Supplemental Digital Content is available in the text.
Abstract
Background:
Nipple reconstruction is the last stage in cosmetic reconstruction of the breast after mastectomy, but no method produces reliable and consistent aesthetic results. This study examined the use of the Biodesign Nipple Reconstruction Cylinder (NRC) during reconstruction of the nipple after mastectomy.
Methods:
Patients with a history of breast cancer and mastectomy desiring nipple reconstruction were invited to participate. After obtaining consent, unilateral or bilateral nipple reconstruction was performed. Skin flaps were raised, the NRC was placed beneath the flaps as a stent, and the site was protected for up to 4 weeks with a nipple shield. Nipple projection was measured for 12 months after surgery. Patient satisfaction was measured and adverse events were recorded. Follow-up examinations were performed at 1 week, and then at 1, 3, 6, and 12 months after surgery.
Results:
Eighty-two nipple reconstructions were performed in 50 patients. Related postoperative adverse events were minor, but reported in 8 reconstructions (9.8%) representing 7 patients (14.0%). Average projection at 6 and 12 months was 4.1 ± 1.6 mm and 3.8 ± 1.5 mm, respectively, compared with 10.5 ± 2.2 mm 1 week after surgery. Of patients completing the satisfaction questionnaire at 12 months, 70/75 (93.3%) of reconstructions were rated “pleased” or “very pleased” with the overall outcome. Overall, 45/46 (97.8%) patients would recommend nipple reconstruction to other women.
Conclusions:
The Biodesign NRC offers a safe alternative to nipple reconstruction, resulting in stable projection and a high level of patient satisfaction for 12 months after placement.
Nipple–areola reconstruction surgery completes the total aesthetic objective of breast reconstruction after mastectomy. Studies have shown that the recreation of the nipple has a high correlation with overall patient satisfaction and acceptance of body image,1 but long-term patient total satisfaction has been reported to be as low as 16%.2 Thus, it is highly important to the psychological health of the patient that completion of the breast reconstruction by creating a nipple–areola complex that matches the contralateral nipple has a positive aesthetic result. Although a wide variety of surgical techniques have been described to reconstruct the nipple–areola complex, loss of projection over time remains a challenge. Projection loss is disappointing to patients, results in poor patient satisfaction, and degrades the aesthetic outcome.
To overcome nipple projection loss with skin flaps alone, many surgeons have advocated the insertion of alloplastic materials, such as calcium hydroxylapatite1 or polytetrafluoroethylene,3 or autologous tissue grafts, to act as an internal stent or bolster to support projection. Although autologous techniques, which use rib cartilage,4 auricular cartilage,5 dermis,6,7 or other autologous tissues,8 generally have been successful, the harvesting of the autologous graft material can lead to increased operative times and greater patient morbidity, including pain and infection.
To avoid the disadvantages of creating a donor site, off-the-shelf materials derived from collagen have also been developed and reported for use in nipple reconstruction.9,10 These materials include devices made from small intestinal submucosa (SIS)9 or human acellular dermis.10 The Biodesign Nipple Reconstruction Cylinder (NRC; Cook Biotech Incorporated, West Lafayette, Ind.) is a tightly rolled cylinder of extracellular matrix collagen derived from porcine SIS. It is available in diameters of 0.7 and 1.0 cm and in lengths of 1.0 and 1.5 cm, can be trimmed to size as required aesthetically, and is the only FDA-cleared device specifically intended for implantation to reinforce soft tissue in plastic and reconstructive surgery of the nipple (Fig. 1). Like dermis or fascia, SIS is composed of fibrillar collagens, glycosaminoglycans, and adhesive glycoproteins, which serve as a scaffold into which cells can migrate and multiply.11 Once implanted, the NRC material allows cells to migrate into the device and form an organized extracellular matrix through the deposition of collagen and other proteins while acting as a biomaterial stent over which skin flaps can be created to achieve aesthetic nipple projection.
Fig. 1.

Biodesign NRC. Cylinders have a length of either 1.0 or 1.5 cm and a diameter of either 0.7 or 1.0 cm. All sizes can be trimmed before implantation.
