Supplemental Digital Content is available in the text.
Abstract
Background:
A concealed penis is a condition where part of the penis is invisible below the surface of the prepubic skin. Dermolipectomy can correct this condition, although it involves a long abdominal crease incision, or infrapubic incision around the base of the penis, and a possibility for genital lymphedema. This study describes Shaeer’s technique, a minimally invasive method for revealing the concealed penis.
Methods:
A 1- to 2-cm-long incision was cut over the anterior superior iliac spine (ASIS) on either side. A long curved blunt forceps was inserted from one incision, down to the base of the penis and then up to the contralateral ASIS. A 5-mm wide nonabsorbable tape was picked up by the forceps from 1 incision and pulled through to emerge from the other. Pulling on the tape cephalad pulled the mons pubis and revealed the penis. The tape was sutured to the periosteum overlying the ASIS on either side. Patients were followed up for 18 months for penile length, complications, and overall satisfaction.
Results:
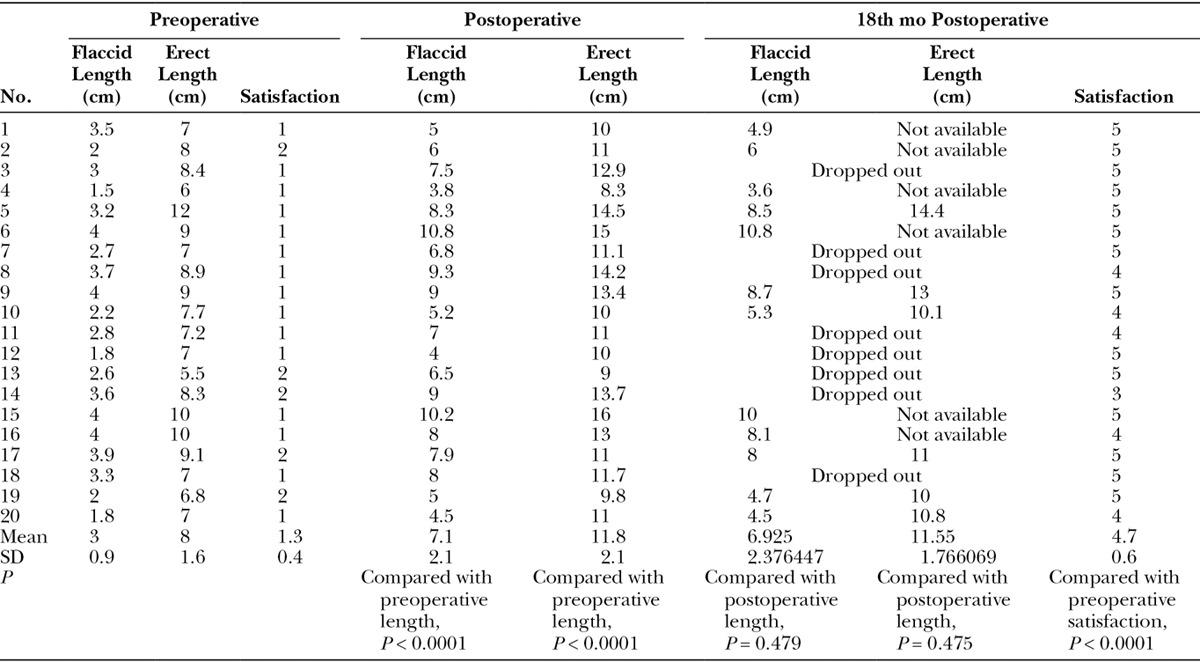
Twenty patients were operated upon. Preoperatively, flaccid visible length was 3 ± 0.9 cm, and erect visible length was 8 ± 4.6 cm. Postoperatively, the flaccid visible length was 7.1 ± 2.1 cm, with a 57.9% improvement in length (P < 0.0001). Erect visible length was 11.8 ± 2.1 cm, with a 32% improvement in length (P < 0.0001). Length gain was maintained for 18 months.
Conclusion:
Shaeer’s technique is a minimally invasive, short, and simple procedure for monsplasty and revealing the concealed penis.
Dissatisfaction with the length of the penis has a drastic impact on sexual well-being of a considerable subset of males and sexual life of many couples. It had been observed that 30% of males in the Middle East had concerns over genital size compared with 35.4% in United States and that this concern was a risk factor for erectile dysfunction.1–3 Concerns over genital size in males should be scrutinized, and couple education is of utmost importance because those concerns may—in many cases—be unjustified, with functional length being adequate while visible length remains the cause for cosmetic concerns. Genital size is not a single entity but is rather multifaceted. Length should be evaluated from the pubic bone to the tip of the penis (true length) and also from the pubic skin surface to tip (visible length), in both the flaccid and erect states, highlighting what is important from a functional viewpoint (true length) and what is not (visible length). Although some men with genital size concerns may be suffering anxiety over the issue, others have more profound distress. Penile dysmorphic disorder (PDD) refers to men in whom the size or shape of the penis is their main, if not their exclusive, preoccupation causing significant shame or handicap.4 With counseling, the former group with mere anxiety can possibly be convinced into accepting their body configuration and living in harmony with it. In contrast, those with PDD are a very difficult group to handle and may frequently require psychiatric help.
On the other hand, it is not uncommon that the genital size concerns are justified, whether due to a concealed but normally sized penis (buried/concealed penis) or due to an actual deficiency in length. The former can be due to a redundant suprapubic fat pad on account of obesity, severe or rapid weight loss ending up with skin redundancy, a hormonal disorder, abnormal fibrous bands retracting the penis,5 a redundant penoscrotal web,6 overzealous circumcision,7 poor attachment of skin to the base of the penis with poor definition of the penopubic junction (PPJ), iatrogenic complications, or even the aging process.8 The latter (an actually short penis) can be due to Peyronie’s disease, several hypospadias surgeries resulting in adhesions, scarring or a short neourethra, or an actual micropenis.
