Abstract
Background
The number of states proposing school-entry requirements for human papillomavirus (HPV) vaccination has increased over the last decade. However, data are currently limited regarding parents' support of such laws. We sought to obtain the first national estimates of parents' support of HPV vaccination school-entry requirements.
Methods
A national sample of 1501 parents of 11- to 17-year-old children completed a web-based survey between November 2014 and January 2015. Analyses used multivariable logistic regression to assess correlates of support for school-entry requirements for HPV vaccination.
Results
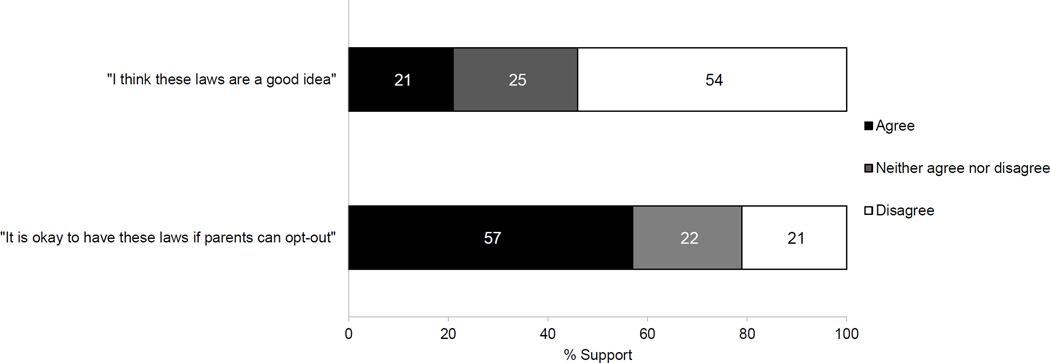
Overall, 21% of parents agreed that laws requiring HPV vaccination for school attendance "are a good idea," and 54% disagreed. If school-entry requirements included opt-out provisions, agreement increased to 57%, and only 21% disagreed. Parents more often agreed with requirements without opt-out provisions if they were Hispanic (OR=1.53, 95% CI: 1.05–2.22), believed HPV vaccine was as or more important than other adolescent vaccines (OR=2.76, 95% CI: 1.98–3.83), or believed HPV vaccine was effective for preventing cervical cancer (OR=2.55, 95% CI: 1.93–3.37). Parents less often agreed if they resided in Midwest states or believed that HPV vaccine was being pushed to make money for drug companies (both p<.05).
Conclusion
Opt-out provisions almost tripled parents' support for HPV vaccine school-entry requirements. Our findings suggest that race/ethnicity, attitudes about HPV vaccine, and region of residence may influence support for requirements without opt-out provisions.
Impact
Opt-out provisions greatly increase parent support of school-entry requirements for HPV vaccination but may make them ineffective.
Keywords: Human papillomavirus, HPV vaccine, vaccination laws, school-entry, parent attitudes
Introduction
Human papillomavirus (HPV)-attributable diseases are a serious public health threat in the U.S (1). Nearly 80 million Americans are infected with at least one type of HPV (2), and HPV types 16 and 18 are responsible for more than 22,000 new cases of cancer each year (3). Most HPV-associated cancers could be prevented through widespread HPV vaccination (1). For this reason, national guidelines recommend routine and timely HPV vaccination of boys and girls at age 11 or 12 (4). However, HPV vaccine coverage is low, lagging far behind other adolescent vaccines. Among 13- to 17-year-olds, only 40% of girls and 22% of boys had completed the HPV vaccine series by 2014 (5). These coverage levels fall considerably short of the Healthy People 2020 goal of having 80% of 13- to 15-year-olds fully vaccinated (6).
In the U.S., policy interventions, such as school-entry requirements, have contributed to high uptake of adolescent vaccination and, in turn, low prevalence of many vaccine-preventable diseases (7–9). The Task Force on Community Preventive Services recommends school-entry requirements as an evidence-based strategy to increase vaccine coverage (10). Requiring vaccination as a condition to school attendance is within state’s legislative power to protect the public’s health. As of 2016, all 50 states and Washington, D.C. have vaccine requirements for school entry. All of these laws allow for medical exemptions (11), which typically require a physician’s certificate stating that a vaccination would be harmful. Most states also allow nonmedical exemptions; 47 states permit religious exemptions and 18 states allow philosophical exemptions on the basis of personal, moral or other beliefs against vaccination (11). States differ in the process parents must go through to get a nonmedical exemption (12–14). In states where there is no rigorous process for claiming the exemption, more people opt out of vaccination (15).
The unprecedented opportunity to prevent HPV-associated cancers through vaccination led many states to propose laws requiring HPV vaccine for school attendance, similar to those for tetanus, diphtheria, and pertussis (Tdap). Since Michigan introduced the first legislation requiring HPV vaccination for school entry in September 2006, 24 other states and Washington, D.C. have proposed similar laws (16). However, only Virginia and Washington, D.C. have enacted such legislation into law, with Rhode Island more recently adopting the policy by means of administrative ruling. Ethical, political, and legal concerns from opponents have been the focus of the policy debate (17–19), shifting discussions away from the demonstrated effectiveness of HPV vaccination to prevent many cancers (20, 21).
Policymakers consider their constituents’ opinions as they decide how to act on health policies (22), including HPV vaccination school-entry requirements (17). However, data are currently limited regarding parents’ support for these laws. Previous studies were limited to samples in Georgia (23), North Carolina (24), and Los Angeles, California (25) and happened prior to ACIP recommendations that boys routinely receive HPV vaccination. To fill this large gap in the literature, we conducted a national survey among parents of 11- to 17-year-old boys and girls to better understand their support for these laws. The aims of our study were to: 1) assess parents’ support for HPV vaccine school-entry requirements, without and with opt-out provisions, and 2) identify correlates of parental support for such laws. We hypothesized higher support for school-entry requirements when including opt-out provisions and among parents with positive attitudes about HPV vaccine.
Materials and Methods
Participants and Procedures
Participants were members of an existing, national panel of non-instutionalized U.S. adults maintained by a survey research company (26). The company constructed the panel using probability-based sampling of list-assisted, random-digit dialed (RDD) phone numbers supplemented by address-based sampling (ABS). The ABS strategy was incorporated in response to the growing number of cell phone-only households that are outside the traditional RDD landline telephone frame. Thus our overall sampling design captured households with landline phones, cell phone-only households, and households without telephones. Eligible panel members were parents of at least one 11- to 17-year-old child living primarily in their households. The survey instructed respondents with more than one age-eligible child to respond with regard to the child with the most recent birthday.
