Abstract
Context:
Musculoskeletal ultrasound (US) research is expanding due to increased clinical utility of sonography.
Study Design:
Clinical review.
Level of Evidence:
Level 4.
Results:
Ultrasound is widely applied in musculoskeletal imaging and sports medicine. The real-time capabilities and favorable cost profile of US make it ideal for use in diagnosis of musculoskeletal conditions. The enthusiasm for the use of US in musculoskeletal imaging has led to an increase in US research to broaden its applications.
Conclusion:
Several recent advances have been made in conventional and novel US imaging techniques, quantitative US imaging, and US-guided interventions.
Strength of Recommendations Taxonomy (SORT):
C
Keywords: musculoskeletal ultrasound, research, contrast-enhanced ultrasound, elastography, ultrasound-guided interventions
Ultrasound (US) imaging in musculoskeletal (MSK) health is quite widespread, benefiting clinicians in the care of their patients. Improved US imaging quality has allowed for its expanded use in diagnosis of MSK conditions. As MSK US is used more in clinical practice, there has been increased desire to further innovate its use.
Conventional Diagnostic us Imaging
Combining the benefits of high-resolution imaging, portability, and cost-effectiveness, US is gaining popularity in the evaluation of ligaments, tendons, and nerves in the extremities.6,50 Sonography remains limited in the evaluation of MSK pathology in the axial skeleton, especially deep in the abdomen or pelvis. Additionally, the evaluation for diffuse pathology can be cumbersome using US. In general, the more focused the clinical question (ie, tendon tear, peripheral neuropathy, ligament disruption), the more beneficial MSK US is in clinical practice.
Arthropathy
Features of arthropathy such as synovitis (Figure 1), proliferative bone formation, osseous erosion, bursitis, and tendinopathy can be readily detected using US.39,48 Much of the MSK US literature involves the use of sonography in the clinical evaluation of rheumatoid arthritis, and several studies have validated sonography in the evaluation of joint synovitis7,24 and tenosynovitis.9,85,104 More recently, studies have shown that US markers can be used to assess disease response to treatment with methotrexate and biologic therapy.20,49
Figure 1.
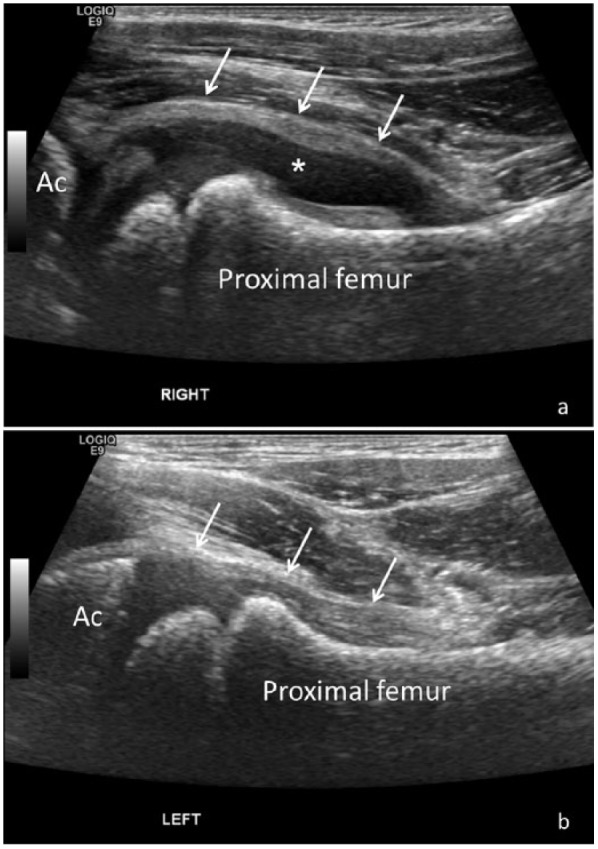
Sonographic evaluation of the hips in a pediatric patient with right hip pain and clinical suspicion for juvenile inflammatory arthritis. (a) Longitudinal ultrasound (US) image of the right hip reveals distension of the joint capsule (white arrows) by a large joint effusion (*), in keeping with synovitis. (b) Comparative longitudinal US of the left hip demonstrates a normal hip joint with a decompressed joint capsule (arrows). Ac, acetabulum.
Neurosonology
Nerves have a characteristic appearance on US, and, with knowledge of anatomy, peripheral nerves can be sonographically traced and evaluated for pathology.8,109 Several studies have demonstrated high sensitivity of US for the diagnosis of nerve pathology (Figure 2), with good correlation to magnetic resonance imaging (MRI) and electromyography (EMG).102,111 Sonography is now commonly incorporated in the evaluation of carpal tunnel syndrome,46,71,98 and there are well-described techniques for the US evaluation of peripheral nerve entrapment disorders including cubital tunnel syndrome, meralgia paraesthetica, peroneal neuropathy, and tarsal tunnel syndrome.71,78,86 US is even useful in the evaluation of posttraumatic brachial plexopathy, where it can be used in the diagnosis of nerve root avulsion, pseudomeningocele, and traction neuroma (Figure 3).14,43 There remain limitations to neurosonology, particularly in the study of deep neural structures. US for the evaluation of nerves is operator dependent, and there can be a steep learning curve. Nonetheless, neurosonology is a promising field with ongoing prospective studies hoping to further evaluate its efficacy.
Figure 2.
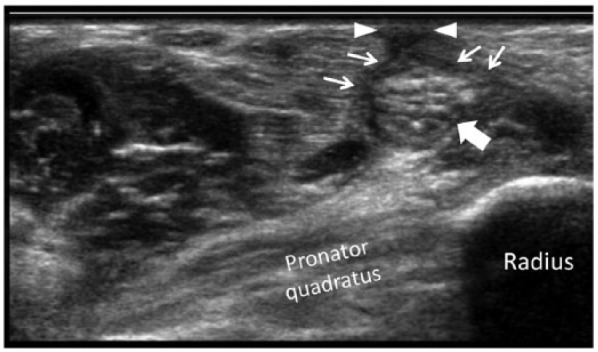
Sonographic evaluation of the median nerve in a patient with hand numbness and prior plate fixation of the distal radius. Transverse ultrasound image at the distal forearm reveals hypoechoic scar tissue extending from the skin (arrowheads) to the volar surface of the median nerve (arrows), in keeping with scar tethering. The median nerve (block arrow) in this region is abnormally enlarged and has prominent internal fascicles, consistent with neuritis.
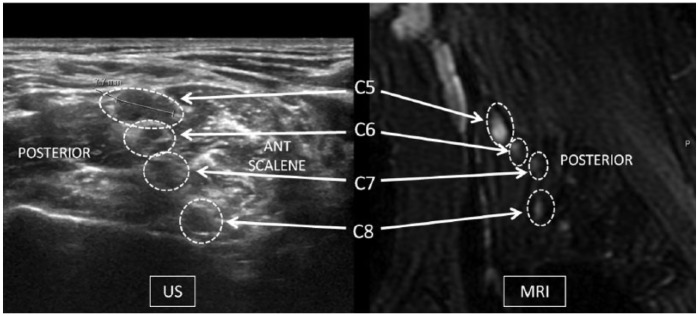
Figure 3.