Focusing on cases with a concealed penis, patients should be reassured that the true length is normal despite a short visible length and that true length is what matters functionally. However, the condition may limit some sexual positions and may pose a problem if obesity is mutual in the couple. For aesthetic reasons, weight loss is an option. However, patients should be warned that they may still end up with a buried penis because of the wide skin surface area that is left behind and/or laxity of the adhesions/ligaments that define the PPJ resulting in redundancy. Patients undergoing bariatric surgery commonly end up with a thin waif in an oversized suit of skin, with consequent functional and aesthetic problems. It is interesting that a bariatric surgical procedure may result in demand and need for consequent plastic surgery procedures. It was estimated that 89.9% of patients who underwent a gastric bypass considered plastic surgery for removal of excess skin.9 The same applies for liposuction, which will remove some of the suprapubic fat but will fail to remove the redundant skin or define the PPJ. In such cases, surgical removal of the SFP and excess skin along with tacking-in of the PPJ can be performed. Various approaches are available for this procedure, one through an incision along the abdominal crease8,10 and another through an infrapubic incision around the base of the penis.11
This study describes Shaeer’s technique, a minimally invasive method for revealing the concealed penis by a tape threaded from a 1- to 2-cm-long incision to another, overlying both anterior superior iliac spines (ASISs), and pulled tight to pull the mons pubis upward, backward, and laterally, and then fixed to the ASIS.
METHODS
One hundred twenty male patients were included in this study, all with genital size concerns due to a concealed penis. All patients had an overhanging SFP. All patients had normal erectile function as per history taking and the abbreviated version of the International Index of Erectile Function (IIEF-5) and had no anatomical abnormality of the penis such as penile curvature, hypospadias, Peyronie’s disease, or an erect length shorter than 9 cm (micropenis) as measured from the pubic bone to the tip (erect true length).
Patients were counseled to understand the normal anatomical measurements of the penis and vagina, the difference between visible and true lengths of the penis and the lack of functional effect for penile concealment on coital activity, and were informed of the recommended sexual positions for males with a concealed penis. Counseling failed to convince 65/120 patients to accept their current status and avoid intervention. Surgical and nonsurgical options for men with penile concealment were discussed, including weight loss, liposuction, and dermolipectomy, and also the technique at hand. Flaccid and erect visible lengths were evaluated in the standing position using rigid ruler. Erection was induced by intracavernosal injection of prostaglandin E1. To decide whether the patient was candidate for Shaeer’s technique, the examiner manually pushed the pubic fat backward, upward, and laterally toward ASIS bilaterally, with the patient standing in front of a mirror, for the patient to judge whether the improvement in visible length was satisfactory. Preoperative satisfaction with penile length was evaluated on a 5-point Likert scale.
Forty-five patients chose not to participate in this study and were managed by weight reduction (5/45), liposuction (32/45), and dermolipectomy (8/45). Twenty patients chose to participate in this study and undergo Shaeer’s technique. PDD was excluded by the psychiatrist. All patients provided a written informed consent and ethical approval was obtained from the Internal Review Board of the author’s institution. Preoperative marking was performed in the standing position, plotting the best possible path for the tape, from the ASIS on one side to the other, passing down to the PPJ, picking up the points of maximum redundancy on either side of the base of the penis along the plotted line (Fig. 1).
Fig. 1.