PATIENTS AND METHODS
This study was designed as a prospective, nonblinded, multicenter, single-arm study to examine the use of the Biodesign NRC during reconstruction of the nipple after mastectomy. It was conducted according to international standards of Good Clinical Practice (ISO 14155 and International Conference on Harmonization guidelines) and additional institutional research policies and procedures. The study protocol and informed consent statements were reviewed and approved by either an independent institutional review board (IRB) or each location’s governing IRB. All patients were consented before enrollment. The rights, safety, and well-being of study subjects were protected in accordance with the ethical principles laid down in the Declaration of Helsinki. As required by U.S. law, this study was listed at www.ClinicalTrials.gov and assigned #NCT01216319, listed on October 5, 2010.
Adult patients with a history of breast cancer, having previously completed either unilateral or bilateral breast removal and reconstruction, were consented to participate. Patients with a history of radiation to the affected breast within the last 3 months and patients who had received chemotherapy within the past 4 weeks were excluded. Patient demographics, comorbidities, and relevant history, including the type of breast reconstruction, were recorded. At the time of nipple reconstruction, the size of the NRC implant was selected based on the patient’s aesthetic preference and the size of the contralateral nipple. If a contralateral nipple was absent, the overall size of the reconstructed breast, the presence or absence of a well-vascularized skin flap, and/or the patient’s desired final appearance were considered when determining the cylinder length and diameter, allowing for some shrinkage following implant.
The NRC implantation technique was performed as follows. (See figure, Supplemental Digital Content 1, which depicts schematically the standardized surgical procedure used in the study, http://links.lww.com/PRSGO/A238.) The position of the nipple was determined with the patient seated in a relaxed position, and the skin was marked with a surgical marker to guide the creation of the skin flap. Breast tissue flaps were raised at the superficial subcutaneous level to preserve the subdermal plexus using either a C–V or S-flap technique, using a specially designed template provided in the NRC kit. The flaps were formed into an appropriately sized silo to create the appearance of a breast nipple. The NRC was allowed to rehydrate for approximately 10 seconds immediately before it was inserted into the silo formed from the skin flap so as to bolster and maintain flap projection. Care was taken to ensure that an adequate blood supply was projected into the skin flap and reached the device. The cylinder was then secured into place with a combination of 3-0 vicryl and 4-0 monocryl (Ethicon, Somerville, N.J.) sutures at the base of the nipple reconstruction to prevent migration of the cylinder into the subcutaneous region under the flaps. After reconstruction, incisions were closed with a combination of inverted dermal 3-0 vicryl sutures and simple interrupted 4-0 monocryl sutures. Baseline projection measurements were taken directly on the reconstructed nipple, and reconstructed nipples were protected using a nipple shield for up to 4 weeks after surgery. Areolar tattooing was allowed according to individual patient preference but was discouraged until after the nipple reconstruction had fully healed.
Photographs of reconstructed nipples were taken at 1 week, 1 month, 3 months, 6 months, and 12 months after reconstruction (Fig. 2). Nipple projection was measured directly on the patient at the time of each follow-up examination, and compared with baseline. A questionnaire was developed to assess the level of overall patient satisfaction with the cosmetic results and patient satisfaction with multiple aspects of the reconstructed nipple (eg, size, position, color, softness, symmetry, sensation, and overall appearance) because no validated questionnaire specific to nipple reconstruction is available. (See survey, Supplement Digital Content 2, which depicts the satisfaction questionnaire, http://links.lww.com/PRSGO/A238.) This questionnaire was completed by the patient at 1, 3, 6, and 12 months after reconstruction; for patients undergoing bilateral procedures, a questionnaire was completed for each nipple at each time point.
Fig. 2.