Ultrasound (US) and magnetic resonance image (MRI) of the right brachial plexus roots in a patient with upper extremity weakness after a motor vehicle accident. The US image at the interscalene triangle shows marked enlargement of the right C5 nerve root at the interscalene triangle, suspicious for a traction injury. The corresponding sagittal MRI of the right brachial plexus in the same patient shows abnormal enlargement and high signal of the C5 nerve root, confirming injury. ANT SCALENE, anterior scalene muscle.
Muscle and Tendon Imaging
Grayscale US can be useful in the clinical evaluation of posttraumatic muscle conditions such as myofascial tear and intramuscular hematoma. US can also detect fatty atrophy and fibrosis of muscle. There are differences in the sonographic appearance of muscle abnormality related to myopathy versus that seen with neuropathy (Figure 4).73 Sonography has also been used to evaluate patients with glyocogen storage diseases,103 correlating muscle ultrasound density with muscle weakness. Recently developed software can assess depletion of glycogen stores in high-level athletes using US images.45 However, this technique has not yet been clinically validated. Some studies have reported using high-resolution US cine loops to detect muscle fasciculations,4,79 aiding the diagnosis of neuromuscular disorders such as amyotrophic lateral sclerosis. Although these muscle imaging techniques have not been validated clinically, they do have potential for the evaluation of muscle injury and assessment of muscle health.
Figure 4.
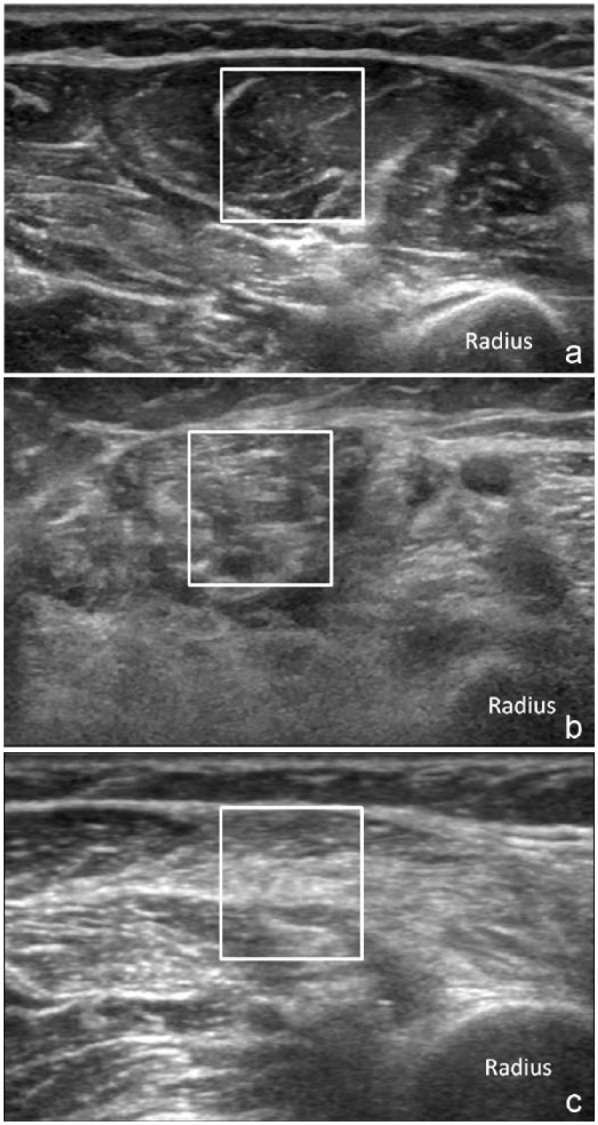
Transverse sonographic images of the forearm. Sampling of muscle images (squares) demonstrates differential muscle echogenicity in (a) a normal patient, (b) a patient with myopathy, and (c) a patient with neuropathy. Note that the superficial cortex of the radius is poorly visualized in the patient with myopathy (b), a characteristic feature.
Grayscale US has long been used in the evaluation of tendinopathy (tendinosis, tenosynovitis [Figure 5], and tendon tear). The real-time imaging capabilities of US also make it ideal to evaluate tendon impingement or abrasion by surgical hardware.40,64 US could also be beneficial for imaging plantaris tendon involvement in mid-Achilles tendinopathy.2 In fact, a new US imaging technique, ultrasound tissue characterization, has shown promise in detection of disorganized tissue at the medial border of the Achilles,72 which may suggest plantaris dysfunction in mid-Achilles tendinopathy.
Figure 5.
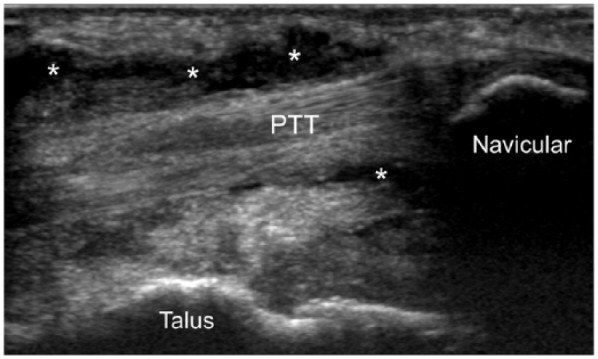
Sonographic assessment of the ankle in a patient with medial-sided pain. Ultrasound image demonstrates a thickened and hypoechoic distal posterior tibial tendon (PTT) surrounded by complex tendon sheath effusion (*), in keeping with tenosynovitis.
Novel Ultrasound Imaging Technology
Fusion Imaging
As US cannot produce the anatomic detail of MRI and computed tomography (CT), there are limitations to its use in image-guided procedures, particularly in those targeting structures located deep in the body where US imaging is poor. Image fusion technology allows the combination of real-time capabilities of US and the anatomic detail afforded by CT or MRI. Using this technology, procedures can be performed in a more cost-effective manner compared with CT or MR guidance.
CT-US and MRI-US fusion imaging have mainly been utilized in biopsy of hepatic lesions. However, there is a place for their use in MSK imaging. The benefits have been seen in image-guided biopsy of bone lesions67 and are also translatable to biopsy of MSK soft tissue masses and evaluation of MSK injury.108 Additionally, the fusion software can be utilized in sacroiliac and facet joint injections.58 This could be particularly beneficial in young patients with inflammatory arthropathy, with the software eliminating the repeated use of ionizing radiation. Larger, more robust clinical studies are needed to determine the efficacy of these techniques compared with conventional methods.
Contrast-Enhanced Sonography and Superb Microvascular Imaging
Doppler sonography can be used to evaluate tissue vascularity and detect inflammatory conditions. However, Doppler can only demonstrate limited sensitivity in the evaluation of slow blood flow.34,101 Contrast-enhanced ultrasound (CEUS) increases the ability of sonography to evaluate tissue perfusion. During CEUS, a contrast agent consisting of microbubbles is injected intravenously, and the body part in question is imaged using sonography. After injection, perfusion can be monitored by obtaining sequential US frames to evaluate the pattern of blood flow.19,107 It is most commonly used in liver and cardiac imaging, but CEUS has been studied in MSK imaging.
