Abstract
Purpose
Poor sleep quality during pregnancy is associated with adverse obstetric and neuropsychiatric outcomes. Despite its routine use as a sleep quality assessment scale among men and non-pregnant women, the psychometric properties of the Pittsburgh Sleep Quality Index (PSQI) have not been assessed among US pregnant women. We sought to evaluate the construct validity and factor structure of the PSQI among 1,488 pregnant women.
Methods
A structured interview was used to collect information about demographics and sleep characteristics in early pregnancy. The Patient Health Questionnaire-9 (PHQ-9) and the Depression, Anxiety, and Stress Scale-21 (DASS-21) were used to assess symptoms of depression, anxiety and stress. Consistency indices, exploratory and confirmatory factor analyses (EFA and CFA), correlations, and logistic regression procedures were used.
Results
The reliability coefficient, Cronbach’s alpha for the PSQI items was 0.74. Results of the EFA showed that a rotated factor solution for the PSQI contained two factors with eigenvalues >1.0 accounting for 52.8% of the variance. The PSQI was significantly positively correlated with the PHQ-9 (rs=0.48) and DASS-21 (rs=0.42) total scores. Poor sleepers (PSQI global score>5) had increased odds of experiencing depression (OR=6.47; 95%CI: 4.56–9.18), anxiety (OR=3.59; 95%CI: 2.45–5.26) and stress (OR=4.37; 95%CI: 2.88–6.65) demonstrating evidence of good construct validity. CFA results corroborated the two-factor structure finding from the EFA; and yielded reassuring measures indicating goodness of fit (comparative fit index=0.975) and accuracy (root mean square error of approximation=0.035).
Conclusions
The PSQI has good construct validity and reliability for assessing sleep quality among pregnant women.
Keywords: PSQI, pregnancy, factor analysis, depression, PHQ-9, DASS-21
INTRODUCTION
Sleep complaints including poor sleep quality and disorders in pregnancy have been associated with a myriad of adverse pregnancy outcomes including hyperemesis [1], cesarean delivery [2], preterm delivery [2, 3], gestational diabetes [4], fetal growth restriction [3], preeclampsia [2], placental abruption[5], antepartum depression, and suicidal ideation [6]. On the basis of these observations, investigators have suggested that it may be important to screen for and address sleep problems among pregnant women [7]. To that end, the Pittsburgh Sleep Quality Index (PSQI), a widely used self-reported measure of sleep quality with acceptable psychometric properties when used among men and non-pregnant women [8–18], has been suggested as appropriate for use among pregnant women [7, 19]. However, the psychometric properties of the PSQI have not been adequately assessed among pregnant women. We are aware of only three published studies that have evaluated the psychometric properties of the PSQI among pregnant women in Britain [19], Australia[7] and Peru [5]. Given the dearth of studies documenting the psychometric properties of the PSQI when used among pregnant women, we sought to evaluate the psychometric properties of the PSQI among pregnant US women during early pregnancy. We also assessed the relationship of maternal early pregnancy sleep quality with measures of antepartum depressive and anxiety symptoms as measured using the Patient Health Questionnaire-9 (PHQ-9) and the Depression, Anxiety, and Stress Scale-21 (DASS-21).
METHODS
Study Population
This study is based on 1,488 pregnant women enrolled in the Migraine and Pregnancy Study, a prospective cohort study of pregnant women, during the period between November 2009 and March 2013. The Migraine and Pregnancy Study was designed to investigate the relationship between maternal history of migraine and risk of developing preeclampsia later in pregnancy. Participants were recruited from women attending prenatal care at clinics affiliated with Swedish Medical Center in Seattle, Washington. Women were ineligible if they initiated prenatal care after 20 weeks gestation, were younger than 18 years of age, did not speak and read English, did not plan to carry the pregnancy to term, or did not plan to deliver at Swedish Medical Center. The procedures used in the study were in agreement with the protocol approved by the Institutional Review Board of Swedish Medical Center, Seattle, WA. All participants provided written informed consent.
Data Collection
Participants completed a questionnaire administered by trained interviewers at enrollment in early pregnancy. Interviewers were supervised by a multidisciplinary team of investigators that included a study neurologist, epidemiologists and a perinatologist. Data were collected via interviews not by self-administered questionnaires. Information regarding maternal socio-demographics, lifestyle characteristics, medical and reproductive history, migraine status, symptoms of depression and anxiety, and sleep problems was collected. The interview included a structured migraine assessment questionnaire adapted from the deCODE Genetics migraine questionnaire (DMQ3)[20] and an assessment of disability associated with headaches experienced before pregnancy.
Measures
Pittsburgh Sleep Quality Index (PSQI)
The PSQI is a 19-item, self-rated questionnaire designed to measure sleep quality and disturbance over the past month in clinical populations [17]. The 19 items are combined into 7 clinically-derived component scores including 1) sleep duration; 2) sleep disturbance; 3) sleep latency; 4) daytime dysfunction due to sleepiness; 5) sleep efficiency; 6) overall sleep quality; and 7) sleep medication use. Each sleep component yields a score ranging from 0 to 3, with 3 indicating the greatest dysfunction. Sleep component scores were summed to yield a total score ranging from 0 to 21 with the higher total score (referred to as global score) indicating worse sleep quality. In distinguishing good and poor sleepers, a global PSQI score >5 yields a sensitivity of 89.6% and a specificity of 86.5% [17].