The survey company emailed invitations to a random sample of 2,845 panel members, and 1,760 responded by visiting the survey website, confirming eligibility criteria, and providing informed consent. A total of 1,504 parents were eligible and completed the survey between November 2014 and January 2015. After accounting for ineligible respondents (n=335) and excluding respondents who failed to complete at least two-thirds of the survey (n=14), the survey response rate was 61%, calculated using American Association for Public Opinion Research Response Rate 5 (27). For the present study, we also excluded respondents who did not provide data on the main outcome variable (n=3). The final analytic sample had 1,501 parents. Forty-three respondents (3% of the sample) came from Virginia and Washington, D.C., which had HPV vaccine school-entry requirements in place at the time of the survey. Since we sought to obtain the first national estimate of support for such requirements, we included these parents in our sample.
Prior to fielding the survey, we cognitively tested our instrument with 18 parents of adolescents to maximize respondent comprehension. We then pre-tested the survey online with 26 panel members to ensure proper functioning. The survey instrument is available online at www.unc.edu/~ntbrewer/hpv.htm. The University of North Carolina Institutional Review Board approved the study protocol.
Measures
Following the approach of previous studies (24, 25), our survey introduced respondents to HPV vaccine school-entry requirements with the prompt, "Some states are trying to pass laws that would require all 11 and 12 year-olds to get HPV vaccine before they are allowed to start 6th grade.” Parents then said whether they agreed with the statement, “I think these laws are a good idea” using a 5-point response scale. Parents who did not agree with the previous statement received an additional item: “It is okay to have these laws only if parents can opt out if they want to.” For each statement, we categorized parents as agreeing (somewhat or strongly agree) or disagreeing/neither (somewhat or strongly disagree, or neither disagree or agree).
The survey assessed key candidate correlates previously identified in the literature as potential predictors of parental support of HPV vaccine school-entry requirements (24, 25). The survey company provided data on parents’ sex, race/ethnicity, educational attainment, annual household income, and location of residence in terms of U.S. state and region. We created a variable to assess whether respondents had their residence in a state that requires HPV vaccination for school attendance. We dichotomized this variable as yes (respondents from Virginia and Washington, D.C.) and no (respondents from other states). The survey also assessed the sex and age of the index child, and whether parents had received a provider recommendation for HPV vaccination for that child. The survey assessed HPV vaccination status with one item: “How many shots of the HPV vaccine has [child’s name] had?” We defined HPV vaccine initiation as responses of ≥1 shots.
Rules or regulations (e.g., requiring vaccination for school attendance) that people perceive as threatening personal freedoms can elicit a motivational state, reactance, which is characterized by anger and counter arguing and may elicit oppositional behavior (e.g., refusing vaccination) (28). The survey assessed psychological reactance with three items: “I become frustrated when I am unable to make free and independent decisions,” “Regulations trigger a sense of resistance in me,” and “When someone forces me to do something, I feel like doing the opposite.” These items had a 5-point response scale that ranged from “strongly disagree” to “strongly agree”. We created an index of reactance by calculating the mean response value and creating two categories: low (<4) and high (4–5).
The survey assessed parents’ agreement with statements shown to be associated with HPV vaccination uptake in the U.S. (29) and support for school-entry requirements for HPV vaccination (24, 25). The survey assessed perceptions regarding harms of HPV vaccines (e.g., "The HPV vaccine might cause lasting health problems"), barriers to vaccination (e.g., “It would be hard to find a provider or clinic where I can afford HPV vaccine for my child"), vaccine effectiveness (e.g., “The HPV vaccine is effective in preventing cervical cancer”), and uncertainty about the vaccine (e.g., "I don’t have enough information about the HPV vaccine to decide whether to give it to my child"). We adapted these items from the Carolina HPV Immunization Attitudes and Beliefs Scale (29). The 5-point response scale ranged from “strongly disagree” to “strongly agree.”
The survey also assessed importance of HPV vaccination with the statement: “I felt that the HPV vaccine for [child’s name] is…,” accompanied by a 5-point response scale that ranged from “not important” to “extremely important.” The survey repeated the same statement for meningococcal and Tdap vaccines. We calculated relative vaccine importance, giving a score of 1 if parents rated HPV vaccine as important as, or more important than, the average score for Tdap and meningococcal vaccines and 0 otherwise.
Statistical analysis
We calculated the percentage of support for HPV vaccine school-entry requirements, without and with opt-out provisions. We used bivariate logistic regressions to identify bivariate associations of candidate correlates with support for HPV vaccine requirements. We then entered covariates showing associations (p<.05) in bivariate analyses into a multivariable logistic regression model. We used separate logistic regression models to assess the associations between potential correlates and HPV vaccine requirements without and with opt-out provisions. Statistical tests were two-tailed with a critical alpha of .05. We conducted analyses using Stata 12.0 (College Station, TX).
Results
Respondents included residents of all 50 states and Washington D.C., and 33% were from the South (Table 1). About one-fifth (22%) had a household income of less than $35,000 per year. Parents were evenly split between having reported on a son (51%) or a daughter (49%), and the mean age of children was 14 years. Forty-six percent of children had received at least 1 dose of HPV vaccine. Fifty-six percent of parents were female, and the majority were non-Hispanic white (70%) or Hispanic (14%). More than one-third (38%) of parents had a high school degree or less education. Almost three-fourths (73%) of the sample scored low in the 3-item index of psychological reactance. About half (52%) of parents had received a provider recommendation for HPV vaccination.
Table 1.
