Abstract
Background
In the context of the shifting legal landscape of medical marijuana, different methods of cannabis administration have important public health implications. How medical marijuana laws (MML) may influence patterns of use of alternative methods of cannabis administration (vaping and edibles) compared to traditional methods (smoking) is unclear. The purpose of this study was to determine if the prevalence of use of alternative methods of cannabis administration varied in relation to the presence of and variation in MMLs among states in the United States.
Method
Using Qualtrics and Facebook, we collected survey data from a convenience sample of n=2838 individuals who had used cannabis at least once in their lifetime. Using multiple sources, U.S. states were coded by MML status, duration of MML status, and cannabis dispensary density. Adjusted logistic and linear regression analyses were used to analyze outcomes of ever use, preference for, and age of initiation of smoking, vaping, and edibles in relation to MML status, duration of MML status, and cannabis dispensary density.
Results
Individuals in MML states had a significantly higher likelihood of ever use of vaping (OR: 2.04, 99% CI: 1.62-2.58) and edibles (OR: 1.78, 99% CI: 1.39-2.26) than those in states without MMLs. Longer duration of MML status and higher dispensary density were also significantly associated with ever use of vaping and edibles.
Conclusions
MMLs are related to state-level patterns of utilization of alternative methods of cannabis administration. Whether discrepancies in MML legislation are causally related to these findings will require further study. If MMLs do impact methods of use, regulatory bodies considering medical or recreational legalization should be aware of the potential impact this may have on cannabis users.
Keywords: Marijuana use, Medical Marijuana, Dispensaries, Legalization, Vaping, Edibles
1. Introduction
Close to half of states in the United States allow in-state procurement and consumption of cannabis (marijuana) for medical or compassionate purposes (National Conference of State Legislatures, 2015; ProCon.org, 2015b), four states also allow for recreational use, and more states are considering similar legislation (ProCon.org, 2015a, 2015c). Misuse of cannabis can have a variety of negative effects on users (Hall, 2009) and in states where cannabis is medically legal, individuals appear to have a higher likelihood of cannabis use and report lower perceived risk associated with cannabis use (Cerda, Wall, Keyes, Galea, & Hasin, 2012; Wall et al., 2011). Other studies, however, suggest that medical marijuana laws (MML) have little impact on the prevalence of current use status (Choo et al., 2014; Harper, Strumpf, & Kaufman, 2012; Hasin et al., 2015; Lynne-Landsman, Livingston, & Wagenaar, 2013). One important component of medical cannabis legalization that has yet to be explored is the relationship between MMLs and the methods that individuals use to consume cannabis.
There are a variety of ways to consume cannabis (Schauer, King, Bunnell, Promoff, & McAfee, 2016). The three most common methods are inhalation via smoking, inhalation via vaporization (vaping), and ingestion of edible products. The method of administration can impact the onset, intensity, and duration of psychoactive effects, effects on organ systems, and the addictive potential and negative consequences associated with use (Julien, 1995). With smoked cannabis, the psychoactive effects and peak THC blood levels occur in minutes, and the effects last approximately one to four hours (Huestis, Henningfield, & Cone, 1992; Huestis, Sampson, Holicky, Henningfield, & Cone, 1992; Lemberger et al., 1972). Vaping, defined as “using electricity to heat cannabis products so that the cannabis resin is released as a vapor that is inhaled,” (Malouff, Rooke, & Copeland, 2014) has a similar onset, peak, and duration as smoking and produces a similar high (Abrams et al., 2007). Eating cannabis (edibles) produces a different pharmacokinetic profile than smoking or vaping (Aggarwal, Kyashna-Tocha, & Carter, 2007; Carter, Weydt, Kyashna-Tocha, & Abrams, 2004). Onset of the effect is delayed to approximately 30 to 60 minutes (Lemberger et al., 1972), peak blood levels of THC occur approximately three hours later (Lemberger et al., 1972), and the effects can last over six hours (Lemberger et al., 1972).