Patient Health Questionnaire-9 (PHQ-9)
The PHQ-9 is a 9-item self-reported, diagnostic and severity measure for current (in the prior 14 days) depression using criteria from the Diagnostic and Statistical Manual of Mental Disorders, fourth edition (DSM-IV) [21, 22]. The nine items include: 1) anhedonia; 2) depressed mood; 3) insomnia or hypersomnia; 4) fatigue or loss of energy; 5) appetite disturbance; 6) guilt or worthlessness; 7) diminished ability to think or concentrate; 8) psychomotor agitation or retardation; and 9) suicidal thoughts. Scores for each item range from 0 (“not at all”) to 3 (“nearly every day”). The PHQ-9 total score is the sum of scores for the nine items for each participant and ranges from 0 to 27. Among patients from general care clinics and obstetrics-gynecology clinics, a score of ≥ 10 is associated with a sensitivity of 88% and a specificity of 88% in diagnosing major depressive disorder (MDD) [21]. The Spanish-language version of the PHQ-9 was shown to work well in pregnant women with good reliability and construct validity [23, 24]. In the current study, the presence of depression was defined as PHQ-9 score ≥ 10.
Depression, Anxiety Stress Scale-21 (DASS-21)
The DASS-21 is a set of three self-report scales designed to measure the negative emotional states of depression, anxiety, and stress [25, 26]. The depression scale assessed dysphoria, hopelessness, devaluation of life, self-deprecation, lack of interest or involvement, anhedonia, and inertia; the anxiety scale assessed autonomic arousal, situational anxiety, and subjective experience of anxious affect; and the stress scale assessed difficulty relaxing, nervous arousal, easy agitation, irritability, and impatience [25, 26]. The 21-item instrument asks respondents to rate the relevancy of each of the three negative affective states over the past week on a four-point scale ranging from: (0) not at all, (1) some of the time, (2) a good part of the time, and (3) most of the time. Scores range from 0 to 21 in each of the three domains, and are then multiplied by two to produce a possible score of 0 to 42 in each of the three domains. Validated cutoffs were used to categorize DASS-21 scores [26]. Briefly, we categorized participants as exhibiting minimal (score 0–9), mild (score 10–13), moderate (score 14–20), and severe (score ≥21) depressive symptoms on the DASS Depression subscale. The corresponding cutoffs for the DASS Anxiety subscale were minimal (score 0–7), mild (score 8–9), moderate (score 10–14), and severe (score ≥15). The corresponding cutoffs for the DASS Stress subscale were minimal (score 0–14), mild (score 15–18), moderate (score 19–25), and severe (score ≥26). Internal consistencies for each scale for the DASS normative sample are: depression 0.91; anxiety 0.84; and stress 0.90 [26].
Other Covariates
Maternal age was categorized as: 20–29, 30–34, and ≥35 years. Other variables included: maternal race/ethnicity (non-Hispanic white, African-American, Asian, other), annual household income in U.S. thousands (<50, 50–69, ≥70), single marital status (yes, no), nulliparous (yes, no), unplanned pregnancy (yes, no), and cigarette smoker (never, prior, current). Pre-pregnancy body mass index (BMI) was calculated from pre-pregnancy height and weight (kg/m2) and categorized as: <18.5, 18.5–24.9, 25.0–29.9, and ≥30 kg/m2 based on cutoffs from the WHO Global Database on BMI [27].
Statistical Analysis
We first examined the frequency distributions of maternal socio-demographic, behavioral characteristics, medical and reproductive history. We used the Student’s t-test and the Chi-square test to assess bivariate differences according to sleep quality for continuous and categorical variables, respectively. We then assessed the reliability and validity of the PSQI using several agreement and consistency indices. Briefly, we calculated the Cronbach’s alpha to assess the internal consistency for the PSQI using the seven clinically-derived component scores. We completed an exploratory factor analysis (EFA) using the principal component analysis with oblique rotation (promax) to assess the factor structure of the PSQI. Prior to conducting factor analysis, we assessed the suitability for performing the factor analysis. The result of the suitability analysis supported the appropriateness of proceeding with the factor analysis (Bartlett’s test of sphericity, P<0.001; the Kaiser-Meyer-Olkin measure of sampling adequacy = 0.72). We used the scree plot and eigenvalues associated with each factor to identify the number of meaningful factors. Factors with eigenvalues > 1 were assumed to be meaningful and retained for rotation [28]. Sleep components with rotated factor loading ≥0.4 in absolute value were considered “dominant” and were considered as a defining item for each specific factor. Further, we also completed a confirmatory factor analysis (CFA) to complement the EFA. Given that the multivariate normality assumption was not met in our database, we used the weighted least squares (WLS) estimation for the CFA. We calculated the following parameters to evaluate model fit: the comparative fit index (CFI), the standardized root mean square residual (SRMR), and the root mean square error of approximation (RMSEA). For this study, we used the following criteria for consideration of a reasonable fit: 1) CFI close to 0.90 or above; 2) SRMR close to 0.08 or below; and 3) RMSEA close to 0.06 or below [29]. For the best fit models, we summarized the standardized regression weights for path (factor loadings on each factor) in all reported figures. As an additional measure of construct validity, we computed unadjusted and age adjusted Spearman’s Rank-Order correlation coefficients (rs) between the PSQI scores with the PHQ-9, and the DASS-21. We calculated correlation coefficients of the three subscale scores with scores derived from the DASS-21 instruments, respectively. Finally, we fitted multivariate logistic regression models to calculate odds ratios (ORs) and 95% confidence intervals (CIs) of poor sleep quality (yes vs. no) in relation with depression (yes vs. no), anxiety disorder (yes vs. no), and stress (yes vs. no). We included potential confounders of a priori interest (i.e., maternal age, parity, pre-pregnancy body mass index, and annual household income) in final logistic regression models. Statistical analyses were performed using SAS 9.4 (SAS Institute, Cary, NC, USA). The level of statistical significance was set at P-value < 0.05 and all tests were two-sided.
