Abstract
While therapy with mineralocorticoid receptor antagonists (MRA) is recommended for patients with chronic heart failure (HF) with reduced ejection fraction and in post-infarction HF, it has not been studied well in acute HF (AHF) despite being commonly used in this setting. At high doses, MRA therapy in AHF may relieve congestion through its natriuretic properties and mitigate the effects of adverse neurohormonal activation associated with intravenous loop diuretics. The Aldosterone Targeted Neurohormonal Combined with Natriuresis Therapy in Heart Failure (ATHENA-HF) trial is a randomized, double blind, placebo-controlled study of the safety and efficacy of 100 mg daily spironolactone vs. placebo (or continued low-dose spironolactone use in participants who are already receiving spironolactone at baseline) in 360 patients hospitalized for AHF. Patients are randomized within 24 hours of receiving the first dose of intravenous diuretics. The primary objective is to determine if high-dose spironolactone, when compared to standard care, will lead to greater reductions in N-terminal pro-B-type natriuretic peptide levels from randomization to 96 hours. The secondary endpoints include changes in the clinical congestion score, dyspnea relief, urine output, weight change, loop diuretic dose, and inhospital worsening HF. Index hospital length of stay and 30-day clinical outcomes will be assessed. Safety endpoints include risk of hyperkalemia and renal function. Differences among patients with reduced versus preserved ejection fraction will be determined.
Keywords: Heart failure, acute heart failure, hospitalization, mineralocorticoid receptor antagonist, aldosterone, natriuretic peptides
Heart failure (HF) accounts for over a million hospitalizations in the United States annually.1, 2 Hospitalizations for HF are associated with a significantly elevated risk for post-discharge mortality and recurrent hospitalizations. Mortality or readmission risk at 60-days post discharge is ~30% and may be as high as 50% by 6 months in these patients.3–7 While therapy for chronic HF with reduced ejection fraction has evolved over time favorably impacting survival, outcomes for patients with acute heart failure (AHF) have not changed much in the past two decades. Thus far none of the trials have shown an improvement in post-discharge outcomes in patients with acute heart failure.8, 9 Thus there remains a pressing need to develop interventions that can improve outcomes safely in this high-risk group of patients.
PERSISTENT CONGESTION AND OUTCOMES IN ACUTE HEART FAILURE
Worsening congestion is the main reason for hospitalization for the majority of AHF patients and diuretics remains the mainstay of therapy. Even with the use of intravenous diuretics, over half of the patients lose ≤5 lbs. and up to 20% may actually gain weight during hospitalization.10 Despite improvement in symptoms, a large proportion of these patients continue to have persistent congestion at discharge,11 which whether measured clinically,12, 13 with right heart catheterization, or by natriuretic peptide levels,14,15 predict post-discharge outcome. Persistent congestion may be sub-clinical, related to diuretic resistance, or when further diuretic use is difficult in the face of worsening renal function.
IMPORTANCE OF ALDOSTERONE IN ACUTE HEART FAILURE
The renin-angiotensin-aldosterone-system (RAAS) is activated in HF. In normal subjects, aldosterone levels range between 2–9 ng/dL but in one AHF trial, median levels were 11.0 ng/dL and were over the upper normal range in 33.2% of patients.16 Aldosterone levels are only transiently suppressed with ACE inhibition. Intravenous loop diuretic use in AHF further intensifies RAAS activation and secondary hyperaldosteronism17, 18, enhancing proximal tubular sodium absorption and decreased distal sodium delivery, impairing the normal escape mechanism from the sodium-retaining effect of aldosterone. Therefore, beyond myocardial and vascular adverse effects, hyperaldosteronism directly contributes to diuretic resistance.19 Loop diuretics also block sodium chloride transport at the macula densa, which stimulates the RAAS independent of renal sodium loss17. (Figure 1)
Figure 1. Mechanism of Diuretic Resistance and Potential Benefit with Mineralocorticoid Antagonists.
From Bansal S, Lindenfeld J, Schrier RW. Sodium Retention in Heart Failure and Cirrhosis: Potential Role of Natriuretic Doses of Mineralocorticoid Antagonist? Circ Heart Fail 2009:2:373. Reprinted with permission of Wolters Kluwer Health
MINERALOCORTICOID RECEPTOR ANTAGONIST USE IN ACUTE HEART FAILURE
The low dose mineralocorticoid receptor antagonists (MRA) used in chronic HF are believed to benefit patients by anti-fibrotic but not natriuretic effects.20 Inhibition of mineralocorticoid receptors at higher MRA doses may cause significant natriuresis. Resistance to loop diuretics in AHF may be overcome by natriuretic doses of spironolactone (>50 mg/day).19 In a study of 6 HF patients, 200 mg twice a day of spironolactone caused a marked increase in sodium excretion leading to negative sodium balance.21 In another study, patients with severe HF who were resistant to high-dose loop diuretics responded with increased natriuresis with the use of 100 mg/day spironolactone.22
The clinical benefit and safety of high dose MRA use in AHF was recently supported by a single-center, single-blind trial of 100 patients treated with standard therapy alone or with addition of spironolactone initiated within 24 hours.23 Spironolactone dose was 94.5±23.3 mg on day 1 and 62.7±24.3 mg on day 3. Increase in creatinine by ≥0.3 mg/dL from day 1 to day 3 was more likely to occur in the standard of care arm (20% vs. 4%; P=0.038). Plasma N-terminal pro B-type natriuretic peptide (NT-proBNP) levels were comparable at baseline but were lower in the spironolactone group at day 3 (2488 [4579] pg/ml in controls vs. 1555 [1832] pg/ml in spironolactone group; P=0.05). A greater proportion of patients in the spironolactone group were free of congestion at day 3 and a higher proportion had transitioned from intravenous to oral furosemide (82% vs. 44%; P<0.001). These findings support the safety and potential efficacy of a high-dose spironolactone strategy in AHF. However, this was a single center non-randomized study and the intervention was not blinded to the investigators, which raises concerns for potential bias. While high dose MRA may be effective in the setting of congestion, increased risks of hyperkalemia or elevation in creatinine also need to be studied further.24
