Introduction
Basophils, the least abundant granulocyte, were first identified by Paul Ehrlich in 1879 based on their unique microscopic appearance [1]. As basophils comprise less than 1% of the peripheral leukocyte population, they were not extensively studied initially due to their rarity, despite their early discovery [2]. However, due to their morphologic and functional similarities to tissue-resident mast cells and their accessibility in the peripheral blood, basophils were employed as a tool to gain better insight into the function of mast cells. Thus, their unique functions were not appreciated for some time [3–5]. Seminal studies in the 1970s and 1980s identified basophils as orchestrators of anti-helminth immunity [6–10], however, defining the role of basophils in various disorders was difficult due to the lack of genetic models.
In the early 1980s, basophils were identified in mice [11,12], and the advent of transgenic mouse technology allowed for both the visualization and experimental manipulation of basophils in vivo [13–17]. Studies employing newly generated genetically modified mouse strains demonstrated that basophils critically contribute to anti-helminth immunity, allergic inflammation and the pathogenesis of various disorders in models of human disease [3,13–18]. Further, recent discoveries have uncovered previously unrecognized heterogeneity in basophil regulation and function. Two distinct basophil populations have been identified: (i) the classical interleukin (IL)-3-elicited basophils that are efficiently activated through immunoglobulin (Ig)E-dependent mechanisms and (ii) the recently identified thymic stromal lymphopoietin (TSLP)-elicited basophils that demonstrate IgE-independent mechanisms [3,19,20]. These two unique populations have been shown to have distinct regulatory mechanisms and unique functions in immunity and inflammation.
A number of recent reviews have highlighted the latest advances in our understanding of the broad contributions of basophils in the setting of protective immunity and pathologic inflammation [3,4,18,21–24]. Therefore, in this review, we will focus primarily on new findings with regard to basophil heterogeneity in the context of hematopoiesis, IgE- and cytokine-mediated regulation and activation, and how these findings define the role of basophils in the broader immune response.
Heterogeneity in Basophil Development
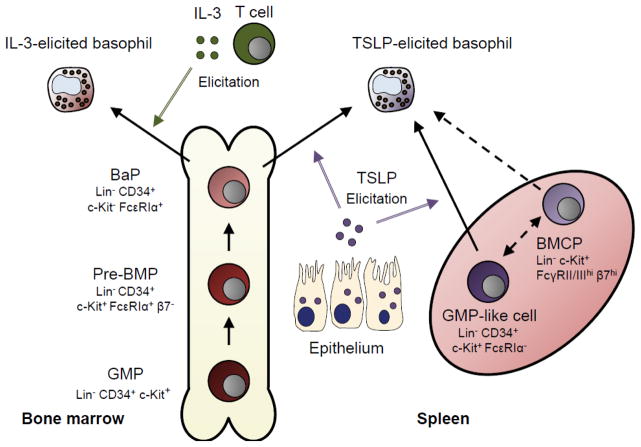
Basophils develop from hematopoietic stem cells and typically complete their differentiation in the bone marrow before entering the circulation as fully matured cells [24]. The earliest basophil precursors are hematopoietic stem cells (HSCs) that reside in the bone marrow and subsequently differentiate into granulocyte-monocyte precursors (GMPs). GMPs are devoid of common lineage markers for lymphocytes and granulocytes but do express the progenitor cell surface markers CD34 and c-Kit (CD117) [20]. Thus, they are defined as lineage-negative (Lin−) CD34+ c-Kit+ cells in the bone marrow (Fig. 1). In addition to their cell surface markers, GMPs express the transcription factor C/EBPα and have the potential to develop into other myeloid cell lineages including eosinophils, macrophages, mast cells and neutrophils [25]. During development, as C/EBPα expression decreases in a subset of GMPs, in conjunction with subsequent increased expression of the transcription factor GATA2, a shared basophil mast cell progenitor emerges [25,26]. More recently, GATA2 expression has been shown to be controlled by another transcription factor, IRF8, and furthermore, progenitor cells taken from Irf8−/− mice show reduced potential to generate basophils and mast cells in vitro [27]. Taken together, these studies outline a critical transcriptional program early in hematopoiesis that directs the development of basophils.
Figure 1. Medullary and extramedullary pathways of basophil development.
Basophils arise from progenitor populations in both the bone marrow and spleen. In the bone marrow, GMPs differentiate sequentially into pre-BMPs and BaPs prior to becoming fully differentiated basophils. Basophil development from bone marrow precursors has been shown to be regulated by both IL-3 and TSLP. The predominate source of IL-3 are activated T cells, while TSLP is predominately derived from epithelia. Splenic GMP-like cells have been shown to be a potent extramedullary source of basophils in response to TSLP (solid line). However, whether BMCPs arise from GMP-like cells and whether BMCPs give rise to basophils in vivo remains to be fully defined (dashed line).
GMP – granulocyte-monocyte progenitor. Pre-BMP – pre-basophil mast cell progenitor. BaP – basophil progenitor. BMCP – basophil mast cell common progenitor. TSLP – thymic stromal lymphopoietin.
Although GMPs typically reside in the bone marrow, the location and cell surface markers of a shared basophil and mast cell progenitor have been controversial. Arinobu et al. showed that in the spleen, a Lin− c-Kit+ FcγRII/IIIhi β7 integrinhi common basophil mast cell progenitor (BMCP) gives rise to populations resembling both basophils and mast cells in the presence of IL-3 (Fig. 1) [26]. In contrast, Mukai et al. demonstrated that these splenic BMCPs selectively differentiate into mast cells rather than basophils based on comprehensive analysis of cell surface markers and expression of basophil-associated genes such as Mcpt8 [28]. Thus, whether BMCPs are truly bipotent towards both basophil and mast cell lineages is unclear. Subsequently, Qi et al. identified a new population of FcεRIα+ β7− GMPs in the bone marrow that demonstrated bipotency and thus the ability to differentiate into both basophils and mast cells in the presence of IL-3 [29]. These cells were then defined formally as pre-basophil and mast cell progenitors (pre-BMPs), distinguishing them from β7hi BMCPs in the spleen (Fig. 1). As expected, pre-BMPs in the bone marrow could not differentiate into basophils or mast cells in the absence of GATA2 [30], and recent work has demonstrated the importance of the related transcription factor GATA1 [31], as well as STAT5 [30,32], in the continued differentiation of committed basophil progenitors (BaPs) (Fig. 1). Within this emerging area of basophil biology, these studies highlight that putative bipotent progenitors may exist in both the bone marrow (pre-BMPs) and the spleen (BMCPs).
In support of the existence of splenic basophil precursors, Siracusa et al. recently identified a multipotent GMP-like Lin− CD34+ c-Kit+ FcεRIα− cell population present in the spleen that can give rise to both basophils and mast cells in addition to other cell lineages (Fig. 1) [20]. These cells, like their medullary GMP counterparts, are Sca-1−/lo, FcγRII/III+ and express the TSLP receptor (TSLPR+) [20]. Whether BMCPs arise directly from this splenic GMP-like progenitor in a manner parallel to how pre-BMPs arise from GMPs in the bone marrow remains to be determined. In contrast to BMCP differentiation, which was induced IL-3, GMP-like cells undergo extramedullary hematopoiesis in response to the predominantly epithelial cell-derived cytokine TSLP [20]. The splenic TSLP-elicited GMP-like cells are distinguished from classical medullary GMPs by their elevated expression of Runx1 and C/EBPα, and their enhanced capacity to promote type-2 cytokine responses [20]. Specifically, these GMP-like cells give rise to more basophils than their bone marrow counterparts under identical in vitro conditions [20]. Thus, there appears to be conserved expression of specific transcription factors that promote basophil hematopoiesis, whether in the bone marrow or the spleen. However, how regulatory cytokines such as IL-3 and TSLP specifically modulate both medullary and extramedullary hematopoiesis remains an active area of investigation.
Classical Regulators of Basophil Function: IL-3 and IgE
The Role of IL-3 in Basophil Biology
The role of IL-3 as a growth and pro-survival factor of basophils has been well documented (Fig. 1) [32–35]. As IL-3 is predominantly produced by activated T cells [36], it plays an important role in promoting basophilia in the context of anti-helminth immunity to parasites such as Nippostrongylus brasiliensis and Strongyloides venezuelensis [32–34]. Further, IL-3Rα, a subunit of the IL-3 receptor (IL-3R), is one of the first markers expressed on basophils during fetal development, supporting its role in promoting basophil hematopoiesis [37]. Indeed, multiple in vitro studies have shown that increased numbers of basophils arise from bone marrow precursors in response to IL-3 (Fig. 1) [32–35]. In addition to growth, IL-3 increases basophil survival via NF-κB induction [38] and up-regulation of Pim1 [39]. Taken together, IL-3 is a critical and distinct hematopoietic growth and survival factor for basophils, resulting in enhanced basophil numbers both in vitro and in vivo.
IL-3 also plays a critical role in the induction of basophil effector function. For example, IL-3:IL-3R interactions activate the production of IL-4 in basophils via JAK2 and STAT5 signaling [35]. In addition to cytokine production, studies have shown that IL-3 promotes enhanced responsiveness of basophils to activation mediated by the high affinity IgE receptor FcεRI. For example, human basophils produce more IL-4 and IL-13 in response to IgE-mediated cross-linking in the presence of IL-3 [40,41]. Reciprocally, FcεRI signaling enhances responsiveness of basophils to IL-3. Although IL-3 alone can directly stimulate IL-4 production from basophils, FcεRI components are required for optimal IL-3:IL-3R signaling and production of IL-4 [42,43]. Thus, this coordinated integration of IL-3 and IgE signaling may allow for unique effector functions in a context-specific manner [44].
More recently, it has been recognized that basophil development and maturation can be regulated by microbial-derived signals in conjunction with IL-3 [45,46]. Hill et al. demonstrated that germ-free mice and mice with compromised microbial diversity induced by broad spectrum antibiotic treatment exhibited elevated systemic IgE levels and increased Il3ra expression on basophil progenitors, resulting in elevated numbers of peripheral blood basophils and enhanced susceptibility to allergic inflammation [45–49]. Basophils have also been shown to infiltrate the intestines of patients with inflammatory bowel disease (IBD) [50]. As IBD is widely associated with alterations in gut commensal microbiota and T cell dysregulation, dysbiosis may be driving the increased basophil responses in IBD patients in addition to IL-3 released by activated T cells [51]. Likewise, basophils have been shown to be dysregulated in the setting of asthma in humans [52–55], and new evidence suggests that exposure to rhinovirus, one of the most common triggers of asthma exacerbation [56], causes basophils from atopic individuals to become more responsive to IgE cross-linking [57]. Therefore, the effect of IL-3 on basophil growth, survival and activation may be influenced by commensal and/or pathogenic signals. Collectively, these studies demonstrate the dynamic network of potential interactions centered on IL-3-mediated regulation of basophil function.