RESULTS
Select sociodemographic, lifestyle and reproductive characteristics of the study cohort are presented in Table 1. The mean age of the 1,488 participants was 33.4 years (standard deviation, SD = 4.2 years), and the mean gestational age at interview was 21.7 weeks (SD=8.8 weeks). The majority of participants were white (81.5%), married (91.8%), never smokers (74.5%), with an annual household income ≥70,000 (88.2%), and planned index pregnancy (87.6%). Nearly half of the participants were nulliparous (51.7%). The mean scores of the PHQ-9 and the DASS-21 total score were 5.6 (SD = 3.6) and 17.1 (SD = 13.8), respectively. The mean scores for the DASS-21 subscales of anxiety, depression, and stress were 3.7 (SD = 4.3), 4.4 (SD = 5.3), and 9.0 (SD = 6.8), respectively.
Table 1.
Characteristics of the Pittsburgh Sleep Quality Index (PSQI) among pregnant women (N=1,488)
| Selected variables | All participants (N=1488)
|
Poor sleep quality (PSQI > 5) (N=551)
|
Good sleep quality (PSQI ≤ 5) (N=937)
|
P-value** | |||
|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | ||
| Maternal age (years)* | 33.4 ± 4.2 | 33.6 ± 4.4 | 33.3 ± 4.0 | 0.31 | |||
| Maternal age (years) | |||||||
| 20 – 29 | 245 | 16.5 | 89 | 16.2 | 156 | 16.6 | 0.95 |
| 30 – 34 | 691 | 46.4 | 255 | 46.3 | 436 | 46.5 | |
| ≥35 | 552 | 37.1 | 207 | 37.6 | 345 | 36.8 | |
| Maternal ethnicity | |||||||
| Non-Hispanic white | 1212 | 81.5 | 441 | 80.0 | 771 | 82.3 | 0.39 |
| African American | 21 | 1.4 | 11 | 2.0 | 10 | 1.1 | |
| Asian | 181 | 12.2 | 71 | 12.9 | 110 | 11.7 | |
| Other | 62 | 4.2 | 25 | 4.5 | 37 | 3.9 | |
| Married | 1366 | 91.8 | 498 | 90.4 | 868 | 92.6 | 0.13 |
| Annual household income | |||||||
| < 50,000 | 43 | 2.9 | 22 | 4.0 | 21 | 2.2 | 0.03 |
| 50,000 – 69,000 | 78 | 5.2 | 38 | 6.9 | 48 | 4.3 | |
| ≥70,000 | 1312 | 88.2 | 473 | 85.8 | 839 | 89.5 | |
| Nulliparous | 770 | 51.7 | 262 | 47.5 | 508 | 54.2 | 0.01 |
| Planned pregnancy | 1303 | 87.6 | 469 | 85.1 | 834 | 89.0 | 0.03 |
| Gestational age at interview (weeks)* | 21.7 ± 8.8 | 22.0 ± 9.9 | 21.5 ± 8.1 | 0.38 | |||
| Smoking status | |||||||
| Never | 1109 | 74.5 | 394 | 71.5 | 715 | 76.3 | 0.10 |
| Prior | 321 | 21.6 | 135 | 24.5 | 186 | 19.9 | |
| Current | 58 | 3.9 | 22 | 4.0 | 36 | 3.8 | |
| Pre pregnancy body mass index (kg/m2) | |||||||
| <18.5 | 50 | 3.4 | 16 | 2.9 | 34 | 3.6 | 0.0002 |
| 18.5–24.9 | 1053 | 70.8 | 362 | 65.7 | 691 | 73.7 | |
| 25–29.9 | 276 | 18.5 | 116 | 21.1 | 160 | 17.1 | |
| ≥30 | 103 | 6.9 | 56 | 10.2 | 47 | 5.0 | |
| Lifetime migraine diagnosis** (ICHD-II) | 415 | 27.9 | 198 | 35.9 | 217 | 23.2 | <0.001 |
| PHQ-9* | 5.6 ± 3.6 | 7.5 ± 3.8 | 4.4 ± 3.0 | <0.0001 | |||
| DASS-21 Total score * | 17.1 ± 13.8 | 23.0 ± 15.7 | 13.6 ± 11.3 | <0.0001 | |||
| DASS-21 Anxiety* | 3.7 ± 4.3 | 5.0 ± 5.0 | 2.9 ± 3.5 | <0.0001 | |||
| DASS-21 Depression* | 4.4 ± 5.3 | 6.3 ± 6.2 | 3.3 ± 4.2 | <0.0001 | |||
| DASS-21 Stress* | 9.0 ± 6.8 | 11.7 ± 7.3 | 7.5 ± 5.9 | <0.0001 | |||
Abbreviations: PHQ-9, Patient Health Questionnaire 9-Item; DASS-21, Depression, Anxiety, and Stress Scale-21 Item; ICHD, the International Classification of Headache Disorders.
Due to missing data, percentages may not add up to 100%.
