Abstract
Background:
Current cost data on tissue expansion followed by exchange for permanent implant (TE/I) reconstruction lack a necessary assessment of the experience of a heterogenous breast cancer patient population and their multiple outcome pathways. We extend our previous analysis to that of direct hospital cost as bundling of payments is likely to follow the changing centralization of cancer care at the hospital level.
Methods:
We performed a retrospective analysis (2003–2009) of TE/I reconstructions with or without an acellular dermal matrix (ADM), namely Alloderm RTM. Postreconstructive events were analyzed and organized into outcome pathways as previously described. Aggregated and normalized inpatient and outpatient hospital direct costs and physician reimbursement were generated for each outcome pathway with or without ADM.
Results:
Three hundred sixty-seven patients were analyzed. The average 2-year hospital direct cost per TE/I breast reconstruction patient was $11,862 in the +ADM and $12,319 in the −ADM groups (P > 0.05). Initial reconstructions were costlier in the +ADM ($6,868) than in the −ADM ($5,615) group, but the average cost of subsequent postreconstructive events within 2 years was significantly lower in +ADM ($5,176) than −ADM ($6,704) patients (P < 0.05). When a complication occurred, but reconstruction was still completed within 2 years, greater costs were incurred in the −ADM than in the +ADM group for most scenarios, leading to a net equalization of cost between study groups.
Conclusion:
Although direct hospital cost is an important factor for resource and fund allocation, it should not remain the sole factor when deciding to use ADM in TE/I reconstruction.
With a price tag of $7 billion dollars in 2011, breast reconstruction is under close scrutiny for cost reduction and value maximization in a healthcare system, experiencing increased pressure to focus on cost containment.1–3 Payers continue to evolve new reimbursement strategies to parallel geographic consolidation of multidisciplinary breast cancer care with bundled payments. Numerous studies have examined the costs associated with autologous breast reconstruction.4,5 However, the Nationwide Inpatient Sample database shows an absolute and relative increase in the number of breast reconstructions performed with tissue expansion followed by exchange for a permanent implant (TE/I).6 In fact, TE/I reconstruction has increased more than 2-fold and presently accounts for the majority of all reconstructive breast procedures in the United States, thus highlighting the need for studying resource allocation and funding of this treatment approach.7,8 Paralleling national trends, individual institutions have reported that TE/I reconstructions account for 45% of total cost attributed to breast reconstruction.7 Despite these changes, there is a paucity of data to guide how bundling should occur for TE/I. We have previously reported outcome pathways in TE/I with acellular dermal matrices and sought to examine the costs incurred at the hospital level by these outcome pathways.
Practice patterns, including those for TE/I reconstructions evolve as new, innovative technology, are incorporated into practice. Acellular dermal matrices (ADMs) have caused a paradigm shift in TE/I reconstructions in the past decade, citing numerous indications, including but not limited to improved aesthetic outcomes, increased expansion volumes, and shorter time to final exchange for permanent implants.9–12 The cost-effectiveness of such technology has been examined, albeit in a limited fashion, using either retrospective review of previous studies, samples of a larger cohort to extrapolate cost data, or only index operation costs as cost-minimization, cost-effectiveness, and cost-utility analyses.7,13–15 To date, no study has performed an analysis of ADMs in two-stage implant–based reconstruction using actual cost data directly incurred by the hospital with representation of the divergent outcome pathways TE/I reconstruction patients undergo. With the advent of accountable care organizations, bundling of payments and disbursement of funds is likely to occur at the hospital level. Currently, the hospital typically absorbs the cost of a device like ADM with supply cost of the item readily apparent to hospital managers. However, the extent to which there are off-setting cost savings for the hospital over time has not been well studied. It is imperative for plastic surgeons to be aware of the hospital costs associated with the services they provide patients in TE/I reconstruction.
Although cost data should not be the sole factor when developing a reconstructive plan for a patient, it should be examined within the context of patient demographics, risk factors, and their individual treatment algorithms, which may include chemotherapy and radiation. Current data about cost of TE/I reconstruction does not fully represent the experience of a heterogenous patient population and their multiple outcome pathways. Cost analyses often use shortened time frames, capturing only costs at or near the time of reconstruction and missing the full impact of service required to complete a two-staged reconstruction. We extend our previous analysis to that of cost to set the stage for meaningful discussions between providers, patients, and payers to define the value of breast reconstruction.