Preoperative markings.
Under general anesthesia, a 1- to 2-cm-long incision was cut just medial to the ASIS on either side (See video, Supplemental Digital Content 1, which displays Part 1 of the surgical technique. This video is available in the “Related Videos” section of the Full-Text article on PRSGlobalOpen.com or available at http://links.lww.com/PRSGO/A249). A 25-cm-long curved blunt forceps (BH226R, SAROT HAEMOSTATIC FORCEPS CURVED, Aesculap, Center Valley, Pa.) was inserted from one incision, following the preplotted marking, picking up the points of maximum redundancy and the PPJ, to emerge from the incision on the contralateral side (Fig. 2). A 5-mm-wide nonabsorbable Mersilene (Astralan 5-960, Assut Sutures, Lausanne, Switzerland) or polyester tape (Poly-tape 102-1054 by Neoligaments, Leeds, United Kingdom) was picked up by the forceps from one incision and pulled through to emerge from the other (Figs. 3, 4). Pulling on the tape tight resulted in pulling the SFP cephalad revealing the penis and defining the PPJ (Fig. 5) (See video, Supplemental Digital Content 2, which displays Part 2 of the surgical technique. This video is available in the “Related Videos” section of the Full-Text article on PRSGlobalOpen.com or available at http://links.lww.com/PRSGO/A250). The tape was sutured to the periosteum overlying the ASIS or to the external oblique aponeurosis on either side. Overlying subcutaneous fat and skin were closed. Average operative time was 15.2 ± 5.6 minutes.
Fig. 2.