In the EVEREST trial, which enrolled patients with left ventricular ejection fraction of <40% who were hospitalized for acute heart failure and were receiving standard therapy, median baseline aldosterone blood level was 11.0 ng/dL (25–75 percentile: 2–21 ng/dL and was over the upper normal range in 33.2% of patients. Median aldosterone levels increased during hospital stay from 11 ng/dL at baseline to 15 ng/dL at discharge (P<0.001) and remained increased 6 months after discharge (16 ng/dL, P<0.001 vs. baseline). Higher serum aldosterone levels correlated with worse post-discharge outcomes. After a median follow-up of 9.9 months, higher baseline aldosterone levels were associated with an increased risk for mortality and the combined endpoint of cardiovascular mortality plus heart failure readmission in adjusted models (HR 1.49, 95% CI 1.11–1.99; and HR 1.40, 95% CI 1.11–1.78, respectively), in the highest quartile when compared with the lowest.16
RISK FOR HYPERKALEMIA
Most of the data on hyperkalemia with MRAs is in chronic HF. In AHF, hypokalemia is more common and is often due to a defect in Na+/K+-ATPase activity and an intracellular potassium shift caused by oxidative stress and neurohormonal activation in combination with loop diuretic use.25 Spironolactone is rapidly metabolized to several metabolites that produce natriuretic and antikaliuretic effects.26 While the natriuretic effects decline over a period of 48–72 hours, the antikaliuretic effects may be observed for several days following discontinuation, underscoring the importance of careful monitoring of potassium levels, especially in patients with chronic kidney disease.27 In a study in six chronic HF patients, 200mg bid of spironolactone led to negative sodium balance without significant increases in potassium levels (3.9 to 4.1 mmol/L) or changes in creatinine clearance after 4 days.21 In 18 patients with advanced HF receiving 50–200 mg of spironolactone in addition to standard treatment, there was no significant increase in serum potassium (4.0 vs. 4.2 mEq/l) or creatinine (1.3 vs. 1.4 mg/dl) during an average follow up of 41 weeks.28 In an AHF study assessing 50–100 mg spironolactone use, serum potassium did not differ between control vs. spironolactone groups (3.9 vs. 4.1 mmol/L respectively) at day 3 (p=0.15). 23
ENDPOINTS IN ACUTE HEART FAILURE
Congestion is the most common manifestation of AHF and is related with both symptoms and prognosis. Persistent congestion at discharge is associated with worse outcomes. The effectiveness of decongestion can be measures in multiple ways.
Natriuretic Peptide Levels
Natriuretic peptide are markers of wall stretch and have advantage over clinical signs for assessment of congestion due to the lack of sensitivity and inter-rater reliability of examination. Even with symptom relief, readmission and mortality risk remains high if natriuretic peptides stay elevated in patients with AHF. Baseline levels and changes in hospital are both associated with filling pressures and outcomes, with best outcomes seen when natriuretic peptide levels decrease by >30% in hospital.29 Discharge natriuretic peptide levels are superior to admission levels or change in levels during hospitalization for predicting risk.30
Dyspnea
In several studies, dyspnea improvement in AHF was associated with improved outcomes post-discharge. In the Acute Study of Clinical Effectiveness of Nesiritide in Decompensated Heart Failure (ASCEND-HF) trial, early dyspnea relief measured on a 7-point Likert scale was associated with lower 30-day mortality or HF hospitalization risk.31 In the Efficacy and Safety of Relaxin for the Treatment of Acute Heart Failure (RELAX-AHF) trial, serelaxin was associated with both improvement in dyspnea assessed by Visual Analog Scale and lower 6-month mortality risk.32 Thus significant and early improvement in dyspnea may predict improved long-term outcomes, besides being a therapeutic goal by itself.
Clinical Congestion Score
In the Efficacy of Vasopressin Antagonism in Heart Failure Outcome Study with Tolvaptan (EVEREST) trial, a modified composite congestion score at discharge calculated by summing the individual scores for orthopnea, jugular venous distension, and pedal edema (on a standardized 4-point scale ranging from 0 to 3) was predictive of 30-day all-cause mortality (HR 1.34, 95%CI 1.14–1.58), and combined morality and HF readmission risk (HR 1.13, 95%CI 1.03–1.25).12
Mortality
Mortality reduction is the gold standard outcome for clinical trials in chronic heart failure. Though several previous trials focused primarily on symptom improvement in clinical trials for acute heart failure, it is now well recognized that symptom improvement during hospitalization is an inconsistent predictor of post-discharge mortality.33, 34 In fact therapies like inotropes may improve symptoms and worsen the risk for mortality. In-hospital mortality for patients with acute heart failure is low but the main concern is the very high (up to 30% one-year) post discharge mortality.35 Thus assessing post-discharge mortality as both an efficacy and safety outcome in this high-risk group of acute heart failure patients is imperative.
Readmissions
Similar to mortality, readmission post discharge from an acute heart failure hospitalization also remains a critical endpoint, both from a clinical and an economic perspective.36 From a clinical perspective, recurrent hospitalizations are associated with a change in the natural history trajectory of the disease process, with each hospitalization portending a worse prognosis subsequently.37 From an economic perspective, recurrent hospitalizations account for the largest proportion of direct cost of care for heart failure. Considering that heart failure is the number one discharge diagnosis in the United States for the Medicare beneficiaries, there are now financial penalties imposed by the Centers for Medicare and Medicaid Services for hospitals that have a high rate of readmission post discharge after an acute heart failure hospitalization. Thus effective therapies for these patients should preferably translate into a reduction in risk for readmissions.