Regulation of Basophils by IgE and Clinical Applications
The best studied mechanism of basophil activation is cross-linking of IgE with its high-affinity receptor FcεRI [58–61]. In response to IgE-mediated activation, basophils degranulate to rapidly release a variety of effector molecules such as histamine and adenosine triphosphate (ATP) [3,62]. In addition, IgE cross-linking can activate the production and release of other effector molecules such as IL-4, IL-13, leukotrienes and platelet activating factor [63]. Although FcεRI remains the canonical basophil Fc receptor, basophils also express other activating (FcγRIIA) and inhibitory (FcγRIIB) Fc receptors [64]. These receptors collectively signal through downstream Src family kinases Lyn, Fyn and Syk to induce a wide array of cellular changes [60]. Thus, the effects of IgE cross-linking likely depends on the coordinated action of a variety of cell surface signals [65–67].
Interest in how basophils are regulated by immunoglobulins has been spurred by exciting advances in new clinical therapies. One such advance is omalizumab (Xolair), a humanized monoclonal anti-IgE antibody used in the treatment of severe asthma [68,69] and chronic idiopathic urticaria (CIU) [70]. Although omalizumab’s efficacy is derived in part by its modulation of FcεRI+ mast cells, recent studies indicate that its influence on basophil function may be a relevant mechanism of action. Observations in patients have shown that omalizumab decreases free serum IgE levels, diminishes basophil numbers and lowers basophil expression of FcεRI [71–77]. All of these effects are thought to globally reduce basophil activation and may thus dampen allergic inflammation.
Allergic asthma, one of several defined subsets of asthma, is uniquely responsive to omalizumab therapy [68,69]. The condition is associated with increased production of type-2 cytokines such as IL-4, IL-5, IL-9 and IL-13, as well as elevated levels of IgE [52]. Additionally, asthma exacerbations in allergic asthma are mediated primarily by IgE-dependent activation of mast cells and possibly by basophils [52]. Although the role of basophils in human asthma is still unclear, their numbers in sputum and lung tissue correlate with disease severity and exacerbation [53–55]. Improvements in symptoms of asthma in response to omalizumab also correlate with reductions in blood basophil numbers and a decrease in the expression of FcεRI on basophils [72]. Similar to its efficacy in asthma, omalizumab is also effective in some patients with CIU, a disease that manifests as acute pruritic hives for more than six weeks without an identifiable cause [70]. A number of CIU patients have anti-FcεRI auto-antibodies that can bind FcεRI to activate its downstream signaling cascades [78]. In line with its ability to down-regulate FcεRI, these patients respond to treatment with omalizumab therapy [70,79]. Further, we would predict in this setting that IL-3-elicited basophils are the primary pathogenic basophil subset since basophils are known to be critical for the pathogenesis of IgE-mediated dermatitis in mice [19,80–82]. Whether omalizumab can improve outcomes in other IgE- and basophil-associated diseases such as food allergy is currently under investigation [83].
Despite its success in modulating pathogenic IgE-mediated basophil function, omalizumab is not an equally effective therapy for all subtypes of asthma including non-allergic asthma [84] and some subsets of CIU patients [78,79]. The diminished success of omalizumab in these settings may be due to the effects of TSLP and IgE-independent basophil-activating stimuli instead of the effects of IgE on classical IL-3-elicited basophils. Non-allergic asthma patients may have increased release of TSLP from their airway epithelium in response to airway trauma or infection [85], and similarly, TSLP levels are elevated in the lesions of some CIU patients [86]. Additionally, some CIU patients have basophils that do not release histamine in response to IgE cross-linking in vitro [78]. Importantly, TSLP-elicited murine basophils also show decreased histamine release in response to IgE-mediated activation suggesting additional routes of basophil activation in disease pathogenesis in addition to IL-3 and IgE [19]. Collectively, these studies highlight that IgE-mediated activation of basophils plays a critical role in some, but not all allergic disease states. However, the failure of anti-IgE therapy in many disorders associated with increased basophil infiltration suggests the presence of additional basophil subsets that can function independently of IgE.
In summary, IL-3 and IgE act in coordination on basophils to modulate their activation, function and survival. IL-3 is a key hematopoietic factor for basophils, and IgE-mediated activation is critical to many basophil responses. The importance of IgE signaling in various allergic disorders has made IgE an attractive therapeutic target that has been exploited by omalizumab. However, despite the broad success of omalizumab in asthma and CIU, some patients fail to respond to anti-IgE therapy. Further, less encouraging results have been demonstrated for omalizumab in the context of other allergic diseases associated with TSLP-elicited basophils, such as eosinophilic esophagitis (EoE) [87] and atopic dermatitis (AD) [88]. The differential effectiveness of omalizumab therapy across various diseases and disease subsets may be explained by the increased sensitivity of IL-3-elicited basophils to IgE-mediated cross-linking, as compared with TSLP-elicited basophils (discussed in further detail below). Ultimately, the identification of functionally distinct basophil populations may help us to understand how to more effectively target disease mediators such as IgE, IL-3 and TSLP.
TSLP-elicited Basophils: New Implications in Disease
Although the importance of IL-3 and IgE in basophil function has been appreciated for decades, recent studies have highlighted the emergence of a functionally distinct population of basophils that is elicited by TSLP [19,20,89–92]. Importantly, TSLP has been identified as a master initiator of type-2 immune responses [21,93], and TSLP polymorphisms have been positively associated with the pathogenesis of allergic disorders including AD [94], allergic rhinitis [95–97], asthma [98] and EoE [99,100]. As basophils have been associated with all of these diseases [3], a better understanding on how TSLP affects basophil development and activation is critical for the development of new targeted and effective therapeutics.
Similar to IL-3R, TSLPR is expressed on bone marrow basophil progenitors, and basophil numbers increase in response to TSLP both in vitro and in vivo [19,31]. In contrast to IL-3, culture of murine whole bone marrow with TSLP results in selective enrichment towards basophils rather than mast cells [19]. Additionally, culture of bone marrow from mice deficient in IL-3R with TSLP also yields high numbers of basophils [19]. Further, overexpression of TSLP in mice deficient in IL-3:IL-3R signaling also promotes basophil expansion in vivo. Thus, TSLP appears to be a critical developmental factor for basophil hematopoiesis (Fig. 1). While prior studies have demonstrated the importance of IL-3 in increasing basophil numbers to control Nippostrongylus brasiliensis and Strongyloides venezuelensis, recent studies have shown that peripheral basophilia after Trichuris muris [20] and Trichenella spiralis [91] infection is dependent on intact TSLP signaling. Taken together, both IL-3 and TSLP appear to be important in basophil development and anti-helminth immunity. However, how these cytokines elicit unique effector functions in a pathogen-specific manner remains an open area of investigation.
As discussed in previous sections, TSLP can induce basophil development from both bone marrow and splenic precursors (Fig. 1). High levels of circulating TSLP achieved by either injection of TSLP-cDNA plasmid or topical treatment with calcipotriol [101] promotes the differentiation of splenic GMP-like cells giving rise to multiple myeloid lineages including basophils (Fig. 1) [20]. Notably, the effects of TSLP on basophil development appear to be conserved in humans. Circulating CD34+ human hematopoietic progenitors express functional TSLPR [102]. These cells demonstrate higher expression of IL-5 and IL-13 in the sputum of asthmatic patients compared to similar cells from healthy controls, again suggesting the role of TSLP in biasing progenitor cells toward a type-2 immune response [103]. In fact, recent work has shown that TSLP enhances basophil production from these circulating CD34+ cells in vitro [104]. CD34+ progenitor cells give rise to more basophils when incubated with TSLP and IL-3 than with IL-3 alone as measured both by standard morphological approaches and by histamine content in culture [104]. Additionally, patients with active EoE demonstrate fewer GMP-like cells but more FcεRI+ granulocytes in esophageal biopsies compared to patients with inactive disease suggesting that, during a disease flare, GMP-like cells may have differentiated into pro-inflammatory granulocytes [20]. Likewise, patients with EoE that have a single nucleotide polymorphism in TSLP associated with increased TSLP expression have increased GMP-like cells in their peripheral blood [20]. Thus, TSLP may play an important role in both medullary and extramedullary hematopoiesis in both humans and mice.
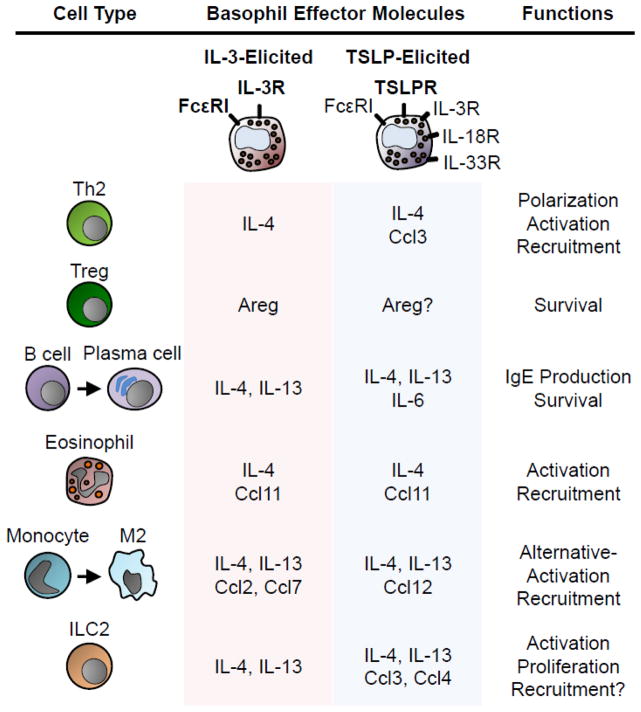
In addition to enhancing basophil numbers, TSLP elicits a population of basophils that has a distinct transcriptional profile compared to basophils elicited by IL-3 [19]. IL-3-elicited basophils have a higher surface expression of CD11b and CD62L (L-selectin), while TSLP-elicited basophils express more IL-3Rα, IL-18 receptor (IL-18R), and IL-33 receptor (IL-33R) (Fig. 2) [19]. The difference in surface protein expression suggests that these subsets of basophils have distinct effector functions. Indeed, basophils that are elicited by TSLP show increased expression of certain cytokines and chemokines in response to various stimuli compared to IL-3 elicited basophils. Stimulation of TSLP-elicited basophils with IL-18 or IL-33 results in expression of IL-4, IL-6, Ccl3, Ccl4, Ccl7, Ccl12 and Cxcl2 at higher levels compared to those elicited by IL-3 (Fig. 2). Further, basophils that were elicited by TSLP in culture did not degranulate efficiently when stimulated with IgE cross-linking compared to IL-3-elicited basophils. Gene set enrichment analysis of these two subsets of basophils revealed that TSLP-elicited basophils are enriched in expression of genes associated with linoleic and arachidonic acid metabolism as well as cell communication and adhesion molecules [19]. Linoleic acid and arachidonic acid are important inflammatory mediators, and both serve as precursors to effector molecules released from basophils like leukotrienes and prostaglandins [105]. IL-3 elicited basophils, in contrast, show enrichment of genes associated with TNF-α signaling, monocyte and dendritic cell maturation, and matrix metalloproteinase production [19]. Collectively, these studies highlight that TSLP induces a unique transcriptional program in basophils that results in the expression of distinct inflammatory cytokines, chemokines and effector molecules. However, how these differences influence distinct immune processes and human disease is an open area of inquiry.