Angiogenesis is one of the earliest physiologic manifestations in inflammatory arthritis. Although contrast-enhanced MRI strongly correlates with the density of synovial blood vessels, its use in the evaluation of rheumatoid arthritis and other inflammatory arthritides is limited by cost and availability. As such, CEUS evaluation of hyperemia can evaluate inflammatory arthritides in diagnosis, evaluation of disease progression, and assessment of response to therapy. CEUS is more sensitive than grayscale and power Doppler US in the posttreatment monitoring of patients with rheumatoid arthritis.88 CEUS could better differentiate between active synovitis and inactive synovial thickening when compared with grayscale US and power Doppler.55 Nonrheumatologic studies have used CEUS to characterize the perfusion pattern of soft tissue masses21,65,66 and the vascularity of repaired rotator cuff tendons.1,11,37
Although this technique is promising, there remain several technical limitations to CEUS that preclude its widespread use in clinical practice.107 If the timing of the postinjection imaging is not optimized, the contrast bolus may be missed. Also, since an intravenous injection is required, this sonographic examination is no longer noninvasive, and patients need to be monitored after the procedure for adverse events from the contrast injection. Finally, although widely used in Europe and Asia, contrast agents for sonography only recently were approved for use in the United States, but only for echocardiography and liver imaging. To overcome the limited sensitivity of Doppler imaging and the need for contrast-enhanced US, superb microvascular imaging (SMI) was developed. This prototype technique depicts microvascular flow in soft tissues and is superior to Doppler US when evaluating breast masses and thyroid and testicular tissue.54,68,69 There is potential for application of this technology in MSK pathology and tissue healing. However, no published studies have used SMI to evaluate MSK conditions.
Quantitative Ultrasound Imaging
Quantitative imaging implies extracting quantifiable features from medical images for the assessment of disease or injury. Elastography, a quantitative US technique, evaluates the stiffness property of a tissue. When stress is applied to a tissue, it deforms. The degree of the deformation corresponds to its stiffness. Tissues that are more stiff deform less when stress is applied, and softer tissues will deform more. In MSK imaging, elastography has largely been used in the evaluation of tendon and muscle pathology.27,56 In general, pathologic tendons appear less stiff on elastography when compared with normal tendons. This convention does not necessarily hold true in muscle, and increased muscle stiffness may signify pathology. The 2 main types of elastograpy used in MSK imaging are strain elastography and shear wave elastography (SWE).27,56
Strain Elastography
Strain elastography measures the relative strain of 1 region compared with another using the same stress. The stress applied is usually freehand transducer compression. The output obtained is a relative strain map, commonly color coded. Measurements in strain elastography are qualitative, although semiquantitative measures can be obtained using strain ratios. Most of the literature on strain elastography in MSK imaging focuses on tendon evaluation, particularly the Achilles tendon. Strain elastography for MSK applications is repeatable,26,27 and studies show good correlation between strain elastography and histologic evaluation of tendinosis57 as well as clinical markers of tendon pain and dysfunction.22,89,90,97,100 There was improved diagnostic accuracy of carpal tunnel syndrome when grayscale US findings were used in conjunction with sonoelastography.80 In addition, spastic muscles have been characterized as abnormally stiff using strain elestography in spasticity disorders.61 The limitations of strain elastography lie in the fact that the measurements are not truly quantitative, and as such, are subjective. Additionally, many of the findings reported with strain elastography in MSK are also seen in morphologic or grayscale US imaging, limiting its clinical efficacy.
Shear Wave Elastography
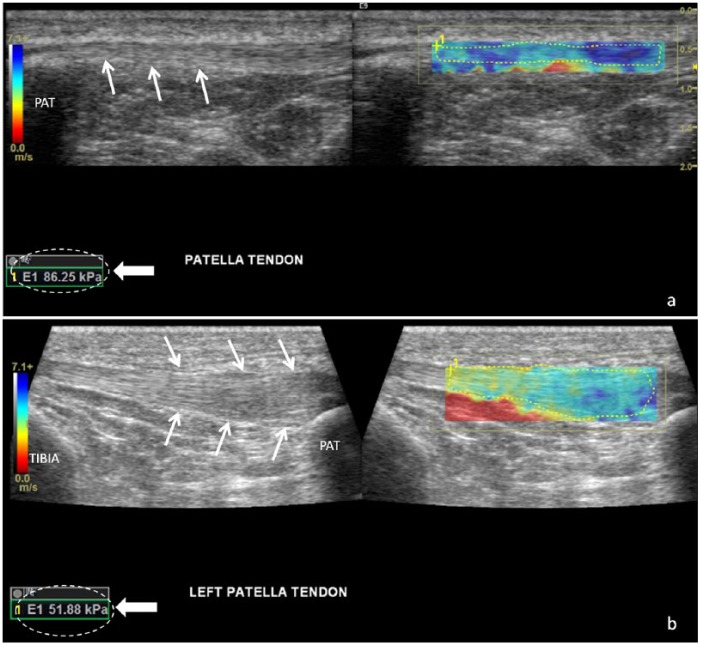
SWE measures the velocity of propagation of an automated pulse through tissue. The faster the shear wave velocity, the stiffer the tissue. Shear wave velocity (V), measured in meters per second (m/s), is related to elasticity via the Young modulus equation, where elasticity (E) = 3 × V2. SWE is well established in the evaluation of the liver, breast, and thyroid gland.5 Its use for MSK applications is relatively recent. However, there are several studies confirming repeatability of SWE in the assessment of tendons, ligaments, and muscle.59,70,92,110 There is a positive correlation between SWE tendon measurement and morphologic changes on grayscale US (Figure 6).15,27 Additionally, there has been correlation between patella tendon elasticity values and validated clinical scores for patellar tendinopathy.89 There is also a decrease in shear wave elasticity of muscle after intramuscular botulinum toxin injection in spastic cerebral palsy.60 The strength of SWE lies in the potential ability to detect tissue changes not visible on regular grayscale US imaging. However, SWE measurements are influenced by changes in transducer pressure and patient positioning, potentially contributing to output variability.59,83
Figure 6.
Shear wave elastography (SWE) of the patellar tendon. (a) The grayscale ultrasound image shows a normal patellar tendon (arrows). The corresponding SWE color map demonstrates expected predominantly dark blue signal in the tendon, with corresponding high elasticity measurement indicating a normal tendon. (b) Grayscale image shows abnormal thickening of the patellar tendon (arrows) toward the proximal (patellar) attachment, in keeping with tendinosis. The SWE map demonstrates heterogeneous yellow and light blue signal in the patellar tendon, and the elasticity measurement is decreased compared with that of the normal tendon. PAT, patella.
Ultrasound-Guided Interventions
US is an ideal modality for image-guided MSK interventions, as it increases the accuracy and efficacy of MSK interventions.12,28,42,84,93,105 Techniques particularly pertinent to sports medicine include tendon fenestration/prolotherapy for the treatment of tendinopathy, injection of muscle tears, and perineural interventions, including hydrodissection.
Tendinopathy Interventions
Peritendinous corticosteroid injection is an effective treatment for tendinopathy, but its effects can be short-lived.18,62,112 Consequently, tendon fenestration, or dry needling, has come into favor as a treatment for tendinopathy. By iatrogenically disrupting degenerated tendon fibers using multiple needle passes (Figure 7), the resultant inflammation and growth factors recruited by the injury may help heal the tendon.16 Several studies have demonstrated efficacy of tendon fenestration in the treatment of tendinosis.47,51,76,77
Figure 7.