METHODS
Study Population
A retrospective analysis of all patients treated with TE/I at Barnes Jewish and Barnes Jewish West County Hospitals and treated by plastic surgeons from the Washington University School of Medicine from January 1, 2003, to December 31, 2009, was conducted under the approval of the institutional Human Research Protection Office (#201106126) as previously described.16 Immediate and delayed TE/I reconstructions were included for analysis in patients undergoing unilateral or bilateral skin-sparing mastectomies performed for cancer or prophylaxis. All TEs were textured Allergan (Allergan Medical, Irvine, Calif.) 133MV devices, and implants were Allergan round moderate- or high-profile silicone or saline devices (style 15, 20, 68MP, and 68HP) as these were on consignment at our institution during the study period. Patients with concomitant or previous ipsilateral flap reconstruction, concurrent congenital or acquired ipsilateral breast deformity, and nipple-sparing mastectomy with immediate implant and patients for whom flap placement after tissue expansion was initially planned were excluded. Patients in which an ADM other than AlloDerm RTM (LifeCell, Branchburg, N.J.) was used were excluded because usage of other ADM products, including Alloderm RTU and vicryl mesh, was too infrequent during the study period to sufficiently power a subset analysis. Medical records were examined for evidence of postreconstructive events, defined as related procedures or complications. Complications identified included seroma, hematoma, mastectomy flap necrosis, wound dehiscence with loss of continuity of the mastectomy incision in the absence of necrosis, cellulitis (infection without seroma), capsular contracture requiring intervention other than during the expander exchange, and ADM complications (poor incorporation or dehiscence of the scaffold). Related procedures included unexpected explantation or capsular revisions and procedures to replace failed devices, manage complications, or improve symmetry. Explantation was recorded for the unintended removal of either the TE or permanent breast implant at any time during the 2-year study period. Capsular revisions were documented when a major revision of the periprosthetic capsule performed other than at the implant exchange was used to obtain symmetry or favorable contour. Nipple areolar reconstruction was not evaluated because it was often performed outside the hospital setting and therefore inconsistently recorded and because it varied according to patient preference. Common sequences of postreconstructive events were combined into outcome pathways and analyzed by study arm. Selection criteria for ADM use were not assessed in this study.
Cost Analyses
Barnes Jewish Hospital provided aggregated cost data on selected patients, exemplifying patient scenarios or “cost exemplars.” For the initial reconstruction, privately insured patients with no unrelated procedures were randomly selected in equal numbers from inpatient and outpatient settings to represent −ADM and +ADM reconstructions from both earlier and later years of ADM use at the institution. We excluded cases with a nondominant brand of tissue expander or unusually long general surgery portion of the case. The mix of bilateral and unilateral reconstructions among cost exemplars was determined by chi-square to be representative of the entire study arm for both +ADM (P > 0.05) and −ADM (P > 0.05) reconstructions. In each study arm, a group of 3 representative patients was identified for each outcome pathway with sufficient frequency for analysis. Patients with incomplete cost data or whose left and right breasts were reconstructed separately were excluded as exemplars.
The hospital supplied aggregated direct cost normalized to 2011 dollars at 3% per annum for postreconstructive events of the cost exemplars in each study arm for each outcome pathway and for initial reconstructions. “Direct costs” are those that can be traced directly to a department, product, or service, excluding overhead costs, and thus reflect the hospital’s assessment of the cost it incurred, providing the specific services and supplies used by the patients.17 The average per-patient cost obtained for each group of exemplars was applied to all patients in the same outcome pathway and study arm. Billing operations from the Washington University Physicians medical group provided aggregated data on physician reimbursement for these “cost exemplars” on the same basis.