Figure 2. Impacts of basophil heterogeneity on other immune cells.
IL-3 and TSLP program basophils to respond differentially to various stimuli including FcεRI cross-linking, IL-3, IL-18 and IL-33. In response to these stimuli, basophils release a wide variety of effector molecules that shape the immune response. Thus, the specific downstream cellular interactions of basophils with other immune cells are likely modulated by IL-3 or TSLP.
TSLP – thymic stromal lymphopoietin. Areg – amphiregulin.
In addition to TSLP, IL-33, another epithelial-derived cytokine that potently promotes type-2 cytokine responses and associated allergic inflammation, regulates basophil function in the context of allergy [106,107]. Genome wide association studies have positively linked IL-33 in addition to TSLP to several allergic conditions like AD, asthma and food allergy [108,109]. Systemic administration of IL-33 in mice has been shown to induce elevated numbers of basophils in the bone marrow through the induction of other hematopoietic factors [110]. In addition, IL-33R on mature basophils is up-regulated by both IL-3 [111] and TSLP [19]. IL-33 also has been shown to increase the responsiveness of basophils to IL-3-mediated activation as basophils that were first exposed to IL-33 produced more IL-4 and IL-13 upon subsequent challenge with IL-3 [111,112]. Likewise, human blood basophils increase their expression of IL-4, IL-5, IL-6, IL-8 and IL-13 when cultured with IL-33 [113], and surface expression of CD11b on basophils, important for adhesion and migration, is increased in response to IL-33 [111]. Therefore, epithelial cell-derived TSLP and IL-33 may direct basophils to peripheral epithelial tissues in contrast to T cell-derived IL-3 which has been shown to be important in directing basophils to lymph nodes [114]. Thus, both TSLP and IL-33 appear to activate basophil function in the setting of allergic diseases at various barrier surfaces.
As the TSLP-basophil axis has emerged as a unique and important pathway in basophil hematopoiesis and type-2 cytokine responses, we have gained a broader understanding of how IgE may have differential effects on basophil function. The observation that TSLP-elicited basophils are less responsive to IgE cross-linking may, in part, explain why TSLP-mediated allergic disease states are less responsive to IgE blockade. For example, EoE, a food allergy-associated inflammatory disease characterized by esophageal eosinophilia, has been linked to polymorphisms in TSLP [94,99,100]. Strikingly, elevated esophageal TSLP expression levels correlate with increased numbers of infiltrating basophils in the biopsy during active disease in comparison to inactive disease periods [90]. Although EoE is often associated with elevated IgE levels [115,116], omalizumab treatment appears to have limited efficacy in the induction of EoE remission with regard to both histologic features of tissue eosinophil infiltration and clinical disease activity [87,117,118]. One possible explanation could be that the TSLP-basophil axis is particularly potent in the setting of EoE, such that IgE-independent processes drive disease pathogenesis. Indeed, a recent study employing a murine model of EoE associated with elevated TSLP expression demonstrated that although TSLP and basophils played a critical role in EoE pathogenesis, IgE was dispensable for disease [90]. Taken together, these studies suggest that the level of polarization towards TSLP-elicited basophils may explain the differential clinical responses to IgE-based therapies in the context of allergic inflammatory disorders.
The critical role of TSLP-elicited basophils in IgE-independent allergic diseases makes anti-TSLP therapy an attractive treatment modality to complement omalizumab therapy. Anti-TSLP biologics have recently shown promise in treating asthma [119], and studies in other allergic diseases including AD and EoE are warranted as murine models of these disorders improve with anti-TSLP treatment [19,90]. Future decisions on whether patients will benefit from anti-IgE, anti-TSLP or a combination of both therapies may ultimately be dictated by the unique composition of basophil subsets driving their allergic disease.
Impacts of Basophil Heterogeneity on Other Immune Cells
Advances in our understanding of basophil heterogeneity are beginning to paint a more complete picture of helminth immunity and allergic diseases. Although commonly associated with IgE responses, many allergic disorders demonstrate IgE-independent processes, and the identification of TSLP-elicited basophils has helped to shed light on how IgE-independent basophil pathways may regulate various disease states. In addition to their differential development and cytokine production, the cellular interactions mediated by different basophil effector programs are currently an active area of investigation.
T cells
Due to the ability of basophils to enhance their expression of IL-4 in response to various stimuli such as IL-3 and TSLP, they have been the subject of intense investigation in terms of their ability to promote the polarization of naïve T cells towards T helper type 2 (Th2) cells (Fig. 2) [17,120–125]. Although basophils have proven to act as sole Th2-inducing antigen presenting cells (APCs) in some experimental model systems, basophils are likely to work in conjunction with dendritic cells (DCs) to initiate optimal Th2 responses [120,122,126,127]. In vitro data show that basophils can stimulate T cells with OVA peptide, but not whole OVA protein, resulting in increased IL-4 expression from CD4+ T cells as wells as increased proliferation [122]. Further, in a model of hapten-induced dermatitis using topical oxazolone, basophils were shown to be critical to initiating the inflammatory response and clustered with T cells in the skin draining lymph nodes [122]. Much like acquired peptide antigens, these studies show that haptens may bind directly to peptides in MHC class II molecules on basophils to facilitate their presentation to T cells [122]. In this model, basophils expressed other co-stimulatory molecules including CD40, CD80 and CD86 to increase T cell responses after repeated hapten application [122]. Therefore, despite lacking the ability to process whole proteins, basophils appear to have the ability to induce Th2 responses in response to some peptides and haptens.
Topical application of oxazalone as well as calcipotriol results in increased TSLP expression in the skin [89,122]. Given the unique chemokine profile of TSLP-elicited basophils, these cells may play an important role in optimal trafficking of Th2 cells. For example, Th2 cells preferentially express the chemokine receptor Ccr4 over other T cell subsets [128]. One of the ligands for Ccr4, Ccl3, is significantly induced when TSLP-elicited basophils are activated with IL-3, IL-18 or IL-33, as compared to IL-3-elicited basophils (Fig. 2) [19]. In models of asthma and lung infection with Nippostrongylus brasiliensis, CD4+ T cells had prolonged interactions with basophils in peripheral tissues while interactions in lymph nodes were much briefer [17]. Therefore, in addition to promoting optimal Th2 polarization, TSLP-elicited basophils may be critical in directing Th2 cells to peripheral sites.
In addition to their pro-inflammatory effects, basophils may also act in an anti-inflammatory manner through their expression of epidermal growth factor amphregulin (Areg) which has been shown to support regulatory T cell responses (Tregs) (Fig. 2) [129,130]. A recent paper demonstrated that ultraviolet B (UVB) irradiation, a therapy used to treat inflammatory skin conditions such as AD and psoriasis, can protect mice from dinitrofluorobenzene (DNFB)-induced contact hypersensitivity in a Treg-dependent manner [131]. In this model, proper Treg function required basophil-derived Areg [131]. Further, it has been shown that IL-3 induces more basophil-derived Areg production than IgE [132], suggesting differential regulation of this anti-inflammatory function and a possible role of basophil heterogeneity. However, whether TSLP differentially modulates Areg production from basophils remains to be tested. Ultimately, how basophils interact with a variety of different T cell populations is a complex balance of pro- and anti-inflammatory pathways that likely depend on specific signals modulating basophil responses.
B cells
Basophils exert most of their influence on B cells through IL-4 and IL-13 signaling cascades, which drive B cells to undergo class switching to produce various antibody isotypes including IgE (Fig. 2) [133]. Further, basophil-derived IL-4 and IL-6 play an important role in B cell and plasma cell differentiation and survival in coordination with CD4+ T cells [134–136]. As TSLP-elicited basophils produce more IL-4 and IL-6 after stimulation with IL-33 compared to IL-3-elicited basophils [19], the combination of TSLP and IL-33 may synergistically activate IgE production in the setting of allergic disease states. However, the precise contributions of IL-33 in the modulation of the basophil-B cell axis remains to be fully defined.
Antigen-specific IgE is clearly linked to the development of food allergies, and the importance of basophils in shaping B cell IgE production has been well established [90,92,108,124]. Additionally, AD in childhood, which is associated with elevated TSLP expression and heightened basophil responses in humans, is an independent risk factor for the development of food allergies later in life [137]. Indeed, recent studies have raised the concern that children with AD may become epicutaneously sensitized to common food allergens [92,138]. In support of this, studies in mice have shown the importance of TSLP-elicited basophil responses in the pathogenesis of IgE-mediated food hypersensitivity [92]. Allergen sensitization on a developing AD-like skin lesion resulted in food-induced allergic intestinal inflammation upon oral allergen re-exposure [92,138]. Additionally, intradermal injection of TSLP-elicited basophils into naïve mice in the presence of topical allergens showed that basophils are sufficient to induce food allergy upon subsequent oral allergen challenge [92]. Due to their limited ability to process large antigens, basophils most likely work in coordination with T cells and DCs to shape B cell responses in this setting [122,138]. However, whether basophils directly or indirectly modulate B cell function in various allergic disease states remains to be determined.
Eosinophils
Basophils have been implicated as key orchestrators of the eosinophil response in both chronic allergic conditions and helminth infections [80,139–142]. Indeed, eosinophils are often found in biopsies of asthma and AD patients, and depletion of basophils resulted in a decrease in the number of eosinophils in a mouse model of AD [142]. Chemokine responses in eosinophils are primarily mediated by Ccr3 [143], and basophils produce the Ccr3 ligand Ccl11 (eotaxin-1) when stimulated with IL-3 [19]. Other groups have described basophils acting through fibroblasts to recruit eosinophils via the induction of Ccl5, another Ccr3 ligand [141]. Additionally, basophils have been shown to activate eosinophils in vitro as measured by eosinophil up-regulation of CD54 (ICAM-1), CD69 and CD86 [141]. Therefore, early basophil entry into tissues may set the stage for chronic immune responses that include activation and recruitment of eosinophils.