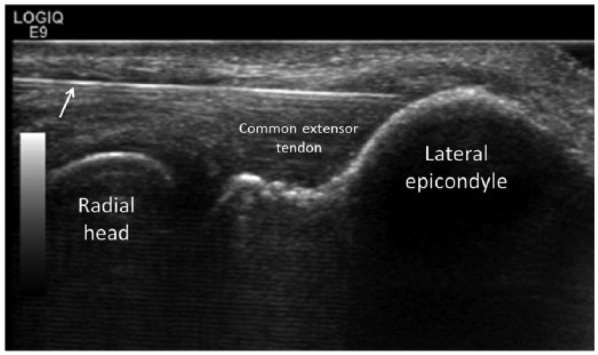
Ultrasound (US)-guided common extensor tendon fenestration in a patient with lateral epicondylitis. US image at the lateral elbow demonstrates a 25-gauge needle (arrow) within a thickened common extensor tendon for fenestration.
Dry needling means that no additives are injected in conjunction with the tendon fenestration procedure. Prolotherapy is the injection of dextrose or other sclerosing agents to further stimulate inflammation in the tendon after needle fenestration.23,75 A number of studies have demonstrated clinical and imaging improvement in tendinopathy after prolotheraphy, particularly in the Achilles and patellar tendons.75,95,96 Multiple treatments may be required to achieve a satisfactory outcome, and long-term outcomes have not been reported.
The injection of platelet-rich plasma (PRP) to promote tissue healing has been recently embraced by the sports medicine community as a treatment for tendinopathy,29,35 with numerous studies, including randomized controlled trials, demonstrating efficacy in a variety of tendinopathies.25,32,63,74,106 A recent meta-analysis of randomized controlled clinical trials suggests there is good evidence to support single US-guided PRP injection for the treatment of tendinopathy, recommending leucocyte-rich PRP formulations in particular.33
Muscle Interventions
High-quality studies evaluating PRP for muscle injury are currently limited.81 One randomized controlled study including athletes did not show improved time to return to play with single PRP injection for hamstring injury,44 but the injections were not performed under image guidance. Another study, which did use US-guided injection, reported no added benefit in sports-related hamstring injury.41 Other studies evaluating US-guided PRP injection in acute muscle tear have demonstrated decreased time to return to sports and higher level of pain relief in athletes,10,94 but these were not controlled clinical trials. The true efficacy of PRP for muscle injury is unclear.
Perineural Interventions
US is frequently used for guidance in nerve blocks to improve accuracy.12,105 US guidance may also provide a safer injection as it may avoid critical vascular structures that often accompany nerves and may decrease the risk of intraneural injection.3 Techniques for US-guided injection of commonly symptomatic upper and lower extremity peripheral nerves are well described.86 Perineural corticosteroid injection is most frequently prescribed, and small volumes of injectant have been shown to produce circumferential and long-segment coverage of peripheral nerves when US guidance is used.87 US-guided percutaneous nerve hydrodissection techniques using larger injectant volumes have been proposed as treatment for nerve entrapment syndromes, potentially serving as an alternative to surgical decompression/neurolysis (Figure 8).13 Limited evidence supports the use of US-guided nerve hydrodissection in the treatment of meralgia paraesthetica,82,99 saphenous neuralgia after total knee arthroplasty,17 and sural neuroma.30
Figure 8.
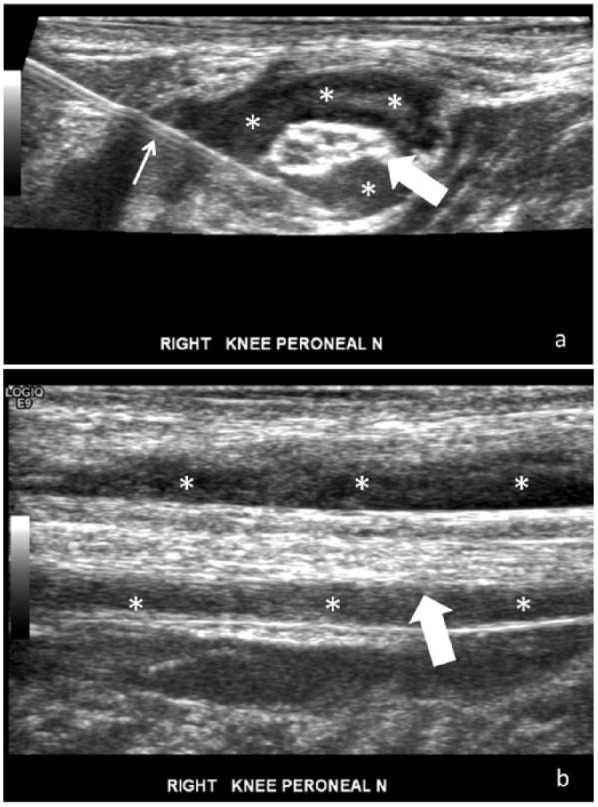
Ultrasound (US)-guided hydrodissection of the common peroneal nerve in a patient with radicular dorsolateral leg and foot weakness. (a) Transverse US image just proximal to the fibular head shows large volume injectant (*) circumferentially dissecting away tissues around the common peroneal nerve (block arrow) during hydrodissection. (b) Longitudinal US image of the common peroneal nerve (block arrow) after hydrodissection demonstrates injectant (*) along the superficial and deep surface of the nerve. Small arrow, 25-gauge needle.
Currently, nerve root injection is most commonly performed using fluoroscopic guidance and contrast injection, relying on bony landmarks and contrast test injection to confirm accurate perineural injection. A few studies have shown similar and sometimes improved efficacy of US-guided cervical spinal nerve root injections compared with conventional techniques,52,91 with the added benefit of not using ionizing radiation. The spread of perineural injectant can vary depending on the volume injected,53 and 1 cadaveric study demonstrated spread of injectant to the phrenic nerve and into the thecal sac after US-guided selective C5 nerve root injection with a 5-mL injectant volume.31 Therefore, US-guided cervical nerve root injection should not be performed without preparation for potential serious complications, including phrenic nerve palsy. Given their deep location in the body, lumbar spine nerve roots are poorly visualized under sonographic guidance, even in very small patients. Small cadaveric studies have described techniques for US-guided lumbar transforaminal injections36,38 but they have yet to be validated by clinical studies.
Conclusion
MSK US has vastly benefited physicians in the diagnosis of MSK conditions. Conventional and novel US imaging techniques, quantitative US imaging, and US-guided interventions continue to show promise. Future investigations should determine the efficacy of these techniques in clinical practice.
Footnotes
The following author declared potential conflicts on interest: O. Kenechi Nwawka, MD, has grants/grants pending from the American Institute of Ultrasound in Medicine and GE Healthcare.