In-hospital Worsening Heart Failure
Acute worsening heart failure (WHF) is reported in a sizable portion of patients hospitalized for heart failure, and is increasingly being recognized as an entity that is associated with an adverse in-hospital course.35 WHF is generally defined as worsening heart failure symptoms and signs requiring an intensification of therapy, and is reported to be seen in anywhere from 5% to 42% of heart failure admissions.37 Recent data suggest that some experimental therapies may reduce the risk of development of WHF among hospitalized heart failure patients, and this is associated with a reduction in the risk of subsequent post-discharge cardiovascular mortality.38 In this respect, WHF holds promise as an endpoint for acute heart failure clinical trials. However, a better understanding of the pathophysiology and a consensus on the definition of WHF is still needed and until then, it serves as a potential secondary endpoint.
THE ALDOSTERONE TARGETED NEUROHORMONAL COMBINED WITH NATRIURESIS THERAPY IN HEART FAILURE (ATHENA-HF) TRIAL
Study Design
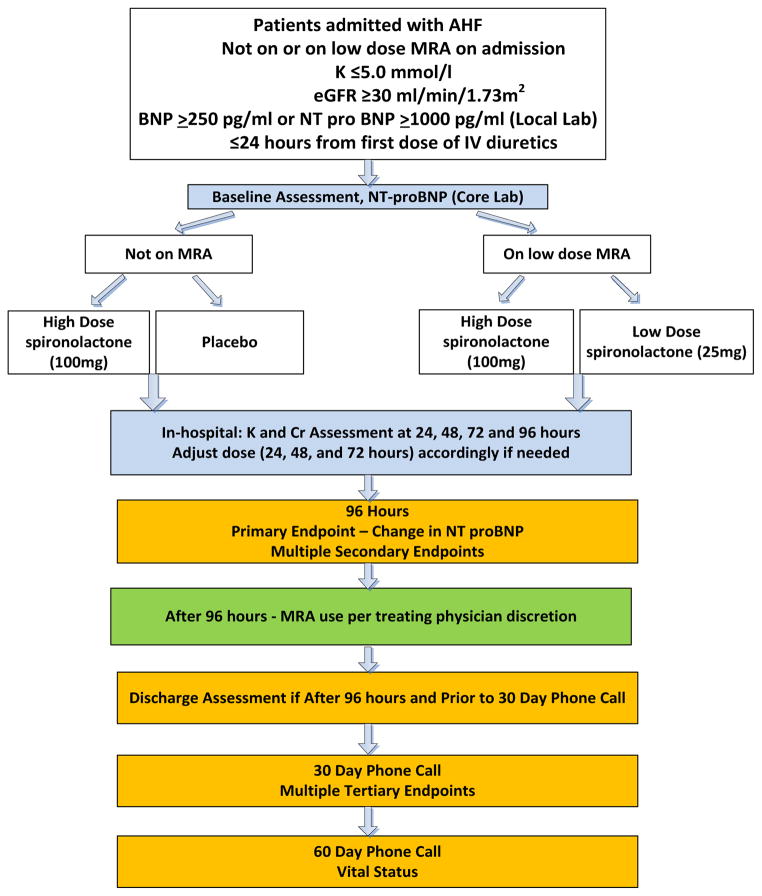
The ATHENA-HF trial is a randomized, double blind, placebo controlled trial assessing the impact of high dose spironolactone vs. placebo (or continued lose dose spironolactone use) on natriuretic peptide levels among patients hospitalized for AHF. The study schema is presented in the Central Illustration.
Central Illustration. ATHENA-HF Trial Schema.
AHF: acute heart failure; BNP: B-type natriuretic peptide; Cr: creatinine; eGFR: estimated glomerular filtration rate; K+: potassium; MRA: mineralocorticoid receptor antagonist; NTproBNP: N terminal pro B-type natriuretic peptide
Objective
To determine if high-dose spironolactone administered to patients with AHF will lead to greater reductions in N-terminal pro-B-type natriuretic peptide (NT-proBNP) levels from randomization to 96 hours compared to standard of care. In order to assess the early use of natriuretic doses of spironolactone in AHF and its impact on preventing diuretic resistance, the study intervention is initiated within 24 hours of the first dose of intravenous diuretics.
Eligibility and Intervention
Eligibility criteria are listed in Table 1. Patients hospitalized with at least one sign and one symptoms of AHF with an NT-proBNP ≥1000 pg/mL or BNP ≥250 pg/mL measured within 24 hours from randomization are eligible. Patients who are either not on spironolactone therapy at home or those who are on low dose spironolactone (12.5 or 25 mg per day) are eligible. Patients must have serum potassium concentration ≤5.0mmol/L, an estimated glomerular filtration rate (eGFR) ≥30 mL/min/1.73m2 and systolic blood pressure >90 mmHg.
Table 1.
Eligibility Criteria for the ATHENA-HF Trial
Inclusion Criteria
|
Exclusion Criteria
|
Patients who are not on spironolactone at home are randomized to 100mg spironolactone or placebo. Those already on 12.5 or 25 mg per day spironolactone are randomized to 100 mg or 25 mg per day but not to placebo, to avoid ethical concerns with discontinuing chronic therapy. Patients on eplerenone will not be included as in the acute setting it may not be easily known if the patient has been previously intolerant to spironolactone. Patients already taking >25 mg of spironolactone will be excluded due to potential overlap with natriuretic potential of intermediate dose spironolactone use.
Baseline Evaluations
Baseline evaluation includes history, physical examination, vital signs and body weight assessment, review of medications, measurement of renal function and electrolytes, dyspnea assessments (7-point Likert and Visual Analog Scale measured off oxygen for >3 minutes), pregnancy test for women of childbearing potential, and collection of blood for core laboratory measurement of NT-proBNP level.