Beyond the expression of chemokines, a recent study has demonstrated that basophil-derived IL-4 increases expression of cell adhesion molecules on endothelia, which in turn allows for the entry of other effector cells into tissue including eosinophils [142]. Specifically, Cheng et al. found that IgE-activated basophils induce expression of vascular cell adhesion molecule-1 (VCAM-1) on endothelial cells, which in turn activates the recruitment of eosinophils to the inflamed tissue [142]. Although these studies demonstrated the role basophils play in recruiting eosinophils, basophils likely recruit other leukocytes in a similar way via the regulation of adhesion molecules on endothelial cells. However, whether TSLP-elicited basophils regulate endothelial function to recruit distinct immune cells from IL-3-elicited basophils remains to be determined.
Monocytes and macrophages
Monocytes and macrophages are also influenced by IL-4 and IL-13 from basophils in allergic diseases (Fig. 2) [81,82,144]. Macrophages undergo alternative activation in the presence of IL-4 or IL-13 which is characterized by increased expression of signature genes including Arginase-I, chitinase-like molecules and resistin-like molecule α (Relmα). Alternatively activated macrophages (referred to as M2 macrophages) are classically believed to be anti-inflammatory in function and also increase their surface expression of CD206, CD301, MHC class II molecules and PD-L2 [144–148]. Basophils, as a potent source of IL-4, are critical for M2 macrophage polarization in allergic and infectious settings in a STAT6-dependent manner [81,82,149]. Indeed, recent studies employing an IgE-dependent model of chronic allergic dermatitis demonstrated that basophil-derived IL-4 plays a key role in the differentiation of Ccr2+ monocytes in the skin to anti-inflammatory M2 macrophages to dampen skin inflammation [81,82]. The recruitment of monocytes was found to be critically dependent on Ccr2, which has several ligands including Ccl2, Ccl7 and Ccl12 [150]. IL-3-elicited basophils produce more Ccl2 and Ccl7 after stimulation with IL-3, IL-18 or IL-33 while TSLP-elicited basophils produce more Ccl12 [19]. Thus, it is possible that basophil heterogeneity may have a fundamental impact on monocyte and macrophage recruitment and polarization states. Given the IgE-dependence of the model of chronic allergic dermatitis, the basophils mediating M2 polarization in this context are likely IL-3-elicited. However, whether TSLP elicits a different basophil-M2 axis remains an open question. Indeed, TSLP has been shown to potently activate M2 polarization in the setting of a murine model of asthma in an IL-4-independent but IL-13-dependent manner [146]. In this setting, M2 macrophages were found to be pro-inflammatory rather than anti-inflammatory [146]. Thus, depending on whether basophils are IL-3-elicited or TSLP-elicited, their effect on M2 macrophage differentiation and function may be either anti-inflammatory or pro-inflammatory, respectively. Newer studies in macrophage biology are extending our interpretation of macrophage polarization to view M2 macrophages as having diverse activation states and functions [151]. Thus, further investigations into the effects of the basophil-M2 axis on inflammation are likely to yield broader insight into macrophage functions.
Innate lymphoid cells
Group 2 ILCs (ILC2s) are a rare population of innate immune cells that produce type 2 cytokines which in turn augment anti-helminth immunity and allergic inflammation in a number of settings [52,152–154]. Recently, the importance of the basophil-ILC2 axis has been demonstrated in various allergic disease states [89,153,155]. For example, ILC2s are thought to play an important role in some subsets of asthma [52,153], and basophils activate lung ILC2 in models of asthma via IL-4. In response to IL-4, ILC2s release IL-5, IL-9, IL-13, Ccl3, Ccl5 and Ccl11 which can drive the expansion and recruitment of eosinophils and other effector cells to promote chronic inflammation [155]. Therefore, ILC2s are critical in amplifying the effects of basophils on additional effector cells by their potent production of cytokines and chemokines.
Similar results have been found in AD. Basophils and ILC2s are increased in lesional AD skin compared to healthy human control skin, and imaging studies of the skin have demonstrated that ILC2s cluster in close proximity to basophils in lesional skin [89]. Studies employing a murine model of AD-like disease further demonstrated that TSLP-elicited basophils critically influence ILC2 responses in the skin via IL-4 signaling (Fig. 2) [89]. Further, IL-3, IL-18 and IL-33 induce high levels of Ccl3 and Ccl4 from TSLP-elicited basophils as compared to IL-3-elicited basophils (Fig. 2) [19]. The receptors for these chemokines, Ccr4 and Ccr5, are enriched on ILC2s [156], suggesting that TSLP-elicited basophils may efficiently recruit ILC2s to mucosal tissues in allergic diseases such as AD or asthma. However, future studies will be required to definitively establish basophils as mediators of ILC2 chemotaxis.
In addition to activation and potential recruitment, basophils play a key role in driving ILC2 proliferation in models of both AD and asthma. Ex vivo experiments have shown that TSLP-elicited basophils can promote proliferation of ILC2s via IL-4 signaling (Fig. 2) [89]. Further, in a model of asthma, mice reconstituted with IL-4 deficient basophils had fewer ILC2s in the lung tissue demonstrating that IL-4 from basophils is necessary in optimal ILC2 expansion in vivo [155]. Collectively, these studies demonstrate that basophils influence ILC2 function in a variety of different ways across multiple barrier surfaces. Interrupting the basophil-ILC2 axis in allergic disorders via disruption of IL-4 signaling may be an important therapeutic target. In fact, recent trials with dupilumab, a monoclonal antibody to a subunit of the IL-4 receptor (IL-4Rα), in asthma and AD have shown promising disease limiting results [157–159]. Whether these interventions result in decreased ILC2, basophil or other effector cell numbers and whether these effects are the relevant therapeutic mechanism of dupilumab in patients both remain to be tested.
Concluding Remarks
Once thought to be a redundant effector cell, basophils continue to gain more appreciation for their role in a wide variety of disease states, and studies have now shown that basophils are much more complex than previously recognized. Currently, two distinct phenotypes of basophils have been defined based on their developmental pathways and effector profile: (i) IL-3-elicited basophils and (ii) TSLP-elicited basophils. This conceptual advance has allowed us to better understand how various allergic disease states may respond to therapies such as anti-IgE treatment. Specifically, certain diseases may respond more robustly to anti-IgE therapy (e.g, food allergy and urticarial), while others may respond more to anti-TSLP therapy (AD and EoE). In the setting of asthma, it appears that certain subsets respond to IgE while others respond to anti-TSLP treatment [83,119]. Thus, a deeper understanding of basophil biology may help us to better direct future treatments in allergic diseases.
References
- 1.Ehrlich P. Beiträge zur Theorie und Praxis der Histologischen Färbung. Leipzig University; 1878. [Google Scholar]
- 2.Ishizaka T, De Bernardo R, Tomioka H, Lichtenstein LM, Ishizaka K. Identification of basophil granulocytes as a site of allergic histamine release. J Immunol Baltim Md 1950. 1972;108:1000–1008. [PubMed] [Google Scholar]
- 3.Siracusa MC, Kim BS, Spergel JM, Artis D. Basophils and allergic inflammation. J Allergy Clin Immunol. 2013;132:789–801. doi: 10.1016/j.jaci.2013.07.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Crivellato E, Nico B, Ribatti D. The history of the controversial relationship between mast cells and basophils. Immunol Lett. 2011;141:10–17. doi: 10.1016/j.imlet.2011.06.008. [DOI] [PubMed] [Google Scholar]
- 5.Schroeder JT. Basophils beyond effector cells of allergic inflammation. Adv Immunol. 2009;101:123–161. doi: 10.1016/S0065-2776(08)01004-3. [DOI] [PubMed] [Google Scholar]
- 6.Ogilvie BM, Hesketh PM, Rose ME. Nippostrongylus brasiliensis: peripheral blood leucocyte response of rats, with special reference to basophils. Exp Parasitol. 1978;46:20–30. doi: 10.1016/0014-4894(78)90153-4. [DOI] [PubMed] [Google Scholar]
- 7.Ogilvie BM, Askenase PW, Rose ME. Basophils and eosinophils in three strains of rats and in athymic (nude) rats following infection with the nematodes Nippostrongylus brasiliensis or Trichinella spiralis. Immunology. 1980;39:385–389. [PMC free article] [PubMed] [Google Scholar]
- 8.Roth RL, Levy DA. Nippostrongylus brasiliensis: Peripheral leukocyte responses and correlation of basophils with blood histamine concentration during infection in rats. Exp Parasitol. 1980;50:331–341. doi: 10.1016/0014-4894(80)90036-3. [DOI] [PubMed] [Google Scholar]
- 9.Rothwell TL. Studies of the responses of basophil and eosinophil leucocytes and mast cells to the nematode Trichostrongylus colubriformis. I. Observations during the expulsion of first and second infections by guinea-pigs. J Pathol. 1975;116:51–60. doi: 10.1002/path.1711160109. [DOI] [PubMed] [Google Scholar]
