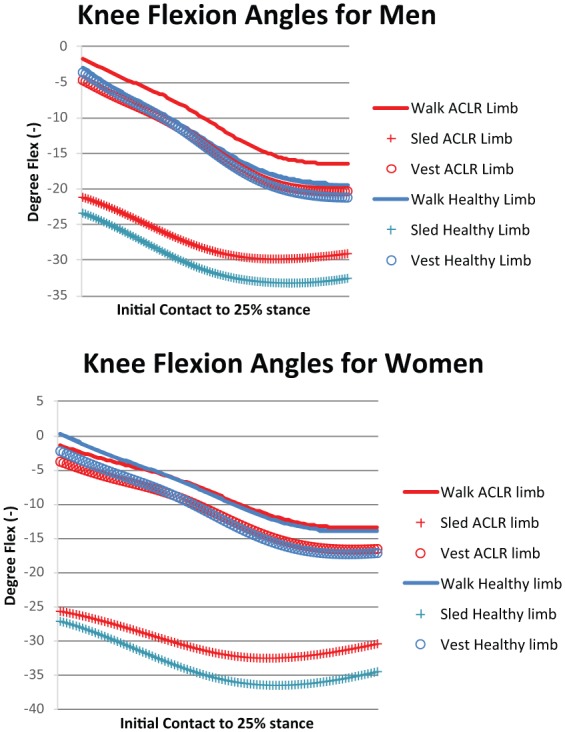
Knee flexion angles during the early stance phase of gait highlight the different knee kinematics between the sled and weighted vest tasks. ACLR, anterior cruciate ligament reconstruction.
Repeated-measures analysis of variance (2 within-subject factors: limb and tasks) were performed using SPSS v21 (IBM Corp) for each measure to compare limbs and tasks. Planned comparisons were performed when significant differences were found for a main effect of task or a task by limb interaction. Alpha was set to P ≤ 0.05.
Results
Men
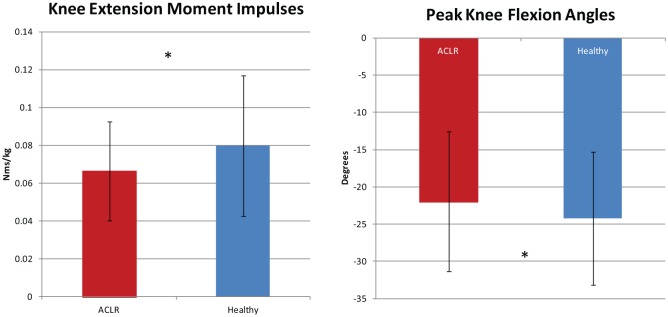
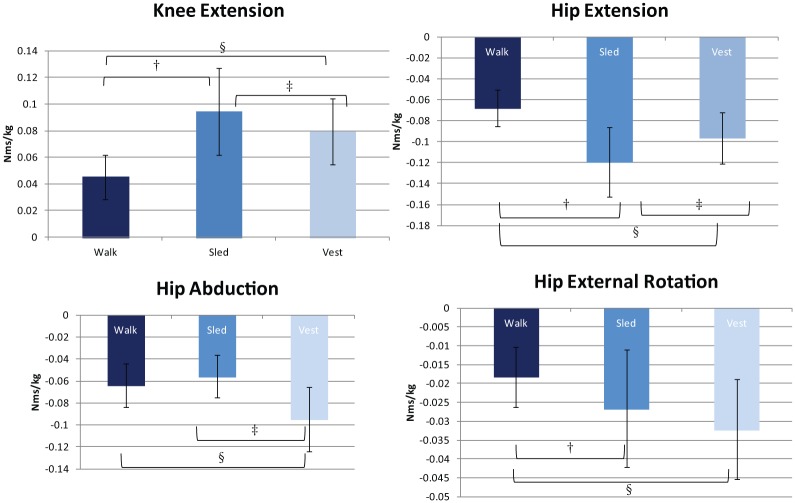
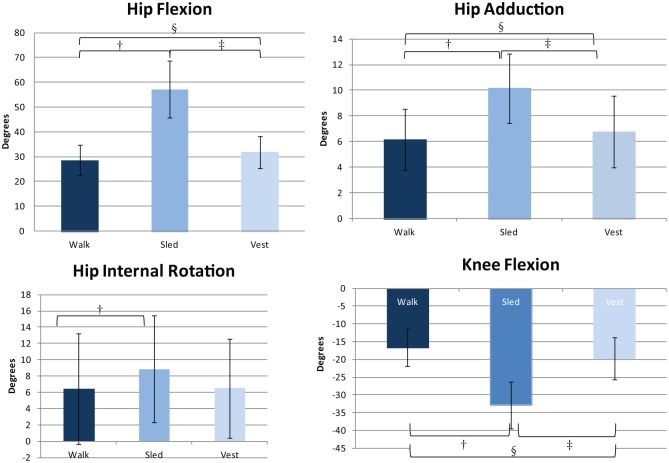
The KEM impulses and KFA for the ACLR limb were significantly less than the healthy limb (Figure 3). All joint moment impulses significantly differed among tasks. Post hoc tests indicated the following: KEM (walk < vest < sled), HEM (walk < vest < sled), HABDM (walk = sled < vest), and HERM (walk < sled = vest) (Figure 4). Peak angles significantly differed among tasks for: HFA, HADDA, and KFA (walk < vest < sled) (Figure 5). Peak HIRA significantly differed between walk and sled tasks (walk < sled, walk = vest, sled = vest) (Figure 6).