Duration of Intervention
The median length of stay for HF hospitalization in the United States is 4.3 days.39 In order to have comparable efficacy assessment within the two arms and avoid comparing outcomes among patients with potentially different lengths of stay, and to conform with the prevalent norms of the duration of hospitalization, the duration of intervention and the primary endpoint assessment was chosen to be 96 hours.
Volume Assessment and Dose Adjustment
All other medications, including diuretics, are left at the discretion of the treating physician. The study drug is discontinued after 96 hours and further MRA use is left to the treating physician’s discretion. If the patient is clinically euvolemic in <96 hours, the investigators may consider changing loop diuretics to oral dosing.
Ejection Fraction
Ejection fraction measured within 6 months prior to randomization is obtained. Those without this information undergo ejection fraction assessment by any modality during the hospitalization. Patients will be eligible regardless of ejection fraction and therefore this determination does not need to precede randomization. Ejection fraction assessment is performed for a pre-specified secondary analysis to ascertain possible differential effects of intervention in patients with reduced vs. preserved ejection fraction.
Renal Function and Hyperkalemia
Modest increase in serum creatinine with diureses seen in many patients with AHF that usually reverses over time. In some patients however, a rise in serum creatinine portend poor prognosis.40 There remains clinical concern about acute kidney injury with high dose MRA use in AHF. The decision regarding management of patients with worsening creatinine is left to the discretion of the treating physicians. It is recommended that,
If serum creatinine is increased ≤0.5 mg/dl and the patient is diuresing and improving, and is still fluid overloaded, continue study drug per protocol
If serum creatinine is increased >0.5 mg/dl and the patient is diuresing and clinically improving but is still fluid overloaded, consider decreasing study drug to 50 mg
If the patient becomes oliguric with worsening serum creatinine and develops acute kidney injury criteria, hold study drug and reassess in 24 hours
To closely follow the patients to mitigate the risk of hyperkalemia, electrolytes are measured at least every 24h until 96h and at discharge. Potassium supplementation and potassium containing salt substitutes are discontinued and high potassium containing foods are avoided during the study protocol. Study drug dose is adjusted based on serum potassium level as shown in Table 2.
Table 2.
Protocol for Study Drug Adjustment based on Serum Potassium Concentration
| Serum Potassium concentration | Action | Protocol |
|---|---|---|
| ≤ 5.0 mmol/L | Continue protocol | |
| 5.1–6.0 mmol/L | Check if sample hemolyzed | Hold protocol Repeat K within 6 hours |
| Check if K+ supplement given | ||
| Treat per physician preference | ||
| If repeat value is ≤5.0 - | Continue protocol | |
| If repeat value is 5.1–6.0 Treat according to physician preference |
Hold protocol Repeat K next day and follow protocol If day 4 – Stop study protocol |
|
| If repeat value is >6.0 | Stop study drug | |
| > 6.0 mmol/L | Check if sample hemolyzed | |
| Check if K+ supplement given | ||
| Treat per physician preference | ||
| If sample not hemolyzed and patient not on K+ supplements | Stop study drug | |
| If sample hemolyzed or patient receiving K+ | Repeat K within 6 hours | |
| supplements - | ||
| If repeat value is ≤5.0 | Continue protocol | |
| If repeat value is between 5.1–6.0 | Hold protocol Repeat K next day and follow protocol If day 4 – Stop study drug |
|
| If repeat value is >6.0 | Stop study drug |
Endpoints
Efficacy
The primary endpoint of ATHENA-HF is the proportional change in NT-proBNP from randomization to 96 hours. Multiple secondary endpoints from randomization to 96 hours are also assessed, including, a) clinical congestion score; b) dyspnea relief by Likert and by Visual Analog Scales; c) net urine output; d) weight change; e) loop diuretic dose need in furosemide dose equivalents, and f) development of in-hospital worsening HF, defined as worsening HF signs and symptoms requiring additional therapy.
Exploratory analyses include a day-30 post randomization telephone call to ascertain, a) all-cause mortality, b) all-cause readmissions, c) outpatient worsening HF, defined as HF readmission or emergency department visits or need for outpatient IV diuretics, d) MRA use and loop diuretic dose requirement at day 30 and e) length of stay for index hospitalization. All participants are also contacted by telephone at 60±3 days to assess vital status.
Safety
Safety endpoints include change in serum creatinine and incidence of hyperkalemia (>5.5mmol/L or >6.0mmol/L) from randomization to 96 hours post randomization.
STATISTICAL CONSIDERATIONS
Sample Size and Power Calculations
Prior HF network data suggest that the standard deviation for the proportional change (on the log scale) in NT-proBNP from randomization to 96 hours is approximately 0.55 to 0.60.41 It is anticipated that 25% of subjects enrolled will be on low-dose MRA at randomization. Assuming a 20% reduction in NT-proBNP from enrollment in the MRA group compared to placebo for the subset of patients not on an MRA at enrollment and a 10% improvement in the subset on low-dose MRA at baseline yields an overall benefit of 17.5% for the study population. With a 1:1 randomization and a two-sided type I error rate of 0.05, a total sample size of 360 subjects would provide approximately 85% power. These calculations are based on the two-sample t-test. For the sensitivity analysis using the worst-rank approach for missing values due to death, the total sample size of 360 subjects provides 90% power to detect a difference in the setting in which a randomly selected individual on high dose spironolactone has a 60% chance of having a better response than a randomly selected individual on the placebo/low-dose arm. Both calculations allow for a consent withdrawal rate of approximately 2%. For continuous secondary endpoints, the study will have ≈90% power to detect differences of 0.35 standard deviations between treatment groups. These calculations assume a common variance and normally distributed errors for the two-sample t-test with a two-sided type I error rates of 0.05.
There is potential for greater reductions in natriuretic peptide levels in patients in the placebo arm of the study based on the special expertise for heart failure management at the sites where patients are being enrolled, though this is a concern with most heart failure trials where the placebo arm outcomes are better than seen in real-life based on similar concerns.