Insertion of the instrument.
Fig. 3.

The tape.
Fig. 4.

The tape inserted from one side to the other.
Fig. 5.

Pulling on the tape lifts the mons pubis and defines the PPJ.
Video Graphic 1.

See video, Supplemental Digital Content 1, which displays Part 1 of the surgical technique. This video is available in the “Related Videos’ section of the Full-Text article on PRSGlobalOpen.com or available at http://links.lww.com/PRSGO/A249.
Video Graphic 2.

See video, Supplemental Digital Content 2, which displays Part 2 of the surgical technique. This video is available in the “Related Videos’ section of the Full-Text article on PRSGlobalOpen.com or available at http://links.lww.com/PRSGO/A250.
Patients were discharged the same day and allowed to resume sexual intercourse 7 to 10 days postoperatively. Patients were evaluated for flaccid and erect visible lengths and for satisfaction with length on a 5-point Likert scale, for up to 18 months postoperatively.
Points of Technique
Passing the forceps through, it was maintained in a fairly superficial plane above Scarpa’s fascia to avoid injury to the spermatic cords, with the inguinal skin and fat pinched upward in the palm of the surgeon’s hand, and even more superficially around the base of the penis to pick up most of the redundant skin and fat.
In patients with a larger body built where the forceps was not long enough to pass from one side to the other, 2 instruments were used, one passed from 1 ASIS to the midline and another loaded with the tape and passed in from the incision on the contralateral side to the midline to meet the first instrument and hand over the tape, which is then pulled out (Fig. 6). If handing over the tape is difficult, a puncture incision 5 mm long is cut in the midline, such that handing over is performed under vision (n = 9/20). In patients with a massive SFP and excessive skin redundancy, several tapes can be used passing through different planes between the base of the penis and the abdominal crease (n = 3/20).
Fig. 6.

Bilateral insertion of the instruments.
Statistical analysis was performed using Microsoft Excel 2010 and SPSS for windows version 19. Results were expressed in mean ± SD, frequencies (number of cases), and percentages when appropriate. Comparison of means was performed using paired samples t test. Student t test was used to evaluate statistical significance for continuous numerical values. Chi-square test was used to evaluate statistical significance for categorical values. A probability value (P value) less than 0.05 was considered statistically significant.
RESULTS
Twenty patients were operated upon by Shaeer’s technique, with an average age of 27.4 ± 5.7. Average body mass index was 32.1 ± 2. Preoperatively, flaccid visible length was 3 ± 0.9 cm, and erect visible length was 8 ± 4.6 cm (Fig. 7). Average preoperative satisfaction with length was 1.3 ± 0.4 cm. All patients were evaluated in-office at the third month postoperatively for complications and maintained length, and then every 3 months for a total of 18 months.
Fig. 7.