Characteristics of a national sample of parents of 11- to 17-year-old adolescents, 2014–2015 (N=1,501).
| N | % | |
|---|---|---|
| Household characteristics | ||
| Income | ||
| <$35,000 | 329 | 22 |
| $35,000 – $74,999 | 467 | 31 |
| ≥$75,000 | 705 | 47 |
| Region | ||
| Northeast | 261 | 17 |
| Midwest | 392 | 26 |
| South | 497 | 33 |
| West | 351 | 23 |
| Resident of state that requires HPV vaccination for school attendance |
43 | 3 |
| Child characteristics | ||
| Female | 738 | 49 |
| Age (years) | ||
| 11–12 | 420 | 28 |
| 13–17 | 1,081 | 72 |
| HPV vaccination status | ||
| 0 doses | 807 | 54 |
| ≥1 dose | 694 | 46 |
| Parents’ characteristics and attitudes about HPV vaccine | ||
| Female | 835 | 56 |
| Race/Ethnicity | ||
| Non-Hispanic White | 1,056 | 70 |
| Non-Hispanic Black | 134 | 9 |
| Hispanic | 212 | 14 |
| Other | 99 | 7 |
| Education | ||
| High school degree or less | 574 | 38 |
| Some college | 389 | 26 |
| Bachelor’s degree or higher | 538 | 36 |
| Psychological reactance | ||
| Low | 1,089 | 73 |
| High | 412 | 27 |
| Has a doctor or other health care provider ever told your child should get the HPV vaccine? |
||
| No | 721 | 48 |
| Yes | 780 | 52 |
| Relative importance of HPV vaccine compared to Tdap and meningococcal vaccines |
||
| Less important | 736 | 49 |
| As or more important | 765 | 51 |
| The HPV vaccine might cause lasting health problems. | ||
| Disagree/neither | 1,153 | 77 |
| Agree | 348 | 23 |
| The HPV vaccine is being pushed to make money for drug companies. |
||
| Disagree/neither | 1,022 | 68 |
| Agree | 479 | 32 |
| I don’t have enough information about the HPV vaccine to decide whether to give it to my child. |
||
| Disagree/neither | 1,022 | 68 |
| Agree | 479 | 32 |
| The HPV vaccine is effective in preventing cervical cancer. | ||
| Disagree/neither | 900 | 60 |
| Agree | 601 | 40 |
| It would be hard to find a provider or clinic where I can afford HPV vaccine for my child. |
||
| Disagree/neither | 1,419 | 94 |
| Agree | 82 | 6 |
Regarding HPV vaccine attitudes, about half (51%) of parents said that HPV vaccine was as or more important than the Tdap and meningococcal vaccines (Table 1). Nearly one-fourth (23%) of the sample thought that HPV vaccine might cause lasting health problems and about one-third (32%) thought that HPV vaccine was being pushed to make money for drug companies. Thirty-two percent of parents said that they did not have enough information about HPV vaccine to decide whether to vaccinate their children and only 40% agreed that the vaccine was effective in preventing cervical cancer. Few parents (6%) said that it would be hard to find a provider or clinic where they can afford HPV vaccine for their children.
Support for HPV vaccine requirements without opt-out provisions
Twenty-one percent of parents agreed that laws requiring HPV vaccination for school attendance "are a good idea" (Figure 1). Hispanic parents had higher odds (OR=1.53, 95% CI: 1.05–2.22) of agreeing with HPV vaccine school-entry requirements than non-Hispanic whites in multivariable analysis (Table 2). Likewise, parents more often agreed with these requirements if they believed that HPV vaccine was as or more important than other adolescent vaccines (OR=2.76, 95% CI: 1.98–3.83), that HPV vaccine was effective for preventing cervical cancer (OR=2.55, 95% CI: 1.93–3.37), or that it would be hard to find a provider or clinic where they can afford the vaccine for their children (OR=2.50, 95% CI: 1.45–4.33). On the other hand, parents less often agreed with school-entry requirements if they believed that HPV vaccines were being pushed to make money for drug companies (OR=0.47, 95% CI: 0.32–0.69) or resided in Midwest states compared to Northeast states (OR=0.64, 95% CI: 0.42–0.98). In bivariate but not multivariate analyses, agreement with school-entry requirements was associated (p<.05) with living in a state requiring HPV vaccination for school attendance, having initiated HPV vaccination, having received a provider recommendation for HPV vaccination, lower psychological reactance, and believing that HPV vaccine might cause lasting health problems and that respondents do not have enough information to decide whether to give the vaccine to their children.
Figure 1.
Agreement with school-entry requirements for HPV vaccine.
Table 2.
Correlates of parental agreement for HPV vaccine school-entry requirements (N=1,501).
| No. respondents who agreed with “I think these laws are a good idea” (%) |
Bivariate OR (95% CI) |
Multivariable OR (95% CI) |
|
|---|---|---|---|
| Household characteristics | |||
| Income | |||
| <$35,000 | 79/329 (24) | Ref | - |
| $35,000 – $74,999 | 95/467 (20) | 0.81 (0.58, 1.13) | - |
| ≥$75,000 | 147/705 (21) | 0.83 (0.61, 1.14) | - |
