Abstract
Background:
Le Fort I osteotomy imparts significant changes to the nasolabial region. Past studies have relied on 2-dimensional data and have not delineated differences among various Le Fort I subtypes. The purpose of this study is to 3-dimensionally analyze Le Fort I–induced nasal and lip changes comparing advancement alone versus widening alone [surgically assisted maxillary expansion (SAME)] versus advancement and widening. We hypothesize that the combination of maxillary advancement with widening will result in the most profound changes.
Methods:
A retrospective cohort study was performed. Included Le Fort I patients were grouped as: (1) nonsegmental straight advancement, (2) widening without advancement, and (3) segmental advancement and widening. Pre- and postoperative 3-dimensional photogrammetry (Canfield) were analyzed. Anthropometric landmarks were placed and measured by 2 independent observers. Statistics involved both paired and unpaired t tests (significance = P < 0.05).
Results:
One hundred eight photogrammetric data sets were analyzed, including 46 single-piece, 26 SAME, and 36 segmental. Significant postoperative nasal changes were observed within each intragroup analysis. The most dramatic changes were seen after segmental Le Fort I with advancement and widening, which included alar base width, alar width, nostril width, and soft triangle angle, all P < 0.05.
Conclusions:
Le Fort I osteotomy results in significant alteration of the nasolabial morphology. This is the first study to 3-dimensionally analyze nasal changes that occur comparing maxillary advancement alone versus widening alone (SAME) versus advancement with widening. These objective data permit improved patient counseling and surgical planning.
The most significant soft tissue changes after maxillary orthognathic surgery occur within the nasolabial envelope. To effectively guide treatment and direct patient expectations, it is critical to understand and predict these soft tissue changes. Previous literature has attempted to assess postsurgical soft tissue changes after orthognathic surgery through the use of 2-dimensional (2D) analysis with radiologic superimposition.1–19 However, high resolution of the 3-dimensional (3D) nasolabial complexity was not permitted using 2D methods. Three-dimensional predictions were introduced in the 1990s.6–8,20,21 However, these were based on computed tomography (CT) soft tissue, which proved inaccurate.20,21 The recent advent of 3D photogrammetry has enabled objective soft tissue surface analysis.22 Three-dimensional photogrammetric analysis has been recently applied to nasolabial changes after orthognathic surgery.23–25 However, past studies have either examined small cohorts or emphasized changes after a single-piece Le Fort advancement alone. To our knowledge, there are no studies comparing nasolabial change after different subcategories of Le Fort I movements. In particular, the impact of maxillary advancement, maxillary widening, and a combination of advancement and widening has not been directly compared. The purpose of this study was to 3D describe the nasal changes after single-piece Le Fort I advancement, surgically assisted maxillary expansion (SAME) alone, and segmentally Le Fort I advancement with widening. We hypothesize that concurrent advancement with widening will have the most profound influence on the nasolabial region.
MATERIALS AND METHODS
Subjects
This retrospective analysis was performed in concordance with the Yale University Institutional Review Board (protocol number: HIC 1101007932). Patients who underwent single-piece Le Fort I advancement, SAME, and segmental Le Fort I with advancement and widening performed by a single surgeon were included. Exclusion criteria were superior or inferior positioning of the maxilla and previous nasolabial and palatal or midfacial surgery. Demographic information was tabulated, including patients’ age and sex, amount of maxillary advancement and expansion, and follow-up period were documented. Pre- and postoperatively, all subjects were assessed using a 3D photogrammetric imaging technique. The postoperative interval was at least 3 months to exclude any bias due to soft tissue swelling or hematoma.
Imaging and Data Processing
The 3D photogrammetric data were acquired under standard lighting using the 3D VECTRA photosystem (Canfield, Fairfield, N.J.). System calibration was performed before every capture process. Natural head position (Frankfurt horizontal line parallel to the floor) was chosen for data acquisition. Data sets were saved and calculated into a 3D model. Further data processing was performed using the imaging software (Mirror, Canfield, Fairfield, N.J.). Validity and reliability of the 3D photogrammetric tool for anthropometric measurements were confirmed in previous studies.23,24,26,27
Two blinded observers indicated the landmarks on each facial soft tissue image (Tables 1 and 2; Fig. 1). The zoom and rotation tools were used to correctly identify and set the landmarks on the 3D surface. It should be noted that there were no significant differences (P > 0.05) between the left and the right side for any group for the sill width, nostril height, nostril width, soft tissue triangle, and lateral alar triangle; therefore, the average of both sides was used for comparing postoperative changes. To evaluate postoperative soft tissue changes, a paired 2-sample t test was used. An α-level of ≤0.05 indicated a significant difference in values.
Table 1.