Method of administration of cannabis can also have differential impact on the user's health. Smoking allows the user to more effectively self-titrate the dose and desired level of intoxication (Carter et al., 2004) but portends inhalation of carcinogenic materials and adverse effects on respiratory health (Aldington et al., 2007; Tetrault et al., 2007; Wu, Tashkin, Djahed, & Rose, 1988). Additionally, enlisting multiple ways of smoking cannabis (e.g., joints, pipes, bongs) is associated with greater probability of problematic use or dependence (Baggio et al., 2014; Chabrol, Roura, & Armitage, 2003). The long-term health consequences of regularly vaping cannabis are not known but vaping may minimize impact on respiratory function compared with smoking cannabis by reducing the inhalation of combustible smoke and its carcinogenic constituents (Abrams et al., 2007; Gieringer, 2001; Hazekamp, Ruhaak, Zuurman, van Gerven, & Verpoorte, 2006; Pomahacova, Van der Kooy, & Verpoorte, 2009; Van Dam & Earleywine, 2010). People may prefer vaping instead of smoking as their primary method of administration as it is reported to be a better tasting, more efficient, and cost effective way to obtain the desired euphoric effect (Budney, Sargent, & Lee, 2015; Malouff et al., 2014). These “positive” aspects of vaping and the perception of reduced respiratory system harm could conceivably lead to more frequent consumption or earlier initiation of cannabis, and a concomitant increased risk of developing problematic use or addiction (Budney et al., 2015). Edibles also allow the user to avoid inhaling smoke; however, it is harder to titrate the intoxicating effects due to the delayed and variable onset of effects. Consequently edibles have recently been tied to cannabis “overdose” following ingestion of additional doses because of the misperception that the initial dose had not produced the desired effect (Ghosh et al., 2015; MacCoun & Mello, 2015). Availability of edibles has also been associated with increased rates of accidental pediatric ingestion of cannabis and associated adverse effects (Ghosh et al., 2015; Wang, Roosevelt, & Heard, 2013; Wang et al., 2014).
The regulation of medical marijuana across the United States is marked by extreme legislative and regulatory heterogeneity. Medical marijuana laws enacted to address the dispensation and consumption of marijuana for medical purposes have been in place for over a decade in some states and only a few years in others (ProCon.org, 2015b). Additionally, some MML states, but not all, have developed state regulated cannabis dispensary systems (i.e., stores or “pharmacies”) that provide access to novel cannabis products such as vaporizers and edibles. Dispensaries have been linked with availability of higher potency (% THC) cannabis (Ghosh et al., 2015; Sevigny, Pacula, & Heaton, 2014) increased cannabis related hospitalizations (Mair, Freisthler, Ponicki, & Gaidus, 2015), and the sale of cannabis products with highly inaccurate labeling of the active ingredients in cannabis (e.g., %THC and cannabidiol) (Vandrey et al., 2015). Among the MML states that allow for dispensaries, the number of dispensaries varies greatly, with hundreds of dispensaries permitted in some states to only a handful permitted in others (Colorado Department of Revenue Enforcement Division, 2015; State of New Jersey Department of Health). Consequently, states that have had an MML in place for longer periods of time do not necessarily have more dispensaries.
Legalization of cannabis use and the sale of cannabis most likely prompt increased development, production, and marketing of desirable cannabis products and delivery systems to increase sales and meet consumer demand (Colorado Department of Revenue Enforcement Division, 2015; Ghosh et al., 2015). The goal of the present study was to explore how the existence of MMLs and differing MML dispensary policies are related to three methods of cannabis administration – smoking, vaping, and edibles. Specifically, we examined three aspects of legalization status across states, (1) MML status (yes or no); (2) the duration of time a state has had an MML in place; and (3) the density of cannabis dispensaries within each state. Primary hypotheses were that having an MML, increased duration of MML status, and higher density of dispensaries would be associated with increased likelihood of ever use, preference for, and younger age of initiation of the less common methods of cannabis administration (i.e., vaping and edibles).
2. Methods
2.1. Survey and Recruitment
The Dartmouth Committee for the Protection of Human Subjects approved the study. A survey was administered using Facebook paid advertising mechanisms to target and recruit a self-selected convenience sample of cannabis users. Advertisements for the survey were shown to a targeted audience of cannabis users through the use of proprietary marketing algorithms that utilize Facebook users' self-reported interests. Examples of marijuana-related interests included association with organizations such as NORML or High Times Magazine. Facebook delivered an advertisement to the screens of these individuals when they logged into their account. Clicking on the advertisement led to the informed consent page. The informed consent page explained the purpose of the survey and included language stating that IP addresses and other identifying information would not be collected or linked to responses (Qualtrics default IP address logging features were disabled for this study). Respondents who provided consent were re-directed to the survey hosted through the Qualtrics online survey platform. Multiple responses for a given participant were prevented with a Qualtrics feature that uses cookies instead of IP addresses to block participants from taking the survey more than once and preserves anonymity. The survey first screened for cannabis use and excluded those who had never used. A data quality-check question, “Please click 4 for this question”, ensured that responses came from people and not internet bots and that respondents were attending to the questions. Respondents were not compensated.