P-value was calculated using the Student’s t-test for continuous variables and the Chi-square test for categorical variables
Mean ± Standard deviation
Women with “migraine” refer to the combination of both women with definitive migraine (IHS category 1.1) and probable migraine (IHS category 1.6). IHS=International Headache Society
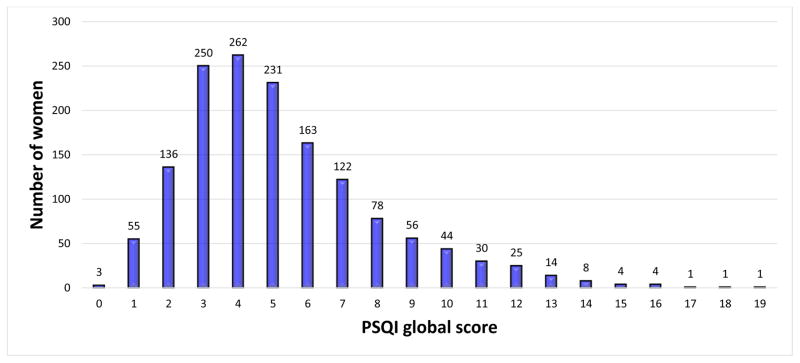
Figure 1 shows the distribution of the global PSQI score. The global PSQI score ranged from 0 to 19, with a mode of 4. The mean score was 5.2 and the median score was 5. Based on the PSQI global score, 37.0% of study participants were classified as poor sleepers (PSQI global score >5) and 63.0% were classified as good sleepers (PSQI global score ≤5) (Table 1). Compared with good sleepers, poor sleepers were less likely to be nulliparous and within BMI range of 18.5 to 24.9 kg/m2, and report current pregnancy as planned. Poor sleepers were more likely to have an annual household income <$70, 000. Compared with good sleepers, poor sleepers had significantly higher mean scores on all other measures (i.e., PHQ-9, DASS-21 total score, and three DASS-21 subscales; all P-value < 0.0001), reflecting higher depressive, anxiety, and stress symptomatology.
Figure 1.
Distribution of the global score of the Pittsburgh Sleep Quality Index (PSQI) among pregnant women (N=1,488)
An overall Cronbach’s alpha of 0.74 was observed (Table 2). The correlations between the seven component scores of the PSQI and the global PSQI score ranged from 0.31 to 0.64 (Table 2). An exploratory factor analysis yielded a two-factor solution with eigenvalues of 2.23 and 1.69, corresponding to sleep quality (factor 1) and sleep disturbance (factor 2) (Table 3). Subjective sleep quality cross-loaded on both factors. The two factors together explained 52.8% of the total variance.
Table 2.
Item Characteristics, item-total correlation, alpha if item deleted from the Pittsburgh Sleep Quality Index (PSQI) among pregnant women (N=1,488)
| Components | Mean | SD | Corrected item- total correlation | Alpha if item deleted |
|---|---|---|---|---|
| 1. Sleep duration | 0.22 | 0.54 | 0.57 | 0.71 |
| 2. Sleep disturbance | 1.34 | 0.51 | 0.44 | 0.73 |
| 3. Sleep latency | 0.81 | 0.79 | 0.54 | 0.70 |
| 4. Daytime dysfunction due to sleepiness | 0.97 | 0.78 | 0.39 | 0.72 |
| 5. Sleep efficiency | 0.58 | 0.89 | 0.62 | 0.69 |
| 6. Subjective sleep quality | 1.12 | 0.67 | 0.64 | 0.70 |
| 7. Sleep medication use | 0.18 | 0.56 | 0.31 | 0.74 |
| Global PSQI score | 5.23 | 2.84 |
Overall Cronbach’s alpha (the overall reliability of the PSQI) is 0.74
Abbreviations: SD, standard deviation
“Corrected item-total correlation” are the correlations between each components and the global PSQI score.
“Alpha if item deleted” – represents the PSQI’s Cronbach alpha reliability coefficient for internal consistence if the specific item is removed from the scale.
Table 3.
The factor loadings in exploratory factor analysis of the Pittsburgh Sleep Quality Index (PSQI) among pregnant women (N=1,488)
| Components | Factor loadings
|
|
|---|---|---|
| Factor 1 | Factor 2 | |
| 1. Sleep duration | 0.87 | −0.08 |
| 2. Sleep disturbance | 0.04 | 0.72 |
| 3. Sleep latency | 0.47 | 0.30 |
| 4. Daytime dysfunction due to sleepiness | −0.14 | 0.80 |
| 5. Sleep efficiency | 0.88 | −0.04 |
| 6. Subjective sleep quality | 0.47 | 0.49 |
| 7. Sleep medication use | 0.13 | 0.31 |
Exploratory factor analysis was conducted using the principal component analysis with promax rotation
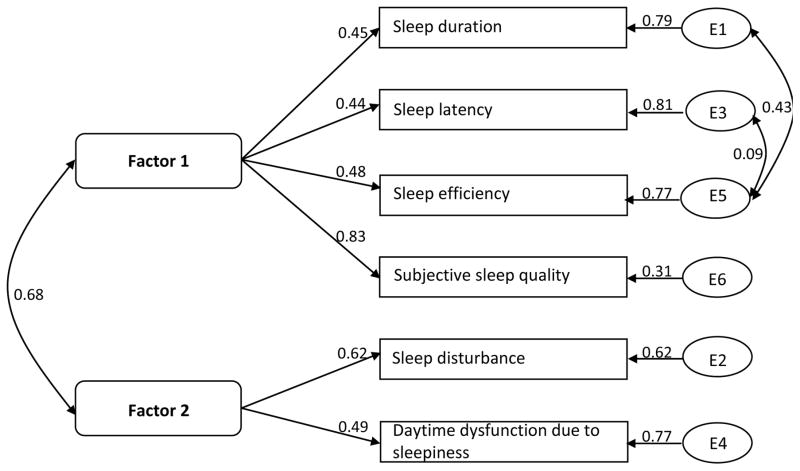
As shown in Figure 2 and Table 4, results from CFA corroborated the EFA findings showing a two-factor solution for the six components. Indicators of goodness of fit: CFI, RMSEA and SRMR were 0.975, 0.035, and 0.026, respectively. Sleep duration and sleep efficiency were associated with an approximate correlation of 0.43. We re-examined the model, allowing for these two items to be correlated with each other, which improved the fit (model 3b).