Figure 3.
Sagittal plane knee biomechanics illustrate limb differences for men, with data collapsed for tasks. *Significant differences between the anterior cruciate ligament reconstruction (ACLR) and healthy limbs for knee extension moment impulse (mean difference [x], –0.013; P = 0.034; 95% CI, −0.025 to −0.001) and peak knee flexion angles (x, 2.246; P = 0.042; 95% CI, 0.094 to 4.397).
Figure 4.
Knee and hip kinetic illustrate task differences for men, with data collapsed for limb. †Significant difference between walk and sled tasks: knee extension moments (mean difference [x], −0.049; P < 0.001; 95% CI, −0.061 to −0.037), hip extension moments (x, 0.052; P < 0.001; 95% CI, 0.036 to 0.068), and hip external rotation moments (x, 0.008; P = 0.017; 95% CI, 0.002 to 0.015). §Significant difference between walk and vest tasks: knee extension moments (x, −0.034; P < 0.001; 95% CI, −0.042 to −0.026), hip extension moments (x, 0.029; P < 0.001; 95% CI, 0.018 to 0.039), hip abduction moments (x, 0.031; P < 0.001; 95% CI, 0.023 to 0.038), and hip external rotation moments (x, 0.014; P < 0.001; 95% CI, 0.010 to 0.018). ‡Significant difference between sled and vest tasks: knee extension moments (x, 0.015; P = 0.025; 95% CI, 0.002 to 0.028), hip extension moments (x, −0.023; P = 0.046; 95% CI, −0.046 to 0.000), and hip abduction moments (x, 0.039; P < 0.001; 95% CI, 0.030 to 0.048).
Figure 5.
Knee and hip kinematics illustrate task differences for men, with data collapsed for limb. †Significant difference between walk and sled tasks: peak hip flexion (mean difference [x], –29.135; P < 0.001; 95% CI, −34.617 to −23.653), hip adduction (x, −3.971; P < 0.001; 95% CI, −5.172 to −2.771), hip internal rotation (x, −2.462; P = 0.027; 95% CI, −4.602 to −0.321), and knee flexion (x, 16.173; P < 0.001; 95% CI, 13.139 to 19.208) angles. §Significant difference between walk and vest tasks: peak hip flexion (x, −3.769; P = 0.001; 95% CI, −5.657 to −1.880), hip adduction (x, −0.576; P = 0.006; 95% CI, −0.954 to −0.198), and knee flexion (x, 3.067; P = 0.002; 95% CI, 1.394 to 4.739) angles. ‡Significant difference between sled and vest tasks: peak hip flexion (x, 25.367; P < 0.001; 95% CI, 20.407 to 30.326), hip adduction (x, 3.395; P < 0.001; 95% CI, 2.098 to 4.692), and knee flexion (x, −13.106; P < 0.001; 95% CI, −16.797 to −9.416) angles.
Figure 6.