Preoperative length, flaccid and erect, in the standing position.
At 3 months postoperatively, the flaccid visible length was 7.1 ± 2.1 cm, with a 57.9% improvement in length (P < 0.0001), and erect visible length was 11.8 ± 2.1 cm, with a 32% improvement in length (P < 0.0001) (Fig. 8). On the 18th month, 12/20 patients were evaluated in-office and 8/20 over phone interviews (drop outs). In-office-measured flaccid length in the 12 patients was 6.9 ± 2.4 cm, with no statistically significant difference from length at the third month postoperatively (P = 0.479). Erect length could be evaluated in only 6/20 patients. Four patients agreed to have erection induced pharmacologically and 2 patients agreed to provide photographs of the self-induced erection alongside a ruler. In those patients (6/20), erect length was 11.55 ± 1.8 cm, with no statistically significant difference from length at the third month postoperatively (P = 0.475).
Fig. 8.

Postoperative length, flaccid and erect, in the standing position.
All 20 patients subjectively reported maintenance of the length gain on the 18th month whether in-office (12/20) or over phone interviews (8/20). None of the patients experienced persistent pain, wound gaping, wound infection, or extrusion of the tape (Table 1). Satisfaction at final follow-up (18 mo) was 4.7 ± 0.6 for the 20 patients, with a 73.1% improvement (P < 0.0001).
Table 1.
Preoperative and Postoperative Measurements
DISCUSSION
A concealed/buried penis is a condition where the shaft of the penis is invisible below the surface of the suprapubic skin and/or scrotum, to an extent that gives an impression of a short phallus, despite an adequate true length.11 The impact of a buried penis on sexual function, self-image, and psychological well-being can be profound. Patients with this condition may suffer embarrassment both in sexual life and in particular social contexts such as locker rooms, leading a subset of men to avoid relationships and some social activities, and limiting improvement of some patients with body dysmorphic disorders, and leading to sexual dysfunction in other cases.3
Dermolipectomy/monsplasty is an effective procedure for management of the buried penis, whether through an incision along the abdominal crease8,10 or through an infrapubic incision around the base of the penis,11 although with a long incision in the abdominal crease in the former or a scar on the dorsal aspect of the base of the penis in the latter. Mons pubis reduction in width through medial thigh lifting incision was also described, although with the possibility of disturbance of lymphatics of lower limb.12 Liposuction can ameliorate the condition but will not necessarily address pubic skin redundancy.
It is expected that dermolipectomy should offer the most volume reduction of suprapubic fat. In 64 males with buried penis, the combination of adhesiolysis, suprapubic and lateral lipectomy, anchoring the penoscrotal and PPJs, and skin coverage by a local flap resulted in a 93% improvement in flaccid visible length11 compared with a 57.9% improvement in the current series. However, in the current era of minimally invasive day case surgeries, seeking a less invasive alternative to dermolipectomy to correct penile concealment is in harmony with the trend. In addition to being minimally invasive, the technique at hand may address patient concerns over a longer incision in case of the abdominal crease approach to dermolipectomy or the stigmatizing circum-penile scar in case of the infrapubic approach,11 not to mention avoiding complications such as wound dehiscence, wound infection, or edema of the genital region. Shaeer’s technique is a trial to address those concerns by employing short incisions, away from the stigmatizing circum-penile region, without interfering with lymphatic drainage. Operative time is significantly less than alternative procedures. The technique can further be combined with liposuction to address the shortcoming of fat evacuation without skin tacking.
This study has some limitations such as the limited number of patients considering that counseling may defer patients from seeking aesthetic surgery (55/120 patients in the current series) and that there are alternatives that patients may opt for (45/120 patients). In addition, follow-up over extended periods of time, possibly decades, could better evaluate complications and sustainability.
Although complications are part of any procedure, none were encountered in this small series. However, possible complications could be encountered in a larger series with longer follow-up, including infection, extrusion, wound dehiscence or keloid formation, recurrence, and/or deformity due to either weight gain or loosening of the anchored ends of the tape. Synthetic materials have been used as mesh in hernia repair for decades; they do have their infection/extrusion rates but are still valid options. In case this sets in, the tape can be extracted in a minimally invasive procedure. Recurrence due to loosening/detachment of the tape from the anchored end points should be rare because of the wide sutures anchored to the periosteum. Furthermore, as with meshes and other synthetic materials used for reconstruction, their presence induces a mild inflammatory reaction and fibrous tissue formation, which further enforce their effect. Finally, several tapes can be inserted in several planes to back each other up. However, if recurrence occurs, the tape in vivo should not be harmful and should not prevent repetition of the procedure or performing alternative procedures such as liposuction or dermolipectomy.
Shaeer’s technique is not recommended in patients with morbid obesity in which bariatric surgery would be preferred, and patients with a massive suprapubic fat pad in which alternative procedures such as liposuction or dermolipectomy are recommended, perhaps aided by the technique at hand. Further contraindications include patients with an inguinal hernia or an undescended testis and patients with body dysmorphic disorders in which psychiatric counseling is the treatment of choice.
CONCLUSIONS
Shaeer’s technique is a minimally invasive, short, and simple procedure for monsplasty and revealing the concealed penis, through short laterally positioned incisions, avoiding long abdominal incisions, circum-penile stigmatizing incisions, and genital or lower limb edema, with aesthetically and functionally appealing results and high patient satisfaction rates. Long-term follow-up will determine sustainability of the length gain.
Supplementary Material
Footnotes
Disclosure: The author has no financial interest to declare in relation to the content of this article. The Article Processing Charge was paid for by the author.
Supplemental digital content is available for this article. Clickable URL citations appear in the text.
REFERENCES
- 1.Shaeer O, Shaeer K. The Global Online Sexuality Survey (GOSS): erectile dysfunction among Arabic-speaking internet users in the Middle East. J Sex Med. 2011;8:2152–2160. doi: 10.1111/j.1743-6109.2011.02297.x. quiz 2160–2163. [DOI] [PubMed] [Google Scholar]
- 2.Shaeer O, Shaeer K. The Global Online Sexuality Survey (GOSS): ejaculatory function, penile anatomy, and contraceptive usage among Arabic-speaking Internet users in the Middle East. J Sex Med. 2012;9:425–433. doi: 10.1111/j.1743-6109.2011.02338.x. [DOI] [PubMed] [Google Scholar]
- 3.Shaeer O, Shaeer K. The Global Online Sexuality Survey (GOSS): the United States of America in 2011. Chapter I: Erectile dysfunction among English-speakers. J Sex Med. 2012;9:3018–3027. doi: 10.1111/j.1743-6109.2012.02976.x. [DOI] [PubMed] [Google Scholar]
- 4.Veale D, Miles S, Read J, et al. Penile dysmorphic disorder: development of a screening scale. Arch Sex Behav. 2015;44:2311–2321. doi: 10.1007/s10508-015-0484-6. [DOI] [PubMed] [Google Scholar]
- 5.Lim DJ, Barraza MA, Stevens PS. Correction of retractile concealed penis. J Urol. 1995;153:1668–1670. [PubMed] [Google Scholar]
- 6.Shepard GH, Wilson CS, Sallade RL. Webbed penis. Plast Reconstr Surg. 1980;66:453–454. [PubMed] [Google Scholar]
- 7.Shaeer O. Restoration of the penis following amputation at circumcision: Shaeer’s A-Y plasty. J Sex Med. 2008;5:1013–1021. doi: 10.1111/j.1743-6109.2007.00675.x. [DOI] [PubMed] [Google Scholar]
- 8.Alter GJ, Ehrlich RM. A new technique for correction of the hidden penis in children and adults. J Urol. 1999;161:455–459. [PubMed] [Google Scholar]
- 9.Wagenblast AL, Laessoe L, Printzlau A. Self-reported problems and wishes for plastic surgery after bariatric surgery. J Plast Surg Hand Surg. 2014;48:115–121. doi: 10.3109/2000656X.2013.822384. [DOI] [PubMed] [Google Scholar]
- 10.Alter GJ. Surgical techniques: surgery to correct hidden penis. J Sex Med. 2006;3:939–942. doi: 10.1111/j.1743-6109.2006.00298.x. [DOI] [PubMed] [Google Scholar]
- 11.Shaeer O, Shaeer K. Revealing the buried penis in adults. J Sex Med. 2009;6:876–885. doi: 10.1111/j.1743-6109.2008.01162.x. [DOI] [PubMed] [Google Scholar]
- 12.Rezak KM, Borud LJ. Integration of the vertical medial thigh lift and monsplasty: the double-triangle technique. Plast Reconstr Surg. 2010;126:153e–154e. doi: 10.1097/PRS.0b013e3181e3b5e6. [DOI] [PubMed] [Google Scholar]