| Region | |||
| Northeast | 65/261 (25) | Ref | Ref |
| Midwest | 60/392 (15) | 0.54 (0.37, 0.81)** | 0.64 (0.42, 0.98)* |
| South | 113/497 (23) | 0.89 (0.63, 1.26) | 0.92 (0.62, 1.36) |
| West | 83/351 (24) | 0.93 (0.64, 1.36) | 0.88 (0.58, 1.33) |
| Resident of state that requires HPV vaccination for school attendance |
|||
| No | 306/1,458 (21) | Ref | Ref |
| Yes1 | 15/43 (35) | 2.01 (1.06, 3.82)* | 1.68 (0.81, 3.48) |
| Child characteristics | |||
| Sex | |||
| Male | 172/763 (23) | Ref | - |
| Female | 149/738 (20) | 0.87 (0.68, 1.11) | - |
| Age (years) | |||
| 11–12 | 93/420 (22) | Ref | - |
| 13–17 | 228/1081 (21) | 0.94 (0.72, 1.23) | - |
| HPV vaccination | |||
| 0 doses | 107/807 (13) | Ref | Ref |
| ≥1 dose | 214/694 (31) | 2.92 (2.25, 3.78)** | 1.33 (0.95, 1.86) |
| Parents’ characteristics and attitudes about HPV vaccine | |||
| Sex | |||
| Male | 151/666 (23) | Ref | - |
| Female | 170/835 (20) | 0.87 (0.68, 1.12) | - |
| Race/Ethnicity | |||
| Non-Hispanic White | 198/1,056 (19) | Ref | Ref |
| Non-Hispanic Black | 31/134 (23) | 1.30 (0.85, 2.01) | 0.98 (0.61, 1.58) |
| Hispanic | 67/212 (32) | 2.00 (1.44, 2.78)** | 1.53 (1.05, 2.22)* |
| Other | 25/99 (25) | 1.46 (0.91, 2.36) | 1.16 (0.69, 1.98) |
| Education | |||
| High school degree or less | 125/574 (22) | Ref | - |
| Some college | 73/389 (19) | 0.83 (0.60, 1.15) | - |
| Bachelor’s degree or higher | 123/538 (23) | 1.06 (0.80, 1.41) | - |
| Psychological reactance | |||
| Low | 251/1,089 (23) | Ref | Ref |
| High | 70/412 (17) | 0.68 (0.51, 0.92)* | 0.99 (0.71, 1.37) |
| Has a doctor or other health care provider ever told your child should get the HPV vaccine? |
|||
| No | 114/721 (16) | Ref | Ref |
| Yes | 207/780 (27) | 1.92 (1.49, 2.48)** | 1.13 (0.82, 1.55) |
| Relative importance of HPV vaccine compared to Tdap and meningococcal vaccines |
|||
| Less important | 74/736 (10) | Ref | Ref |
| As or more important | 247/765 (32) | 4.27 (3.21, 5.67)** | 2.76 (1.98, 3.83)** |
| The HPV vaccine might cause lasting health problems. | |||
| Disagree/neither | 279/1,153 (24) | Ref | Ref |
| Agree | 42/348 (12) | 0.43 (0.30, 0.61)** | 0.71 (0.47, 1.08) |
| The HPV vaccine is being pushed to make money for drug companies. |
|||
| Disagree/neither | 270/1,022 (26) | Ref | Ref |
| Agree | 51/479 (11) | 0.33 (0.24, 0.46)** | 0.47 (0.32, 0.69)** |
| I don’t have enough information about the HPV vaccine to decide whether to give it to my child. |
|||
| Disagree/neither | 247/1,022 (24) | Ref | Ref |
| Agree | 74/479 (16) | 0.57 (0.43, 0.76)** | 1.14 (0.80, 1.62) |
| The HPV vaccine is effective in preventing cervical cancer. |
|||
| Disagree/neither | 117/900 (13) | Ref | Ref |
| Agree | 204/601 (34) | 3.44 (2.66, 4.45)** | 2.55 (1.93, 3.37)** |
| It would be hard to find a provider or clinic where I can afford HPV vaccine for my child. |
|||
| Disagree/neither | 290/1,419 (20) | Ref | Ref |
| Agree | 31/82 (38) | 2.37 (1.49, 3.77)** | 2.50 (1.45, 4.33)** |
NOTE: HPV = Human papillomavirus; OR = Odds ratio; CI = confidence interval; Ref = Referent group. Dashes (−) indicate the variable was not included in the multivariable model because it was not statistically significant at the bivariate level.
Respondents from Virginia and Washington, DC. Rhode Island did not have a school-entry requirement at the time of data collection.
p < .05;
p < .01
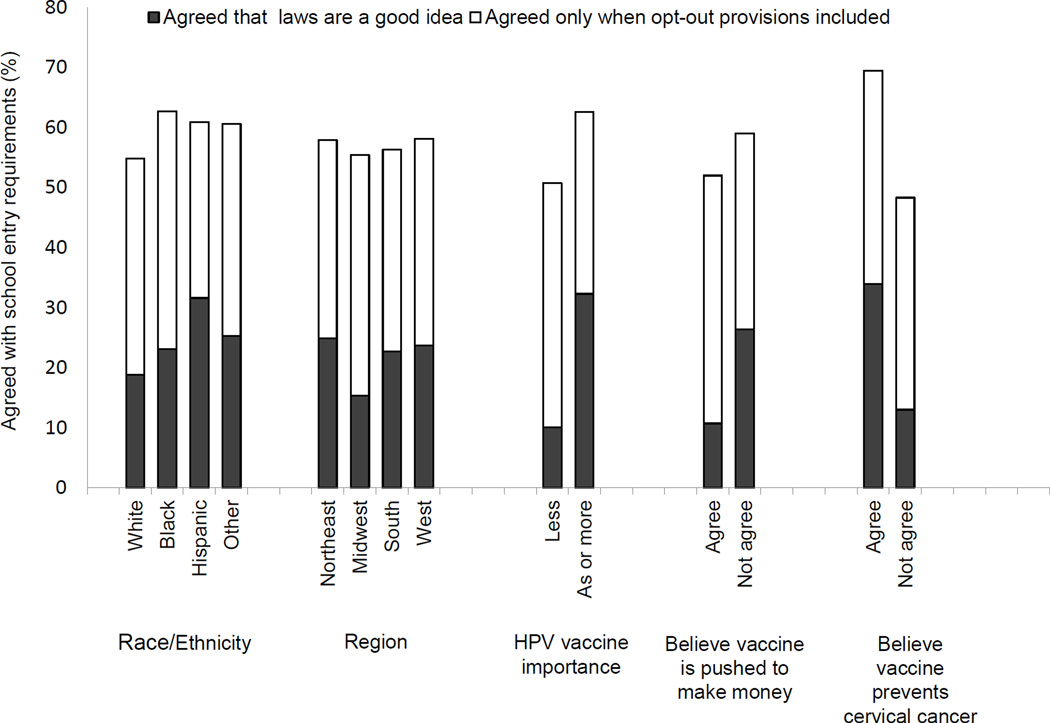
Support for HPV vaccine requirements that include opt-out provisions
Support for HPV vaccine school-entry requirements increased to 57% when including parents who agreed "these laws are okay only if parents can opt out" (Figure 1). Support for HPV vaccine requirements also increased when examined for each variable independently associated with agreeing that school-entry requirements “are a good idea” (Figure 2). In multivariable analysis, when including agreement with opt-out provisions, parents who believed HPV vaccine was effective in preventing cervical cancer (OR=2.18, 95% CI: 1.73–2.74) and believed HPV vaccine was as or more important than Tdap and meningococcal vaccines (OR=1.29, 95% CI: 1.02–1.66) still had higher odds of agreeing with school-entry requirements (data not shown). When opt-out provisions were included, no other variable associated with agreeing school-entry requirements “are a good idea” remained associated in multivariable analysis.
Figure 2.
Parental support for school-entry requirement laws with and without opt-out provisions.
NOTE: Black bars show the proportion of parents agreeing that HPV vaccine requirements “are a good idea,” when opt-out provisions were not mentioned in the statement, and white bars show the additional proportion of parents agreeing that “these laws are okay only if parents can opt out if they want to.”