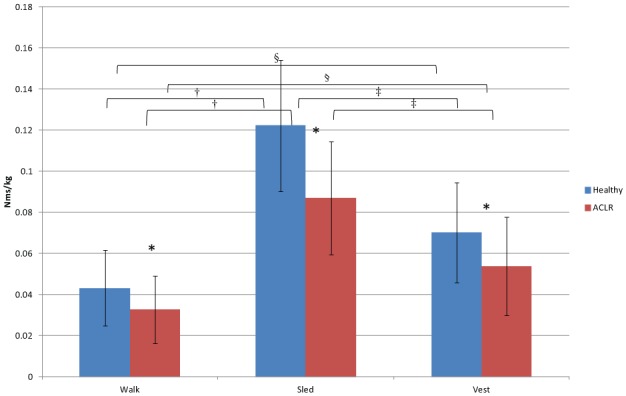
Knee kinetics illustrate limb and task differences for women. *Significant differences between the anterior cruciate ligament reconstruction (ACLR) and healthy limbs for walk (mean difference [x], −0.011; P = 0.001; 95% CI, −0.017 to −0.005), sled (x, −0.035; P < 0.001; 95% CI, −0.047 to −0.023), and vest (x, −0.016; P = 0.002; 95% CI, −0.026 to −0.007) tasks. †Significant difference between walk and sled tasks: ACLR limb (x, −0.054; P < 0.001; 95% CI, −0.063 to −0.045) and healthy limb (x, −0.079; P < 0.001; 95% CI, −0.090 to −0.068). §Significant difference between walk and vest tasks: ACLR limb (x, −0.021; P < 0.001; 95% CI, −0.028 to −0.014) and healthy limb (x, −0.027; P < 0.001; 95% CI, −0.036 to −0.018). ‡Significant difference between sled and vest tasks: ACLR limb (x, 0.033; P < 0.001; 95% CI, 0.023 to 0.044) and healthy limb (x, 0.052; P < 0.001; 95% CI, 0.042 to 0.062).
Women
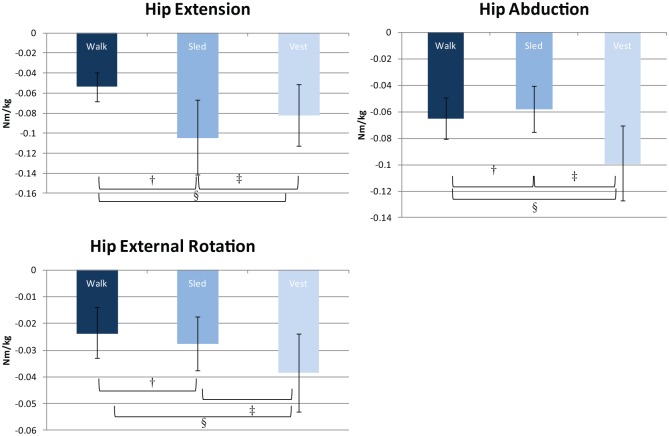
There was a limb by task interaction for KEM impulses, with ACLR < healthy for all tasks and walk < vest < sled for both limbs (Figure 6). There was also a limb by task interaction for peak KFA: ACLR < healthy for sled, ACLR = healthy for walk and vest, and walk < vest < sled for each limb (Figure 7). The HEM, HABDM, HERM, HFA, and HADDA significantly differed among tasks. Post hoc tests for joint moments indicated: HEM (walk < vest < sled), HABDM (sled < walk < vest), and HERM (walk < sled < vest) (Figure 8). Post hoc tests for peak angles indicated: HFA (walk = vest < sled) and HADDA (walk < vest < sled) (Figure 9). The HEM and peak HIRA for the ACLR limb were significantly greater than the healthy limb (Figure 10).
Figure 7.