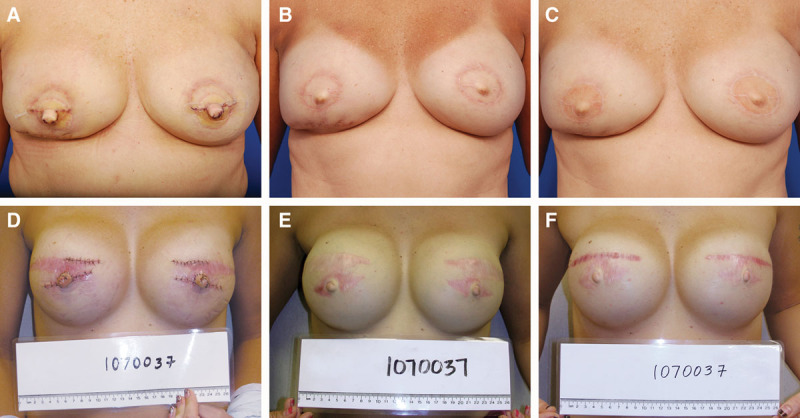
Representative photographs of 2 patients at 1 week after surgery (A, D), 6 months postoperative (B, E), and at the final follow-up visit 12 months after NRC placement (C, F).
Statistical Analysis
Study data were collected and entered into a study database by a contract research organization (MED Institute, West Lafayette, Ind.) using quality-control procedures. A quality-assurance check of the database datasets versus the case report forms was performed. All statistical analyses were performed with SAS software (version 9.3 for Windows; SAS Inc, Cary, N.C.) on the intent-to-treat population. Continuous variables were reported as means, standard deviations, and ranges. Categorical variables were reported as percent. Logistic and mixed linear models were used to identify predictors of nipple projection at 12 months. A mixed linear model with repeated measures was used to assess differences in projection maintenance over time.
RESULTS
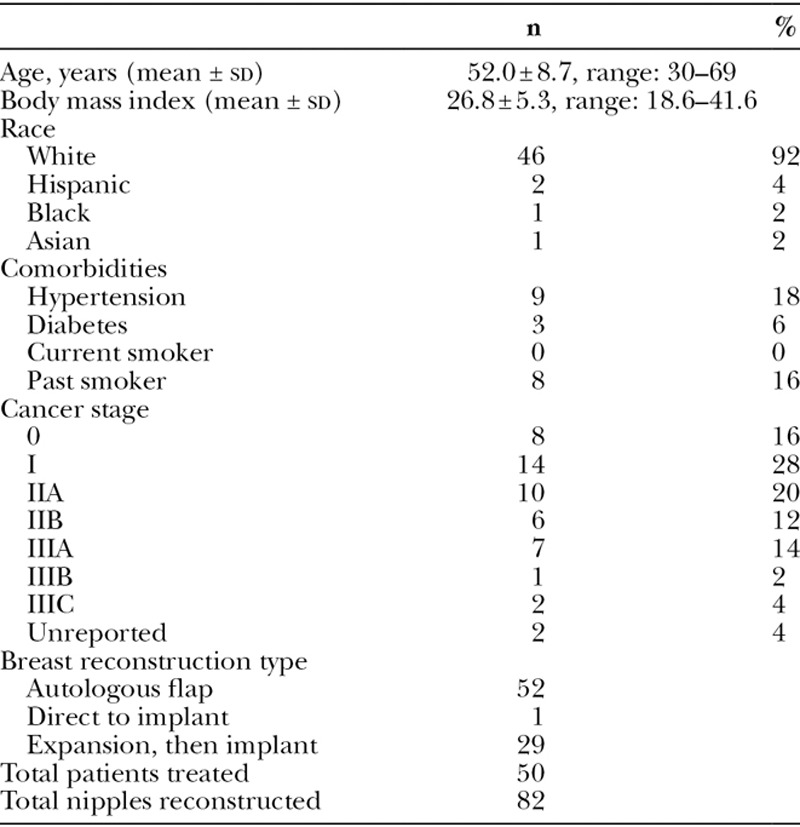
A total of 82 nipple reconstructions were performed in 50 patients between September 2011 and December 2012 (Table 1), and 46 patients were available for their final study visit at 12 months. Two patients were lost to follow-up and 2 patients were removed from the study early because of recurrence of their cancer, requiring additional surgery and chemotherapy. Although men were not excluded from participation if they met the eligibility criteria, all patients in this study were women. Mean patient age was 52.0 years; mean body mass index was 26.8. The majority of patients classified themselves as of white descent. Nine patients (18%) reported a hypertension diagnosis; there was 1 Type I diabetic and 2 Type II diabetics. A total of 8 patients (16%) reported a previous smoking history, although none of the patients were smokers at the time of nipple reconstruction. Furthermore, none of the patients reported a history of radiation to the affected nipple within the last 3 months. Of the total number of reconstructions performed, modified S-flaps were created in 6 nipples (7.3%), whereas the remaining 76 nipples (92.7%) were reconstructed using a C–V flap technique.