Figure 2.
Standardized regression weights for paths associated with the best fit model for the Pittsburgh Sleep Quality Index (PSQI) among pregnant women (N=1,488). Numbers next to arrows indicate factor loadings. Numbers next to error terms (left side of the figure) indicate correlation coefficients.
Table 4.
Models evaluated for the Pittsburgh Sleep Quality Index (PSQI) and corresponding fit indices using confirmatory factor analysis among pregnant women (N=1,488)
| Models | χ2 | df | CFI | SRMR | RMSEA |
|---|---|---|---|---|---|
| Model 1: 2 factors (correlated), 6 components (F1: 1, 3, 5, 6; F2: 2, 4, 6) | 69.967 | 7 | 0.851 | 0.054 | 0.078 |
| Model 2: 2 factors (correlated), 6 components (F1: 1, 3, 5; F2: 2, 4, 6) | 109.008 | 8 | 0.762 | 0.073 | 0.092 |
| Model 2a: 2 factors (correlated), 6 components (F1: 1, 3, 5; F2: 2, 4, 6) correlation between e1& e5 | 56.633 | 7 | 0.883 | 0.046 | 0.069 |
| Model 2b: 2 factors (correlated), 6 components (F1: 1, 3, 5; F2: 2, 4, 6) correlation between e1& e5, e2&e4 | 16.648 | 6 | 0.975 | 0.019 | 0.035 |
| Model 3: 2 factors (correlated), 6 components (F1: 1, 3, 5, 6; F2: 2, 4) | 136.848 | 8 | 0.696 | 0.091 | 0.104 |
| Model 3a: 2 factors (correlated), 6 components (F1: 1, 3, 5, 6; F2: 2, 4) correlation between e1& e5 | 36.292 | 7 | 0.931 | 0.036 | 0.053 |
| Model 3b: 2 factors (correlated), 6 components (F1: 1, 3, 5, 6; F2: 2, 4) correlation between e1& e5, e3&e5 | 16.806 | 6 | 0.975 | 0.026 | 0.035 |
Abbreviations: df, degree of freedom; CFI, comparative fit index;
SRMR, Standardized Root Mean Square Residual; RMSEA, root mean square error of approximation
Table 5 presents correlation coefficients between the global PSQI score and scores derived from the PHQ-9 and the DASS-21. The global PSQI score was significantly positively correlated with the scores of all other measures (all P-value < 0.0001). In sensitivity analyses that excluded the “sleep medication use” component from the PSQI global score, correlation coefficients of similar magnitudes were obtained. Further adjustment for maternal age resulted in negligible changes in the magnitude of partial correlation coefficients. Finally, as an additional measure of construct validity, we completed multivariable logistic regression analyses to assess associations of poor sleep quality (PSQI score > 5) with depression, anxiety, and stress. We found that poor sleepers (PSQI global score > 5) had increased odds of experiencing depression (PHQ-9 ≥ 10) as assessed by the PHQ-9 (OR=6.47; 95%CI: 4.56–9.18). Compared with good sleepers, poor sleepers had a 4.34-fold increased odds of depression (95% CI: 2.74, 6.86) (DASS-21 Depression subscale ≥ 14); a 3.59-fold increased odds (95% CI: 2.45, 5.26) of anxiety (DASS-21 Anxiety subscale ≥ 10); and a 4.37-fold increased odds (95% CI: 2.88, 6.65) of stress (DASS-21 Stress subscale ≥ 19) (Table 6). We explored the possibility that maternal lifetime history of migraine may have confounded reported associations. However, when we added this covariate into multivariable models, we found no evidence of confounding. For example, when we added maternal history of lifetime migraine to the model for PHQ-defined depression the odds of depression increased very slight from 6.47 (95% CI 4.56 –9.18) to 6.51 (95% CI 4.57–9.26).
Table 5.
Spearman’s Rank-Order Correlation coefficients for scores of the Pittsburgh Sleep Quality Index (PSQI) and other measures (N=1,488)
| Measures | PSQI during pregnancy
|
|||
|---|---|---|---|---|
| PSQI global score
|
PSQI global score excluding component 7
|
|||
| Unadjusted | Adjusted* | Unadjusted | Adjusted* | |
| PHQ-9 (Depression) | 0.478 | 0.478 | 0.467 | 0.468 |
| DASS-21 Total Score | 0.420 | 0.421 | 0.415 | 0.416 |
| DASS-21 Anxiety | 0.292 | 0.294 | 0.290 | 0.292 |
| DASS-21 Depression | 0.377 | 0.378 | 0.372 | 0.373 |
| DASS-21 Stress | 0.366 | 0.367 | 0.361 | 0.362 |
Adjusted for maternal age
Abbreviations: PHQ-9, Patient Health Questionnaire 9-Item; DASS-21, Depression, Anxiety, and Stress Scale-21 Item
All correlations are statistically significant with P-value <0.0001.
Table 6.