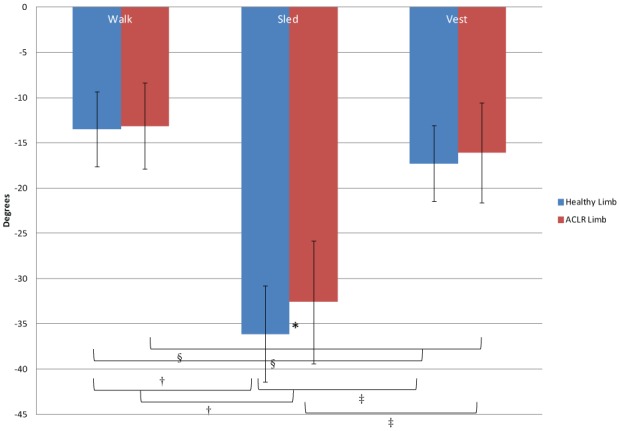
Knee kinematics illustrate limb and task differences for women. *Significant differences between the anterior cruciate ligament reconstruction (ACLR) and healthy limbs for the sled task (mean difference [x], 3.55; P = 0.001; 95% CI, 1.59 to 5.51). †Significant differences between walk and sled tasks: ACLR limb (x, 19.43; P < 0.001; 95% CI, 16.73 to 22.13) and healthy limb (x, 22.64; P < 0.001; 95% CI, 20.49 to 24.78). §Significant difference between walk and vest tasks: ACLR limb (x, 2.96; P < 0.001; 95% CI, 1.98 to 3.93) and healthy limb (x, 3.78; P < 0.001; 95% CI, 2.81 to 4.74). ‡Significant difference between sled and vest tasks: ACLR limb (x, −16.47; P < 0.001; 95% CI, −19.23 to −13.71) and healthy limb (x, −18.86; P < 0.001; 95% CI, −20.94 to −16.78).
Figure 8.
Hip kinetics illustrate limb and task differences for women, with data collapsed for limb. †Significant moment impulse difference between walk and sled tasks: hip extension moments (mean difference [x], 0.050; P < 0.001; 95% CI, 0.037 to 0.063), hip abduction moments (x, −0.007; P = 0.002; 95% CI, −0.011 to −0.003), and hip external rotation moments (x, 0.004; P = 0.033; 95% CI, 0.000 to 0.007). §Significant difference between walk and vest tasks: hip extension moments (x, 0.028; P < 0.001; 95% CI, 0.018 to 0.038), hip abduction moments (x, 0.034; P < 0.001; 95% CI, 0.026 to 0.041), and hip external rotation moments (x, 0.015; P < 0.001; 95% CI, 0.011 to 0.019). ‡Significant difference between sled and vest tasks: hip extension moments (x, −0.022; P = 0.001; 95% CI, −0.034 to −0.011), hip abduction moments (x, 0.041; P < 0.001; 95% CI, 0.033 to 0.049), and hip external rotation moments (x, 0.011; P < 0.001; 95% CI, 0.006 to 0.016).
Figure 9.
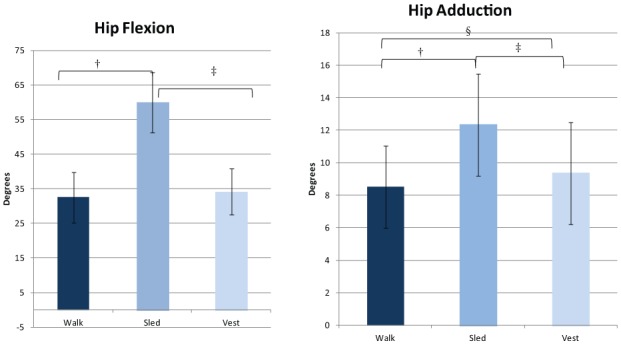
Hip kinematics illustrate limb and task differences for women, with data collapsed for limb. †Significant difference between walk and sled tasks: peak hip flexion (mean difference [x], −27.454; P < 0.001; 95% CI, −30.501 to −24.406.) and hip adduction (x, −3.815; P < 0.001; 95% CI, −4.326 to −3.303) angles. §Significant difference between walk and vest tasks: peak hip adduction angles (x, −0.844; P < 0.001; 95% CI, −1.259 to −0.430). ‡Significant difference between sled and vest tasks: peak hip flexion (x, 25.762; P < 0.001; 95% CI, 22.368 to 29.157) and hip adduction (x, 2.970; P < 0.001; 95% CI, 2.324 to 3.617) angles.
Figure 10.