Table 1.
Patient Demographics
Mean nipple projection 1 week after surgery was 10.5 mm (range: 6–16 mm). Flaps were oversized an average of 19% at surgery to allow for placement of the cylinder and to prevent tension that could lead to flap necrosis, cylinder extrusion, or wound complications. At 6 months, mean projection was 4.1 ± 1.6 mm (range: 1–8 mm), and at 12 months, mean projection was 3.8 ± 1.5 mm (range: 0–8 mm). A plot of projection over time is presented in Figure 3. The maintenance of nipple projection is the percentage of projection at 1 year in relation to the projection immediately after the reconstruction. The average difference in maintenance of nipple projection from 6 to 12 months was 2.7%. The mixed linear model with repeated measures showed significant decreases in projection maintenance from 1 to 3 months (P < 0.0001) and from 3 to 6 months (P < 0.0001). However, there was not a significant change in projection maintenance from 6 to 12 months (P = 0.16). Nipples in which the cylinder extruded after surgery (n = 3) were excluded from all projection measurements to provide an accurate picture of the maintenance of nipple projection when the cylinder remains in place. Of importance, covariate models found no significant relationship between the extent of projection loss and either the type of breast reconstruction or removal of the nipple shield at 1 month after procedure.
Fig. 3.
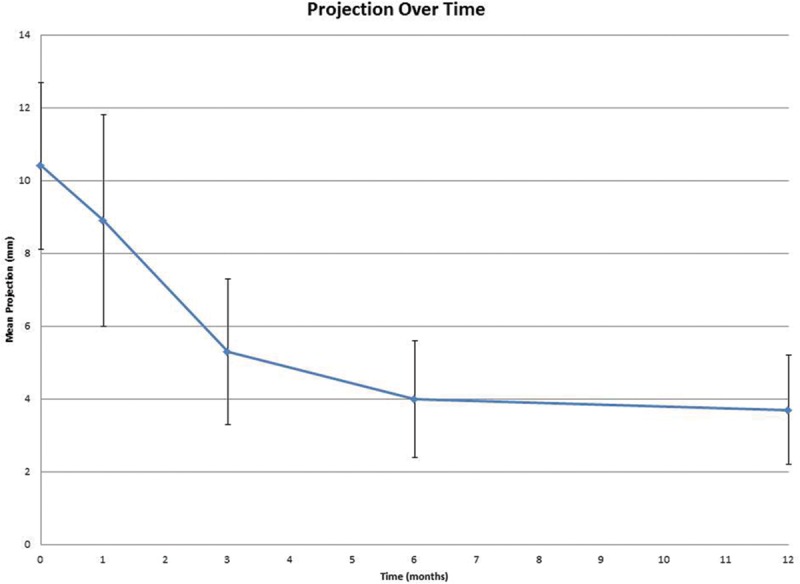
Nipple projection as a function of time.
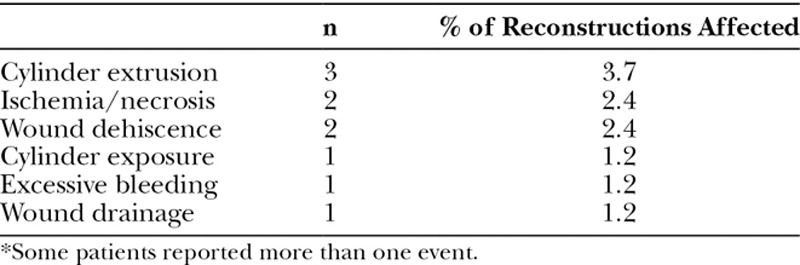
There were no intraoperative adverse events reported. Related postoperative adverse events occurred in 7 patients (14.0%) and in 8 reconstructions (9.8%). These adverse events are presented in Table 2. In addition to these events, 2 patients had recurrence of malignant cancer during the follow-up period, one patient had an unrelated adverse event requiring breast implant revision, one patient complained of an allergic reaction to topical antibiotic, and one patient opted to have cosmetic surgery to remove excess scar tissue related to her mastectomy.