Statistical Analyses
The overall cost data between patients who had ADM and those who did not was amenable to statistical comparison with a two-sample independent t test because there was no variance in the averaged costs assigned to patients in each reconstructive pathway. Statistical analyses were performed using SAS/STAT version 9.2 (SAS Corporation, Cary, N.C.). Statistically significant findings were reported when P < 0.05. Hospital requirements preclude disclosure of patient-level cost data because of its proprietary nature. Because we could not perform patient-level analyses, we averaged costs for patients exemplifying a particular pathway. Because all patients in a pathway are assigned the same cost, based on the pathway average, there is no variance between patients. As such, cost differences between the 2 study arms for the same pathway or for the initial reconstruction cannot be evaluated statistically.
RESULTS
Three hundred sixty-seven of 415 patients had sufficient information for inclusion in the cost analyses (+ADM = 265; −ADM = 102), and their demographic information is summarized in Table 1. The average age of patients was 50 (+ADM = 50; −ADM = 50), and body mass index (BMI) was 28.2 kg/m2 (+ADM = 27.7; −ADM = 29.4). The total average 2-year hospital direct cost per TE/I breast reconstruction patient was $11,862 in the +ADM and $12,319 in the −ADM groups (Fig. 1A). Initial reconstructions were costlier in the +ADM ($6,868) than the −ADM ($5,615) group, but the average cost of subsequent postreconstructive events within 2 years was significantly lower in +ADM ($5,176) than –ADM ($6,704) patients (P < 0.05) (Table 2). Uneventful implant exchange cost an additional $2,974 in the +ADM and $4,036 in the –ADM groups, whereas the need for additional revisions further escalated cost (Table 2). Of note, only 1 patient in the +ADM group and none in the –ADM group experienced capsular contracture requiring surgery not concurrent with the expander exchange.
Table 1.
Cost Study Patient Population Demographics
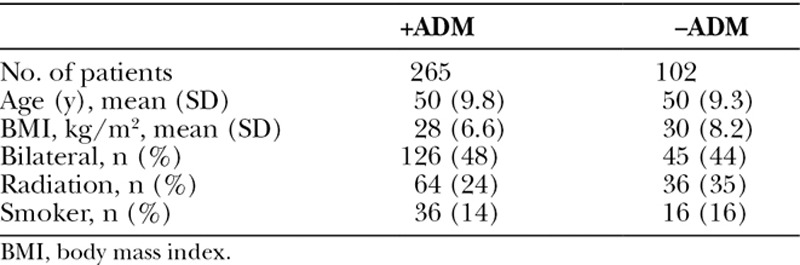
Fig. 1.
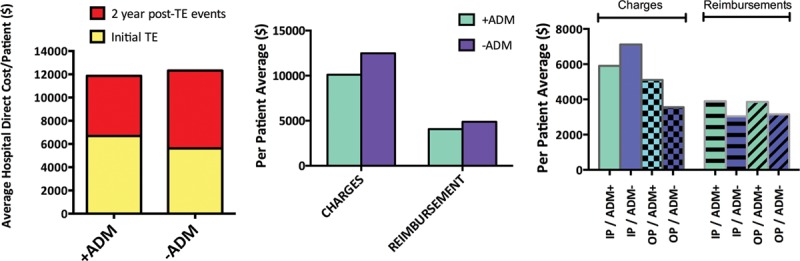
Two-year hospital direct costs, surgeon charges, and reimbursement for staged TE/I reconstructions. Data are reported as per-patient average. A, Hospital direct costs, including initial TE operation ±ADM and 2 y post TE reconstructive events. B, Surgeon charges and reimbursements for initial TE/I reconstruction ±ADM in inpatient versus outpatient settings. C, Surgeon charges and reimbursements for 2 y after initial TE reconstruction ±ADM. IP, inpatient setting; OP, outpatient setting.
Table 2.