- 10.Rothwell TLW, Dineen JK. Cellular reactions in guinea-pigs following primary and challenge infection with Trichostrongylus colubriformis with special reference to the roles played by eosinophils and basophils in rejection of the parasite. Immunology. 1972;22:733–745. [PMC free article] [PubMed] [Google Scholar]
- 11.Dvorak AM, Nabel G, Pyne K, Cantor H, Dvorak HF, Galli SJ. Ultrastructural identification of the mouse basophil. Blood. 1982;59:1279–1285. [PubMed] [Google Scholar]
- 12.Schrader JW, Lewis SJ, Clark-Lewis I, Culvenor JG. The persisting (P) cell: histamine content, regulation by a T cell-derived factor, origin from a bone marrow precursor, and relationship to mast cells. Proc Natl Acad Sci. 1981;78:323–327. doi: 10.1073/pnas.78.1.323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Voehringer D, Shinkai K, Locksley RM. Type 2 immunity reflects orchestrated recruitment of cells committed to IL-4 production. Immunity. 2004;20:267–277. doi: 10.1016/s1074-7613(04)00026-3. [DOI] [PubMed] [Google Scholar]
- 14.Min B, Prout M, Hu-Li J, Zhu J, Jankovic D, Morgan ES, et al. Basophils produce IL-4 and accumulate in tissues after infection with a Th2-inducing parasite. J Exp Med. 2004;200:507–517. doi: 10.1084/jem.20040590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sawaguchi M, Tanaka S, Nakatani Y, Harada Y, Mukai K, Matsunaga Y, et al. Role of mast cells and basophils in IgE responses and in allergic airway hyperresponsiveness. J Immunol. 2012;188:1809–1818. doi: 10.4049/jimmunol.1101746. [DOI] [PubMed] [Google Scholar]
- 16.Wada T, Ishiwata K, Koseki H, Ishikura T, Ugajin T, Ohnuma N, et al. Selective ablation of basophils in mice reveals their nonredundant role in acquired immunity against ticks. J Clin Invest. 2010;120:2867–2875. doi: 10.1172/JCI42680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sullivan BM, Liang H-E, Bando JK, Wu D, Cheng LE, McKerrow JK, et al. Genetic analysis of basophil function in vivo. Nat Immunol. 2011;12:527–535. doi: 10.1038/ni.2036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Karasuyama H, Yamanishi Y. Basophils have emerged as a key player in immunity. Curr Opin Immunol. 2014;31:1–7. doi: 10.1016/j.coi.2014.07.004. [DOI] [PubMed] [Google Scholar]
- 19.Siracusa MC, Saenz SA, Hill DA, Kim BS, Headley MB, Doering TA, et al. TSLP promotes interleukin-3-independent basophil haematopoiesis and type 2 inflammation. Nature. 2011;477:229–233. doi: 10.1038/nature10329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Siracusa MC, Saenz SA, Tait Wojno ED, Kim BS, Osborne LC, Ziegler CG, et al. Thymic stromal lymphopoietin-mediated extramedullary hematopoiesis promotes allergic inflammation. Immunity. 2013;39:1158–1170. doi: 10.1016/j.immuni.2013.09.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hammad H, Lambrecht BN. Barrier epithelial cells and the control of type 2 immunity. Immunity. 2015;43:29–40. doi: 10.1016/j.immuni.2015.07.007. [DOI] [PubMed] [Google Scholar]
- 22.Pulendran B, Artis D. New paradigms in type 2 immunity. Science. 2012;337:431–435. doi: 10.1126/science.1221064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Schwartz C, Eberle JU, Voehringer D. Basophils in inflammation. Eur J Pharmacol. 2015 doi: 10.1016/j.ejphar.2015.04.049. [DOI] [PubMed] [Google Scholar]
- 24.Voehringer D. Protective and pathological roles of mast cells and basophils. Nat Rev Immunol. 2013;13:362–375. doi: 10.1038/nri3427. [DOI] [PubMed] [Google Scholar]
- 25.Iwasaki H, Mizuno S, Arinobu Y, Ozawa H, Mori Y, Shigematsu H, et al. The order of expression of transcription factors directs hierarchical specification of hematopoietic lineages. Genes Dev. 2006;20:3010–3021. doi: 10.1101/gad.1493506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Arinobu Y, Iwasaki H, Gurish MF, Mizuno S, Shigematsu H, Ozawa H, et al. Developmental checkpoints of the basophil/mast cell lineages in adult murine hematopoiesis. Proc Natl Acad Sci. 2005;102:18105–18110. doi: 10.1073/pnas.0509148102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sasaki H, Kurotaki D, Osato N, Sato H, Sasaki I, Koizumi S, et al. Transcription factor IRF8 plays a critical role in the development of murine basophils and mast cells. Blood. 2015;125:358–369. doi: 10.1182/blood-2014-02-557983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mukai K, BenBarak MJ, Tachibana M, Nishida K, Karasuyama H, Taniuchi I, et al. Critical role of P1-Runx1 in mouse basophil development. Blood. 2012;120:76–85. doi: 10.1182/blood-2011-12-399113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Qi X, Hong J, Chaves L, Zhuang Y, Chen Y, Wang D, et al. Antagonistic regulation by the transcription factors C/EBPα and MITF specifies basophil and mast cell fates. Immunity. 2013;39:97–110. doi: 10.1016/j.immuni.2013.06.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Li Y, Qi X, Liu B, Huang H. The STAT5–GATA2 pathway is critical in basophil and mast cell differentiation and maintenance. J Immunol. 2015;194:4328–4338. doi: 10.4049/jimmunol.1500018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Nei Y, Obata-Ninomiya K, Tsutsui H, Ishiwata K, Miyasaka M, Matsumoto K, et al. GATA-1 regulates the generation and function of basophils. Proc Natl Acad Sci. 2013;110:18620–18625. doi: 10.1073/pnas.1311668110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ohmori K, Luo Y, Jia Y, Nishida J, Wang Z, Bunting KD, et al. IL-3 induces basophil expansion in vivo by directing granulocyte-monocyte progenitors to differentiate into basophil lineage-restricted progenitors in the bone marrow and by increasing the number of basophil/mast cell progenitors in the spleen. J Immunol. 2009;182:2835–2841. doi: 10.4049/jimmunol.0802870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lantz CS, Boesiger J, Song CH, Mach N, Kobayashi T, Mulligan RC, et al. Role for interleukin-3 in mast-cell and basophil development and in immunity to parasites. Nature. 1998;392:90–93. doi: 10.1038/32190. [DOI] [PubMed] [Google Scholar]
- 34.Shen T, Kim S, Do J, Wang L, Lantz C, Urban JF, et al. T cell-derived IL-3 plays key role in parasite infection-induced basophil production but is dispensable for in vivo basophil survival. Int Immunol. 2008;20:1201–1209. doi: 10.1093/intimm/dxn077. [DOI] [PubMed] [Google Scholar]
- 35.Voehringer D. Basophil modulation by cytokine instruction. Eur J Immunol. 2012;42:2544–2550. doi: 10.1002/eji.201142318. [DOI] [PubMed] [Google Scholar]
- 36.Schroeder JT, Chichester KL, Bieneman AP. Human basophils secrete IL-3: evidence of autocrine priming for phenotypic and functional responses in allergic disease. J Immunol. 2009;182:2432–2438. doi: 10.4049/jimmunol.0801782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ohnmacht C, Voehringer D. Basophil effector function and homeostasis during helminth infection. Blood. 2009;113:2816–2825. doi: 10.1182/blood-2008-05-154773. [DOI] [PubMed] [Google Scholar]
- 38.Zheng X, Karsan A, Duronio V, Chu F, Walker DC, Bai TR, et al. Interleukin-3, but not granulocyte-macrophage colony-stimulating factor and interleukin-5, inhibits apoptosis of human basophils through phosphatidylinositol 3-kinase: requirement of NF-kappaB-dependent and -independent pathways. Immunology. 2002;107:306–315. doi: 10.1046/j.1365-2567.2002.01517.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Didichenko SA, Spiegl N, Brunner T, Dahinden CA. IL-3 induces a Pim1-dependent antiapoptotic pathway in primary human basophils. Blood. 2008;112:3949–3958. doi: 10.1182/blood-2008-04-149419. [DOI] [PubMed] [Google Scholar]
- 40.Gibbs BF, Haas H, Falcone FH, Albrecht C, Vollrath IB, Noll T, et al. Purified human peripheral blood basophils release interleukin-13 and preformed interleukin-4 following immunological activation. Eur J Immunol. 1996;26:2493–2498. doi: 10.1002/eji.1830261033. [DOI] [PubMed] [Google Scholar]
- 41.MacGlashan D, White JM, Huang SK, Ono SJ, Schroeder JT, Lichtenstein LM. Secretion of IL-4 from human basophils. The relationship between IL-4 mRNA and protein in resting and stimulated basophils. J Immunol. 1994;152:3006–3016. [PubMed] [Google Scholar]
- 42.Hida S, Yamasaki S, Sakamoto Y, Takamoto M, Obata K, Takai T, et al. Fc receptor γ-chain, a constitutive component of the IL-3 receptor, is required for IL-3-induced IL-4 production in basophils. Nat Immunol. 2009;10:214–222. doi: 10.1038/ni.1686. [DOI] [PubMed] [Google Scholar]
- 43.Kamijo S, Nunomura S, Ra C, Kanaguchi Y, Suzuki Y, Ogawa H, et al. Innate basophil IL-4 responses against allergens, endotoxin, and cytokines require the Fc receptor γ-chain. J Allergy Clin Immunol. 2015 doi: 10.1016/j.jaci.2015.10.037. [DOI] [PubMed] [Google Scholar]
- 44.Bezbradica JS, Rosenstein RK, DeMarco RA, Brodsky I, Medzhitov R. A role for the ITAM signaling module in specifying cytokine-receptor functions. Nat Immunol. 2014;15:333–342. doi: 10.1038/ni.2845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Hill DA, Siracusa MC, Abt MC, Kim BS, Kobuley D, Kubo M, et al. Commensal bacteria-derived signals regulate basophil hematopoiesis and allergic inflammation. Nat Med. 2012;18:538–546. doi: 10.1038/nm.2657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Hill DA, Artis D. The influence of commensal bacteria-derived signals on basophil-associated allergic inflammation. Gut Microbes. 2013;4:76–83. doi: 10.4161/gmic.22759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Cahenzli J, Köller Y, Wyss M, Geuking MB, McCoy KD. Intestinal microbial diversity during early-life colonization shapes long-term IgE levels. Cell Host Microbe. 2013;14:559–570. doi: 10.1016/j.chom.2013.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Herbst T, Sichelstiel A, Schär C, Yadava K, Bürki K, Cahenzli J, et al. Dysregulation of allergic airway inflammation in the absence of microbial colonization. Am J Respir Crit Care Med. 2011;184:198–205. doi: 10.1164/rccm.201010-1574OC. [DOI] [PubMed] [Google Scholar]