Table 2.
Postoperative Adverse Events*
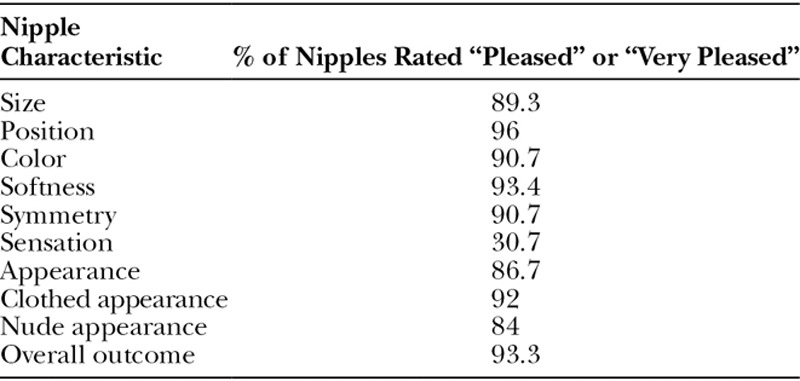
Patient-reported satisfaction results for each reconstructed nipple are presented in Table 3. Of patients completing the satisfaction questionnaire at 12 months, they rated 70/75 (93.3%) nipple reconstructions as being “pleased” or “very pleased” with the overall reconstruction. On the individual aspects of the reconstructed nipple, patients were “pleased” or “very pleased” with nipple: size 67/75 (89.3%); position 72/75 (96%); color 68/75 (90.7%); softness 70/75 (93.4%); symmetry 68/75 (90.7%); sensation 23/75 (30.7%); and appearance 65/75 (86.7%). Patients were pleased or very pleased with the clothed appearance of the reconstructed nipple in 69/75 (92%) and with the nude appearance of the reconstructed nipple in 63/75 (84%) responses, but only 25/46 (54.3%) reported that the reconstruction contributed significantly to their sex life. Overall, 45/46 (97.8%) patients would recommend nipple reconstruction to other women.
Table 3.
Patient Satisfaction at 12 Months
DISCUSSION
Maintenance of nipple projection has been reported to be as little as 30% after reconstruction, with significant flattening occurring in the first 3 months before eventually stabilizing.6,12 We believed that the addition of a biomaterial stent, in this case the Biodesign NRC, may fill the dead space present beneath the skin when flaps are raised, prevent scar contraction, and lead to a better long-term aesthetic result. Although long-term projection appeared to stabilize over time, maintenance of projection was only 37.3% at 1 year, which is slightly less than the approximately 50% reported at 6 months by Tierney et al9 when using the NRC and also slightly less than the 47% reported by Garramone and Lam10 when human acellular dermis was used along with tissue expanders. We further thought that breast reconstruction with an expander and implant would provide a solid foundation for the NRC, whereas breast reconstruction using flaps would not provide as solid of a foundation, resulting in the NRC sinking into the breast tissue and leading to decreased projection over time. However, statistical analyses were unable to detect a significant correlation between projection and the type of breast reconstruction that had been performed.
The time course of projection loss could be related to the known remodeling characteristics of the Biodesign implant or to the fact that we enrolled patients with a relatively recent history of radiation to the breast. Of note, radiation has been reported to impair wound healing for months to years after treatment is given.13 Thus, it may be possible to improve results if patients were selected more stringently. Alternatively, the SIS material used in the NRC has an established time frame of remodeling, which in the abdominal wall has been demonstrated to occur within 6 to 9 months.14,15 This natural tissue remodeling results in a nipple that retains a natural texture with adequate projection of 3 to 5 mm in the nipple area that becomes stable over time. This study demonstrated that the extent of projection loss changes minimally between 6 and 12 months, supporting this hypothesis, and suggests that 6-month projection may be predictive of longer-term projection for patients.