Hospital Direct Cost per Patient for Postreconstructive Services Within 2 y by Outcome Pathway
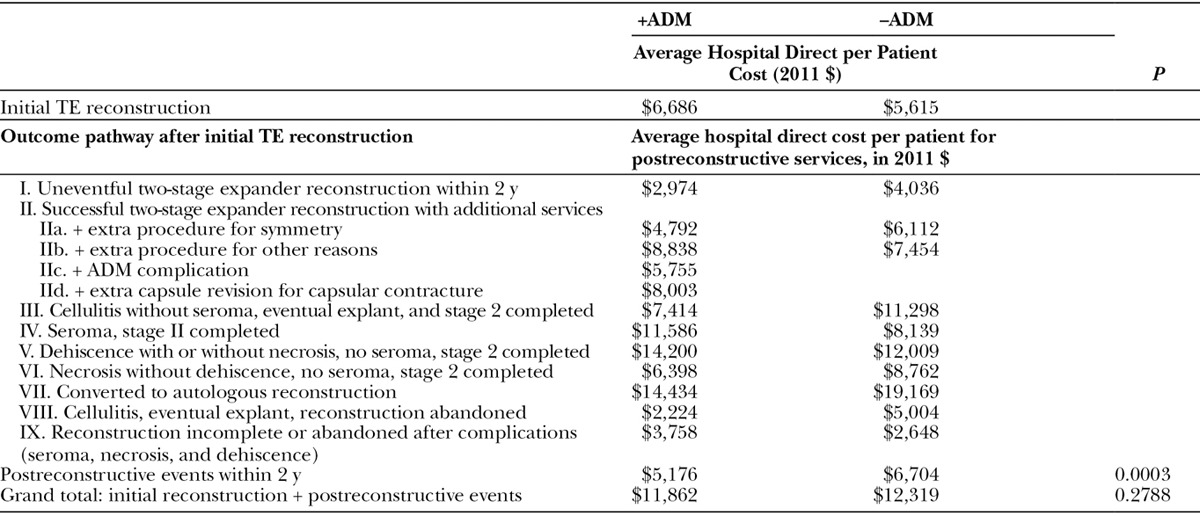
In cases where a complication occurred, but reconstruction was still completed within 2 years, costs incurred were greater in the –ADM than in +ADM group for most scenarios (Table 2 and Fig. 1A). Rates of cellulitis without seroma requiring explant with eventual implant exchange within 2 years (Table 2, pathway III) occurred in 4% of +ADM ($7,414) and 5% of –ADM ($11,298) reconstructions. Rates of seroma (Table 2, pathway IV) were also similar in both groups (4% vs 3%) but cost more for +ADM ($11,586) than −ADM ($8,139) reconstructions. Dehiscence without necrosis (Table 2, pathway V) was more common in −ADM versus +ADM reconstructions (12% vs 4%) with an additional cost of $12,009 and $14,200, respectively. Necrosis without dehiscence (Table 2, pathway VI) occurred more commonly with ADM reconstruction (6% vs 2%) but cost less on average per patient ($6,398 vs $8,762). Rates of conversion to autologous reconstruction (Table 2, pathway VII) were similar in both groups and cost $14,434 and $19,169 for +ADM and −ADM groups. Cellulitis eventually leading to explantation with an abandoned reconstruction at 2 years (Table 2, pathway VIII) was less costly in the +ADM group ($2,224 vs $5,004). Reconstruction that was incomplete or abandoned after complications (Table 2, pathway IX) were similar (7% and 5%) with costs of $3,758 and $2,648 in the +ADM and −ADM groups.
Surgeon charges and reimbursements with ADM for inpatient services were $5,900 and $3,887 and for outpatient services $5,103 and $3,849, respectively (Fig. 1B). Without ADM, surgeon charges and reimbursements for inpatient services were $7,116 and $3,028 and for outpatient services $3,559 and $3,144, respectively. Charges and reimbursements were not significantly different regardless of ADM use or inpatient versus outpatient setting of services rendered.
The average surgeon charges per patient for postreconstruction services was $10,112 with ADM and $12,476 without ADM. Average surgeon reimbursement per patient for postreconstruction services was $4,067 with ADM and $4,887 without ADM. Physician charges and reimbursements were similar between study arms (Fig. 1C).