Landmarks Used for 3D Nasolabial Soft Tissue Assessment
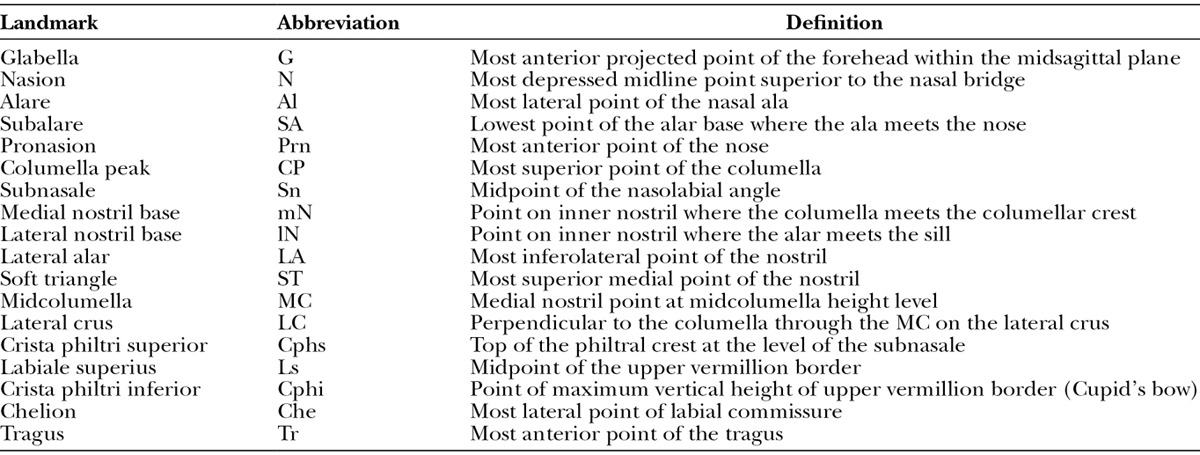
Table 2.
Parameters (Direct Distances and Angles) Used for 3D Nasolabial Soft Tissue Assessment
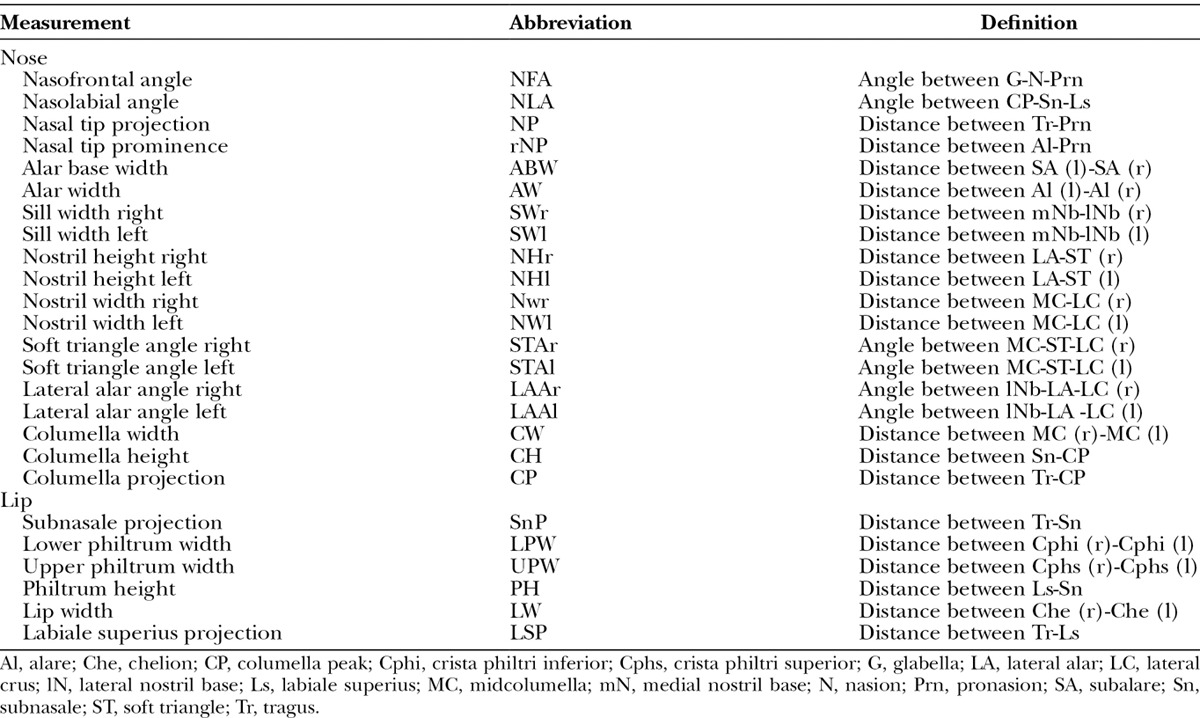
Fig. 1.
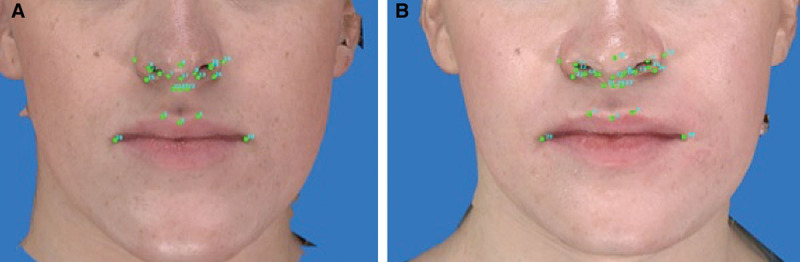
Overview of nasolabial landmarks for pre- (A) and postoperative (B) 3D photometric analysis.