This study has several limitations, the least of which include the associated out-of-pocket costs of an elective, cosmetic procedure using an off-the-shelf device. The patient population in this study was generally homogenous, consisting of mostly white, nondiabetic, and nonsmokers. Therefore, these results may not be generalizable to the broader patient population that includes women of varying ethnicities and comorbidities. Additionally, because the majority of reconstructions were performed using C–V flaps, it is not possible to predict long-term outcomes if different flap techniques are used. Similarly, the absence of a control group limits the generalizability of the results, allowing comparisons to be made only to historical literature reports. Even though these are limitations of this study, this study is important because it is the first multicenter study on this device and demonstrates the amount of projection loss that can be expected when the NRC is used to reconstruct the nipple. The extent of projection observed at 12 months postimplant provides valuable information to surgeons to help refine their techniques and strategies to obtain an optimal aesthetic result for patients. Surgeons can use this information to tailor each nipple reconstruction more closely to the patient’s final desired level of projection, and patient expectations can be set more accurately before the procedure.
This study also demonstrated that the placement of the NRC can be performed safely with few postoperative complications. The most common complication, cylinder extrusion, occurred in 3 of the 82 nipples, yielding an extrusion rate of 3.7%. This extrusion rate is similar to that reported elsewhere9 and would be expected for any type of implanted graft. Other complications were typical of nipple flap reconstruction regardless of the type of implanted graft and included flap ischemia and necrosis, wound complications, and unexpected bleeding after the procedure. What is important to note in this study, however, is that in all patients experiencing the typical adverse events of cylinder exposure, localized flap necrosis, and wound dehiscence, only one of these adverse events led to eventual cylinder extrusion, and in none of them was device removal required. It is likely that the inherent remodeling characteristics of the graft, including its native composition and ability to support rapid angiogenesis from adjacent vascularized tissue structures, prevented long-term infectious results that would have necessitated device removal.16
Selecting the properly sized flap can affect outcome of the procedure and is a key reason that complications can occur. For example, small flaps may not leave sufficient space for the NRC, resulting in increased suture line tension and device exposure or extrusion. However, flaps need to be wrapped securely around the cylinder to promote incorporation of the device. Flaps that are too long may have decreased vascularization at the tips, leading to tissue necrosis. This can be avoided by carefully trimming the flap ends to proper size before wrapping them around the NRC. Additionally, if the flap has a thick layer of fat, limited or careful trimming away of that fat may increase contact between the NRC and skin tissue to promote device incorporation.
Aside from patient safety, perhaps the most important measure of a successful nipple reconstruction is patient satisfaction. The primary goal of breast and nipple reconstruction is to ease the emotional and psychological burden of mastectomy for the patient, so patient satisfaction with the aesthetic outcome of the procedure is critical to considering the procedure a success. In this study, we asked patients about their satisfaction with many parameters of their reconstructed nipples, including overall appearance, symmetry, color, softness, sensation, nude appearance, clothed appearance, and size. The vast majority of patients (93%) were “pleased” or “very pleased” overall, in sharp contrast to the satisfaction rates of 16% previously reported in other series,2,7 demonstrating that patient satisfaction depends more on the total aesthetic result of the reconstruction than on the level of sustained projection alone. The psychological and emotional benefit that comes from completing breast and nipple reconstruction with the NRC after recovery from breast cancer and mastectomy is seen in the patient satisfaction results obtained.
Supplementary Material
Footnotes
Supported by Cook Biotech Incorporated, 1425 Innovation Place, West Lafayette, Ind. All institutions received compensation and devices from the study sponsor to support the research.
Disclosure: JPH is an employee of Cook Biotech Incorporated. VAM is an employee of MED Institute, Inc., a Cook Group Company. HK has received compensation as a medical advisor to Cook Medical. Neither of the other authors has any financial disclosures. This study was supported by Cook Biotech Incorporated. The Article Processing Charge was paid for by Cook Biotech Incorporated.
Supplemental digital content is available for this article. Clickable URL citations appear in the text.