References
- 1. Adler RS, Johnson KM, Fealy S, et al. Contrast-enhanced sonographic characterization of the vascularity of the repaired rotator cuff: utility of maximum intensity projection imaging. J Ultrasound Med. 2011;30:1103-1109. [DOI] [PubMed] [Google Scholar]
- 2. Alfredson H. Midportion Achilles tendinosis and the plantaris tendon. Br J Sports Med. 2011;45:1023-1025. [DOI] [PubMed] [Google Scholar]
- 3. Antonakakis JG, Ting PH, Sites B. Ultrasound-guided regional anesthesia for peripheral nerve blocks: an evidence-based outcome review. Anesthesiol Clin. 2011;29:179-191. [DOI] [PubMed] [Google Scholar]
- 4. Arts IM, Overeem S, Pillen S, et al. Muscle ultrasonography: a diagnostic tool for amyotrophic lateral sclerosis. Clin Neurophysiol. 2012;123:1662-1667. [DOI] [PubMed] [Google Scholar]
- 5. Barr RG. Elastography in clinical practice. Radiol Clin North Am. 2014;52:1145-1162. [DOI] [PubMed] [Google Scholar]
- 6. Beggs I. Musculoskeletal Ultrasound. 1st ed Philadelphia, PA: Lippincott Williams & Wilkins; 2014. [Google Scholar]
- 7. Boesen M, Ellegaard K, Boesen L, et al. Ultrasound Doppler score correlates with OMERACT RAMRIS bone marrow oedema and synovitis score in the wrist joint of patients with rheumatoid arthritis. Ultraschall Med. 2012;33:E166-E172. [DOI] [PubMed] [Google Scholar]
- 8. Brown JM, Yablon CM, Morag Y, Brandon CJ, Jacobson JA. US of the peripheral nerves of the upper extremity: a landmark approach. Radiographics. 2016;36:452-463. [DOI] [PubMed] [Google Scholar]
- 9. Bruyn GA, Hanova P, Iagnocco A, et al. Ultrasound definition of tendon damage in patients with rheumatoid arthritis. Results of a OMERACT consensus-based ultrasound score focussing on the diagnostic reliability. Ann Rheum Dis. 2014;73:1929-1934. [DOI] [PubMed] [Google Scholar]
- 10. Bubnov R, Yevseenko V, Semeniv I. Ultrasound guided injections of platelets rich plasma for muscle injury in professional athletes. Comparative study. Med Ultrason. 2013;15:101-105. [DOI] [PubMed] [Google Scholar]
- 11. Cadet ER, Adler RS, Gallo RA, et al. Contrast-enhanced ultrasound characterization of the vascularity of the repaired rotator cuff tendon: short-term and intermediate-term follow-up. J Shoulder Elbow Surg. 2012;21:597-603. [DOI] [PubMed] [Google Scholar]
- 12. Casati A, Danelli G, Baciarello M, et al. A prospective, randomized comparison between ultrasound and nerve stimulation guidance for multiple injection axillary brachial plexus block. Anesthesiology. 2007;106:992-996. [DOI] [PubMed] [Google Scholar]
- 13. Cass SP. Ultrasound-guided nerve hydrodissection: what is it? A review of the literature. Curr Sports Med Rep. 2016;15:20-22. [DOI] [PubMed] [Google Scholar]
- 14. Chen DZ, Cong R, Zheng MJ, et al. Differential diagnosis between pre- and postganglionic adult traumatic brachial plexus lesions by ultrasonography. Ultrasound Med Biol. 2011;37:1196-1203. [DOI] [PubMed] [Google Scholar]
- 15. Chen XM, Cui LG, He P, Shen WW, Qian YJ, Wang JR. Shear wave elastographic characterization of normal and torn Achilles tendons: a pilot study. J Ultrasound Med. 2013;32:449-455. [DOI] [PubMed] [Google Scholar]
- 16. Chiavaras MM, Jacobson JA. Ultrasound-guided tendon fenestration. Semin Musculoskelet Radiol. 2013;17:85-90. [DOI] [PubMed] [Google Scholar]
- 17. Clendenen S, Greengrass R, Whalen J, O’Connor MI. Infrapatellar saphenous neuralgia after TKA can be improved with ultrasound-guided local treatments. Clin Orthop Relat Res. 2015;473:119-125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Coombes BK, Bisset L, Vicenzino B. Efficacy and safety of corticosteroid injections and other injections for management of tendinopathy: a systematic review of randomised controlled trials. Lancet. 2010;376:1751-1767. [DOI] [PubMed] [Google Scholar]
- 19. Cosgrove D. Ultrasound contrast agents: an overview. Eur J Radiol. 2006;60:324-330. [DOI] [PubMed] [Google Scholar]
- 20. D’Agostino MA, Wakefield RJ, Berner-Hammer H, et al. Value of ultrasonography as a marker of early response to abatacept in patients with rheumatoid arthritis and an inadequate response to methotrexate: results from the APPRAISE study [published online November 20, 2015]. Ann Rheum Dis. doi: 10.1136/annrheumdis-2015-207709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. De Marchi A, Prever EB, Cavallo F, et al. Perfusion pattern and time of vascularisation with CEUS increase accuracy in differentiating between benign and malignant tumours in 216 musculoskeletal soft tissue masses. Eur J Radiol. 2015;84:142-150. [DOI] [PubMed] [Google Scholar]
- 22. De Zordo T, Lill SR, Fink C, et al. Real-time sonoelastography of lateral epicondylitis: comparison of findings between patients and healthy volunteers. AJR Am J Roentgenol. 2009;193:180-185. [DOI] [PubMed] [Google Scholar]
- 23. Distel LM, Best TM. Prolotherapy: a clinical review of its role in treating chronic musculoskeletal pain. PM R. 2011;3(6 suppl 1):S78-S81. [DOI] [PubMed] [Google Scholar]
- 24. Dougados M, Jousse-Joulin S, Mistretta F, et al. Evaluation of several ultrasonography scoring systems for synovitis and comparison to clinical examination: results from a prospective multicentre study of rheumatoid arthritis. Ann Rheum Dis. 2010;69:828-833. [DOI] [PubMed] [Google Scholar]
- 25. Dragoo JL, Wasterlain AS, Braun HJ, Nead KT. Platelet-rich plasma as a treatment for patellar tendinopathy: a double-blind, randomized controlled trial. Am J Sports Med. 2014;42:610-618. [DOI] [PubMed] [Google Scholar]
- 26. Drakonaki EE, Allen GM, Wilson DJ. Real-time ultrasound elastography of the normal Achilles tendon: reproducibility and pattern description. Clin Radiol. 2009;64:1196-1202. [DOI] [PubMed] [Google Scholar]
- 27. Drakonaki EE, Allen GM, Wilson DJ. Ultrasound elastography for musculoskeletal applications. Br J Radiol. 2012;85:1435-1445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Drakonaki EE, Kho JS, Sharp RJ, Ostlere SJ. Efficacy of ultrasound-guided steroid injections for pain management of midfoot joint degenerative disease. Skeletal Radiol. 2011;40:1001-1006. [DOI] [PubMed] [Google Scholar]
- 29. Engebretsen L, Steffen K, Alsousou J, et al. IOC consensus paper on the use of platelet-rich plasma in sports medicine. Br J Sports Med. 2010;44:1072-1081. [DOI] [PubMed] [Google Scholar]