RESULTS
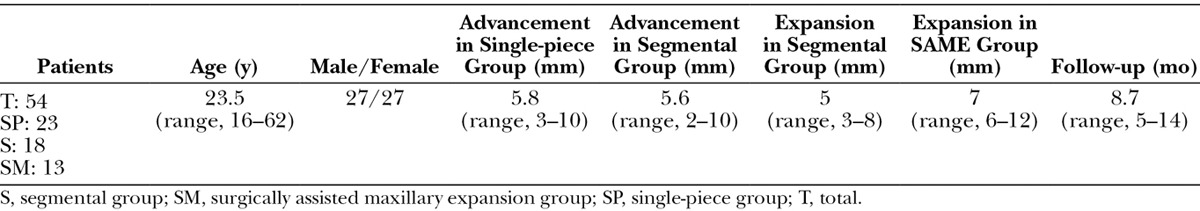
One hundred eight 3D photogrammetric data sets were included (54 pre- and postoperative 3D photogrammetric analysis). Male/female ratio was 1.0, with a mean age of 23.5 years. No significant difference was found between male/female ratio and mean age among the groups. Also, no significant changes existed among the groups with regard to soft tissue closure, as a standard alar cinch and V-Y closure was performed for each patient to control the alar base and the upper lip respectfully. Postoperative images were analyzed from an average of 8.7 months postoperatively. Mean maxillary advancement for the single-piece Le Fort group was 5.8 (± 1.8) mm. Mean maxillary advancement and mean transverse expansion for the segmental groups were 5.6 (± 2.3) mm and 5 (± 1.2) mm, respectively. Mean transverse expansion for the SAME group was 7 (± 2.1) mm. There was no statistically significant difference in the amount of advancement between the single-piece and segmental groups, but there was a statistically significant difference in the amount of expansion between the segmental and the SAME group, with more expansion after SAME (Table 3).
Table 3.
Demographics
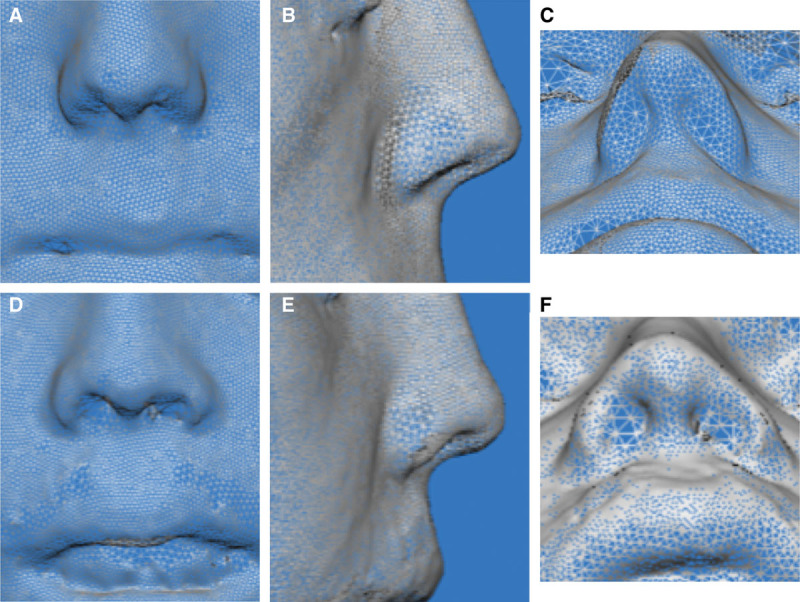
Pre- and postoperative measurements for all 3 groups were recorded for all nasolabial parameters along with P values obtained using a 2-sample paired t test for each parameter (Tables 4–6). Figures 2, 3, and 4 show the postoperative nasolabial changes for all 3 groups using a mesh 3D photometric overlay.
Table 4.