Associations between the Pittsburgh Sleep Quality Index (PSQI) during pregnancy and other measures (N=1,488)
| Measures | All participants (N=1488)
|
Poor sleep quality (PSQI > 5) (N=551)
|
Good sleep quality (PSQI ≤5) (N=937)
|
Unadjusted OR (95% CI) | Adjusted OR* (95% CI) | |||
|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | |||
| PHQ-9 | ||||||||
| No depression (PHQ-9 < 10) | 1279 | 86.0 | 401 | 72.8 | 878 | 93.7 | Reference | Reference |
| Major depressive disorders (PHQ-9 ≥10) | 202 | 13.6 | 149 | 27.0 | 53 | 5.7 | 6.16 (4.40, 8.61) | 6.47 (4.56, 9.18) |
| DASS-21 Depression | ||||||||
| Normal (0–9) | 1265 | 85.0 | 415 | 75.3 | 850 | 90.7 | Reference | Reference |
| Mild (10–13) | 118 | 7.9 | 67 | 12.2 | 51 | 5.4 | 2.69 (1.84, 3.95) | 2.59 (1.74, 3.86) |
| Moderate-Severe (≥14) | 99 | 6.7 | 68 | 12.3 | 31 | 3.3 | 4.49 (2.89, 6.98) | 4.34 (2.74, 6.86) |
| DASS-21 Anxiety | ||||||||
| Normal (0–7) | 1238 | 83.2 | 405 | 73.5 | 833 | 88.9 | Reference | Reference |
| Mild (8–9) | 101 | 6.8 | 54 | 9.8 | 47 | 5.0 | 2.36 (1.57, 3.56) | 2.41 (1.58, 3.69) |
| Moderate-Severe (≥10) | 143 | 9.6 | 91 | 16.5 | 52 | 5.5 | 3.60 (2.51, 5.16) | 3.59 (2.45, 5.26) |
| DASS-21 Stress | ||||||||
| Normal (0–14) | 1227 | 82.5 | 390 | 70.8 | 837 | 89.3 | Reference | Reference |
| Mild (15–18) | 136 | 9.1 | 80 | 14.5 | 56 | 6.0 | 3.07 (2.13, 4.40) | 3.16 (2.17, 4.59) |
| Moderate-Severe (≥19) | 119 | 8.0 | 80 | 14.5 | 39 | 4.2 | 4.40 (2.95, 6.57) | 4.37 (2.88, 6.65) |
Due to missing data, percentages may not add up to 100%.
Abbreviations: PHQ-9, Patient Health Questionnaire 9-Item; DASS-21, Depression, Anxiety, and Stress Scale-21 Item
Adjusted for maternal age (years), parity (nulliparous vs. multiparous), pre-pregnancy body mass index (kg/m2) (<18.5; 18.5–24.9; 25.0–29.9; ≥30), and annual household income (< $50,000; $50,000–69,000; ≥$70,000).
DISCUSSION
The PSQI demonstrated good reliability and construct validity when used among a cohort of US pregnant women. Both exploratory and confirmatory factor analyses indicated a two-factor solution: sleep quality and sleep disturbance. Although the assumption for one-factor structure was not met, an overall Cronbach’s alpha of 0.74 was reported. Women classified as having poor sleep quality in early pregnancy (i.e., poor sleepers; PSQI global score > 5) had significantly increased odds of depression (OR=6.47; 95%CI: 4.56–9.18) as assessed by the PHQ-9. Poor sleepers were also associated with increased odds of anxiety (OR=3.59; 95% CI: 2.45, 5.26) and stress (OR=4.37; 95% CI: 2.88, 6.65) as assessed using the DASS-21 scale. Removal of the component “sleep medication use” did not have a noticeable influence on the construct validity of the PSQI.
Although the total score of PSQI is typically used to identify sleep quality, the results of our exploratory factor analysis yielded a two-factor structure, including a sleep quality factor and sleep disturbance factor. Based on the results of exploratory and confirmatory factor analysis, a two-factor model demonstrated a better fit than the one-factor model proposed by Buysse [17], which was consistent with reports from several previous studies [12, 14, 18, 30]. Our study findings and those of others suggest that the use of a single summed global score of all the six sub scales of PSQI might not best capture the multidimensional nature of poor sleep quality.
However, despite accumulating evidence in favor of a two- or three-factor structure of the PSQI across medically and ethnically diverse research populations, studies designed to further validate the two-factor structure of the PSQI across and to assess the comparative validity and clinical utility of the two factor-specific scoring versus the single global score of the PSQI are warranted.
The PSQI demonstrated good construct and convergent validity in our study population. We found that the PSQI global score was moderately correlated with depressive symptoms (assessed using the PHQ-9), and symptoms of depressive, anxiety, and stress (assessed using the DASS-21). Neither maternal age nor “sleep medication use” had a noticeable influence on these correlations. Our findings are similar to reports from other investigators. For example, among a sample of 660 Peruvian pregnant women, Zhong et al [5] reported statistically significant correlations of scores from the PSQI and the PHQ-9 and generalized anxiety disorders (GAD-7). These results and those of ours suggest that the PSQI and scales designed to measure symptoms of mood and anxiety disorders support the similarity in constructs between scales and reinforce evidence from clinical epidemiological studies documenting high degrees of co-morbidity of sleep and psychiatric disorders [16, 19].
The present study has several limitations. First, objective measurements of maternal sleep quality were not available (e.g., actigraphy or polysomnography), precluding evaluation of associations between the questionnaire-based measures and objective measurements of sleep quality. Second, our cross-sectional study did not provide information regarding the persistence of poor sleep quality over the course of pregnancy. Importantly, we cannot establish the temporal relation between sleep quality, and mood or anxiety disorders. We did ask women to report whether they had received a physician diagnosis of depression. In this cohort 2.7% of women responded affirmatively to this question. Although interpretation of these data are limited, there remained a trend of increased poor sleep quality among women with a self-reported history of ever having physician-diagnosed depression (3.6% vs. 2.1%). Longitudinal studies are needed to estimate potential bi-directional associations of sleep and psychiatric disorders among reproductive aged and pregnant women. Third, we did not have access to information concerning maternal use of prescribed psychotropic or neurotropic medications. Despite these limitations, this is the first study to evaluate the psychometric properties of the PSQI among pregnant women in the US. Another strength of this study was the relatively large sample of pregnant women, which allowed us to examine factor structures and to ensure the stability of the factor solution. Moreover, our study made allowances for assessing relations of PSQI assessed sleep quality with multiple measures of maternal antepartum mood and anxiety disorders.