Statistical Analysis
The primary analysis will be based on a regression model using an outcome variable based on the log of the proportional change in NT-proBNP from randomization to 96 hours. The primary analysis will use a linear regression model with an indicator variable for treatment assignment, an indicator for MRA use prior to admission, and the log of the baseline NT-proBNP level. Missing values of the 96-hour NT-proBNP levels will be imputed using a multiple imputation algorithm.42 In a sensitivity analysis, values missing due to death will be imputed to the worst possible value. This analysis will account for low-dose MRA at enrollment using a stratified version of the Wilcoxon-Mann-Whitney test.
General linear models and nonparametric approaches will be used to analyze the continuous outcomes. For binary outcomes, chi-square tests and Fisher’s exact test will be used for unadjusted comparisons. For adjusted comparisons, logistic regression analysis will be used to compare with the estimated odds ratio and 95% confidence interval. Unadjusted time-to-event comparisons will be conducted using Kaplan-Meier survival estimates and log-rank tests. For adjusted analyses, Cox proportional hazards regression models will be used to estimate hazard ratios. Sensitivity analyses will be employed to assess the influence of informatively missing values on the results. Subgroup analyses will be conducted based on baseline factors including; MRA use prior to hospitalization, sex, preserved vs. reduced ejection fraction, and age ≥ or <65 years. Interim data analysis for efficacy and futility will not be conducted due to small size and short duration of this trial. The safety analyses will be based on the entire randomized population.
Trial Status
The first patient in ATHENA HF trial was enrolled on December 13, 2014 and the last patient was enrolled in May 2016. Follow up of the patients is ongoing.
CONCLUSION
There remains a need to find novel interventions that effectively and safely promote diuresis and improve outcome in AHF. MRA therapy has shown benefit across the spectrum of chronic HF with reduced ejection fraction and a suggestion of benefit in those with preserved ejection fraction as well in certain regions.43 There are sound theoretical reasons to expect benefit with high dose MRA therapy in AHF as well. If the ATHENA-HF trial shows promising results, it will lay the groundwork for a more definite outcome trial in AHF. This is even more intriguing considering the development of the novel selective MRA, finerenone that has shown benefit in early phase trials in patients with worsening HF and chronic kidney disease,44 as well as the growing literature on the efficacy and safety of chronic use of novel potassium binders to help mitigate the complications related to the use of RAAS inhibitors.
Acknowledgments
Funding Sources: The Heart Failure Clinical Research Network is supported by the NHLBI, National Institutes of Health (U10HL084904 for the coordinating center; and U10HL084861, U10HL084875, U10HL084877, U10HL084889, U10HL084890, U10HL084891, U10HL084899, U10HL084907, and U10HL084931 for the clinical centers). ClinicalTrials.gov Identifier: NCT02235077
URL: http://www.clinicaltrials.gov. Unique identifier: NCT02235077.
Abbreviations
- ACE
Angiotensin converting enzyme
- AHF
Acute heart failure
- ASCEND-HF
Acute Study of Clinical Effectiveness of Nesiritide in Decompensated Heart Failure
- ATHENA-HF
Aldosterone Targeted Neurohormonal Combined with Natriuresis Therapy in Heart Failure
- eGFR
Estimated glomerular filtration rate
- EVEREST
Efficacy of Vasopressin Antagonism in Heart Failure Outcome Study with Tolvaptan
- HF
Heart failure
- MRA
Mineralocorticoid receptor antagonists
- NT-proBNP
N-terminal pro B-type natriuretic peptide
- RELAX-AHF
Efficacy and Safety of Relaxin for the Treatment of Acute Heart Failure
- RAAS
Renin-angiotensin-aldosterone-system
- WHF
Worsening heart failure
Footnotes
Disclosures: None
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Lloyd-Jones D, Adams RJ, Brown TM, Carnethon M, Dai S, De Simone G, Ferguson TB, Ford E, Furie K, Gillespie C, Go A, Greenlund K, Haase N, Hailpern S, Ho PM, Howard V, Kissela B, Kittner S, Lackland D, Lisabeth L, Marelli A, McDermott MM, Meigs J, Mozaffarian D, Mussolino M, Nichol G, Roger VL, Rosamond W, Sacco R, Sorlie P, Roger VL, Thom T, Wasserthiel-Smoller S, Wong ND, Wylie-Rosett J. Heart disease and stroke statistics--2010 update: a report from the American Heart Association. Circulation. 2010;121:e46–e215. doi: 10.1161/CIRCULATIONAHA.109.192667. [DOI] [PubMed] [Google Scholar]
- 2.Lloyd-Jones D, Adams R, Carnethon M, De Simone G, Ferguson TB, Flegal K, Ford E, Furie K, Go A, Greenlund K, Haase N, Hailpern S, Ho M, Howard V, Kissela B, Kittner S, Lackland D, Lisabeth L, Marelli A, McDermott M, Meigs J, Mozaffarian D, Nichol G, O'Donnell C, Roger V, Rosamond W, Sacco R, Sorlie P, Stafford R, Steinberger J, Thom T, Wasserthiel-Smoller S, Wong N, Wylie-Rosett J, Hong Y. Heart disease and stroke statistics--2009 update: a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation. 2009;119:480–6. doi: 10.1161/CIRCULATIONAHA.108.191259. [DOI] [PubMed] [Google Scholar]