- 49.Ohnmacht C, Park J-H, Cording S, Wing JB, Atarashi K, Obata Y, et al. The microbiota regulates type 2 immunity through RORγt+ T cells. Science. 2015;349:989–993. doi: 10.1126/science.aac4263. [DOI] [PubMed] [Google Scholar]
- 50.Chapuy L, Bsat M, Mehta H, Rubio M, Wakahara K, Van VQ, et al. Basophils increase in Crohn disease and ulcerative colitis and favor mesenteric lymph node memory TH17/TH1 response. J Allergy Clin Immunol. 2014;134:978–981. doi: 10.1016/j.jaci.2014.05.025. [DOI] [PubMed] [Google Scholar]
- 51.Rodriguez Gomez M, Talke Y, Hofmann C, Ketelsen I, Hermann F, Reich B, et al. Basophils control T-cell responses and limit disease activity in experimental murine colitis. Mucosal Immunol. 2014;7:188–199. doi: 10.1038/mi.2013.38. [DOI] [PubMed] [Google Scholar]
- 52.Lambrecht BN, Hammad H. The immunology of asthma. Nat Immunol. 2015;16:45–56. doi: 10.1038/ni.3049. [DOI] [PubMed] [Google Scholar]
- 53.Kimura I, Tanizaki Y, Saito K, Takahashi K, Ueda N, Sato S. Appearance of basophils in the sputum of patients with bronchial asthma. Clin Allergy. 1975;5:95–98. doi: 10.1111/j.1365-2222.1975.tb01840.x. [DOI] [PubMed] [Google Scholar]
- 54.Kepley CL, McFeeley PJ, Oliver JM, Lipscomb MF. Immunohistochemical detection of human basophils in postmortem cases of fatal asthma. Am J Respir Crit Care Med. 2001;164:1053–1058. doi: 10.1164/ajrccm.164.6.2102025. [DOI] [PubMed] [Google Scholar]
- 55.Koshino T, Teshima S, Fukushima N, Takaishi T, Hirai K, Miyamoto Y, et al. Identification of basophils by immunohistochemistry in the airways of post-mortem cases of fatal asthma. Clin Exp Allergy. 1993;23:919–925. doi: 10.1111/j.1365-2222.1993.tb00276.x. [DOI] [PubMed] [Google Scholar]
- 56.Duff AL, Pomeranz ES, Gelber LE, Price GW, Farris H, Hayden FG, et al. Risk factors for acute wheezing in infants and children: viruses, passive smoke, and IgE antibodies to inhalant allergens. Pediatrics. 1993;92:535–540. [PubMed] [Google Scholar]
- 57.Agrawal R, Wisniewski J, Yu MD, Kennedy JL, Platts-Mills T, Heymann PW, et al. Infection with human rhinovirus 16 promotes enhanced IgE responsiveness in basophils of atopic asthmatics. Clin Exp Allergy. 2014;44:1266–1273. doi: 10.1111/cea.12390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Kinet JP. The high-affinity IgE receptor (Fc epsilon RI): from physiology to pathology. Annu Rev Immunol. 1999;17:931–972. doi: 10.1146/annurev.immunol.17.1.931. [DOI] [PubMed] [Google Scholar]
- 59.Kraft S, Kinet J-P. New developments in FcεRI regulation, function and inhibition. Nat Rev Immunol. 2007;7:365–378. doi: 10.1038/nri2072. [DOI] [PubMed] [Google Scholar]
- 60.Bruhns P, Jönsson F. Mouse and human FcR effector functions. Immunol Rev. 2015;268:25–51. doi: 10.1111/imr.12350. [DOI] [PubMed] [Google Scholar]
- 61.Galli SJ, Tsai M. IgE and mast cells in allergic disease. Nat Med. 2012;18:693–704. doi: 10.1038/nm.2755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Tsai SH, Kinoshita M, Kusu T, Kayama H, Okumura R, Ikeda K, et al. The ectoenzyme E-NPP3 negatively regulates ATP-dependent chronic allergic responses by basophils and mast cells. Immunity. 2015;42:279–293. doi: 10.1016/j.immuni.2015.01.015. [DOI] [PubMed] [Google Scholar]
- 63.Broide DH. Molecular and cellular mechanisms of allergic disease. J Allergy Clin Immunol. 2001;108:S65–S71. doi: 10.1067/mai.2001.116436. [DOI] [PubMed] [Google Scholar]
- 64.Cassard L, Jönsson F, Arnaud S, Daëron M. Fcγ receptors inhibit mouse and human basophil activation. J Immunol. 2012;189:2995–3006. doi: 10.4049/jimmunol.1200968. [DOI] [PubMed] [Google Scholar]
- 65.Malbec O, Daëron M. The mast cell IgG receptors and their roles in tissue inflammation. Immunol Rev. 2007;217:206–221. doi: 10.1111/j.1600-065X.2007.00510.x. [DOI] [PubMed] [Google Scholar]
- 66.Wu LC. Immunoglobulin E receptor signaling and asthma. J Biol Chem. 2011;286:32891–32897. doi: 10.1074/jbc.R110.205104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Schwartz C, Turqueti-Neves A, Hartmann S, Yu P, Nimmerjahn F, Voehringer D. Basophil-mediated protection against gastrointestinal helminths requires IgE-induced cytokine secretion. Proc Natl Acad Sci. 2014;111:E5169–E5177. doi: 10.1073/pnas.1412663111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Milgrom H, Fick RB, Su JQ, Reimann JD, Bush RK, Watrous ML, et al. Treatment of allergic asthma with monoclonal anti-IgE antibody. N Engl J Med. 1999;341:1966–1973. doi: 10.1056/NEJM199912233412603. [DOI] [PubMed] [Google Scholar]
- 69.Strunk RC, Bloomberg GR. Omalizumab for asthma. N Engl J Med. 2006;354:2689–2695. doi: 10.1056/NEJMct055184. [DOI] [PubMed] [Google Scholar]
- 70.Maurer M, Rosén K, Hsieh H-J, Saini S, Grattan C, Gimenéz-Arnau A, et al. Omalizumab for the treatment of chronic idiopathic or spontaneous urticaria. N Engl J Med. 2013;368:924–935. doi: 10.1056/NEJMoa1215372. [DOI] [PubMed] [Google Scholar]
- 71.Borkowski TA, Jouvin M-H, Lin S-Y, Kinet J-P. Minimal requirements for IgE-mediated regulation of surface FcεRI. J Immunol. 2001;167:1290–1296. doi: 10.4049/jimmunol.167.3.1290. [DOI] [PubMed] [Google Scholar]
- 72.Hill DA, Siracusa MC, Ruymann KR, Tait Wojno ED, Artis D, Spergel JM. Omalizumab therapy is associated with reduced circulating basophil populations in asthmatic children. Allergy. 2014;69:674–677. doi: 10.1111/all.12375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Lin H, Boesel KM, Griffith DT, Prussin C, Foster B, Romero FA, et al. Omalizumab rapidly decreases nasal allergic response and FcεRI on basophils. J Allergy Clin Immunol. 2004;113:297–302. doi: 10.1016/j.jaci.2003.11.044. [DOI] [PubMed] [Google Scholar]
- 74.MacGlashan DW, Jr, Bochner BS, Adelman DC, Jardieu PM, Togias A, McKenzie-White J, et al. Down-regulation of FcεRI expression on human basophils during in vivo treatment of atopic patients with anti-IgE antibody. J Immunol. 1997;158:1438–1445. [PubMed] [Google Scholar]
- 75.Saini SS, MacGlashan DW, Sterbinsky SA, Togias A, Adelman DC, Lichtenstein LM, et al. Down-regulation of human basophil IgE and FC epsilon RI alpha surface densities and mediator release by anti-IgE-infusions is reversible in vitro and in vivo. J Immunol. 1999;162:5624–5630. [PubMed] [Google Scholar]
- 76.Zaidi AK, Saini SS, Macglashan DW. Regulation of Syk kinase and FcRbeta expression in human basophils during treatment with omalizumab. J Allergy Clin Immunol. 2010;125:902–908.e7. doi: 10.1016/j.jaci.2009.12.996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.MacGlashan DW. Endocytosis, recycling, and degradation of unoccupied FcepsilonRI in human basophils. J Leukoc Biol. 2007;82:1003–1010. doi: 10.1189/jlb.0207103. [DOI] [PubMed] [Google Scholar]
- 78.Eckman JA, Hamilton RG, Gober LM, Sterba PM, Saini SS. Basophil phenotypes in chronic idiopathic urticaria in relation to disease activity and autoantibodies. J Invest Dermatol. 2008;128:1956–1963. doi: 10.1038/jid.2008.55. [DOI] [PubMed] [Google Scholar]
- 79.Kaplan AP, Joseph K, Maykut RJ, Geba GP, Zeldin RK. Treatment of chronic autoimmune urticaria with omalizumab. J Allergy Clin Immunol. 2008;122:569–573. doi: 10.1016/j.jaci.2008.07.006. [DOI] [PubMed] [Google Scholar]
- 80.Mukai K, Matsuoka K, Taya C, Suzuki H, Yokozeki H, Nishioka K, et al. Basophils play a critical role in the development of IgE-mediated chronic allergic inflammation independently of T cells and mast cells. Immunity. 2005;23:191–202. doi: 10.1016/j.immuni.2005.06.011. [DOI] [PubMed] [Google Scholar]
- 81.Egawa M, Mukai K, Yoshikawa S, Iki M, Mukaida N, Kawano Y, et al. Inflammatory monocytes recruited to allergic skin acquire an anti-inflammatory M2 phenotype via basophil-derived interleukin-4. Immunity. 2013;38:570–580. doi: 10.1016/j.immuni.2012.11.014. [DOI] [PubMed] [Google Scholar]
- 82.Hashimoto T, Satoh T, Yokozeki H. Protective role of STAT6 in basophil-dependent prurigo-like allergic skin inflammation. J Immunol. 2015;194:4631–4640. doi: 10.4049/jimmunol.1401032. [DOI] [PubMed] [Google Scholar]
- 83.Bauer RN, Manohar M, Singh AM, Jay DC, Nadeau KC. The future of biologics: Applications for food allergy. J Allergy Clin Immunol. 2015;135:312–323. doi: 10.1016/j.jaci.2014.12.1908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Garcia G, Magnan A, Chiron R, Contin-Bordes C, Berger P, Taillé C, et al. A proof-of-concept, randomized, controlled trial of omalizumab in patients with severe, difficult-to-control, nonatopic asthma. Chest. 2013;144:411–419. doi: 10.1378/chest.12-1961. [DOI] [PubMed] [Google Scholar]
- 85.Allakhverdi Z, Comeau MR, Jessup HK, Yoon B-RP, Brewer A, Chartier S, et al. Thymic stromal lymphopoietin is released by human epithelial cells in response to microbes, trauma, or inflammation and potently activates mast cells. J Exp Med. 2007;204:253–258. doi: 10.1084/jem.20062211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Kay Ab, Clark P, Maurer M, Ying S. Elevations in T-helper-2-initiating cytokines (interleukin-33, interleukin-25 and thymic stromal lymphopoietin) in lesional skin from chronic spontaneous (“idiopathic”) urticaria. Br J Dermatol. 2015;172:1294–1302. doi: 10.1111/bjd.13621. [DOI] [PubMed] [Google Scholar]