REFERENCES
- 1.Evans KK, Rasko Y, Lenert J, et al. The use of calcium hydroxylapatite for nipple projection after failed nipple-areolar reconstruction: early results. Ann Plast Surg. 2005;55:25–9. doi: 10.1097/01.sap.0000168370.81333.97. [DOI] [PubMed] [Google Scholar]
- 2.Jabor MA, Shayani P, Collins DR, Jr, et al. Nipple-areola reconstruction: satisfaction and clinical determinants. Plast Reconstr Surg. 2002;110:457–63. doi: 10.1097/00006534-200208000-00013. [DOI] [PubMed] [Google Scholar]
- 3.Wong RK, Wichterman L, Parson SD. Skin sparing nipple reconstruction with polytetrafluoroethylene implant. Ann Plast Surg. 2008;61:256–258. doi: 10.1097/SAP.0b013e31815d5bfa. [DOI] [PubMed] [Google Scholar]
- 4.Guerra AB, Khoobehi K, Metzinger SE, et al. New technique for nipple areola reconstruction: arrow flap and rib cartilage graft for long-lasting nipple projection. Ann Plast Surg. 2003;50:31–37. doi: 10.1097/00000637-200301000-00006. [DOI] [PubMed] [Google Scholar]
- 5.Norton S, Akhavani MA, Kang N. The ‘Hamburger’ technique for harvesting cartilage grafts in nipple reconstruction. J Plast Reconstr Aesthet Surg. 2007;60:957–959. doi: 10.1016/j.bjps.2005.11.047. [DOI] [PubMed] [Google Scholar]
- 6.Chia HL, Wong M, Tan BK. Nipple reconstruction with rolled dermal graft support. Arch Plast Surg. 2014;41:158–162. doi: 10.5999/aps.2014.41.2.158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nahabedian MY. Nipple reconstruction. Clin Plast Surg. 2007;34:131–7. doi: 10.1016/j.cps.2006.11.009. [DOI] [PubMed] [Google Scholar]
- 8.Bernard RW, Beran SJ. Autologous fat graft in nipple reconstruction. Plast Reconstr Surg. 2003;112:964–968. doi: 10.1097/01.PRS.0000076245.12249.BE. [DOI] [PubMed] [Google Scholar]
- 9.Tierney BP, Hodde JP, Changkuon DI. Biologic collagen cylinder with skate flap technique for nipple reconstruction. Plast Surg Int. 2014;2014:194087. doi: 10.1155/2014/194087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Garramone CE, Lam B. Use of AlloDerm in primary nipple reconstruction to improve long-term nipple projection. Plast Reconstr Surg. 2007;119:1663–1668. doi: 10.1097/01.prs.0000258831.38615.80. [DOI] [PubMed] [Google Scholar]
- 11.Teodori L, Costa A, Marzio R, et al. Native extracellular matrix: a new scaffolding platform for repair of damaged muscle. Front Physiol. 2014;5:218. doi: 10.3389/fphys.2014.00218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Shestak KC, Gabriel A, Landecker A, et al. Assessment of long-term nipple projection: a comparison of three techniques. Plast Reconstr Surg. 2002;110:780–786. doi: 10.1097/00006534-200209010-00010. [DOI] [PubMed] [Google Scholar]
- 13.Mathes SJ, Alexander J. Radiation injury. Surg Oncol Clin N Am. 1996;5:809–824. [PubMed] [Google Scholar]
- 14.Nguyen KP, Zotos V, Hsueh EC. Long-term outcome of biologic graft: a case report. J Med Case Rep. 2014;8:255. doi: 10.1186/1752-1947-8-255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Badylak S, Kokini K, Tullius B, et al. Morphologic study of small intestinal submucosa as a body wall repair device. J Surg Res. 2002;103:190–202. doi: 10.1006/jsre.2001.6349. [DOI] [PubMed] [Google Scholar]
- 16.Hodde JP. Extracellular matrix as a bioactive material for soft tissue reconstruction. ANZ J Surg. 2006;76:1096–1100. doi: 10.1111/j.1445-2197.2006.03948.x. [DOI] [PubMed] [Google Scholar]