Discussion
The present study, to our knowledge, is the first to employ a national sample to assess parental attitudes about HPV vaccine school-entry requirements. We found that 21% of parents agreed that school-entry requirements “are a good idea.” Previous studies reported higher levels of support than we observed; 46% of parents in five southeastern North Carolina counties (24) and 59% in Los Angeles (25) agreed with HPV vaccine school-entry requirements. However, such levels of support could be particular to those study participants and may not be generalizable to the general population because data were collected from individuals who lived in counties with elevated cervical cancer rates (25) or participated in a study about sexually transmitted infections (24). In addition, previous estimates of support could be higher because the response scale did not have a midpoint response option, thus requiring participants to take either side of the agree or disagree scale. In the present study, we found that 25% of the sample neither agreed nor disagreed with HPV vaccine school-entry requirements. Although some scholars debate that providing this response option makes it easier to respondents to avoid the mental process necessary to select their true response (30), other also argue that not everyone has strong thoughts one way or the other, even for very polarized policy issues (31). Public education and social marketing campaigns may be important for increasing support among parents who held middle-of-the-road attitudes about HPV vaccine requirements (32, 33).
Agreement with HPV vaccine school-entry requirements almost tripled when opt-out provisions were mentioned to parents, and disagreement decreased from 54% to 21%. Although vaccine opt-out provisions vary across state jurisdictions, in general, such provisions allow parents to refuse vaccination for any reasons. Previous research showed that some parents opt out vaccination for their child, or file non-medical exemptions, because opting out is far more convenient than completing the immunization schedule for school attendance (34). Broader opt-out provisions for HPV vaccination may have the effect of creating a culture of vaccine refusal and may lead parents to seek exemptions for other vaccines (19, 35). In Virginia and Washington, D.C., parents have broad authority to opt out HPV vaccination, but procedures vary by jurisdiction. Although both jurisdictions provide parents with information about HPV infection and the benefits of vaccination, only Washington, D.C. requires parents to sign a standardized form to opt out HPV vaccination. The impact of this process on HPV vaccination is unknown. The 2014 National Immunization Survey–Teen (NIS-Teen) shows that Virginia’s coverage for HPV vaccine initiation (59%) and 3-dose series completion (36%) for females aged 13–17 were below national averages (60% and 39%, respectively) (5). On the other hand, Washington, D.C. had one of the highest coverage levels for HPV vaccine initiation (75%) and completion (57%) in the U.S. Research is needed to investigate the extent to which different forms of opt-out provisions may contribute to or detract from vaccination.
A growing number of states are tightening opt-out provision and non-medical exemption requirements (36). Several states, for example, require parents to submit documentation that they received information about the benefits and risks of vaccination from health care providers before opting out (37). Similar informational steps and application processes might be added to existing and future HPV vaccine school-entry requirement laws to reduce the likelihood that parents will opt-out vaccination solely for convenience. It is also important to note that vaccine advocates have expressed caution that a poorly timed push for HPV vaccine school-entry requirements or changes in opt-out provision rules might provoke a public backlash (13, 18). In light of previous failures legislating HPV vaccine requirements, such policies should be judiciously conceived and well supported by key stakeholders (13, 17).
Our data showed that parents were less likely to agree with HPV vaccine school-entry requirements if they resided in Midwest states compared to Northeast states. This finding is novel in the literature because no previous research has examined support for such requirements across U.S. regions or states. Public support for school-entry requirements is key for state legislatures to introduce and enact such proposals (17), so understanding parents’ attitudes towards these requirements is important for informing state policy discussions. An analysis of HPV vaccine legislation reveals different patterns of legislative activity across U.S. regions (16). Since 2006, only half of the 12 states comprising the Midwest region introduced legislation requiring HPV vaccination for school attendance, and none of those policies was subsequently considered for enactment. In contrast, two-thirds of the 9 states in the Northeast region introduced legislation to adopt HPV vaccine school-entry requirements with Rhode Island successfully passing an administrative policy on the matter. Alternatively, three quarters of Midwestern states enacted laws to fund or educate the public or school children about HPV vaccination versus only a third of states in the Northeast region. Taken together, these data suggested that Midwest states have responded introducing and enacting legislation aimed to increase funding and information about the vaccine rather than require HPV vaccination for school entry. Our finding that parents living in the Midwest expressed low levels of support for HPV vaccine school-entry requirements may shed some light with regard to the failure of state legislatures in introducing and passing such legislation. Although, in the absence of school-entry requirements, other laws alone are unlikely to considerably raise HPV vaccine coverage rates, laws to increase awareness of and access to HPV vaccination may serve to complement state immunization programs (38). Research on the public’s opinions about a range of HPV vaccine policy strategies is needed to ensure that new legislative developments are carefully conceived and supported by state’s constituents.
Support for school-entry requirements was higher among Hispanic parents compared to other racial/ethnic groups. This finding is consistent with a previous study showing that HPV vaccine requirements for school entry were highly acceptable to Hispanics (25, 39). Data from the 2014 NIS-Teen showed higher rates of HPV vaccine initiation and 3-dose completion among Hispanic adolescents aged 13–17 than their non-Hispanic white counterparts (5). Hispanics’ cultural factors may explain their higher uptake of HPV vaccine and greater agreement with school-entry requirements compared to other populations (40). Robitz et al. (25) argued that Hispanics had a strong “respect for authority figures” and so, Hispanic parents may be more likely to agree with vaccine requirements because they are more likely to follow advice from health care professionals. Although we were unable to assess the effect of any cultural factors on the level of support for HPV vaccine school-entry requirements, previous data showed that Hispanic parents responding to survey research in Spanish were more supportive of such immunization requirements than those responding in English (25). Interestingly, other studies show a more positive effect of acculturation with regard to HPV vaccination. Gerend et al. (41), for example, reported that Hispanic parents who are more acculturated into U.S. society were more likely to get the HPV vaccine for their daughters. The specific mechanisms that account for the relationships between Hispanic ethnicity, acculturation, HPV vaccine uptake, and support for school-entry requirements are understudied. Nonetheless, the finding that Hispanics are consistently more supportive of HPV vaccine school-entry requirements suggests that Hispanic communities might be important partners in advocacy and vaccine campaign mobilization efforts.