- 87.Rocha R, Vitor AB, Trindade E, Lima R, Tavares M, Lopes J, et al. Omalizumab in the treatment of eosinophilic esophagitis and food allergy. Eur J Pediatr. 2011;170:1471–1474. doi: 10.1007/s00431-011-1540-4. [DOI] [PubMed] [Google Scholar]
- 88.Noda S, Krueger JG, Guttman-Yassky E. The translational revolution and use of biologics in patients with inflammatory skin diseases. J Allergy Clin Immunol. 2015;135:324–336. doi: 10.1016/j.jaci.2014.11.015. [DOI] [PubMed] [Google Scholar]
- 89.Kim BS, Wang K, Siracusa MC, Saenz SA, Brestoff JR, Monticelli LA, et al. Basophils promote innate lymphoid cell responses in inflamed skin. J Immunol. 2014;193:3717–3725. doi: 10.4049/jimmunol.1401307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Noti M, Wojno EDT, Kim BS, Siracusa MC, Giacomin PR, Nair MG, et al. Thymic stromal lymphopoietin-elicited basophil responses promote eosinophilic esophagitis. Nat Med. 2013;19:1005–1013. doi: 10.1038/nm.3281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Giacomin PR, Siracusa MC, Walsh KP, Grencis RK, Kubo M, Comeau MR, et al. Thymic Stromal Lymphopoietin-Dependent Basophils Promote Th2 Cytokine Responses following Intestinal Helminth Infection. J Immunol. 2012;189:4371–4378. doi: 10.4049/jimmunol.1200691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Noti M, Kim BS, Siracusa MC, Rak GD, Kubo M, Moghaddam AE, et al. Exposure to food allergens through inflamed skin promotes intestinal food allergy through the thymic stromal lymphopoietin–basophil axis. J Allergy Clin Immunol. 2014;133:1390–1399. doi: 10.1016/j.jaci.2014.01.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Liu Y-J. Thymic stromal lymphopoietin: master switch for allergic inflammation. J Exp Med. 2006;203:269–273. doi: 10.1084/jem.20051745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Gao P-S, Rafaels NM, Mu D, Hand T, Murray T, Boguniewicz M, et al. Genetic variants in thymic stromal lymphopoietin are associated with atopic dermatitis and eczema herpeticum. J Allergy Clin Immunol. 2010;125:1403–1407.e4. doi: 10.1016/j.jaci.2010.03.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Kimura S, Pawankar R, Mori S, Nonaka M, Masuno S, Yagi T, et al. Increased expression and role of thymic stromal lymphopoietin in nasal polyposis. Allergy Asthma Immunol Res. 2011;3:186–193. doi: 10.4168/aair.2011.3.3.186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Nagarkar DR, Poposki JA, Tan BK, Comeau MR, Peters AT, Hulse KE, et al. Thymic stromal lymphopoietin activity is increased in nasal polyps of patients with chronic rhinosinusitis. J Allergy Clin Immunol. 2013;132:593–600.e12. doi: 10.1016/j.jaci.2013.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Ramasamy A, Curjuric I, Coin LJ, Kumar A, McArdle WL, Imboden M, et al. A genome-wide meta-analysis of genetic variants associated with allergic rhinitis and grass sensitization and their interaction with birth order. J Allergy Clin Immunol. 2011;128:996–1005. doi: 10.1016/j.jaci.2011.08.030. [DOI] [PubMed] [Google Scholar]
- 98.Iijima H, Kaneko Y, Yamada H, Yatagai Y, Masuko H, Sakamoto T, et al. A distinct sensitization pattern associated with asthma and the thymic stromal lymphopoietin (TSLP) genotype. Allergol Int. 2013;62:123–130. doi: 10.2332/allergolint.12-OA-0488. [DOI] [PubMed] [Google Scholar]
- 99.Rothenberg ME, Spergel JM, Sherrill JD, Annaiah K, Martin LJ, Cianferoni A, et al. Common variants at 5q22 associate with pediatric eosinophilic esophagitis. Nat Genet. 2010;42:289–291. doi: 10.1038/ng.547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Sherrill JD, Gao P-S, Stucke EM, Blanchard C, Collins MH, Putnam PE, et al. Variants of thymic stromal lymphopoietin and its receptor associate with eosinophilic esophagitis. J Allergy Clin Immunol. 2010;126:160–165.e3. doi: 10.1016/j.jaci.2010.04.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Li M, Hener P, Zhang Z, Kato S, Metzger D, Chambon P. Topical vitamin D3 and low-calcemic analogs induce thymic stromal lymphopoietin in mouse keratinocytes and trigger an atopic dermatitis. Proc Natl Acad Sci. 2006;103:11736–11741. doi: 10.1073/pnas.0604575103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Allakhverdi Z, Comeau MR, Smith DE, Toy D, Endam LM, Desrosiers M, et al. CD34+ hemopoietic progenitor cells are potent effectors of allergic inflammation. J Allergy Clin Immunol. 2009;123:472–478.e1. doi: 10.1016/j.jaci.2008.10.022. [DOI] [PubMed] [Google Scholar]
- 103.Smith SG, Gugilla A, Mukherjee M, Merim K, Irshad A, Tang W, et al. Thymic stromal lymphopoietin and IL-33 modulate migration of hematopoietic progenitor cells in patients with allergic asthma. J Allergy Clin Immunol. 2015;135:1594–1602. doi: 10.1016/j.jaci.2014.12.1918. [DOI] [PubMed] [Google Scholar]
- 104.Hui CCK, Rusta-Sallehy S, Asher I, Heroux D, Denburg JA. The effects of thymic stromal lymphopoietin and IL-3 on human eosinophil–basophil lineage commitment: Relevance to atopic sensitization. Immun Inflamm Dis. 2014;2:44–55. doi: 10.1002/iid3.20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Calder PC. Polyunsaturated fatty acids, inflammation, and immunity. Lipids. 2001;36:1007–1024. doi: 10.1007/s11745-001-0812-7. [DOI] [PubMed] [Google Scholar]
- 106.Lott JM, Sumpter TL, Turnquist HR. New dog and new tricks: evolving roles for IL-33 in type 2 immunity. J Leukoc Biol. 2015;97:1037–1048. doi: 10.1189/jlb.3RI1214-595R. [DOI] [PubMed] [Google Scholar]
- 107.Molofsky AB, Savage AK, Locksley RM. Interleukin-33 in tissue homeostasis, injury, and inflammation. Immunity. 2015;42:1005–1019. doi: 10.1016/j.immuni.2015.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Muto T, Fukuoka A, Kabashima K, Ziegler SF, Nakanishi K, Matsushita K, et al. The role of basophils and proallergic cytokines, TSLP and IL-33, in cutaneously sensitized food allergy. Int Immunol. 2014;26:539–549. doi: 10.1093/intimm/dxu058. [DOI] [PubMed] [Google Scholar]
- 109.Saluja R, Ketelaar ME, Hawro T, Church MK, Maurer M, Nawijn MC. The role of the IL-33/IL-1RL1 axis in mast cell and basophil activation in allergic disorders. Mol Immunol. 2015;63:80–85. doi: 10.1016/j.molimm.2014.06.018. [DOI] [PubMed] [Google Scholar]
- 110.Schneider E, Petit-Bertron A-F, Bricard R, Levasseur M, Ramadan A, Girard J-P, et al. IL-33 activates unprimed murine basophils directly in vitro and induces their in vivo expansion indirectly by promoting hematopoietic growth factor production. J Immunol. 2009;183:3591–3597. doi: 10.4049/jimmunol.0900328. [DOI] [PubMed] [Google Scholar]
- 111.Suzukawa M, Iikura M, Koketsu R, Nagase H, Tamura C, Komiya A, et al. An IL-1 cytokine member, IL-33, induces human basophil activation via its ST2 receptor. J Immunol. 2008;181:5981–5989. doi: 10.4049/jimmunol.181.9.5981. [DOI] [PubMed] [Google Scholar]
- 112.Junttila IS, Watson C, Kummola L, Chen X, Hu-Li J, Guo L, et al. Efficient cytokine-induced IL-13 production by mast cells requires both IL-33 and IL-3. J Allergy Clin Immunol. 2013;132:704–712.e10. doi: 10.1016/j.jaci.2013.03.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Smithgall MD, Comeau MR, Yoon B-RP, Kaufman D, Armitage R, Smith DE. IL-33 amplifies both Th1- and Th2-type responses through its activity on human basophils, allergen-reactive Th2 cells, iNKT and NK Cells. Int Immunol. 2008;20:1019–1030. doi: 10.1093/intimm/dxn060. [DOI] [PubMed] [Google Scholar]
- 114.Kim S, Prout M, Ramshaw H, Lopez AF, LeGros G, Min B. Cutting Edge: Basophils Are Transiently Recruited into the Draining Lymph Nodes during Helminth Infection via IL-3, but Infection-Induced Th2 Immunity Can Develop without Basophil Lymph Node Recruitment or IL-3. J Immunol. 2010;184:1143–1147. doi: 10.4049/jimmunol.0902447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Cianferoni A, Spergel J. Eosinophilic esophagitis: a comprehensive review. Clin Rev Allergy Immunol. 2015 doi: 10.1007/s12016-015-8501-z. [DOI] [PubMed] [Google Scholar]
- 116.Mulder DJ, Justinich CJ. B cells, IgE and mechanisms of type I hypersensitivity in eosinophilic oesophagitis. Gut. 2010;59:6–7. doi: 10.1136/gut.2009.189316. [DOI] [PubMed] [Google Scholar]
- 117.Stokes JR, Casale TB. The Use of Anti-IgE Therapy Beyond Allergic Asthma. J Allergy Clin Immunol Pract. 2015;3:162–166. doi: 10.1016/j.jaip.2014.10.010. [DOI] [PubMed] [Google Scholar]
- 118.Foroughi S, Foster B, Kim N, Bernardino LB, Scott LM, Hamilton RG, et al. Anti-IgE treatment of eosinophil-associated gastrointestinal disorders. J Allergy Clin Immunol. 2007;120:594–601. doi: 10.1016/j.jaci.2007.06.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Gauvreau GM, O’Byrne PM, Boulet L-P, Wang Y, Cockcroft D, Bigler J, et al. Effects of an anti-TSLP antibody on allergen-induced asthmatic responses. N Engl J Med. 2014;370:2102–2110. doi: 10.1056/NEJMoa1402895. [DOI] [PubMed] [Google Scholar]
- 120.Kambayashi T, Laufer TM. Atypical MHC class II-expressing antigen-presenting cells: can anything replace a dendritic cell? Nat Rev Immunol. 2014;14:719–730. doi: 10.1038/nri3754. [DOI] [PubMed] [Google Scholar]