Anthropometric Evaluation Before and After Single-piece Maxillary Advancement (n = 23)
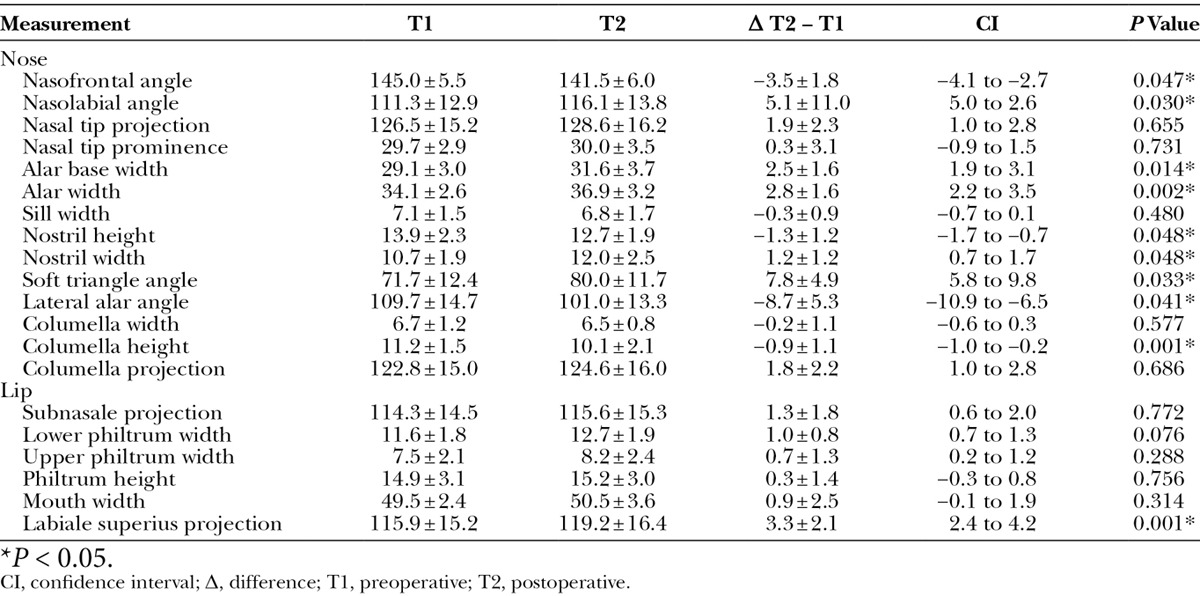
Fig. 2.
Overview of nasolabial landmarks for pre- (A, B, C) and postoperative (D, E, F) 3D photometric analysis (mesh) for single-piece maxillary advancement.
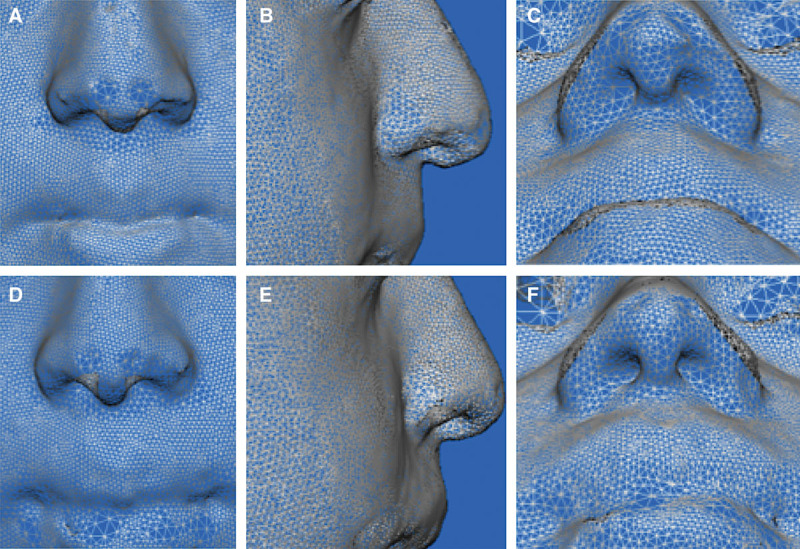
Fig. 3.
Overview of nasolabial landmarks for pre- (A, B, C) and postoperative (D, E, F) 3D photometric analysis (mesh) for surgically assisted maxillary expansion.
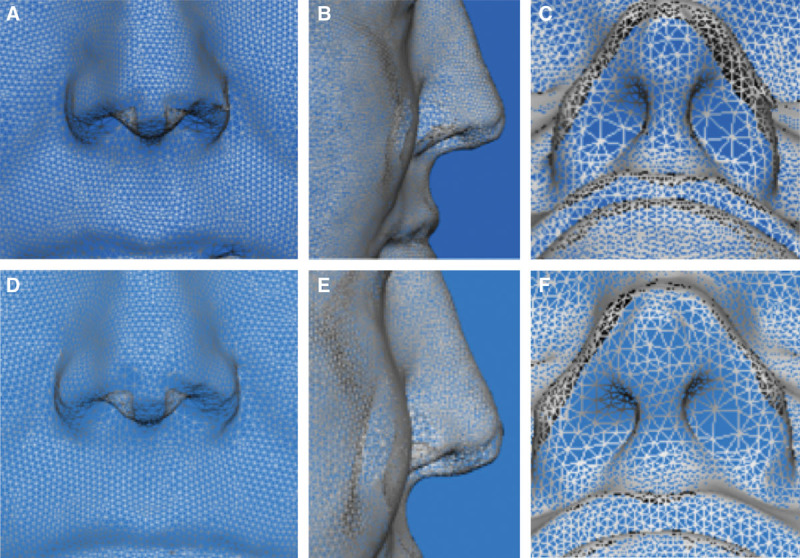
Fig. 4.
Overview of nasolabial landmarks for pre- (A, B, C) and postoperative (D, E, F) 3D photometric analysis (mesh) for segmental maxillary advancement and widening.
The nasolabial response after single-piece Le Fort I with advancement only showed a statistically significant decrease in nasofrontal angle, nostril height, columella height, and lateral alar angle. However, the following nasolabial parameters increased after single-piece Le Fort I advancement: nasolabial angle, nasal tip prominence, alar base width, alar width, nostril width, soft triangle angle, columella projection, and upper lip projection (labiale superius projection) (Table 4).