In summary, the PSQI was appropriate for use with good reliability and good construct validity among pregnant women. Women with poor sleep quality had statistically significantly increased odds of mood, anxiety and stress disorders. Removal of the component “sleep medication use” neither improved the fit of the CFA models nor had a noticeable influence on the construct validity of the PSQI. Future studies are needed to further validate the two-factor structure among diverse populations, address whether a two factor-specific scoring of the PSQI is favored over the PSQI global score, and assess change in sleep quality over the course of gestation. The findings of our study may have clinical and public health implications. Though screening alone is insufficient for addressing sleep disorders, having psychometrically well characterized, reliable and valid screening instruments such as the PSQI allows for identifying sleep quality and associated risk factors in pregnancy. Future development of screening and treatment programs targeting sleep disturbance during the first trimester are warranted to mitigate the risk of mood disorders during late pregnancy and postpartum.
Acknowledgments
Financial support: This research was supported by awards from the Eunice Kennedy Shriver Institute of Child Health and Human Development (R01-HD-055566 and R01-HD-059835) at the National Institutes of Health (NIH).
Awards from the Eunice Kennedy Shriver Institute of Child Health and Human Development (R01-HD-055566 and R01-HD-059835) at the National Institutes of Health (NIH) supported this research. The NIH had no further role in the study design; in the collection, analysis, and interpretation of data; in the writing of the report; and in the decision to submit the paper for publication.
Footnotes
CONFLICT OF INTEREST
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements), or non-financial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript.
References
- 1.Lee KA. Alterations in sleep during pregnancy and postpartum: a review of 30 years of research. Sleep Medicine Reviews. 1998;2(4):231–242. doi: 10.1016/s1087-0792(98)90010-7. [DOI] [PubMed] [Google Scholar]
- 2.Chen Y-H, Kang J-H, Lin C-C, Wang I-T, Keller JJ, Lin H-C. Obstructive sleep apnea and the risk of adverse pregnancy outcomes. American Journal of Obstetrics and Gynecology. 2012;206(2):136.e131–136.e135. doi: 10.1016/j.ajog.2011.09.006. [DOI] [PubMed] [Google Scholar]
- 3.Micheli K, Komninos I, Bagkeris E, Roumeliotaki T, Koutis A, Kogevinas M, Chatzi L. Sleep patterns in late pregnancy and risk of preterm birth and fetal growth restriction. Epidemiology. 2011;22(5):738–744. doi: 10.1097/EDE.0b013e31822546fd. [DOI] [PubMed] [Google Scholar]
- 4.Qiu C, Enquobahrie D, Frederick IO, Abetew D, Williams MA. Glucose intolerance and gestational diabetes risk in relation to sleep duration and snoring during pregnancy: a pilot study. BMC Women’s Health. 2010;10(1):17. doi: 10.1186/1472-6874-10-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zhong QY, Gelaye B, Sanchez SE, Williams MA. Psychometric Properties of the Pittsburgh Sleep Quality Index (PSQI) in a Cohort of Peruvian Pregnant Women. J Clin Sleep Med. 2015 Mar 9; doi: 10.5664/jcsm.4936. (Epub ahead of print) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gelaye B, Barrios YV, Zhong QY, Rondon MB, Borba CP, Sanchez SE, Henderson DC, Williams MA. Association of poor subjective sleep quality with suicidal ideation among pregnant Peruvian women. General Hospital Psychiatry. 2015 May 6; doi: 10.1016/j.genhosppsych.2015.04.014. (Epub ahead of print) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Skouteris H, Germano C, Wertheim EH, Paxton SJ, Milgrom J. Sleep quality and depression during pregnancy: a prospective study. Journal of Sleep Research. 2008;17(2):217–220. doi: 10.1111/j.1365-2869.2008.00655.x. [DOI] [PubMed] [Google Scholar]
- 8.Kotronoulas GC, Papadopoulou CN, Papapetrou A, Patiraki E. Psychometric evaluation and feasibility of the Greek Pittsburgh Sleep Quality Index (GR-PSQI) in patients with cancer receiving chemotherapy. Supportive Care in Cancer. 2011;19(11):1831–1840. doi: 10.1007/s00520-010-1025-4. [DOI] [PubMed] [Google Scholar]
- 9.Curcio G, Tempesta D, Scarlata S, Marzano C, Moroni F, Rossini PM, Ferrara M, De Gennaro L. Validity of the Italian version of the Pittsburgh sleep quality index (PSQI) Neurological Sciences. 2013;34(4):511–519. doi: 10.1007/s10072-012-1085-y. [DOI] [PubMed] [Google Scholar]
- 10.Doi Y, Minowa M, Uchiyama M, Okawa M, Kim K, Shibui K, Kamei Y. Psychometric assessment of subjective sleep quality using the Japanese version of the Pittsburgh Sleep Quality Index (PSQI-J) in psychiatric disordered and control subjects. Psychiatry Research. 2000;97(2–3):165–172. doi: 10.1016/s0165-1781(00)00232-8. [DOI] [PubMed] [Google Scholar]