We found that parents who believed HPV vaccine was as or more important than other adolescent vaccines were more likely to support school-entry requirements. In previous surveys we conducted with family physicians and pediatricians (42, 43), many reported that they endorse HPV vaccine less strongly than Tdap or meningococcal vaccines, often discuss it last, or recommend the vaccine as an optional vaccine. These low quality recommendation practices not only discourage parents from vaccinating their children but may also add distrust and suspicion with regard to HPV vaccine policies. Since physicians are an important source of vaccine information for parents (44, 45), better physician’s communication practices about HPV vaccine in relation to other adolescent vaccines may influence parents’ opinions about school-entry requirements. We also found that parents who had favorable perceptions of HPV vaccine effectiveness were more likely to support school-entry requirements. Our finding is consistent with previous research (25) and highlights the importance of continuing to communicate that the vaccine is a safe and effective health service to prevent cervical cancer, which kills 4,000 U.S. women each year. Since HPV vaccine is recommended for boys and girls, information about parents’ perceptions of vaccine effectiveness in preventing other HPV-attributable cancers may be important to increase support for school-entry requirements. Consistent with previous studies (24, 25), concerns about the involvement of drug companies in pushing HPV vaccination to make money were also associated with parents’ opinions about HPV vaccine school-entry requirements. Many authors argued that drug company lobbying, while not illegal, fueled the public belief that school-entry requirements were legislated solely to benefit such companies (18, 21). Our finding suggests that efforts for maintaining public trust in public health systems are crucial both for improving HPV vaccination and for the viability of legislating school-entry requirements.
Strengths of this research include a large, national sample of parents and a good survey response rate. In addition, the present study is the first to assess support for HPV vaccine school-entry requirements after the ACIP recommended that boys be routinely vaccinated. This study had several limitations. The survey asked about hypothetical school-entry requirements, rather than actual laws, and did not describe the scope of opt-out provisions. Parents’ support for school-entry requirements could differ when asked about actual legislation and may vary by type of opt-out provision (medical, religious, or philosophical exemptions). Future research should explore how support for school-entry requirements and correlates of parental support change with different types of opt-out provisions. The sample included 70% non-Hispanic Whites, which is a slightly higher proportion than the 62% of U.S. adults who identify themselves as such. Even so, our sample included meaningful numbers of non-Hispanic Black (9%) and Hispanic (14%) respondents, making this survey more racially and ethnically diverse than previous studies on this topic. Another limitation is that the survey was administered in English, so participants with limited English proficiency might have faced difficulties interpreting or responding to survey questions. Although participants needed an email account to receive an invitation to participate in the survey, the survey company facilitated the participation of respondents with lower access to technology by providing a laptop computer and free Internet access to those panel members who lacked these resources.
Although we focused on parents, we acknowledge that there are other key stakeholders contributing to policy considerations surrounding HPV vaccine school-entry requirements. Developing sound policy will require incorporating the perspectives of policymakers including whether these requirements should include nonmedical exemptions and, in such a case, the ease with which these opt-out provisions can be obtained by parents and reviewed by state officials (17). Research is needed to identify influential factors in determining how policymakers act on the issue of HPV vaccine requirements. Importantly, the perspectives of medical associations, state health departments, and school districts are also influential to the policymaking process. A recent study showed that 47% of physicians who provide primary care, including vaccines, to adolescents support HPV vaccine school-entry requirements (46). These stakeholders have been key actors advocating about health policies in the U.S (47). Because school-entry requirements are legislated on a state-by-state basis in the U.S., challenges arise with regard to the capacity of states to provide school-required vaccines, monitor compliance, and enforce such policies (48). Our study provides key information about the perspectives of parents towards HPV vaccine school-entry requirements, which can inform state policy discussions about this important topic.
Conclusion
Improving HPV vaccination coverage is a national priority. While school-entry requirements have proven to be a valuable policy mechanism to raise childhood and adolescent vaccination coverage in the U.S., they have also engendered controversy and debate in the case of HPV vaccination. Although school-entry requirements are viewed by some parents as an interference with parental autonomy and freedom of choice (21), through the years, other types of public health legislation (e.g., smoking restrictions, car seat belts, motorcycle helmets) have succeeded in the face of similar concerns (49). As many scholars suggest, before proposing HPV vaccine requirements states must strengthen their immunization programs and ensure that their constituents understand the benefits of HPV vaccination (18, 50). Likewise, the National Vaccine Advisory Committee recommends that states considering HPV vaccine school-entry requirements consider a range of issues including vaccine infrastructure and financing, disease burden and epidemiology, existing vaccine policies, and political and public support (35, 51). Thorough consideration of such issues will allow policymakers to address critical elements related to HPV vaccine requirements in order to ensure that new legislative proposals are carefully designed and supported by the public. Our study provides the first national assessment of parents’ attitudes about HPV vaccine school-entry requirement; our findings suggest that distinctive characteristics of the population may influence support for such laws. Support of school-entry requirements for HPV vaccination continues to be contingent upon the inclusion of opt-out provisions, which may negatively impact the effectiveness of these laws.
Acknowledgments
Financial support: This study was funded by Merck Sharp & Dohme Investigator Studies Program, grant #50928 (N.T. Brewer). Authors’ time was supported by grants from the National Cancer Institute: R25 CA116339 (W.A. Calo), K22 CA186979 (M.B. Gilkey), and F31 CA189411 (J.L. Moss). Funders played no role in: 1) study design; 2) the collection, analysis, and interpretation of data; 3) the writing of the report; or 4) the decision to submit the manuscript for publication. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Cancer Institute, the National Institutes of Health, or Merck Sharp & Dohme.
Brewer has received HPV vaccine-related grants from or been on paid advisory boards for Merck Sharp & Dohme and Pfizer; he served on the National Vaccine Advisory Committee Working Group on HPV Vaccine and is chair of the National HPV Vaccination Roundtable.
Footnotes
Disclosure of Potential Conflicts of Interest: The other authors of this paper have no financial disclosures or potential conflicts of interest to report.