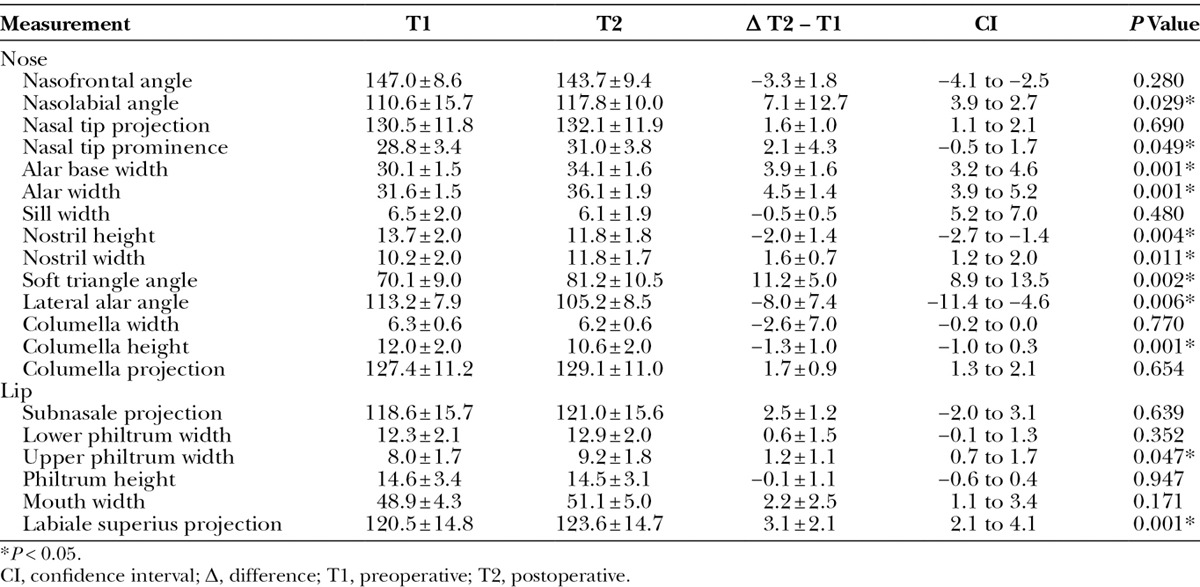
After SAME (widening only) group, the only statistically significant nasolabial change was seen with an increase in alar base width (Table 5). The nasolabial response after segmental Le Fort I with advancement and widening showed a statistically significant decrease in nostril height, columella height, and lateral alar angle. However, the following nasolabial parameters increased after segmental Le Fort I with advancement and widening: nasolabial angle, nasal tip prominence, alar base width, alar width, nostril width, soft triangle angle, columella projection, upper philtrum width, and upper lip projection (labiale superius projection) (Table 6).
Table 5.
Anthropometric Evaluation Before and After Surgically Assisted Maxillary Expansion
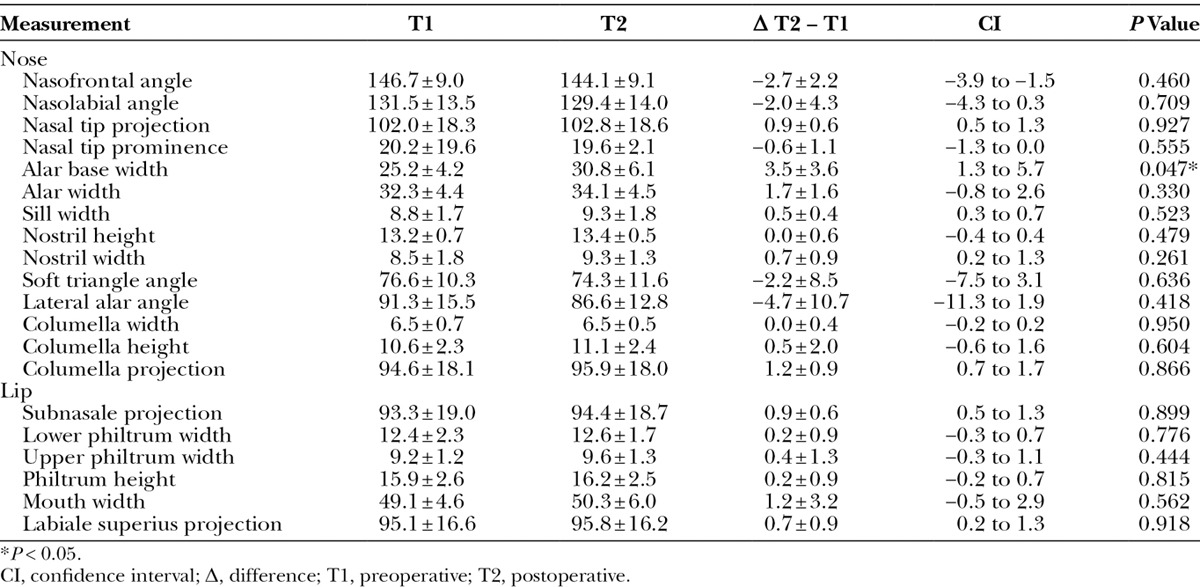
Table 6.