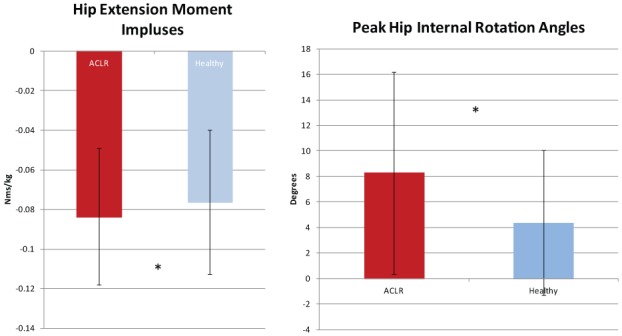
Hip kinetics and kinematics illustrate limb differences for women, with data collapsed for tasks. *Significant differences between the anterior cruciate ligament reconstruction (ACLR) and healthy limbs for hip extension moment impulse (mean difference [x], –0.007; P = 0.037; 95% CI, –0.014 to 0.000) and peak hip internal rotation angles (x, 3.904; P = 0.005; 95% CI, 1.330 to 6.478).
Discussion
The biomechanical profiles related to a “stiff knee gait” and dynamic lower extremity valgus in men and women who were cleared to RTS after ACLR were identified. The hypothesis that weighted gait tasks would increase joint moments (eg, KEM, HEM, HABDM, and HERM) and joint angles (KFA and HFA) was met with the exception of HABDM sled = walk for men and HABDM sled < walk and HFA walk = vest for women. The hypothesis that weighted gait would not create unwanted biomechanics (eg, increase peak HIRA, HADDA, limb asymmetries) was not met. For men, HADDA and HIRA (sled only) significantly increased during weighted gait. For women, HADDA significantly increased for both tasks, and the sled task created significantly lower KFA in the ACLR limb. The acute changes in biomechanics during weighted gait tasks should be considered when determining whether to use either task with individuals after ACLR.
Similar to healthy individuals, those recovering from ACLR increased KEM and HEM during weighted gait tasks as compared with unweighted gait.15,22 Our findings of reduced KEM in the ACLR limb are consistent with compensatory gait patterns present after ACL rupture,4,6,13,20 ACLR,3-5 physical therapy,19 and several years after ACLR.19 Reduced KEM in the ACLR limb is found across multiple functional tasks such as step ups, running, and drop jump landing, implicating the robustness of this biomechanical profile in the ACLR limb.14,16,18,21,23
Men
The ability of the weighted tasks to increase sagittal plane moments and angles (eg, KEM, HEM, HFA, and KFA) suggests that these tasks may effectively mitigate the “stiff knee gait.” Our results, however, indicate that during the weighted tasks, reduced KFA and KEM persisted in the ACLR limb. Thus, increased loads may feed into this aberrant asymmetrical pattern. Additionally, peak HIRA and HADDA increased compared with normal gait, resulting in a greater dynamic limb valgus position during the loading aspect of the stance phase of gait, which is unwanted after ACLR.8,11 Finally, limb asymmetry for peak KFA during the sled task crossed the clinically meaningful 3° difference reported during gait,6 cautioning the clinician in prescription of sled pulls for men after ACLR.
The HADDA during the vest were significantly greater than the walk task. This difference, however, was clinically meaningless (approximately 1° difference). Peak HIRA symmetry also decreased from a 3° difference when walking normally to less than a 2° difference during the vest task. Our results imply that the vest may have potential to protect against a dynamic limb valgus position.11,18
Women
Given that the sled task introduced KFA asymmetries, the greatest peak HADDA, and the smallest HABDM, we do not recommended sled towing for women after ACLR. Increased KEM, HEM, HABDM, and HERM indicate that weighted vest training may have clinical utility for women after ACLR. The vest task also significantly increased peak HADDA, but the unwanted increase was less than 1°. However, asymmetries such as reduced KEM, increased HEM, and increased peak HIRA in the ACLR limb suggest that the hip is compensating for the knee in the ACLR limb in all tasks.
Di Stasi et al5 reported asymmetrical HEM during gait in individuals who RTS 6 months after ACLR. Those who demonstrated asymmetrical HEM in conjunction with asymmetrical KEM failed RTS criteria, whereas those who used symmetrical HEM and asymmetrical KEM were able to pass RTS criteria.5 Thus, women with asymmetrical HEM and reduced KEM during gait appear to be more likely to have decreased functional outcomes.5 Our findings of increased HIRA demonstrated in the ACLR limb by women warrants concern as this position appears to stress the ACL.12 Therefore, interventions that address deleterious knee (our men and women) and hip biomechanics (our women only) when cleared to RTS after ACLR are certainly needed.
