Summary:
Neurothekeomas are rare benign tumors commonly found on the head, neck, and upper extremities of women and younger individuals. They are thought to be of nerve sheath origin and usually present as painless, slow growing masses. We present a case of cellular neurothekeoma on the nasal ala of an 8-year-old girl with no previous history of trauma or piercings. Differential diagnosis, treatment options, and special considerations regarding potentially atypical characteristics are discussed.
Neurothekeomas are rare, benign cutaneous tumors of nerve sheath origin. They are more common in female and younger individuals. They usually present on the head and neck and in most cases are asymptomatic. The treatment is surgical removal and, given the location of these tumors, patients may be referred to a plastic surgeon for resection and/or reconstruction. There are only 13 cases of neurothekeomas in the head and neck region reported in the plastic surgery literature up to date, among which only 4 were located on the nose.
CASE PRESENTATION
An 8-year-old Hispanic girl presented with a slowly growing mass of her left nasal ala. The patient originally noticed the lesion 2 years before presentation. She denied drainage, bleeding, or pain. No previous history of trauma, insect bites, or scarring to the area was elicited.
On examination, the lesion was a firm, nonmobile, hypervascular red-colored papule measuring 8 × 5 × 5 mm (Fig. 1). The lesion extended past the alar rim into the hair-bearing part of her left nostril. No tenderness or visible pore was noted. No other lesions were identified, and examination of her neck and supraclavicular lymph nodes was unremarkable. The patient was otherwise healthy with a noncontributory family and social history.
Fig. 1.

Preoperative image of the lesion measuring 8 × 5 mm on the left ala.
Excisional biopsy was planned, and 1-mm margins were marked around the lesion creating an ellipse measuring 1.8 × 1 cm. The lesion was completely removed and sent for pathology. There was no involvement of the alar cartilage. Undermining was performed to achieve a tension-free closure (Fig. 2).
Fig. 2.

Immediate postoperative image after complete excision of the lesion.
The pathology report revealed a poorly circumscribed tumor with a lobular growth pattern in the reticular dermis and with extension to subcutaneous tissue. Margins were negative. The tumor composed of nests and fascicles of spindle and epithelioid cells with pale eosinophilic cytoplasm and vesicular nuclei in the background of dense collagen, consistent with benign cellular neurothekeoma (Fig. 3). Spindle and epithelioid cells were positive for microphthalmia transcription factor 1 and negative for S100, smooth muscle actin, and CKAE1/AE3. No cellular atypia was identified.
Fig. 3.
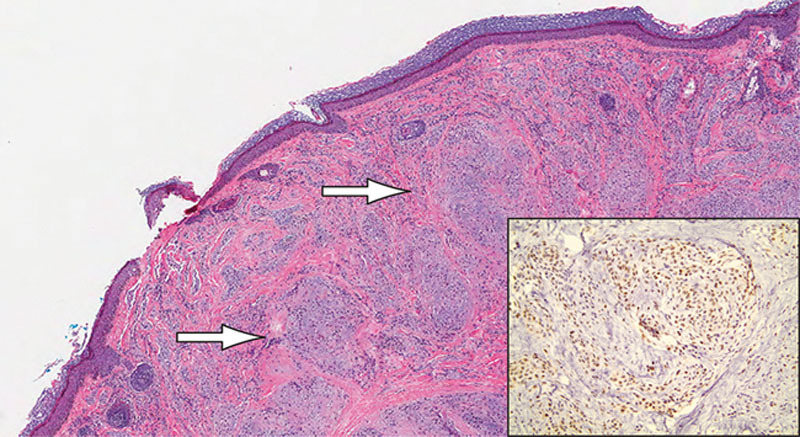
Histopathologic image of lesion. Low-power image (×4) stained with H&E showing nests of spindle and epithelioid cells not connected to the epidermis (arrows); right bottom corner showing high-power image (×20) stained for MITF.
The patient recovered without any complications and has had no evidence of recurrence 4 years postoperatively (Fig. 4).
Fig. 4.