Anthropometric Evaluation Before and After Segmental Maxillary Advancement and Widening
Cross-group analysis using a 2-sample unpaired t test was performed for parameters in which more than 1 group showed statistically significant changes. This analysis revealed most significant (P < 0.05) changes in alar base width, alar width, nostril width, and soft tissue triangle in the segmental Le Fort group (alar base width: Δ3.9 ± 1.6, alar width: Δ4.5 ± 1.4, nostril height: Δ−2.0 ± 1.4, nostril width: Δ1.6 ± 0.7, soft triangle angle: Δ11.2 ± 5.0). Cross-group analysis also revealed most significant (P < 0.05) changes in the lateral alar angle to be in single-piece Le Fort I advancement (Δ−8.7 ± 5.3).
DISCUSSION
Treatment objectives for orthognathic surgery include both creation of a functional occlusion and optimizing facial aesthetics. Traditional emphasis has been placed on skeletal jaw movements to establish a proper occlusion, with requisite soft tissue changes being a secondary benefit. It is widely recognized, however, that maxillary repositioning alters the form and position of the upper lip and nose. In some instances, these morphologic changes are favorable and desirable. However, the nose and lip can be made less aesthetic after Le Fort I.1,2 To optimally use nasal changes after Le Fort I to enhance aesthetics, these predictable patterns of change should be objectively elucidated. Such understanding also will permit counseling and advance warning to the patient when detrimental nasolabial alterations are anticipated.
Most current understanding of Le Fort I–induced nasolabial changes is based on reports using 2D radiologic shadows, hindering complete morphometric understanding.1,2,9–12 In addition, a delineation of nasal changes following different subtypes or magnitudes of Le Fort I has not been performed. Three-dimensional photogrammetry has proven accurate in assessing nasal soft tissue morphology for single-piece Le Fort I.25 However, comparison of upper lip and nasal changes after multipiece segmental Le Fort I is not present in the literature. We know that both advancement and widening of the maxilla produce the requisite changes to the nose. The relative influence of each type of movement has not been compared. The aim of this study was to then (1) describe Le Fort 3D nasolabial changes, and (2) compare the impact of maxillary widening, advancement, and combination advancement/widening on the nose and upper lip position. Given the combination of advancement and widening, we expected the most profound nasal change in this group.
The data showed a significantly decreased nasofrontal angle, between 2 and 5 degrees, after a single-piece Le Fort I advancement, with no significant changes to the nasofrontal angle observed after segmental Le Fort I advancement or SAME. Nasofrontal angle changes seem to be independent of skeletal movements and have been shown to occur mainly as a result of freeing of the nasal septum during soft tissue degloving.28
We hypothesized that the greatest nasolabial changes in the frontal horizontal dimension would occur in the expansion groups (ie, SAME and segmental Le Fort I). A significant increase in alar base width was observed in all 3 groups. Nevertheless, the greatest postoperative increases in alar base width and alar width were observed after a segmental Le Fort I advancement.
Changes in nostril dimensions (including nostril height and nostril width) and in shape (including soft triangle angle and lateral alar angle) after segmental Le Fort I advancement seemed to display similar patterns as those of the single-piece Le Fort I advancement.
After both advancement alone and advancement with widening, the nostrils took on a more rounded shape, showing a height reduction and width increase, becoming more horizontal from the submental view. Nostril morphology after SAME also widened but more inconsistently. Perhaps this is related to unequal expansion from one side to the other. However, the greatest changes in all the aforementioned parameters occurred in the segmental Le Fort I advancement with widening group (ie, decrease in nostril height, increase in nostril width, decrease in soft triangle angle, and decrease in lateral alar angle). Although columella width remained relatively unchanged among all groups, columella height decreased among the single-piece and segmental groups, whereas columella projection increased in both groups. The nasolabial angle and nasal tip prominence increased within the single-piece and segmental groups. Increase in the upper philtrum width was only observed within the segmental group, whereas upper lip projection occurred within both the single-piece and the segmental groups. It should be noted, however, that while our data measured nasal tip projection relative to the measured distance from the tragus to pronasale, changes to the absolute value can be implied from the data we obtained regarding changes to the columella. The absolute change in nasal tip projection (from subnasale to pronasale) decreases after advancement and advancement with widening, which is supported by the fact that the columella height decreases and columella projection increases, thus leading to a “buckling” effect of the columella resulting in an absolute shortening of the nasal tip projection in relation to the upper lip.
In summary, our current study reveals that maxillary advancement has a significantly greater impact on postoperative nasolabial projection and transverse nasolabial dimensions than does maxillary widening alone. Combining both advancement and widening (segmental Le Fort) was shown to have the greatest impact on the nasolabial region. The sagittal advancement contributes greatest to these changes as SAME (which involves the largest magnitude of maxillary expansion only with no advancement) showed the least amount of nasolabial alteration postoperatively. It appears then that continuous widening seems to significantly reduce soft tissue adverse effects, whereas advancement seems to play a larger role in nasolabial changes than does widening. This is especially interesting given that the maxillary widening using SAME procedure is more pronounced within the anterior maxilla directly abutting the overlying soft tissues compared with the segmental maxillary osteotomy, which preferentially widens the posterior maxilla. It is for this reason, we believe, that single-piece Le Fort I advancement and multipiece Le Fort I advancement/widening have a similar overall effect on the nasolabial soft tissues. We hypothesize that the continuous, yet, large degree of distraction, especially within the anterior maxillary region, in combination with a stable columella width, is responsible for this phenomenon.