- 30. Fader RR, Mitchell JJ, Chadayammuri VP, Hill J, Wolcott ML. Percutaneous ultrasound-guided hydrodissection of a symptomatic sural neuroma. Orthopedics. 2015;38:e1046-e1050. [DOI] [PubMed] [Google Scholar]
- 31. Falyar CR, Abercrombie C, Becker R, Biddle C. Intrathecal spread of injectate following an ultrasound-guided selective C5 nerve root injection in a human cadaver model. AANA J. 2016;84:80-84. [PubMed] [Google Scholar]
- 32. Ferrero G, Fabbro E, Orlandi D, et al. Ultrasound-guided injection of platelet-rich plasma in chronic Achilles and patellar tendinopathy. J Ultrasound. 2012;15:260-266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Fitzpatrick J, Bulsara M, Zheng MH. The effectiveness of platelet-rich plasma in the treatment of tendinopathy: a meta-analysis of randomized controlled clinical trials [published online June 6, 2016]. Am J Sports Med. doi: 10.1177/0363546516643716. [DOI] [PubMed] [Google Scholar]
- 34. Forsberg F, Ro RJ, Potoczek M, et al. Assessment of angiogenesis: implications for ultrasound imaging. Ultrasonics. 2004;42:325-330. [DOI] [PubMed] [Google Scholar]
- 35. Foster TE, Puskas BL, Mandelbaum BR, Gerhardt MB, Rodeo SA. Platelet-rich plasma: from basic science to clinical applications. Am J Sports Med. 2009;37:2259-2272. [DOI] [PubMed] [Google Scholar]
- 36. Galiano K, Obwegeser AA, Bodner G, et al. Real-time sonographic imaging for periradicular injections in the lumbar spine: a sonographic anatomic study of a new technique. J Ultrasound Med. 2005;24:33-38. [DOI] [PubMed] [Google Scholar]
- 37. Gamradt SC, Gallo RA, Adler RS, et al. Vascularity of the supraspinatus tendon three months after repair: characterization using contrast-enhanced ultrasound. J Shoulder Elbow Surg. 2010;19:73-80. [DOI] [PubMed] [Google Scholar]
- 38. Gofeld M, Bristow SJ, Chiu SC, McQueen CK, Bollag L. Ultrasound-guided lumbar transforaminal injections: feasibility and validation study. Spine (Phila Pa 1976). 2012;37:808-812. [DOI] [PubMed] [Google Scholar]
- 39. Grassi W, Filippucci E, Busilacchi P. Musculoskeletal ultrasound. Best Pract Res Clin Rheumatol. 2004;18:813-826. [DOI] [PubMed] [Google Scholar]
- 40. Guillin R, Botchu R, Bianchi S. Sonography of orthopedic hardware impingement of the extremities. J Ultrasound Med. 2012;31:1457-1463. [DOI] [PubMed] [Google Scholar]
- 41. Guillodo Y, Madouas G, Simon T, Le Dauphin H, Saraux A. Platelet-rich plasma (PRP) treatment of sports-related severe acute hamstring injuries. Muscles Ligaments Tendons J. 2016;5:284-288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Gutierrez M, Di Matteo A, Rosemffet M, et al. Short-term efficacy to conventional blind injection versus ultrasound-guided injection of local corticosteroids in tenosynovitis in patients with inflammatory chronic arthritis: a randomized comparative study. Joint Bone Spine. 2016;83:161-166. [DOI] [PubMed] [Google Scholar]
- 43. Haber HP, Sinis N, Haerle M, Schaller HE. Sonography of brachial plexus traction injuries. AJR Am J Roentgenol. 2006;186:1787-1791. [DOI] [PubMed] [Google Scholar]
- 44. Hamilton B, Tol JL, Almusa E, et al. Platelet-rich plasma does not enhance return to play in hamstring injuries: a randomised controlled trial. Br J Sports Med. 2015;49:943-950. [DOI] [PubMed] [Google Scholar]
- 45. Hill JC, Millan IS. Validation of musculoskeletal ultrasound to assess and quantify muscle glycogen content. A novel approach. Phys Sportsmed. 2014;42(3):45-52. [DOI] [PubMed] [Google Scholar]
- 46. Hong JP, Lew HL, Lee CH, Tang SF. Ultrasound-guided injection for the treatment of carpal tunnel syndrome. Am J Phys Med Rehabil. 2015;94:e119-e120. [DOI] [PubMed] [Google Scholar]
- 47. Housner JA, Jacobson JA, Misko R. Sonographically guided percutaneous needle tenotomy for the treatment of chronic tendinosis. J Ultrasound Med. 2009;28:1187-1192. [DOI] [PubMed] [Google Scholar]
- 48. Iagnocco A, Ceccarelli F, Perricone C, Valesini G. The role of ultrasound in rheumatology. Semin Ultrasound CT MR. 2011;32:66-73. [DOI] [PubMed] [Google Scholar]
- 49. Iagnocco A, Naredo E, Wakefield R, et al. Responsiveness in rheumatoid arthritis. A report from the OMERACT 11 ultrasound workshop. J Rheumatol. 2014;41:379-382. [DOI] [PubMed] [Google Scholar]
- 50. Jacobson JA. Fundamentals of Musculoskeletal Ultrasound. Philadelphia, PA: Saunders/Elsevier; 2007:345. [Google Scholar]
- 51. Jacobson JA, Rubin J, Yablon CM, Kim SM, Kalume-Brigido M, Parameswaran A. Ultrasound-guided fenestration of tendons about the hip and pelvis: clinical outcomes. J Ultrasound Med. 2015;34:2029-2035. [DOI] [PubMed] [Google Scholar]
- 52. Jee H, Lee JH, Kim J, Park KD, Lee WY, Park Y. Ultrasound-guided selective nerve root block versus fluoroscopy-guided transforaminal block for the treatment of radicular pain in the lower cervical spine: a randomized, blinded, controlled study. Skeletal Radiol. 2013;42:69-78. [DOI] [PubMed] [Google Scholar]
- 53. Kang S, Yang SN, Kim SH, Byun CW, Yoon JS. Ultrasound-guided cervical nerve root block: does volume affect the spreading pattern [published online March 23, 2016]? Pain Med. doi: 10.1093/pm/pnw027. [DOI] [PubMed] [Google Scholar]
- 54. Karaca L, Oral A, Kantarci M, et al. Comparison of the superb microvascular imaging technique and the color Doppler techniques for evaluating children’s testicular blood flow. Eur Rev Med Pharmacol Sci. 2016;20:1947-1953. [PubMed] [Google Scholar]
- 55. Klauser A, Demharter J, De Marchi A, et al. Contrast enhanced gray-scale sonography in assessment of joint vascularity in rheumatoid arthritis: results from the IACUS study group. Eur Radiol. 2005;15:2404-2410. [DOI] [PubMed] [Google Scholar]
- 56. Klauser AS, Miyamoto H, Bellmann-Weiler R, Feuchtner GM, Wick MC, Jaschke WR. Sonoelastography: musculoskeletal applications. Radiology. 2014;272:622-633. [DOI] [PubMed] [Google Scholar]
- 57. Klauser AS, Miyamoto H, Tamegger M, et al. Achilles tendon assessed with sonoelastography: histologic agreement. Radiology. 2013;267:837-842. [DOI] [PubMed] [Google Scholar]
- 58. Klauser AS, Peetrons P. Developments in musculoskeletal ultrasound and clinical applications. Skeletal Radiol. 2010;39:1061-1071. [DOI] [PubMed] [Google Scholar]