References
- 1.President's Cancer Panel Annual Report. A Report to the President of the United States from the President’s Cancer Panel. Bethesda, MD: National Cancer Institute; 2014. Accelerating HPV Vaccine Uptake: Urgency for Action to Prevent Cancer. [Google Scholar]
- 2.Satterwhite CL, Torrone E, Meites E, Dunne EF, Mahajan R, Ocfemia MC, et al. Sexually transmitted infections among US women and men: prevalence and incidence estimates, 2008. Sex Transm Dis. 2013;40:187–193. doi: 10.1097/OLQ.0b013e318286bb53. [DOI] [PubMed] [Google Scholar]
- 3.Centers for Disease Control and Prevention (CDC) Human papillomavirus-associated cancers - United States, 2004–2008. MMWR Morb Mortal Wkly Rep. 2012;61:258–261. [PubMed] [Google Scholar]
- 4.Markowitz LE, Dunne EF, Saraiya M, Chesson HW, Curtis CR, Gee J, et al. Human papillomavirus vaccination: recommendations of the Advisory Committee on Immunization Practices (ACIP) MMWR Recomm Rep. 2014;63:1–30. [PubMed] [Google Scholar]
- 5.Reagan-Steiner S, Yankey D, Jeyarajah J, Elam-Evans LD, Singleton JA, Curtis CR, et al. National, Regional, State, and Selected Local Area Vaccination Coverage Among Adolescents Aged 13–17 Years - United States, 2014. MMWR Morb Mortal Wkly Rep. 2015;64:784–792. doi: 10.15585/mmwr.mm6429a3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.U.S. Department of Health and Human Services. Washington DC: U.S. Department of Health and Human Services; 2014. [cited 2015 Sept 16]. 2020 topics and objectives: Immunization and infectious diseases objectives. Available from: http://www.healthypeople.gov/2020/topics-objectives/topic/immunization-and-infectious-diseases/objectives?topicId=23. [Google Scholar]
- 7.Hinman AR, Orenstein WA, Williamson DE, Darrington D. Childhood immunization: laws that work. J Law Med Ethics. 2002;30:S122–S127. [PubMed] [Google Scholar]
- 8.Orenstein WA, Hinman AR. The immunization system in the United States - the role of school immunization laws. Vaccine. 1999;17:S19–S24. doi: 10.1016/s0264-410x(99)00290-x. [DOI] [PubMed] [Google Scholar]
- 9.Wilson TR, Fishbein DB, Ellis PA, Edlavitch SA. The impact of a school entry law on adolescent immunization rates. J Adolesc Health. 2005;37:511–516. doi: 10.1016/j.jadohealth.2005.07.009. [DOI] [PubMed] [Google Scholar]
- 10.Task Force on Community Preventive Services. Recommendations regarding interventions to improve vaccination coverage in children, adolescents, and adults. Am J Prev Med. 2000;18:S92–S96. [PubMed] [Google Scholar]
- 11.National Conference of State Legislatures. States with Religious and Philosophical Exemptions from School Immunization Requirements. Washington DC: National Conference of State Legislatures; 2016. [cited 2016 February 24]. Available from: www.ncsl.org/research/health/school-immunization-exemption-state-laws.aspx. [Google Scholar]
- 12.Gostin LO. Law, ethics, and public health in the vaccination debates: Politics of the measles outbreak. JAMA. 2015;313:1099–1100. doi: 10.1001/jama.2015.1518. [DOI] [PubMed] [Google Scholar]
- 13.Horlick G, Shaw FE, Gorji M, Fishbein DB. Delivering new vaccines to adolescents: The role of school-entry laws. Pediatrics. 2008;121:S79–S84. doi: 10.1542/peds.2007-1115I. [DOI] [PubMed] [Google Scholar]
- 14.Yang YT, Silverman RD. Legislative prescriptions for controlling nonmedical vaccine exemptions. JAMA. 2015;313:247–248. doi: 10.1001/jama.2014.16286. [DOI] [PubMed] [Google Scholar]
- 15.Wang E, Clymer J, Davis-Hayes C, Buttenheim A. Nonmedical exemptions from school immunization requirements: a systematic review. Am J Public Health. 2014;104:e62–e84. doi: 10.2105/AJPH.2014.302190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.National Conference of State Legislatures. HPV Vaccine Policies. Washington DC: National Conference of State Legislatures; 2016. [cited 2015 Sept 16]. Available from: http://www.ncsl.org/research/health/hpv-vaccine-state-legislation-and-statutes.aspx. [Google Scholar]
- 17.Colgrove J, Abiola S, Mello MM. HPV vaccination mandates--lawmaking amid political and scientific controversy. N Engl J Med. 2010;363:785–791. doi: 10.1056/NEJMsr1003547. [DOI] [PubMed] [Google Scholar]
- 18.Gostin LO. Mandatory HPV vaccination and political debate. JAMA. 2011;306:1699–1700. doi: 10.1001/jama.2011.1525. [DOI] [PubMed] [Google Scholar]
- 19.Javitt G, Berkowitz D, Gostin LO. Assessing mandatory HPV vaccination: who should call the shots? J Law Med Ethics. 2008;36:384–395. doi: 10.1111/j.1748-720X.2008.00282.x. [DOI] [PubMed] [Google Scholar]
- 20.Gilkey MB, Brewer NT. Mandatory HPV vaccination. JAMA. 2012;307:252–253. doi: 10.1001/jama.2011.2018. author reply 4–5. [DOI] [PubMed] [Google Scholar]
- 21.Haber G, Malow RM, Zimet GD. The HPV vaccine mandate controversy. J Pediatr Adolesc Gynecol. 2007;20:325–331. doi: 10.1016/j.jpag.2007.03.101. [DOI] [PubMed] [Google Scholar]
- 22.Burstein P. The impact of public opinion on public policy: A review and an agenda. Polit Res Q. 2003;56:29–40. [Google Scholar]
- 23.Horn L, Howard C, Waller J, Ferris DG. Opinions of parents about school-entry mandates for the human papillomavirus vaccine. J Low Genit Tract Dis. 2010;14:43–48. doi: 10.1097/LGT.0b013e3181b0fad4. [DOI] [PubMed] [Google Scholar]
- 24.Smith JS, Brewer NT, Chang Y, Liddon N, Guerry S, Pettigrew E, et al. Acceptability of school requirements for human papillomavirus vaccine. Hum Vaccin. 2011;7:952–957. doi: 10.4161/hv.7.9.15995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Robitz R, Gottlieb SL, De Rosa CJ, Guerry SL, Liddon N, Zaidi A, et al. Parent attitudes about school requirements for human papillomavirus vaccine in high-risk communities of Los Angeles, California. Cancer Epidemiol Biomarkers Prev. 2011;20:1421–1429. doi: 10.1158/1055-9965.EPI-10-1236. [DOI] [PubMed] [Google Scholar]
- 26.GfK. [cited 2015 Sept 16];GfK Knowledge Panel. 2015 Available from: http://www.gfk.com/us/Solutions/consumer-panels/Pages/GfK-KnowledgePanel.aspx. [Google Scholar]