However, our current findings only represent a fraction of the wide variety of soft tissue changes resulting from orthognathic maxilla surgery. Individual anatomic structural differences and the variability in surgical osteotomies—including ramped versus parallel to the maxillary plane, with or without fracture of the lateral nasal wall or pterygomaxillary junction, 2 or multiple pieces, and more—considerably influence the 3D skeletal movements and the corresponding overlying soft tissues. In addition, soft tissue closure techniques (such as V-Y, alar base suture, and their various modifications) play an important role in the establishment or reconstruction of aesthetic facial proportions and dimensions after skeletal movement. More attention should be paid to that in the daily routine.
Only an in-depth understanding of the impact of orthognathic procedures on 3D nasal morphology allows an individually tailored treatment plan to achieve the best aesthetic results. Patient counseling and postoperative prediction planning will be considerably more reliable today and in the future by utilizing 3D analytical tools.
Given what we now know about postoperative nasolabial morphology after Le Fort I, we recommend placing special consideration on patients who present with unfavorable preoperative nasolabial parameters, such as an obtuse nasolabial angle, a prominent nasal tip, columella projection, and upper lip projection; a wide alar width, alar base, nostril width, and upper philtrum width; a narrow alar angle; and a short nostril height, upper lip length, and columella height. If such abnormalities exist preoperatively, it can be expected that they will change more dramatically after maxillary advancement or advancement with widening and may need to be addressed concurrently or later. The morphologic prediction and understanding gained from our 3D results allow proper counseling regarding the potential for improvement or worsening of the nasolabial form, with attention to individual Le Fort procedure subtypes.
CONCLUSIONS
Maxillary advancement with or without widening significantly influences nasolabial morphology greater than maxillary widening alone. Segmental Le Fort I with advancement and widening exhibits the greatest nasolabial change, whereas SAME has the least effect. These expected nasolabial alterations should be considered in treatment planning.
Footnotes
Disclosure: The authors have no financial interest to declare in relation to the content of this article. The Article Processing Charge was paid for by Yale Department of Surgery, Charles Ohse grant.
REFERENCES
- 1.Obwegeser HL. Principles in treatment planning of facial skeletal anomalies. Clin Plast Surg. 2007;34:585–587. doi: 10.1016/j.cps.2007.05.015. [DOI] [PubMed] [Google Scholar]
- 2.Obwegeser HL, Marentette LJ. Profile planning based on alterations in the positions of the bases of the facial thirds. J Oral Maxillofac Surg. 1986;44:302–311. doi: 10.1016/0278-2391(86)90081-9. [DOI] [PubMed] [Google Scholar]
- 3.Kahnberg KE. Transverse expansion of the maxilla using a multisegmentation technique. Scand J Plast Reconstr Surg Hand Surg. 2007;41:103–108. doi: 10.1080/02844310601159923. [DOI] [PubMed] [Google Scholar]
- 4.Kahnberg KE, Hagberg C. The approach to dentofacial skeletal deformities using a multisegmentation technique. Clin Plast Surg. 2007;34:477–484. doi: 10.1016/j.cps.2007.05.003. [DOI] [PubMed] [Google Scholar]
- 5.Vasudavan S, Jayaratne YSN, Padwa BL. Nasolabial soft tissue changes after Le Fort I advancement. J Oral Maxillofac Surg. 2012;70:e270–e277. doi: 10.1016/j.joms.2011.11.022. [DOI] [PubMed] [Google Scholar]
- 6.Dann JJ, III, Fonseca RJ, Bell WH. Soft tissue changes associated with total maxillary advancement: a preliminary study. J Oral Surg. 1976;34:19–23. [PubMed] [Google Scholar]
- 7.Lines PA, Steinhauser WW. Soft tissue changes in relationship of movement of hard structures in orthognathic surgery. J Oral Surg. 1974;32:891. [Google Scholar]
- 8.Burstone CJ, James RB, Legan H, et al. Cephalometrics for orthognathic surgery. J Oral Surg. 1978;36:269–277. [PubMed] [Google Scholar]
- 9.Rosen HM. Lip-nasal Is following Le Fort I osteotomy. Plast Reconstr Surg. 1988;81:171–182. doi: 10.1097/00006534-198802000-00005. [DOI] [PubMed] [Google Scholar]