DISCUSSION
With the advent of bundled payments and geographic consolidation of cancer care around hospitals and cancer centers,18,19 it remains imperative for plastic surgeons to be informed about the costs at the hospital level for patients who undergo TE/I reconstruction, as this is the most commonly performed reconstruction and is increasing in popularity.6 Previous studies have compared the costs of TE/I reconstruction versus autologous reconstruction, but the TE/I reconstructions examined did not include reconstructions with ADM.5,8 Other studies examining the cost of ADM use have studied the costs incurred based on individual complication events and not in the setting of a longitudinal experience or outcome pathways as we have previously described.13–16 The present study is important because very little has been published previously about cost from a hospital’s perspective as these data are difficult to obtain, yet it is the hospital that absorbs the cost of the ADM. Although the cost of ADM or any surgical device may be obvious to the hospital, no hospital administration’s budget has a line item that would show offsetting cost reductions over time. We think that the perspective offered by this study is not only novel but also particularly informative to discussions on value in breast reconstruction.
At our institution, the use of ADM in TE/I reconstruction increased substantially after its introduction in 2005, was limited to sheets that were 12 × 6, 16 × 6, or 16 × 8 cm2 and parallels other single-institution experiences with ADM.7,15 One of the main criticisms of using any ADM is its product cost. In our series, the initial direct hospital cost of TE/I reconstruction was higher when ADM was used, but the difference was lower than the list price for even the smallest sheet of ADM used in this series (6 × 12 cm).13,20 One variable that may influence this cost discrepancy is lower negotiated ADM product costs at the institutional level. Our analysis, however, highlights an important fact about not only the present study but also cost analysis as a whole: the cost of an ADM may not be accurately reflected by simply inputting its retail cost into a hypothetical model as its utilization may impact operative time, surgical technique, negotiated product costs with the vendor, among other factors that influence direct hospital cost.
Cost also needs to be evaluated in the context of patient’s outcome pathways. We found that the weighted, average hospital direct cost of reconstructive events in the 2 years after TE insertion varied by clinical pathway, but overall it was significantly lower in patients who had ADM. The net effect was an equalization of overall cost between study arms inclusive of the initial TE procedure and any procedures up until exchange with an implant or autologous flap within the 2-year period of the study. Importantly, although the majority of 2-year reconstructive pathways were less costly in the +ADM study arm, these differences must be interpreted with caution as pathway-level statistical comparisons could not be performed for reasons outlined in the Methods section.
The 2-year costs of successful reconstructions that require no or only minor revisions or unsuccessful reconstructions that were abandoned were considerably cheaper than those requiring interventions for salvage. BMI, radiation, and smoking influenced postreconstructive events and the outcome pathways that they associate with to a greater extent than whether ADM was used as we have previously reported.16 Hence, the decision to use ADM or not needs to be based on patient-specific factors, including but not limited to BMI and radiation and not solely on cost.
We found that the percent of patients who were irradiated differed significantly between the study arms (±ADM, P < 0.05). Our previous study found that irradiated patients were 2.2 times more likely than patients without radiation to have complications or additional procedures, veering away from an uneventful reconstruction.16 Subset analysis of ADM patients who were irradiated showed average downstream costs of $6,422 versus $4,704 for those without radiation. If 35% of the ADM study arm had incurred $1,719 in additional costs (i.e., 92 instead of 64 irradiated patients), we estimate this would had added $181.59 to total cost per ADM patient. This modest increase in cost (1.5%) is not enough to change our overall finding that over 2 years, average cost per patient reconstructed with ADM trended lower albeit not significantly than patients without ADM. Our findings add to previous reports of TE/I reconstruction without ADM in which pre- or postoperative radiation did not significantly affect costs.8
Our analysis included surgeon charges and reimbursements for initial TE/I reconstruction ±ADM in inpatient versus outpatient settings and also surgeon charges and reimbursements for 2 years after initial TE reconstruction ±ADM. These were not found to be significantly different, suggesting that physician provider cost does not vary with the use of ADM at our institution. Although charges and reimbursements are measures of revenue rather than physician cost, the findings suggest that revenue incentives for physicians are not misaligned with cost incentive for hospitals, as often can happen. From the perspectives we analyzed, over a 2-year time period, neither hospitals nor physicians have a significant financial incentive to use or avoid the use of ADM.