- 59. Kot BC, Zhang ZJ, Lee AW, Leung VY, Fu SN. Elastic modulus of muscle and tendon with shear wave ultrasound elastography: variations with different technical settings. PLoS One. 2012;7(8):e44348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Kwon DR, Park GY, Kwon JG. The change of intrinsic stiffness in gastrocnemius after intensive rehabilitation with botulinum toxin A injection in spastic diplegic cerebral palsy. Ann Rehabil Med. 2012;36:400-403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Kwon DR, Park GY, Lee SU, Chung I. Spastic cerebral palsy in children: dynamic sonoelastographic findings of medial gastrocnemius. Radiology. 2012;263:794-801. [DOI] [PubMed] [Google Scholar]
- 62. Labrosse JM, Cardinal E, Leduc BE, et al. Effectiveness of ultrasound-guided corticosteroid injection for the treatment of gluteus medius tendinopathy. AJR Am J Roentgenol. 2010;194:202-206. [DOI] [PubMed] [Google Scholar]
- 63. Liddle AD, Rodriguez-Merchan EC. Platelet-rich plasma in the treatment of patellar tendinopathy: a systematic review. Am J Sports Med. 2015;43:2583-2590. [DOI] [PubMed] [Google Scholar]
- 64. Lin HY, Wong PK, Ho WP, Chuang TY, Liao YS, Wong CC. Clavicular hook plate may induce subacromial shoulder impingement and rotator cuff lesion—dynamic sonographic evaluation. J Orthop Surg Res. 2014;9:6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Loizides A, Peer S, Plaikner M, Djurdjevic T, Gruber H. Perfusion pattern of musculoskeletal masses using contrast-enhanced ultrasound: a helpful tool for characterisation? Eur Radiol. 2012;22:1803-1811. [DOI] [PubMed] [Google Scholar]
- 66. Loizides A, Widmann G, Freuis T, Peer S, Gruber H. Optimizing ultrasound-guided biopsy of musculoskeletal masses by application of an ultrasound contrast agent. Ultraschall Med. 2011;32:307-310. [DOI] [PubMed] [Google Scholar]
- 67. Lu D, Tchelepi H. Ultrasound fusion: role in interventional musculoskeletal radiology. Ultrasound Q. 2015;31:219-220. [DOI] [PubMed] [Google Scholar]
- 68. Ma Y, Li G, Li J, Ren WD. The diagnostic value of superb microvascular imaging (SMI) in detecting blood flow signals of breast lesions: a preliminary study comparing SMI to color Doppler flow imaging. Medicine (Baltimore). 2015;94:e1502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Machado P, Segal S, Lyshchik A, Forsberg F. A novel microvascular flow technique: initial results in thyroids. Ultrasound Q. 2016;32:67-74. [DOI] [PubMed] [Google Scholar]
- 70. Martin JA, Biedrzycki AH, Lee KS, et al. In vivo measures of shear wave speed as a predictor of tendon elasticity and strength. Ultrasound Med Biol. 2015;41:2722-2730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Martinoli C, Bianchi S, Gandolfo N, Valle M, Simonetti S, Derchi LE. US of nerve entrapments in osteofibrous tunnels of the upper and lower limbs. Radiographics. 2000;20(spec no):S199-S213. Erratum in: Radiographics 2000;20: 1818. [DOI] [PubMed] [Google Scholar]
- 72. Masci L, Spang C, van Schie HT, Alfredson H. How to diagnose plantaris tendon involvement in midportion achilles tendinopathy—clinical and imaging findings. BMC Musculoskelet Disord. 2016;17:97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Maurits NM, Bollen AE, Windhausen A, De Jager AE, Van Der Hoeven JH. Muscle ultrasound analysis: normal values and differentiation between myopathies and neuropathies. Ultrasound Med Biol. 2003;29:215-225. [DOI] [PubMed] [Google Scholar]
- 74. Mautner K, Colberg RE, Malanga G, et al. Outcomes after ultrasound-guided platelet-rich plasma injections for chronic tendinopathy: a multicenter, retrospective review. PM R. 2013;5:169-175. [DOI] [PubMed] [Google Scholar]
- 75. Maxwell NJ, Ryan MB, Taunton JE, Gillies JH, Wong AD. Sonographically guided intratendinous injection of hyperosmolar dextrose to treat chronic tendinosis of the Achilles tendon: a pilot study. AJR Am J Roentgenol. 2007;189:W215-W220. [DOI] [PubMed] [Google Scholar]
- 76. McShane JM, Nazarian LN, Harwood MI. Sonographically guided percutaneous needle tenotomy for treatment of common extensor tendinosis in the elbow. J Ultrasound Med. 2006;25:1281-1289. [DOI] [PubMed] [Google Scholar]
- 77. McShane JM, Shah VN, Nazarian LN. Sonographically guided percutaneous needle tenotomy for treatment of common extensor tendinosis in the elbow: is a corticosteroid necessary? J Ultrasound Med. 2008;27:1137-1144. [DOI] [PubMed] [Google Scholar]
- 78. Miller TT, Reinus WR. Nerve entrapment syndromes of the elbow, forearm, and wrist. AJR Am J Roentgenol. 2010;195:585-594. [DOI] [PubMed] [Google Scholar]
- 79. Misawa S, Noto Y, Shibuya K, et al. Ultrasonographic detection of fasciculations markedly increases diagnostic sensitivity of ALS. Neurology. 2011;77:1532-1537. [DOI] [PubMed] [Google Scholar]
- 80. Miyamoto H, Halpern EJ, Kastlunger M, et al. Carpal tunnel syndrome: diagnosis by means of median nerve elasticity—improved diagnostic accuracy of US with sonoelastography. Radiology. 2014;270:481-486. [DOI] [PubMed] [Google Scholar]
- 81. Mosca MJ, Rodeo SA. Platelet-rich plasma for muscle injuries: game over or time out? Curr Rev Musculoskelet Med. 2015;8:145-153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. Mulvaney SW. Ultrasound-guided percutaneous neuroplasty of the lateral femoral cutaneous nerve for the treatment of meralgia paresthetica: a case report and description of a new ultrasound-guided technique. Curr Sports Med Rep. 2011;10:99-104. [DOI] [PubMed] [Google Scholar]
- 83. Nakamura M, Ikezoe T, Kobayashi T, et al. Acute effects of static stretching on muscle hardness of the medial gastrocnemius muscle belly in humans: an ultrasonic shear-wave elastography study. Ultrasound Med Biol. 2014;40:1991-1997. [DOI] [PubMed] [Google Scholar]
- 84. Naredo E, Cabero F, Beneyto P, et al. A randomized comparative study of short term response to blind injection versus sonographic-guided injection of local corticosteroids in patients with painful shoulder. J Rheumatol. 2004;31:308-314. [PubMed] [Google Scholar]
- 85. Naredo E, D’Agostino MA, Wakefield RJ, et al. Reliability of a consensus-based ultrasound score for tenosynovitis in rheumatoid arthritis. Ann Rheum Dis. 2013;72:1328-1334. [DOI] [PubMed] [Google Scholar]
- 86. Nwawka OK, Miller TT. Ultrasound-guided peripheral nerve injection techniques [published online June 24, 2016]. AJR Am J Roentgenol. doi: 10.2214/AJR.16.16378. [DOI] [PubMed] [Google Scholar]