- 27.American Association for Public Opinion Research (AAPOR) Standard definitions: final dispositions of case codes and outcome rates for surveys. Lenexa, Kansas: American Association for Public Opinion Research; 2008. [Google Scholar]
- 28.Dillard JP, Shen L. On the Nature of Reactance and its Role in Persuasive Health Communication. Commun Monogr. 2005;72:26. [Google Scholar]
- 29.McRee AL, Brewer NT, Reiter PL, Gottlieb SL, Smith JS. The Carolina HPV immunization attitudes and beliefs scale (CHIAS): scale development and associations with intentions to vaccinate. Sex Transm Dis. 2010;37:234–239. doi: 10.1097/OLQ.0b013e3181c37e15. [DOI] [PubMed] [Google Scholar]
- 30.Dilman DA, Smyth JD, Christian LM. The Tailored Design Method. Hoboken, NJ: Wiley; 2014. Internet, Phone, Mail and Mixed-Mode Surveys. [Google Scholar]
- 31.Baka AF, Figgou L, Triga V. 'Neither agree, nor disagree': a critical analysis of the middle answer category in Voting Advice Applications. Int J Electronic Governance. 2012;5:244–263. [Google Scholar]
- 32.Pitts MJ, Adams Tufts K. Implications of the Virginia human papillomavirus vaccine mandate for parental vaccine acceptance. Qual Health Res. 2013;23:605–617. doi: 10.1177/1049732312470871. [DOI] [PubMed] [Google Scholar]
- 33.St John B, 3rd, Pitts M, Tufts KA. Disconnects between news framing and parental discourse concerning the state-mandated HPV vaccine: implications for dialogic health communication and health literacy. Commun Med. 2010;7:75–84. doi: 10.1558/cam.v7i1.75. [DOI] [PubMed] [Google Scholar]
- 34.Rota JS, Salmon DA, Rodewald LE, Chen RT, Hibbs BF, Gangarosa EJ. Processes for obtaining nonmedical exemptions to state immunization laws. Am J Public Health. 2001;91:645–648. doi: 10.2105/ajph.91.4.645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.National Vaccine Advisory Committee. Mandates for adolescent immunizations: recommendations from the National Vaccine Advisory Committee. Am J Prev Med. 2008;35:145–151. doi: 10.1016/j.amepre.2008.03.033. [DOI] [PubMed] [Google Scholar]
- 36.Diekema DS. Personal belief exemptions from school vaccination requirements. Annu Rev Public Health. 2014;35:275–292. doi: 10.1146/annurev-publhealth-032013-182452. [DOI] [PubMed] [Google Scholar]
- 37.Lillvis DF, Kirkland A, Frick A. Power and persuasion in the vaccine debates: an analysis of political efforts and outcomes in the United States, 1998–2012. Milbank Q. 2014;92:475–508. doi: 10.1111/1468-0009.12075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Laugesen MJ, Mistry R, Carameli KA, Ribisl KM, Needleman J, Bastani R. Early policy responses to the human papillomavirus vaccine in the United States, 2006–2010. J Adolesc Health. 2014;55:659–664. doi: 10.1016/j.jadohealth.2014.04.015. [DOI] [PubMed] [Google Scholar]
- 39.Perkins RB, Pierre-Joseph N, Marquez C, Iloka S, Clark JA. Parents' opinions of mandatory human papillomavirus vaccination: does ethnicity matter? Womens Health Issues. 2010;20:420–426. doi: 10.1016/j.whi.2010.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Yeganeh N, Curtis D, Kuo A. Factors influencing HPV vaccination status in a Latino population; and parental attitudes towards vaccine mandates. Vaccine. 2010;28:4186–4191. doi: 10.1016/j.vaccine.2010.04.010. [DOI] [PubMed] [Google Scholar]
- 41.Gerend MA, Zapata C, Reyes E. Predictors of human papillomavirus vaccination among daughters of low-income Latina mothers: the role of acculturation. J Adolesc Health. 2013;53:623–629. doi: 10.1016/j.jadohealth.2013.06.006. [DOI] [PubMed] [Google Scholar]
- 42.Gilkey MB, Moss JL, Coyne-Beasley T, Hall ME, Shah PD, Brewer NT. Physician communication about adolescent vaccination: How is human papillomavirus vaccine different? Prev Med. 2015;77:181–185. doi: 10.1016/j.ypmed.2015.05.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.McRee AL, Gilkey MB, Dempsey AF. HPV vaccine hesitancy: findings from a statewide survey of health care providers. J Pediatric Health Care. 2014;28:541–549. doi: 10.1016/j.pedhc.2014.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Brewer NT, Gottlieb SL, Reiter PL, McRee AL, Liddon N, Markowitz L, et al. Longitudinal predictors of human papillomavirus vaccine initiation among adolescent girls in a high-risk geographic area. Sex Transm Dis. 2011;38:197–204. doi: 10.1097/OLQ.0b013e3181f12dbf. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Reiter PL, McRee AL, Pepper JK, Gilkey MB, Galbraith KV, Brewer NT. Longitudinal predictors of human papillomavirus vaccination among a national sample of adolescent males. Am J Public Health. 2013;103:1419–1427. doi: 10.2105/AJPH.2012.301189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Califano S, Calo WA, Weinberger M, Gilkey MB, Brewer NT. Physician support of HPV vaccination school-entry requirements. Hum Vaccin Immunother. doi: 10.1080/21645515.2016.1149275. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Gruen RL, Campbell EG, Blumenthal D. Public roles of US physicians: community participation, political involvement, and collective advocacy. JAMA. 2006;296:2467–2475. doi: 10.1001/jama.296.20.2467. [DOI] [PubMed] [Google Scholar]
- 48.Hendrix KS, Sturm LA, Zimet GD, Meslin EM. Ethics and Childhood Vaccination Policy in the United States. Am J Public Health. 2016;106:273–278. doi: 10.2105/AJPH.2015.302952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Jones MM, Bayer R. Paternalism and its discontents: motorcycle helmet laws, libertarian values, and public health. Am J Public Health. 2007;97:208–217. doi: 10.2105/AJPH.2005.083204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Schwartz JL, Caplan AL, Faden RR, Sugarman J. Lessons from the failure of human papillomavirus vaccine state requirements. Clin Pharmacol Ther. 2007;82:760–763. doi: 10.1038/sj.clpt.6100397. [DOI] [PubMed] [Google Scholar]
- 51.National Vaccine Advisory Committee. The promise and challenge of adolescent immunization. Am J Prev Med. 2008;35:152–157. doi: 10.1016/j.amepre.2008.03.034. [DOI] [PubMed] [Google Scholar]