- 3.Felker GM, Leimberger JD, Califf RM, Cuffe MS, Massie BM, Adams KF, Jr, Gheorghiade M, O'Connor CM. Risk stratification after hospitalization for decompensated heart failure. Journal of cardiac failure. 2004;10:460–6. doi: 10.1016/j.cardfail.2004.02.011. [DOI] [PubMed] [Google Scholar]
- 4.Massie BM, O'Connor CM, Metra M, Ponikowski P, Teerlink JR, Cotter G, Weatherley BD, Cleland JG, Givertz MM, Voors A, DeLucca P, Mansoor GA, Salerno CM, Bloomfield DM, Dittrich HC. Rolofylline, an adenosine A1-receptor antagonist, in acute heart failure. The New England journal of medicine. 2010;363:1419–28. doi: 10.1056/NEJMoa0912613. [DOI] [PubMed] [Google Scholar]
- 5.Chin MH, Goldman L. Correlates of early hospital readmission or death in patients with congestive heart failure. The American journal of cardiology. 1997;79:1640–4. doi: 10.1016/s0002-9149(97)00214-2. [DOI] [PubMed] [Google Scholar]
- 6.Yamokoski LM, Hasselblad V, Moser DK, Binanay C, Conway GA, Glotzer JM, Hartman KA, Stevenson LW, Leier CV. Prediction of rehospitalization and death in severe heart failure by physicians and nurses of the ESCAPE trial. Journal of cardiac failure. 2007;13:8–13. doi: 10.1016/j.cardfail.2006.10.002. [DOI] [PubMed] [Google Scholar]
- 7.Krumholz HM, Merrill AR, Schone EM, Schreiner GC, Chen J, Bradley EH, Wang Y, Wang Y, Lin Z, Straube BM, Rapp MT, Normand SL, Drye EE. Patterns of hospital performance in acute myocardial infarction and heart failure 30-day mortality and readmission. Circulation Cardiovascular quality and outcomes. 2009;2:407–13. doi: 10.1161/CIRCOUTCOMES.109.883256. [DOI] [PubMed] [Google Scholar]
- 8.Felker GM, Pang PS, Adams KF, Cleland JG, Cotter G, Dickstein K, Filippatos GS, Fonarow GC, Greenberg BH, Hernandez AF, Khan S, Komajda M, Konstam MA, Liu PP, Maggioni AP, Massie BM, McMurray JJ, Mehra M, Metra M, O'Connell J, O'Connor CM, Pina IL, Ponikowski P, Sabbah HN, Teerlink JR, Udelson JE, Yancy CW, Zannad F, Gheorghiade M. Clinical trials of pharmacological therapies in acute heart failure syndromes: lessons learned and directions forward. Circulation Heart failure. 2010;3:314–25. doi: 10.1161/CIRCHEARTFAILURE.109.893222. [DOI] [PubMed] [Google Scholar]
- 9.Vaduganathan M, Greene SJ, Ambrosy AP, Gheorghiade M, Butler J. The disconnect between phase II and phase III trials of drugs for heart failure. Nature reviews Cardiology. 2013;10:85–97. doi: 10.1038/nrcardio.2012.181. [DOI] [PubMed] [Google Scholar]
- 10.Gheorghiade M, Filippatos G. Reassessing treatment of acute heart failure syndromes: the ADHERE Registry. European Heart Journal Supplements. 2005;7:B13–B19. [Google Scholar]
- 11.Gheorghiade M, Vaduganathan M, Fonarow GC, Bonow RO. Rehospitalization for heart failure: problems and perspectives. Journal of the American College of Cardiology. 2013;61:391–403. doi: 10.1016/j.jacc.2012.09.038. [DOI] [PubMed] [Google Scholar]
- 12.Ambrosy AP, Pang PS, Khan S, Konstam MA, Fonarow GC, Traver B, Maggioni AP, Cook T, Swedberg K, Burnett JC, Jr, Grinfeld L, Udelson JE, Zannad F, Gheorghiade M. Clinical course and predictive value of congestion during hospitalization in patients admitted for worsening signs and symptoms of heart failure with reduced ejection fraction: findings from the EVEREST trial. European heart journal. 2013;34:835–43. doi: 10.1093/eurheartj/ehs444. [DOI] [PubMed] [Google Scholar]
- 13.Lala A, McNulty SE, Mentz RJ, Dunlay SM, Vader JM, AbouEzzeddine OF, DeVore AD, Khazanie P, Redfield MM, Goldsmith SR, Bart BA, Anstrom KJ, Felker GM, Hernandez AF, Stevenson LW. Relief and Recurrence of Congestion During and After Hospitalization for Acute Heart Failure: Insights From Diuretic Optimization Strategy Evaluation in Acute Decompensated Heart Failure (DOSE-AHF) and Cardiorenal Rescue Study in Acute Decompensated Heart Failure (CARESS-HF) Circulation Heart failure. 2015;8:741–8. doi: 10.1161/CIRCHEARTFAILURE.114.001957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pimenta J, Paulo C, Mascarenhas J, Gomes A, Azevedo A, Rocha-Goncalves F, Bettencourt P. BNP at discharge in acute heart failure patients: is it all about volemia? A study using impedance cardiography to assess fluid and hemodynamic status. International journal of cardiology. 2010;145:209–14. doi: 10.1016/j.ijcard.2009.08.001. [DOI] [PubMed] [Google Scholar]
- 15.Drazner MH, Hellkamp AS, Leier CV, Shah MR, Miller LW, Russell SD, Young JB, Califf RM, Nohria A. Value of clinician assessment of hemodynamics in advanced heart failure: the ESCAPE trial. Circulation Heart failure. 2008;1:170–7. doi: 10.1161/CIRCHEARTFAILURE.108.769778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Girerd N, Pang PS, Swedberg K, Fought A, Kwasny MJ, Subacius H, Konstam MA, Maggioni A, Gheorghiade M, Zannad F. Serum aldosterone is associated with mortality and re-hospitalization in patients with reduced ejection fraction hospitalized for acute heart failure: analysis from the EVEREST trial. European journal of heart failure. 2013;15:1228–35. doi: 10.1093/eurjhf/hft100. [DOI] [PubMed] [Google Scholar]