The survey was conducted in two phases; a 63 item and then 72 item version of the survey was administered over a 35 day period in October and November, 2014, and an 8 day period in February, 2015, respectively. Questions added in the second survey were aimed at collecting additional data on demographics, patterns of vaping and other substance use. Only questions that were included in both phases were used in these analyses. Survey completion rates did not differ by survey phase (83% vs 80% in phases one and two respectively). Survey items assessed sociodemographics (e.g. age, gender, race, education), current and past cannabis use history and patterns (e.g. lifetime use status, age of initiation, and frequency of use, for each method of administration) and information on reasons and preferences for methods of cannabis use and lifetime use of other substances (Lee, Crosier, Borodovsky, Sargent, & Budney, 2015).
2.3. Classification: MML State, Duration, and Dispensary Density
Respondents were classified as either living in an MML state or a non-MML state using their self-reported state residence. The twenty-four states that permit in-state procurement and consumption of cannabis plant material or psychoactive THC extracts for medical purposes were designated as a current MML state based on legislation that had been enacted as of October 2014 (Law Atlas The Policy Surveillance Portal, 2014; Marijuana Policy Project, 2014; National Conference of State Legislatures, 2015; ProCon.org, 2014, 2015b). MML states were then classified by the duration of time their MML had been in place using three categories: (1) 0 to 5 years (n=11 states), (2) 6 to 10 years (n=3 states), and (3) >10 years (n=10 states). The approximate number of dispensaries per state was obtained using various sources: contacting state representatives of medical marijuana programs, annual state medical marijuana reports, and department of health or state medical marijuana program websites. The number of dispensaries per 100,000 people in each state was estimated using the 2014 US census population estimates (United States Census Bureau), and categorized as follows: (1) MML but no dispensaries (n=13 states), (2) <1 dispensary per 100,000 people (n=5 states) or (3) ≥1 dispensary per 100,000 people (n=6 states).
2.4. Analysis
Initial univariate point estimate analyses using chi squared, t-tests and ANOVAs were performed to examine relationships between the three MML feature variables (MML status, duration of MML status, and density of dispensaries) and the three methods of administration variables (ever use, preference for, and age of initiation of smoking, vaping, and edible cannabis). The outcomes of preference and age of initiation were analyzed only among the subset of respondents who had ever used the method of administration of interest. An alpha of 0.01 was used in all analyses to account for performing multiple tests and the large sample size.
These same relationships were assessed with multivariable logistic and linear regression to control for potential confounders (age, gender, race, education, lifetime days of cannabis use, and age of onset of cannabis use). In each analysis, non-MML states were the reference group when analyzing the effects of duration of MML and dispensary density using dummy variables. To test for trends within MML states only, similar adjusted logistic regressions were performed with an ordinal categorical variable for either duration of MML status or dispensary density. When significant odds ratios were observed for these variables, a second adjusted logistic regression with a dummy coded version of that variable was conducted to clarify any significant differences across duration of MML or density of dispensary categories. In these analyses the referent group was either MML duration of 0-5 years or MML state with no dispensaries. All analyses were conducted using Stata (version 14 StatCorp, College Station, TX).
2.4.1. Missing Data
Only the age variable had a substantial proportion of missing responses (n=659, see Table 1). Chi squared analyses and t-tests comparing those who reported their age vs. those who did not on the primary ever use, preference, and age of initiation outcomes were not significant. (p=0.15 to 0.93). We used a multiple imputation model carried out to 50 iterations to conduct the adjusted logistic and linear regressions. Primary independent variables (MML status, duration of legalization, and dispensary prevalence) and dependent variables (ever use of smoking, vaping, and edibles) were used to impute missing data. Complete case analyses were performed as a sensitivity check, and yielded similar findings as those from the multiple imputation analyses.