- 10.Schendel SA, Williamson LW. Muscle reorientation following superior repositioning of the maxilla. J Oral Maxillofac Surg. 1983;41:235–240. doi: 10.1016/0278-2391(83)90265-3. [DOI] [PubMed] [Google Scholar]
- 11.Carlotti AE, Jr, Aschaffenburg PH, Schendel SA. Facial changes associated with surgical advancement of the lip and maxilla. J Oral Maxillofac Surg. 1986;44:593–596. doi: 10.1016/s0278-2391(86)80068-4. [DOI] [PubMed] [Google Scholar]
- 12.Mommaerts MY, Lippens F, Abeloos JV, et al. Nasal profile changes after maxillary impaction and advancement surgery. J Oral Maxillofac Surg. 2000;58:470–475. doi: 10.1016/s0278-2391(00)90002-8. discussion 475–476. [DOI] [PubMed] [Google Scholar]
- 13.Hack GA, de Mol van Otterloo JJ, Nanda R. Long-term stability and prediction of soft tissue changes after LeFort I surgery. Am J Orthod Dentofacial Orthop. 1993;104:544–555. doi: 10.1016/s0889-5406(05)80438-x. [DOI] [PubMed] [Google Scholar]
- 14.Mansour S, Burstone C, Legan H. An evaluation of soft-tissue changes resulting from Le Fort I maxillary surgery. Am J Orthod. 1983;84:37–47. doi: 10.1016/0002-9416(83)90146-x. [DOI] [PubMed] [Google Scholar]
- 15.Jensen AC, Sinclair PM, Wolford LM. Soft tissue changes associated with double jaw surgery. Am J Orthod Dentofacial Orthop. 1992;101:266–275. doi: 10.1016/0889-5406(92)70096-S. [DOI] [PubMed] [Google Scholar]
- 16.Legan HL, Burstone CJ. Soft tissue cephalometric analysis for orthognathic surgery. J Oral Surg. 1980;38:744–751. [PubMed] [Google Scholar]
- 17.Pospisil OA. Reliability and feasibility of prediction tracing in orthognathic surgery. J Craniomaxillofac Surg. 1987;15:79–83. doi: 10.1016/s1010-5182(87)80023-9. [DOI] [PubMed] [Google Scholar]
- 18.Carlotti AE, Jr, Aschaffenburg PH, Schendel SA. Facial changes associated with surgical advancement of the lip and maxilla. J Oral Maxillofac Surg. 1986;44:593–596. doi: 10.1016/s0278-2391(86)80068-4. [DOI] [PubMed] [Google Scholar]
- 19.Stella JP, Streater MR, Epker BN, et al. Predictability of upper soft tissue changes with maxillary advancement. J Oral Maxillofac Surg. 1989;47:697. doi: 10.1016/s0278-2391(89)80008-4. [DOI] [PubMed] [Google Scholar]
- 20.Altobelli DE, Kikinis R, Mulliken JB, et al. Computer-assisted three-dimensional planning in craniofacial surgery. Plast Reconstr Surg. 1993;92:576–585. discussion 586. [PubMed] [Google Scholar]
- 21.McCance AM, Moss JP, Fright WR, et al. A three dimensional analysis of soft and hard tissue changes following bimaxillary orthognathic surgery in skeletal III patients. Br J Oral Maxillofac Surg. 1992;30:305. doi: 10.1016/0266-4356(92)90180-q. [DOI] [PubMed] [Google Scholar]
- 22.3dMDface System. Available at: www.3dmd.com. Accessed November 6, 2007. [Google Scholar]
- 23.Metzler P, Geiger EJ, Chang CC, et al. Surgically assisted maxillary expansion imparts three-dimensional nasal change. J Oral Maxillofac Surg. 2014;72:2005–2014. doi: 10.1016/j.joms.2014.03.004. [DOI] [PubMed] [Google Scholar]
- 24.Metzler P, Geiger EJ, Chang CC, et al. Assessment of three-dimensional nasolabial response to Le Fort I advancement. J Plast Reconstr Aesthet Surg. 2014;67:756–763. doi: 10.1016/j.bjps.2014.03.023. [DOI] [PubMed] [Google Scholar]
- 25.Yamada T, Mishima K, Moritani N, et al. Nasolabial morphologic changes after a Le Fort I osteotomy: a three-dimensional anthropometric study. J Craniofac Surg. 2010;21:1089–1095. doi: 10.1097/SCS.0b013e3181e1e6ff. [DOI] [PubMed] [Google Scholar]
- 26.Metzler P, Bruegger LS, Kruse Gujer AL, et al. Craniofacial landmarks in young children: how reliable are measurements based on 3-dimensional imaging? J Craniofac Surg. 2012;23:1790–1795. doi: 10.1097/SCS.0b013e318270fa8f. [DOI] [PubMed] [Google Scholar]
- 27.Metzler P, Sun Y, Zemann W, et al. Validity of the 3D VECTRA photogrammetric surface imaging system for cranio-maxillofacial anthropometric measurements. Oral Maxillofac Surg. 2014;18:297–304. doi: 10.1007/s10006-013-0404-7. [DOI] [PubMed] [Google Scholar]
- 28.McFarlane RB, Frydman WL, McCabe SB, et al. Identification of nasal morphologic features that indicate susceptibility to nasal tip deflection with the LeFort I osteotomy. Am J Orthod Dentofacial Orthop. 1995;107:259–267. doi: 10.1016/s0889-5406(95)70141-9. [DOI] [PubMed] [Google Scholar]