Our study has several limitations. Analysis was based on “direct costs” or the cost that can be traced directly to a department, product, or service, excluding overhead costs.17 We felt that the hospital’s assessment of the cost it incurred providing the specific services and supplies used by the patients would be valuable information with the advent of systems, such as accountable care organizations and reimbursement based on hospital billing. In addition, although our assessment of direct cost is at 2 hospitals, it still represents the experience of 1 hospital system but lays the foundation for studies in other institutions in other geographic locations. In our study, costs were aggregated from a limited group of patients, and line item and patient-level cost detail were unavailable.
Trends in TE/I reconstruction are rapidly evolving with increased use of fat grafting as a subsequent procedure.20 Further investigation on the costs incurred by these procedures will need to be examined as fat grafting is becoming a near routine “touch up” procedure for breast revisions in TE/I reconstructions at many institutions, including our own.
Because there is an equalization of overall direct hospital cost between the 2 study groups, our findings point to ADM use as 1 factor in a complex web of interactions that impact costs. Its limited impact on cost over a 2-year period suggests that the more important focus might be on careful attention to risk and patient factors associated with different TE/I reconstruction outcome pathways.
ACKNOWLEDGMENTS
We are grateful to Tracey Guthrie, Director of Clinical Trials in the Department of Surgery at Washington University, for her administrative assistance with coordinating our institutional review board (IRB), research grant, and recruitment of data abstractors. We are grateful to Mr. Vic Agarwal, Senior Financial Analyst, Barnes Hospital, Saint Louis for providing aggregate hospital direct cost data based on clinical pathways. We are grateful to Mrs. Kathy Hoertel, formerly Director of Billing Operations, and Ms. Melissa Wainwright, formerly Manager Third Party Reimbursements from the Department of Surgery of the Washington University School of Medicine for providing physician reimbursement data. In addition, we are grateful to Ann Marie Dawidczyk, formerly from LifeCell for grant and study coordination. We are grateful to LifeCell corporation for providing funds specifically allocated to provide salary support for data abstractors, preparation and renewal of our IRB, and funds for third party support of Strategic Health Resources that developed the relational database and designed and executed the statistical analyses described herein.
Footnotes
Disclosure: Dr. Myckatyn receives grant funding from Lifecell Corporation. Funds from Lifecell Corporation were used to pay for third party statistician and salaries of data abstractors at Washington University. The Article Processing Charge was paid for by the authors.
REFERENCES
- 1.Porter ME. What is value in health care? N Engl J Med. 2010;363:2477–2481. doi: 10.1056/NEJMp1011024. [DOI] [PubMed] [Google Scholar]
- 2.Porter ME. A strategy for health care reform–toward a value-based system. N Engl J Med. 2009;361:109–112. doi: 10.1056/NEJMp0904131. [DOI] [PubMed] [Google Scholar]
- 3.Assurance NCfQ. Breast Cancer Screening in The State of Health Care Quality. 2007 [Google Scholar]
- 4.Fischer JP, Fox JP, Nelson JA, et al. A longitudinal assessment of outcomes and healthcare resource utilization after immediate breast reconstruction-comparing implant- and autologous-based breast reconstruction. Ann Surg. 2015;262:692–699. doi: 10.1097/SLA.0000000000001457. [DOI] [PubMed] [Google Scholar]