- 17.Abdallah JG, Schrier RW, Edelstein C, Jennings SD, Wyse B, Ellison DH. Loop diuretic infusion increases thiazide-sensitive Na(+)/Cl(−)-cotransporter abundance: role of aldosterone. Journal of the American Society of Nephrology : JASN. 2001;12:1335–41. doi: 10.1681/ASN.V1271335. [DOI] [PubMed] [Google Scholar]
- 18.Mentz RJ, Stevens SR, DeVore AD, Lala A, Vader JM, AbouEzzeddine OF, Khazanie P, Redfield MM, Stevenson LW, O'Connor CM, Goldsmith SR, Bart BA, Anstrom KJ, Hernandez AF, Braunwald E, Felker GM. Decongestion strategies and renin-angiotensin-aldosterone system activation in acute heart failure. JACC Heart failure. 2015;3:97–107. doi: 10.1016/j.jchf.2014.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bansal S, Lindenfeld J, Schrier RW. Sodium retention in heart failure and cirrhosis: potential role of natriuretic doses of mineralocorticoid antagonist? Circulation Heart failure. 2009;2:370–6. doi: 10.1161/CIRCHEARTFAILURE.108.821199. [DOI] [PubMed] [Google Scholar]
- 20.RALES Investigators. Effectiveness of spironolactone added to an angiotensin-converting enzyme inhibitor and a loop diuretic for severe chronic congestive heart failure (the Randomized Aldactone Evaluation Study [RALES]) The American journal of cardiology. 1996;78:902–7. doi: 10.1016/s0002-9149(96)00465-1. [DOI] [PubMed] [Google Scholar]
- 21.Hensen J, Abraham WT, Durr JA, Schrier RW. Aldosterone in congestive heart failure: analysis of determinants and role in sodium retention. American journal of nephrology. 1991;11:441–6. doi: 10.1159/000168356. [DOI] [PubMed] [Google Scholar]
- 22.van Vliet AA, Donker AJ, Nauta JJ, Verheugt FW. Spironolactone in congestive heart failure refractory to high-dose loop diuretic and low-dose angiotensin-converting enzyme inhibitor. The American journal of cardiology. 1993;71:21a–28a. doi: 10.1016/0002-9149(93)90241-4. [DOI] [PubMed] [Google Scholar]
- 23.Ferreira JP, Santos M, Almeida S, Marques I, Bettencourt P, Carvalho H. Mineralocorticoid receptor antagonism in acutely decompensated chronic heart failure. European journal of internal medicine. 2014;25:67–72. doi: 10.1016/j.ejim.2013.08.711. [DOI] [PubMed] [Google Scholar]
- 24.Chamsi-Pasha MA, Dupont M, Al Jaroudi WA, Tang WH. Utilization pattern of mineralocorticoid receptor antagonists in contemporary patients hospitalized with acute decompensated heart failure: a single-center experience. Journal of cardiac failure. 2014;20:229–35. doi: 10.1016/j.cardfail.2014.01.017. [DOI] [PubMed] [Google Scholar]
- 25.Seawell MR, Al Darazi F, Farah V, Ramanathan KB, Newman KP, Bhattacharya SK, Weber KT. Mineralocorticoid receptor antagonism confers cardioprotection in heart failure. Current heart failure reports. 2013;10:36–45. doi: 10.1007/s11897-012-0120-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kolkhof P, Borden SA. Molecular pharmacology of the mineralocorticoid receptor: prospects for novel therapeutics. Molecular and cellular endocrinology. 2012;350:310–7. doi: 10.1016/j.mce.2011.06.025. [DOI] [PubMed] [Google Scholar]
- 27.Sica DA. Pharmacokinetics and pharmacodynamics of mineralocorticoid blocking agents and their effects on potassium homeostasis. Heart failure reviews. 2005;10:23–9. doi: 10.1007/s10741-005-2345-1. [DOI] [PubMed] [Google Scholar]
- 28.Shchekochikhin D, Lindenfeld J, Schrier R. Increased Spironolactone in Advanced Heart Failure: Effect of Doses Greater than 25 mg/Day on Plasma Potassium Concentration. Cardiorenal medicine. 2013;3:1–6. doi: 10.1159/000346447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bettencourt P, Azevedo A, Pimenta J, Frioes F, Ferreira S, Ferreira A. N-terminal-pro-brain natriuretic peptide predicts outcome after hospital discharge in heart failure patients. Circulation. 2004;110:2168–74. doi: 10.1161/01.CIR.0000144310.04433.BE. [DOI] [PubMed] [Google Scholar]
- 30.O'Brien RJ, Squire IB, Demme B, Davies JE, Ng LL. Pre-discharge, but not admission, levels of NT-proBNP predict adverse prognosis following acute LVF. European journal of heart failure. 2003;5:499–506. doi: 10.1016/s1388-9842(03)00098-9. [DOI] [PubMed] [Google Scholar]