- 87. Nwawka OK, Miller TT, Jawetz ST, Saboeiro GR. Ultrasound-guided perineural injection for nerve blockade: does a single-sided injection produce circumferential nerve coverage [published online May 7, 2016]? J Clin Ultrasound. doi: 10.1002/jcu.22364. [DOI] [PubMed] [Google Scholar]
- 88. Ohrndorf S, Hensch A, Naumann L, et al. Contrast-enhanced ultrasonography is more sensitive than grayscale and power Doppler ultrasonography compared to MRI in therapy monitoring of rheumatoid arthritis patients. Ultraschall Med. 2011;32(suppl 2):E38-E44. [DOI] [PubMed] [Google Scholar]
- 89. Ooi CC, Richards PJ, Maffulli N, et al. A soft patellar tendon on ultrasound elastography is associated with pain and functional deficit in volleyball players. J Sci Med Sport. 2016;19:373-378. [DOI] [PubMed] [Google Scholar]
- 90. Ooi CC, Schneider ME, Malliaras P, Chadwick M, Connell DA. Diagnostic performance of axial-strain sonoelastography in confirming clinically diagnosed Achilles tendinopathy: comparison with B-mode ultrasound and color Doppler imaging. Ultrasound Med Biol. 2015;41:15-25. [DOI] [PubMed] [Google Scholar]
- 91. Park Y, Ahn JK, Sohn Y, et al. Treatment effects of ultrasound guide selective nerve root block for lower cervical radicular pain: a retrospective study of 1-year follow-up. Ann Rehabil Med. 2013;37:658-667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92. Peltz CD, Haladik JA, Divine G, Siegal D, van Holsbeeck M, Bey MJ. Shear wave elastography: repeatability for measurement of tendon stiffness. Skeletal Radiol. 2013;42:1151-1156. [DOI] [PubMed] [Google Scholar]
- 93. Reach JS, Easley ME, Chuckpaiwong B, Nunley JA., 2nd Accuracy of ultrasound guided injections in the foot and ankle. Foot Ankle Int. 2009;30:239-242. [DOI] [PubMed] [Google Scholar]
- 94. Rossi LA, Molina Rómoli AR, Bertona Altieri BA, Burgos Flor JA, Scordo WE, Elizondo CM. Does platelet-rich plasma decrease time to return to sports in acute muscle tear? A randomized controlled trial [published online April 16, 2016]. Knee Surg Sports Traumatol Arthrosc. doi: 10.1007/s00167-016-4129-7. [DOI] [PubMed] [Google Scholar]
- 95. Ryan M, Wong A, Rabago D, Lee K, Taunton J. Ultrasound-guided injections of hyperosmolar dextrose for overuse patellar tendinopathy: a pilot study. Br J Sports Med. 2011;45:972-977. [DOI] [PubMed] [Google Scholar]
- 96. Ryan M, Wong A, Taunton J. Favorable outcomes after sonographically guided intratendinous injection of hyperosmolar dextrose for chronic insertional and midportion Achilles tendinosis. AJR Am J Roentgenol. 2010;194:1047-1053. [DOI] [PubMed] [Google Scholar]
- 97. Sconfienza LM, Silvestri E, Cimmino MA. Sonoelastography in the evaluation of painful achilles tendon in amateur athletes. Clin Exp Rheumatol. 2010;28:373-378. [PubMed] [Google Scholar]
- 98. Tagliafico A, Bodner G, Rosenberg I, et al. Peripheral nerves: ultrasound-guided interventional procedures. Semin Musculoskelet Radiol. 2010;14:559-566. [DOI] [PubMed] [Google Scholar]
- 99. Tagliafico A, Serafini G, Lacelli F, Perrone N, Valsania V, Martinoli C. Ultrasound-guided treatment of meralgia paresthetica (lateral femoral cutaneous neuropathy): technical description and results of treatment in 20 consecutive patients. J Ultrasound Med. 2011;30:1341-1346. [DOI] [PubMed] [Google Scholar]
- 100. Tan S, Kudas S, Ozcan AS, et al. Real-time sonoelastography of the Achilles tendon: pattern description in healthy subjects and patients with surgically repaired complete ruptures. Skeletal Radiol. 2012;41:1067-1072. [DOI] [PubMed] [Google Scholar]
- 101. Taylor PC. The value of sensitive imaging modalities in rheumatoid arthritis. Arthritis Res Ther. 2003;5:210-213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102. Tsukamoto H, Granata G, Coraci D, Paolasso I, Padua L. Ultrasound and neurophysiological correlation in common fibular nerve conduction block at fibular head. Clin Neurophysiol. 2014;125:1491-1495. [DOI] [PubMed] [Google Scholar]
- 103. Verbeek RJ, Sentner CP, Smit GP, et al. Muscle ultrasound in patients with glycogen storage disease types I and III. Ultrasound Med Biol. 2016;42:133-142. [DOI] [PubMed] [Google Scholar]
- 104. Vlad V, Berghea F, Micu M, et al. Tenosynovitis US scoring systems follow synovitis and clinical scoring systems in RA and are responsive to change after biologic therapy. Med Ultrason. 2015;17:352-360. [DOI] [PubMed] [Google Scholar]
- 105. Walker KJ, McGrattan K, Aas-Eng K, Smith AF. Ultrasound guidance for peripheral nerve blockade. Cochrane Database Syst Rev. 2009;(4):CD006459. [DOI] [PubMed] [Google Scholar]
- 106. Wesner M, Defreitas T, Bredy H, et al. A pilot study evaluating the effectiveness of platelet-rich plasma therapy for treating degenerative tendinopathies: a randomized control trial with synchronous observational cohort. PLoS One. 2016;11(2):e0147842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107. Wilson SR, Greenbaum LD, Goldberg BB. Contrast-enhanced ultrasound: what is the evidence and what are the obstacles? AJR Am J Roentgenol. 2009;193:55-60. [DOI] [PubMed] [Google Scholar]
- 108. Wong-On M, Til-Perez L, Balius R. Evaluation of MRI-US fusion technology in sports-related musculoskeletal injuries. Adv Ther. 2015;32:580-594. [DOI] [PubMed] [Google Scholar]
- 109. Yablon CM, Hammer MR, Morag Y, Brandon CJ, Fessell DP, Jacobson JA. US of the peripheral nerves of the lower extremity: a landmark approach. Radiographics. 2016;36:464-478. [DOI] [PubMed] [Google Scholar]
- 110. Yoshitake Y, Takai Y, Kanehisa H, Shinohara M. Muscle shear modulus measured with ultrasound shear-wave elastography across a wide range of contraction intensity. Muscle Nerve. 2014;50:103-113. [DOI] [PubMed] [Google Scholar]
- 111. Zaidman CM, Seelig MJ, Baker JC, Mackinnon SE, Pestronk A. Detection of peripheral nerve pathology: comparison of ultrasound and MRI. Neurology. 2013;80:1634-1640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112. Zissen MH, Wallace G, Stevens KJ, Fredericson M, Beaulieu CF. High hamstring tendinopathy: MRI and ultrasound imaging and therapeutic efficacy of percutaneous corticosteroid injection. AJR Am J Roentgenol. 2010;195:993-998. [DOI] [PubMed] [Google Scholar]