- 121.Sarfati M, Wakahara K, Chapuy L, Delespesse G. Mutual interaction of basophils and T cells in chronic inflammatory diseases. Front Immunol. 2015;6 doi: 10.3389/fimmu.2015.00399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Otsuka A, Nakajima S, Kubo M, Egawa G, Honda T, Kitoh A, et al. Basophils are required for the induction of Th2 immunity to haptens and peptide antigens. Nat Commun. 2013;4:1738. doi: 10.1038/ncomms2740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Perrigoue JG, Saenz SA, Siracusa MC, Allenspach EJ, Taylor BC, Giacomin PR, et al. MHC class II-dependent basophil-CD4+ T cell interactions promote T(H)2 cytokine-dependent immunity. Nat Immunol. 2009;10:697–705. doi: 10.1038/ni.1740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Yoshimoto T, Yasuda K, Tanaka H, Nakahira M, Imai Y, Fujimori Y, et al. Basophils contribute to TH2-IgE responses in vivo via IL-4 production and presentation of peptide–MHC class II complexes to CD4+ T cells. Nat Immunol. 2009;10:706–712. doi: 10.1038/ni.1737. [DOI] [PubMed] [Google Scholar]
- 125.Sokol CL, Barton GM, Farr AG, Medzhitov R. A mechanism for the initiation of allergen-induced T helper type 2 responses. Nat Immunol. 2008;9:310–318. doi: 10.1038/ni1558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Allenspach EJ, Lemos MP, Porrett PM, Turka LA, Laufer TM. Migratory and lymphoid-resident dendritic cells cooperate to efficiently prime naive CD4 T cells. Immunity. 2008;29:795–806. doi: 10.1016/j.immuni.2008.08.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Hammad H, Plantinga M, Deswarte K, Pouliot P, Willart MAM, Kool M, et al. Inflammatory dendritic cells—not basophils—are necessary and sufficient for induction of Th2 immunity to inhaled house dust mite allergen. J Exp Med. 2010;207:2097–2111. doi: 10.1084/jem.20101563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Bonecchi R, Bianchi G, Bordignon PP, D’Ambrosio D, Lang R, Borsatti A, et al. Differential expression of chemokine receptors and chemotactic responsiveness of type 1 T helper cells (Th1s) and Th2s. J Exp Med. 1998;187:129–134. doi: 10.1084/jem.187.1.129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Zaiss DMW, Gause WC, Osborne LC, Artis D. Emerging functions of amphiregulin in orchestrating immunity, inflammation, and tissue repair. Immunity. 2015;42:216–226. doi: 10.1016/j.immuni.2015.01.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Zaiss DMW, van Loosdregt J, Gorlani A, Bekker CPJ, Gröne A, Sibilia M, et al. Amphiregulin enhances regulatory T cell-suppressive function via the epidermal growth factor receptor. Immunity. 2013;38:275–284. doi: 10.1016/j.immuni.2012.09.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Meulenbroeks C, van Weelden H, Schwartz C, Voehringer D, Redegeld FAM, Rutten VPMG, et al. Basophil-derived amphiregulin is essential for UVB irradiation–induced immune suppression. J Invest Dermatol. 2015;135:222–228. doi: 10.1038/jid.2014.329. [DOI] [PubMed] [Google Scholar]
- 132.Qi Y, Operario DJ, Oberholzer CM, Kobie JJ, Looney RJ, Georas SN, et al. Human basophils express amphiregulin in response to T cell–derived IL-3. J Allergy Clin Immunol. 2010;126:1260–1266.e4. doi: 10.1016/j.jaci.2010.08.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Stone KD, Prussin C, Metcalfe DD. IgE, mast cells, basophils, and eosinophils. J Allergy Clin Immunol. 2010;125:S73–80. doi: 10.1016/j.jaci.2009.11.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Denzel A, Maus UA, Rodriguez Gomez M, Moll C, Niedermeier M, Winter C, et al. Basophils enhance immunological memory responses. Nat Immunol. 2008;9:733–742. doi: 10.1038/ni.1621. [DOI] [PubMed] [Google Scholar]
- 135.Rodriguez Gomez M, Talke Y, Goebel N, Hermann F, Reich B, Mack M. Basophils support the survival of plasma cells in mice. J Immunol Baltim Md 1950. 2010;185:7180–7185. doi: 10.4049/jimmunol.1002319. [DOI] [PubMed] [Google Scholar]
- 136.Charles N, Hardwick D, Daugas E, Illei GG, Rivera J. Basophils and the T helper 2 environment can promote the development of lupus nephritis. Nat Med. 2010;16:701–707. doi: 10.1038/nm.2159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Lack G, Fox D, Northstone K, Golding J. Factors associated with the development of peanut allergy in childhood. N Engl J Med. 2003;348:977–985. doi: 10.1056/NEJMoa013536. [DOI] [PubMed] [Google Scholar]
- 138.Han H, Thelen TD, Comeau MR, Ziegler SF. Thymic stromal lymphopoietin–mediated epicutaneous inflammation promotes acute diarrhea and anaphylaxis. J Clin Invest. 2014;124:5442–5452. doi: 10.1172/JCI77798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Ohnmacht C, Schwartz C, Panzer M, Schiedewitz I, Naumann R, Voehringer D. Basophils orchestrate chronic allergic dermatitis and protective immunity against helminths. Immunity. 2010;33:364–374. doi: 10.1016/j.immuni.2010.08.011. [DOI] [PubMed] [Google Scholar]
- 140.Jin G, Matsushita T, Hamaguchi Y, Le Huu D, Ishii T, Hasegawa M, et al. Basophils and mast cells play critical roles for leukocyte recruitment in IgE-mediated cutaneous reverse passive Arthus reaction. J Dermatol Sci. 2012;67:181–189. doi: 10.1016/j.jdermsci.2012.06.005. [DOI] [PubMed] [Google Scholar]
- 141.Nakashima C, Otsuka A, Kitoh A, Honda T, Egawa G, Nakajima S, et al. Basophils regulate the recruitment of eosinophils in a murine model of irritant contact dermatitis. J Allergy Clin Immunol. 2014;134:100–107.e12. doi: 10.1016/j.jaci.2014.02.026. [DOI] [PubMed] [Google Scholar]
- 142.Cheng LE, Sullivan BM, Retana LE, Allen CDC, Liang H-E, Locksley RM. IgE-activated basophils regulate eosinophil tissue entry by modulating endothelial function. J Exp Med. 2015;212:513–524. doi: 10.1084/jem.20141671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Borchers MT, Ansay T, DeSalle R, Daugherty BL, Shen H, Metzger M, et al. In vitro assessment of chemokine receptor-ligand interactions mediating mouse eosinophil migration. J Leukoc Biol. 2002;71:1033–1041. [PubMed] [Google Scholar]
- 144.Van Dyken SJ, Locksley RM. Interleukin-4- and interleukin-13-mediated alternatively activated macrophages: roles in homeostasis and disease. Annu Rev Immunol. 2013;31:317–343. doi: 10.1146/annurev-immunol-032712-095906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Gundra UM, Girgis NM, Ruckerl D, Jenkins S, Ward LN, Kurtz ZD, et al. Alternatively activated macrophages derived from monocytes and tissue macrophages are phenotypically and functionally distinct. Blood. 2014;123:e110–e122. doi: 10.1182/blood-2013-08-520619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Han H, Headley MB, Xu W, Comeau MR, Zhou B, Ziegler SF. Thymic stromal lymphopoietin amplifies the differentiation of alternatively activated macrophages. J Immunol. 2013;190:904–912. doi: 10.4049/jimmunol.1201808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Huang SC-C, Everts B, Ivanova Y, O’Sullivan D, Nascimento M, Smith AM, et al. Cell-intrinsic lysosomal lipolysis is essential for alternative activation of macrophages. Nat Immunol. 2014;15:846–855. doi: 10.1038/ni.2956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Gordon S. Alternative activation of macrophages. Nat Rev Immunol. 2003;3:23–35. doi: 10.1038/nri978. [DOI] [PubMed] [Google Scholar]
- 149.Obata-Ninomiya K, Ishiwata K, Tsutsui H, Nei Y, Yoshikawa S, Kawano Y, et al. The skin is an important bulwark of acquired immunity against intestinal helminths. J Exp Med. 2013;210:2583–2595. doi: 10.1084/jem.20130761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Griffith JW, Sokol CL, Luster AD. Chemokines and chemokine receptors: positioning cells for host defense and immunity. Annu Rev Immunol. 2014;32:659–702. doi: 10.1146/annurev-immunol-032713-120145. [DOI] [PubMed] [Google Scholar]
- 151.Xue J, Schmidt SV, Sander J, Draffehn A, Krebs W, Quester I, et al. Transcriptome-based network analysis reveals a spectrum model of human macrophage activation. Immunity. 2014;40:274–288. doi: 10.1016/j.immuni.2014.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Kim BS. Innate lymphoid cells in the skin. J Invest Dermatol. 2015;135:673–678. doi: 10.1038/jid.2014.401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Artis D, Spits H. The biology of innate lymphoid cells. Nature. 2015;517:293–301. doi: 10.1038/nature14189. [DOI] [PubMed] [Google Scholar]
- 154.von Moltke J, Locksley RM. I-L-C-2 it: type 2 immunity and group 2 innate lymphoid cells in homeostasis. Curr Opin Immunol. 2014;31:58–65. doi: 10.1016/j.coi.2014.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Motomura Y, Morita H, Moro K, Nakae S, Artis D, Endo TA, et al. Basophil-derived interleukin-4 controls the function of natural helper cells, a member of ILC2s, in lung inflammation. Immunity. 2014;40:758–771. doi: 10.1016/j.immuni.2014.04.013. [DOI] [PubMed] [Google Scholar]
- 156.Monticelli LA, Sonnenberg GF, Abt MC, Alenghat T, Ziegler CGK, Doering TA, et al. Innate lymphoid cells promote lung tissue homeostasis following acute influenza virus infection. Nat Immunol. 2011;12:1045–1054. doi: 10.1031/ni.2131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Beck LA, Thaçi D, Hamilton JD, Graham NM, Bieber T, Rocklin R, et al. Dupilumab treatment in adults with moderate-to-severe atopic dermatitis. N Engl J Med. 2014;371:130–139. doi: 10.1056/NEJMoa1314768. [DOI] [PubMed] [Google Scholar]
- 158.Thaçi D, Simpson EL, Beck LA, Bieber T, Blauvelt A, Papp K, et al. Efficacy and safety of dupilumab in adults with moderate-to-severe atopic dermatitis inadequately controlled by topical treatments: a randomised, placebo-controlled, dose-ranging phase 2b trial. Lancet Lond Engl. 2015 doi: 10.1016/S0140-6736(15)00388-8. [DOI] [PubMed] [Google Scholar]
- 159.Wenzel S, Ford L, Pearlman D, Spector S, Sher L, Skobieranda F, et al. Dupilumab in persistent asthma with elevated eosinophil levels. N Engl J Med. 2013;368:2455–2466. doi: 10.1056/NEJMoa1304048. [DOI] [PubMed] [Google Scholar]