- 5.Fischer JP, Wes AM, Nelson JA, et al. Propensity-matched, longitudinal outcomes analysis of complications and cost: comparing abdominal free flaps and implant-based breast reconstruction. J Am Coll Surg. 2014;219:303–312. doi: 10.1016/j.jamcollsurg.2014.02.028. [DOI] [PubMed] [Google Scholar]
- 6.Albornoz CR, Bach PB, Mehrara BJ, et al. A paradigm shift in U.S. breast reconstruction: increasing implant rates. Plast Reconstr Surg. 2013;131:15–23. doi: 10.1097/PRS.0b013e3182729cde. [DOI] [PubMed] [Google Scholar]
- 7.Fitzpatrick AM, Gao LL, Smith BL, et al. Cost and outcome analysis of breast reconstruction paradigm shift. Ann Plast Surg. 2014;73:141–149. doi: 10.1097/SAP.0b013e318276d979. [DOI] [PubMed] [Google Scholar]
- 8.Yan C, Fischer JP, Wes AM, et al. The cost of major complications associated with immediate two-stage expander/implant-based breast reconstruction. J Plast Surg Hand Surg. 2015;49:166–171. doi: 10.3109/2000656X.2014.970639. [DOI] [PubMed] [Google Scholar]
- 9.Pannucci CJ, Antony AK, Wilkins EG. The impact of acellular dermal matrix on tissue expander/implant loss in breast reconstruction: an analysis of the tracking outcomes and operations in plastic surgery database. Plast Reconstr Surg. 2013;132:1–10. doi: 10.1097/PRS.0b013e318290f917. [DOI] [PubMed] [Google Scholar]
- 10.Sbitany H, Serletti JM. Acellular dermis-assisted prosthetic breast reconstruction: a systematic and critical review of efficacy and associated morbidity. Plast Reconstr Surg. 2011;128:1162–1169. doi: 10.1097/PRS.0b013e318230c29e. [DOI] [PubMed] [Google Scholar]
- 11.Davila AA, Seth AK, Wang E, et al. Human Acellular dermis versus submuscular tissue expander breast reconstruction: a multivariate analysis of short-term complications. Arch Plast Surg. 2013;40:19–27. doi: 10.5999/aps.2013.40.1.19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sbitany H, Sandeen SN, Amalfi AN, et al. Acellular dermis-assisted prosthetic breast reconstruction versus complete submuscular coverage: a head-to-head comparison of outcomes. Plast Reconstr Surg. 2009;124:1735–1740. doi: 10.1097/PRS.0b013e3181bf803d. [DOI] [PubMed] [Google Scholar]
- 13.Krishnan NM, Chatterjee A, Rosenkranz KM, et al. The cost effectiveness of acellular dermal matrix in expander-implant immediate breast reconstruction. J Plast Reconstr Aesthet Surg. 2014;67:468–476. doi: 10.1016/j.bjps.2013.12.035. [DOI] [PubMed] [Google Scholar]
- 14.Krishnan NM, Chatterjee A, Van Vliet MM, et al. A comparison of acellular dermal matrix to autologous dermal flaps in single-stage, implant-based immediate breast reconstruction: a cost-effectiveness analysis. Plast Reconstr Surg. 2013;131:953–961. doi: 10.1097/PRS.0b013e3182865a24. [DOI] [PubMed] [Google Scholar]
- 15.de Blacam C, Momoh AO, Colakoglu S, et al. Cost analysis of implant-based breast reconstruction with acellular dermal matrix. Ann Plast Surg. 2012;69:516–520. doi: 10.1097/SAP.0b013e318217fb21. [DOI] [PubMed] [Google Scholar]
- 16.Qureshi A, Broderick K, Belz J, et al. Uneventful versus successful reconstruction and outcome pathways in implant based breast reconstruction with acellular dermal matrices. Plast Reconstr Surg. 2016;138:173e–183e. doi: 10.1097/PRS.0000000000002402. [DOI] [PubMed] [Google Scholar]
- 17.Nowicki M. The Financial Management of Hospitals and Healthcare Organizations. 4th ed. Chicago, IL: Health Administration Press; 2007. [Google Scholar]
- 18.Elmore L, Myckatyn TM, Gao F, et al. Reconstruction patterns in a single institution cohort of women undergoing mastectomy for breast cancer. Ann Surg Oncol. 2012;19:3223–3229. doi: 10.1245/s10434-012-2530-0. [DOI] [PubMed] [Google Scholar]
- 19.Bauder AR, Sarik JR, Butler PD, et al. Geographic variation in access to plastic surgeons. Plast Reconstr Surg. 2015;136(4 suppl):53. doi: 10.1097/SAP.0000000000000651. [DOI] [PubMed] [Google Scholar]
- 20.American Society of Plastic Surgeons. Complete Plastic Surgery Statistics Report. Washington, DC: 2014. [Google Scholar]