Postoperative image 4 years after resection. No evidence of recurrence and excellent aesthetic outcome.
DISCUSSION
Neurothekeomas are poorly understood, rare, benign tumors of neural sheath origin. The first neurothekeoma was reported in the literature as a nerve sheath myxoma by Harkin and Reed1 in 1969. However, this type of tumor received its current definition as neurothekeoma in 1980 by Gallager and Helwig.2 The largest study of cellular neurothekeomas included 133 cases, 44 of which were in the head and neck region.3 Only 24 have been reported on the nose since 1995.
Neurothekeomas are found predominantly in young females and are commonly located on the head, neck, and upper extremities.3–5 Hornick and Fletcher3 studied 133 neurothekeoma cases and demonstrated that the mean age of presentation is 25 years. In the same study, 33% of the cases were found on the head and neck and 35% on the upper limb. The average size was around 1 cm; however, tumors up to 6 cm have been reported. In a different study of 292 cases, Papadopoulos et al4 showed that the incidence of head and neck lesions was higher in children (45.4%).
There are 3 identified pathologic types of neurothekeomas: cellular, myxoid, and mixed. Myxoid tumors are more rare and have higher mucin content than cellular variants.6,7 They are typically positive for NK1/C3 and negative for S100 protein, which differentiates them from melanocytic tumors.3,8,9 Busam et al8 outlined the features of atypical neurothekeomas. These include size greater than 5 cm, irregular borders, invasion into surrounding tissues and structures, and high mitotic rate. Despite their atypical characteristics, no evidence of recurrence or metastasis were reported.
Differential diagnosis included pyogenic granuloma, keloid, fibrous papule of the nose, angioma, adnexal tumor, hamartoma, melanocytic nevus, and basal cell carcinoma. A similar case was published by Wilson et al10; however, that patient had a history of piercing of her nose. Our patient had no history of trauma, insect bites, or any type of previous lesions in the area.
Treatment consists of surgical resection. There is no consensus on excision margin; however, a few millimeters of grossly negative margins and microscopic clear margins are thought to be sufficient. In tumors with aggressive characteristics, wider margins might be appropriate. Only few cases of recurrence have been reported; however, these lesions were all found to have positive margins.3 In our case, there has been no recurrence 4 years after resection.
SUMMARY
The plastic surgeon should be aware of this rare tumor given the common involvement of the face, neck, and upper extremities. Neurothekeomas can develop not only in areas of previous trauma but also in areas with completely healthy skin. Treatment consists of surgical resection. An incisional or shave biopsy could be considered to rule out atypia or aggressive features that would require wider resection margins to minimize the chances or recurrence.
PATIENT CONSENT
The patient provided written consent for the use of her image.
Footnotes
Disclosure: The authors have no financial interest to declare in relation to the content of this article. The Article Processing Charge was paid for by the authors.
REFERENCES
- 1.Harkin JC, Reed RJ. Atlas of Tumor Pathology. Washington, DC: Armed Forces Institutes of Pathology; 1969. Tumors of the peripheral nervous system. pp. 60–64. [Google Scholar]
- 2.Gallager RL, Helwig EB. Neurothekeoma–a benign cutaneous tumor of neural origin. Am J Clin Pathol. 1980;74:759–764. doi: 10.1093/ajcp/74.6.759. [DOI] [PubMed] [Google Scholar]
- 3.Hornick JL, Fletcher CD. Cellular neurothekeoma: detailed characterization in a series of 133 cases. Am J Surg Pathol. 2007;31:329–340. doi: 10.1097/01.pas.0000213360.03133.89. [DOI] [PubMed] [Google Scholar]
- 4.Papadopoulos EJ, Cohen PR, Hebert AA. Neurothekeoma: report of a case in an infant and review of the literature. J Am Acad Dermatol. 2004;50:129–134. doi: 10.1016/s0190-9622(03)00886-7. [DOI] [PubMed] [Google Scholar]
- 5.Fetsch JF, Laskin WB, Hallman JR, et al. Neurothekeoma: an analysis of 178 tumors with detailed immunohistochemical data and long-term patient follow-up information. Am J Surg Pathol. 2007;31:1103–1114. doi: 10.1097/PAS.0b013e31802d96af. [DOI] [PubMed] [Google Scholar]
- 6.Wang AR, May D, Bourne P, et al. PGP9.5: a marker for cellular neurothekeoma. Am J Surg Pathol. 1999;23:1401–1407. doi: 10.1097/00000478-199911000-00011. [DOI] [PubMed] [Google Scholar]
- 7.Angervall L, Kindblom LG, Haglid K. Dermal nerve sheath myxoma. A light and electron microscopic, histochemical and immunohistochemical study. Cancer. 1984;53:1752–1759. doi: 10.1002/1097-0142(19840415)53:8<1752::aid-cncr2820530823>3.0.co;2-2. [DOI] [PubMed] [Google Scholar]
- 8.Busam KJ, Mentzel T, Colpaert C, et al. Atypical or worrisome features in cellular neurothekeoma: a study of 10 cases. Am J Surg Pathol. 1998;22:1067–1072. doi: 10.1097/00000478-199809000-00004. [DOI] [PubMed] [Google Scholar]
- 9.Zelger BG, Steiner H, Kutzner H, et al. Cellular ‘neurothekeoma’: an epithelioid variant of dermatofibroma? Histopathology. 1998;32:414–422. doi: 10.1046/j.1365-2559.1998.00406.x. [DOI] [PubMed] [Google Scholar]
- 10.Wilson AD, Rigby H, Orlando A. Atypical cellular neurothekeoma–a diagnosis to be aware of. J Plast Reconstr Aesthet Surg. 2008;61:186–188. doi: 10.1016/j.bjps.2007.01.078. [DOI] [PubMed] [Google Scholar]