Limitations
Our study design was meant to test the acute effects of weighted gait on biomechanics to explore the potential of weighted gait paradigms as an intervention after ACLR. Whether the acute biomechanical changes seen during weighted gait tasks produce lasting effects or transfer over to normal gait or other tasks cannot be answered from this investigation. We did not perform a sample size estimation, and our small sample size may limit the ability to detect true differences. We also chose not to use strict inclusion criteria such as type of reconstructive surgery or physical therapy to increase the generalizability of our findings. The wide range of ages and postoperative inclusion criteria were based on larger clinical trials of individuals who intend to RTS after ACLR.10 Skin markers create errors when estimating underlying bone kinematics during gait because of soft tissue artifact created by muscle activity and inertia.2 Whether the weighted tasks increase the inaccuracies associated with using skin markers to measure kinematics is unknown.
Conclusion
Walking with a weighted vest or sled has the ability to increase KEM in the ACLR limb when individuals were discharged from physical therapy and cleared to RTS. Unfortunately, men continue to use asymmetrical knee moments and angles whereas women continue to use asymmetrical knee moments and hip biomechanics after ACLR. Persistent asymmetries and unwanted responses were demonstrated when towing a sled, and therefore, this training apparatus appears to be inappropriate for individuals after ACLR. Our findings of asymmetrical KEM in men and women who were cleared to RTS across weighted gait tasks highlight the need for movement retraining.
Supplementary Material
Acknowledgments
This study would not have been possible without University of New England’s (UNE’s) Patient Population Oriented Research Grant. We acknowledge and appreciate the pilot work and efforts of UNE’s former Doctorate of Physical Therapy students: Samantha Ellis, Stephen Marcil, Allyson Harvey Marcil, Claudia Burns, and Tara Randhawa. We also appreciate the editing expertise of Bethanny Araujo, DPT.
Footnotes
The following author(s) declared potential conflicts of interest: Thomas Murray, MD, Bernadette Shaw, PA-C, Erin Collins, PT, DPT, and James Townsend, PT, DPT, were supported by a grant from PPOR.
References
- 1. Arendt EA, Agel J, Dick R. Anterior cruciate ligament injury patterns among collegiate men and women. J Athl Train. 1999;34:86-92. [PMC free article] [PubMed] [Google Scholar]
- 2. Benoit DL, Ramsey DK, Lamontagne M, Xu L, Wretenberg P, Renstrom P. Effect of skin movement artifact on knee kinematics during gait and cutting motions measured in vivo. Gait Posture. 2006;24:152-164. [DOI] [PubMed] [Google Scholar]
- 3. DeVita P, Hortobagyi T, Barrier J. Gait biomechanics are not normal after anterior cruciate ligament reconstruction and accelerated rehabilitation. Med Sci Sports Exerc. 1998;30:1481-1488. [DOI] [PubMed] [Google Scholar]
- 4. Di Stasi S, Hartigan EH, Snyder-Mackler L. Sex-specific gait adaptations prior to and up to 6 months after anterior cruciate ligament reconstruction. J Orthop Sports Phys Ther. 2015;45:207-214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Di Stasi SL, Logerstedt D, Gardinier ES, Snyder-Mackler L. Gait patterns differ between ACL-reconstructed athletes who pass return-to-sport criteria and those who fail. Am J Sports Med. 2013;41:1310-1318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Di Stasi SL, Snyder-Mackler L. The effects of neuromuscular training on the gait patterns of ACL-deficient men and women. Clin Biomech (Bristol, Avon). 2012;27:360-365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Gardinier ES, Di Stasi S, Manal K, Buchanan TS, Snyder-Mackler L. Knee contact force asymmetries in patients who failed return-to-sport readiness criteria 6 months after anterior cruciate ligament reconstruction. Am J Sports Med. 2014;42:2917-2925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Griffin LY, Agel J, Albohm MJ, et al. Noncontact anterior cruciate ligament injuries: risk factors and prevention strategies. J Am Acad Orthop Surg. 2000;8:141-150. [DOI] [PubMed] [Google Scholar]