- 11.Hita-Contreras F, Martínez-López E, Latorre-Román PA, Garrido F, Santos MA, Martínez-Amat A. Reliability and validity of the Spanish version of the Pittsburgh Sleep Quality Index (PSQI) in patients with fibromyalgia. Rheumatology International. 2014;34(7):929–936. doi: 10.1007/s00296-014-2960-z. [DOI] [PubMed] [Google Scholar]
- 12.Aloba OO, Adewuya AO, Ola BA, Mapayi BM. Validity of the Pittsburgh sleep quality index (PSQI) among Nigerian university students. Sleep Medicine. 2007;8(3):266–270. doi: 10.1016/j.sleep.2006.08.003. [DOI] [PubMed] [Google Scholar]
- 13.Beaudreau SA, Spira AP, Stewart A, Kezirian EJ, Lui L-Y, Ensrud K, Redline S, Ancoli-Israel S, Stone KL. Validation of the Pittsburgh Sleep Quality Index and the Epworth Sleepiness Scale in older black and white women. Sleep Med. 2012;13(1):36–42. doi: 10.1016/j.sleep.2011.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Burkhalter H, Sereika SM, Engberg S, WIRZ-JUSTICE A, Steiger J, De Geest S. Structure validity of the Pittsburgh Sleep Quality Index in renal transplant recipients: A confirmatory factor analysis. Sleep and Biological Rhythms. 2010;8(4):274–281. [Google Scholar]
- 15.Beck SL, Schwartz AL, Towsley G, Dudley W, Barsevick A. Psychometric evaluation of the Pittsburgh Sleep Quality Index in cancer patients. Journal of Pain and Symptom Management. 2004;27(2):140–148. doi: 10.1016/j.jpainsymman.2003.12.002. [DOI] [PubMed] [Google Scholar]
- 16.Carpenter JS, Andrykowski MA. Psychometric evaluation of the Pittsburgh sleep quality index. Journal of Psychosomatic Research. 1998;45(1):5–13. doi: 10.1016/s0022-3999(97)00298-5. [DOI] [PubMed] [Google Scholar]
- 17.Buysse DJ, Reynolds CF, III, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Research. 1989;28(2):193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- 18.Gelaye B, Lohsoonthorn V, Lertmeharit S, Pensuksan WC, Sanchez SE, Lemma S, Berhane Y, Zhu X, Vélez JC, Barbosa C, et al. Construct Validity and Factor Structure of the Pittsburgh Sleep Quality Index and Epworth Sleepiness Scale in a Multi-National Study of African, South East Asian and South American College Students. PLoS One. 2014;9(12):e116383. doi: 10.1371/journal.pone.0116383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jomeen J, Martin CR. Assessment and relationship of sleep quality to depression in early pregnancy. Journal of Reproductive and Infant Psychology. 2007;25(1):87–99. [Google Scholar]
- 20.Kirchmann M, Seven E, Bjornsson A, Bjornssdottir G, Gulcher JR, Stefansson K, Olesen J. Validation of the deCODE Migraine Questionnaire (DMQ3) for use in genetic studies. European Journal of Neurology. 2006;13(11):1239–1244. doi: 10.1111/j.1468-1331.2006.01491.x. [DOI] [PubMed] [Google Scholar]
- 21.Kroenke K, Spitzer RL, Williams JB. The PHQ-9. Journal of General Internal Medicine. 2001;16(9):606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Spitzer RL, Kroenke K, Williams JB Group PHQPCS. Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study. JAMA. 1999;282(18):1737–1744. doi: 10.1001/jama.282.18.1737. [DOI] [PubMed] [Google Scholar]
- 23.Zhong Q, Gelaye B, Fann JR, Sanchez SE, Williams MA. Cross-cultural validity of the Spanish version of PHQ-9 among pregnant Peruvian women: A Rasch item response theory analysis. Journal of Affective Disorders. 2014;158:148–153. doi: 10.1016/j.jad.2014.02.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zhong Q, Gelaye B, Rondon M, Sánchez ES, García JP, Sánchez E, Barrios VY, Simon EG, Henderson CD, May Cripe S. Comparative performance of Patient Health Questionnaire-9 and Edinburgh Postnatal Depression Scale for screening antepartum depression. Journal of Affective Disorders. 2014;162:1–7. doi: 10.1016/j.jad.2014.03.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lovibond PF. Long-term stability of depression, anxiety, and stress syndromes. Journal of Abnormal Psychology. 1998;107(3):520–526. doi: 10.1037//0021-843x.107.3.520. [DOI] [PubMed] [Google Scholar]
- 26.Lovibond PF, Lovibond SH. The structure of negative emotional states: comparison of the Depression Anxiety Stress Scales (DASS) with the Beck Depression and Anxiety Inventories. Behaviour Research and Therapy. 1995;33(3):335–343. doi: 10.1016/0005-7967(94)00075-u. [DOI] [PubMed] [Google Scholar]
- 27.World Health Orgnization. [Accessed on 07/14/2015];Global Database on Body Mass Index. Available at [ http://apps.who.int/bmi/index.jsp?introPage=intro_3.html.
- 28.Kaiser HF. The application of electronic computers to factor analysis. Educational and psychological measurement. 1960;20:141–151. [Google Scholar]
- 29.Brown TA. Confirmatory factor analysis for applied research. Guilford Press; New York, NY: 2012. [Google Scholar]
- 30.Cole JC, Motivala SJ, Buysse DJ, Oxman MN, Levin MJ, Irwin MR. Validation of a 3-factor scoring model for the Pittsburgh sleep quality index in older adults. Sleep. 2006;29(1):112–116. doi: 10.1093/sleep/29.1.112. [DOI] [PubMed] [Google Scholar]