- 31.Mentz RJ, Hernandez AF, Stebbins A, Ezekowitz JA, Felker GM, Heizer GM, Atar D, Teerlink JR, Califf RM, Massie BM, Hasselblad V, Starling RC, O'Connor CM, Ponikowski P. Predictors of early dyspnoea relief in acute heart failure and the association with 30-day outcomes: findings from ASCEND-HF. European journal of heart failure. 2013;15:456–64. doi: 10.1093/eurjhf/hfs188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Filippatos G, Teerlink JR, Farmakis D, Cotter G, Davison BA, Felker GM, Greenberg BH, Hua T, Ponikowski P, Severin T, Unemori E, Voors AA, Metra M. Serelaxin in acute heart failure patients with preserved left ventricular ejection fraction: results from the RELAX-AHF trial. European heart journal. 2014;35:1041–50. doi: 10.1093/eurheartj/eht497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Packer M, Colucci W, Fisher L, Massie BM, Teerlink JR, Young J, Padley RJ, Thakkar R, Delgado-Herrera L, Salon J, Garratt C, Huang B, Sarapohja T. Effect of levosimendan on the short-term clinical course of patients with acutely decompensated heart failure. JACC Heart failure. 2013;1:103–11. doi: 10.1016/j.jchf.2012.12.004. [DOI] [PubMed] [Google Scholar]
- 34.Konstam MA, Gheorghiade M, Burnett JC, Jr, Grinfeld L, Maggioni AP, Swedberg K, Udelson JE, Zannad F, Cook T, Ouyang J, Zimmer C, Orlandi C. Effects of oral tolvaptan in patients hospitalized for worsening heart failure: the EVEREST Outcome Trial. Jama. 2007;297:1319–31. doi: 10.1001/jama.297.12.1319. [DOI] [PubMed] [Google Scholar]
- 35.Chen J, Normand SL, Wang Y, Krumholz HM. National and regional trends in heart failure hospitalization and mortality rates for Medicare beneficiaries, 1998–2008. Jama. 2011;306:1669–78. doi: 10.1001/jama.2011.1474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M, Das SR, de Ferranti S, Despres JP, Fullerton HJ, Howard VJ, Huffman MD, Isasi CR, Jimenez MC, Judd SE, Kissela BM, Lichtman JH, Lisabeth LD, Liu S, Mackey RH, Magid DJ, McGuire DK, Mohler ER, 3rd, Moy CS, Muntner P, Mussolino ME, Nasir K, Neumar RW, Nichol G, Palaniappan L, Pandey DK, Reeves MJ, Rodriguez CJ, Rosamond W, Sorlie PD, Stein J, Towfighi A, Turan TN, Virani SS, Woo D, Yeh RW, Turner MB. Executive Summary: Heart Disease and Stroke Statistics--2016 Update: A Report From the American Heart Association. Circulation. 2016;133:447–54. doi: 10.1161/CIR.0000000000000366. [DOI] [PubMed] [Google Scholar]
- 37.Butler J, Gheorghiade M, Kelkar A, Fonarow GC, Anker S, Greene SJ, Papadimitriou L, Collins S, Ruschitzka F, Yancy CW, Teerlink JR, Adams K, Cotter G, Ponikowski P, Felker GM, Metra M, Filippatos G. In-hospital worsening heart failure. European journal of heart failure. 2015;17:1104–13. doi: 10.1002/ejhf.333. [DOI] [PubMed] [Google Scholar]
- 38.Weatherley BD, Milo-Cotter O, Felker GM, Uriel N, Kaluski E, Vered Z, O'Connor CM, Adams KF, Cotter G. Early worsening heart failure in patients admitted with acute heart failure--a new outcome measure associated with long-term prognosis? Fundamental & clinical pharmacology. 2009;23:633–9. doi: 10.1111/j.1472-8206.2009.00697.x. [DOI] [PubMed] [Google Scholar]
- 39.Adams KF, Jr, Fonarow GC, Emerman CL, LeJemtel TH, Costanzo MR, Abraham WT, Berkowitz RL, Galvao M, Horton DP. Characteristics and outcomes of patients hospitalized for heart failure in the United States: rationale, design, and preliminary observations from the first 100,000 cases in the Acute Decompensated Heart Failure National Registry (ADHERE) American heart journal. 2005;149:209–16. doi: 10.1016/j.ahj.2004.08.005. [DOI] [PubMed] [Google Scholar]
- 40.Logeart D, Tabet JY, Hittinger L, Thabut G, Jourdain P, Maison P, Tartiere JM, Solal AC. Transient worsening of renal function during hospitalization for acute heart failure alters outcome. International journal of cardiology. 2008;127:228–32. doi: 10.1016/j.ijcard.2007.06.007. [DOI] [PubMed] [Google Scholar]
- 41.Bart BA, Goldsmith SR, Lee KL, Givertz MM, O'Connor CM, Bull DA, Redfield MM, Deswal A, Rouleau JL, LeWinter MM, Ofili EO, Stevenson LW, Semigran MJ, Felker GM, Chen HH, Hernandez AF, Anstrom KJ, McNulty SE, Velazquez EJ, Ibarra JC, Mascette AM, Braunwald E. Ultrafiltration in decompensated heart failure with cardiorenal syndrome. The New England journal of medicine. 2012;367:2296–304. doi: 10.1056/NEJMoa1210357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Schafer JL. Multiple imputation: a primer. Statistical methods in medical research. 1999;8:3–15. doi: 10.1177/096228029900800102. [DOI] [PubMed] [Google Scholar]
- 43.Pfeffer MA, Claggett B, Assmann SF, Boineau R, Anand IS, Clausell N, Desai AS, Diaz R, Fleg JL, Gordeev I, Heitner JF, Lewis EF, O'Meara E, Rouleau JL, Probstfield JL, Shaburishvili T, Shah SJ, Solomon SD, Sweitzer NK, McKinlay SM, Pitt B. Regional variation in patients and outcomes in the Treatment of Preserved Cardiac Function Heart Failure With an Aldosterone Antagonist (TOPCAT) trial. Circulation. 2015;131:34–42. doi: 10.1161/CIRCULATIONAHA.114.013255. [DOI] [PubMed] [Google Scholar]
- 44.Pitt B, Anker SD, Bohm M, Gheorghiade M, Kober L, Krum H, Maggioni AP, Ponikowski P, Voors AA, Zannad F, Nowack C, Kim SY, Pieper A, Kimmeskamp-Kirschbaum N, Filippatos G. Rationale and design of MinerAlocorticoid Receptor antagonist Tolerability Study-Heart Failure (ARTS-HF): a randomized study of finerenone vs. eplerenone in patients who have worsening chronic heart failure with diabetes and/or chronic kidney disease. European journal of heart failure. 2015;17:224–32. doi: 10.1002/ejhf.218. [DOI] [PubMed] [Google Scholar]