- 9. Griffin LY, Albohm MJ, Arendt EA, et al. Understanding and preventing noncontact anterior cruciate ligament injuries: a review of the Hunt Valley II meeting, January 2005. Am J Sports Med. 2006;34:1512-1532. [DOI] [PubMed] [Google Scholar]
- 10. Hartigan EH, Axe MJ, Snyder-Mackler L. Time line for noncopers to pass return-to-sports criteria after anterior cruciate ligament reconstruction. J Orthop Sports Phys Ther. 2010;40:141-154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Hewett TE, Ford KR, Myer GD. Anterior cruciate ligament injuries in female athletes: part 2, a meta-analysis of neuromuscular interventions aimed at injury prevention. Am J Sports Med. 2006;34:490-498. [DOI] [PubMed] [Google Scholar]
- 12. Hewett TE, Myer GD, Ford KR. Anterior cruciate ligament injuries in female athletes: part 1, mechanisms and risk factors. Am J Sports Med. 2006;34:299-311. [DOI] [PubMed] [Google Scholar]
- 13. Hurd WJ, Snyder-Mackler L. Knee instability after acute ACL rupture affects movement patterns during the mid-stance phase of gait. J Orthop Res. 2007;25:1369-1377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Ithurburn MP, Paterno MV, Ford KR, Hewett TE, Schmitt LC. Young athletes with quadriceps femoris strength asymmetry at return to sport after anterior cruciate ligament reconstruction demonstrate asymmetric single-leg drop-landing mechanics. Am J Sports Med. 2015;43:2727-2737. [DOI] [PubMed] [Google Scholar]
- 15. Lawrence M, Hartigan E, Tu C. Lower limb moments differ when towing a weighted sled with different attachment points. Sports Biomech. 2013;12: 186-194. [DOI] [PubMed] [Google Scholar]
- 16. Lewek M, Rudolph K, Axe M, Snyder-Mackler L. The effect of insufficient quadriceps strength on gait after anterior cruciate ligament reconstruction. Clin Biomech (Bristol, Avon). 2002;17:56-63. [DOI] [PubMed] [Google Scholar]
- 17. Lohmander LS, Ostenberg A, Englund M, Roos H. High prevalence of knee osteoarthritis, pain, and functional limitations in female soccer players twelve years after anterior cruciate ligament injury. Arthritis Rheum. 2004;50:3145-3152. [DOI] [PubMed] [Google Scholar]
- 18. Paterno MV, Schmitt LC, Ford KR, et al. Biomechanical measures during landing and postural stability predict second anterior cruciate ligament injury after anterior cruciate ligament reconstruction and return to sport. Am J Sports Med. 2010;38:1968-1978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Roewer BD, Di Stasi SL, Snyder-Mackler L. Quadriceps strength and weight acceptance strategies continue to improve two years after anterior cruciate ligament reconstruction. J Biomech. 2011;44:1948-1953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Rudolph KS, Axe MJ, Buchanan TS, Scholz JP, Snyder-Mackler L. Dynamic stability in the anterior cruciate ligament deficient knee. Knee Surg Sports Traumatol Arthrosc. 2001;9:62-71. [DOI] [PubMed] [Google Scholar]
- 21. Schmitt LC, Paterno MV, Ford KR, Myer GD, Hewett TE. Strength asymmetry and landing mechanics at return to sport after anterior cruciate ligament reconstruction. Med Sci Sports Exerc. 2015;47:1426-1434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Seay JF, Fellin RE, Sauer SG, Frykman PN, Bensel CK. Lower extremity biomechanical changes associated with symmetrical torso loading during simulated marching. Mil Med. 2014;179:85-91. [DOI] [PubMed] [Google Scholar]
- 23. von Porat A, Henriksson M, Holmstrom E, Thorstensson CA, Mattsson L, Roos EM. Knee kinematics and kinetics during gait, step and hop in males with a 16 years old ACL injury compared with matched controls. Knee Surg Sports Traumatol Arthrosc. 2006;14:546-554. [DOI] [PubMed] [Google Scholar]
- 24. von Porat A, Roos EM, Roos H. High prevalence of osteoarthritis 14 years after an anterior cruciate ligament tear in male soccer players: a study of radiographic and patient relevant outcomes. Ann Rheum Dis. 2004;63:269-273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Winter DA. Biomechanics and Motor Control of Human Movement. 3rd ed. Hoboken, NJ: Wiley; 2005. [Google Scholar]
- 26. Winter DA. Overall principle of lower limb support during stance phase of gait. J Biomechanics. 1980;13:923-927. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.