Table 1. Participant Characteristics by MML State Status (n=2838).
| MML State Status | ||
|---|---|---|
| Non-MML States (n=1,384) | MML States (n=1,454) | |
| Age, m (SD)* | 34.1 (16.0) | 30.9 (14.8) |
| missing, n | 332 | 327 |
|
| ||
| Gender | ||
| Male, n (%) | 1183 (85.9) | 1208 (83.5) |
| Female, n (%) | 195 (14.2) | 239 (16.5) |
| missing, n | 6 | 7 |
|
| ||
| Race and Ethnicity* | ||
| Caucasian, n (%) | 1056 (77.7) | 992 (71.2) |
| African American, n (%) | 112 (8.2) | 95 (6.8) |
| Hispanic, n (%) | 152 (11.2) | 249 (17.9) |
| Other, n (%) | 39 (2.9) | 57 (4.1) |
| missing, n | 25 | 61 |
|
| ||
| Level of Education* | ||
| High school or less, n (%) | 736 (53.3) | 769 (52.9) |
| Some college, n (%) | 478 (34.6) | 447 (30.7) |
| College or higher, n (%) | 168 (12.2) | 238 (16.4) |
| missing, n | 2 | 0 |
|
| ||
| Lifetime days cannabis use | ||
| ≤99, n (%) | 129 (9.3) | 182 (12.5) |
| 100-999, n (%) | 395 (28.6) | 397 (27.3) |
| >999, n (%) | 858 (62.1) | 873 (60.1) |
| missing, n | 2 | 2 |
|
| ||
| Age first use cannabis, m (SD) | 15.8 (4.2) | 15.6 (4.6) |
| missing, n | 14 | 11 |
Analysis was significant (p<0.01)
Chi squared tests used to calculate p values for categorical variables, T-Tests used to calculate p value for continuous variables
3. Results
3.1. Description of the Sample
Advertisements were shown to 168,894 people out of whom 3,708 (2.2%) clicked the link, and of which 2,838 (1.7%) passed the data-quality check question, completed the survey, reported use of cannabis in their lifetime and reported the state in which they lived. Table 1 displays detailed characteristics of the sample. The mean age was 32.5 years (SD=15.5), 84.5% were male, and the race/ethnicity distribution was 74.4% Caucasian, 14.6% Hispanic or Latino, 7.5% Black and 3.5% other. Approximately 14.5% reported having at least a college degree.
A comparison with 2014 United States census data indicated that the proportion of survey respondents from each state corresponded closely to the population proportion across US states (Pearson's r = 0.94, p<0.0001) suggesting that states with more liberal marijuana laws were not over represented in this convenience sample. Using the public dataset from the 2013 National Survey on Drug Use and Health (United States Department of, Human Services. Substance, Mental Health Services Administration. Center for Behavioral Health, & Quality, 2015), we compared the final sample to a nationally representative sample of individuals who used cannabis in the past month. Cannabis users in the current study were more likely to be daily cannabis users and have an earlier age of onset of cannabis use.
3.2. Univariate Analyses
Findings from the univariate analyses are detailed in Table 2.
Table 2. Point Estimates and Univariate Tests of Method of Administration Among MML Features (MML Status / Duration of MML / Dispensary Density).
| Ever Used Method | Preferred Method† | |||||
|---|---|---|---|---|---|---|
| Smoke | Vape* | Edible* | Smoke* | Vape | Edible | |
| MML Status | ||||||
| No | 99.7% | 53.8% | 68.0% | 84.3% | 19.1% | 8.1% |
| Yes | 99.5% | 68.6% | 77.6% | 78.9% | 21.7% | 9.25% |
|
| ||||||
| Duration of MML | ||||||
| No MML | 99.7% | 53.8% | 68.0% | 84.3% | 19.1% | 8.1% |
| 0-5 years | 99.5% | 66.7% | 71.5% | 78.8% | 23.9% | 9.5% |
| 6-10 years | 100% | 62.9% | 82.3% | 84.6% | 17.3% | 5.6% |
| > 10 years | 99.4% | 72.9% | 86.1% | 77.7% | 19.5% | 9.8% |
|
| ||||||
| Dispensary (per 100k people) | ||||||
| No MML | 99.7% | 53.8% | 68.0% | 84.3% | 19.1% | 8.1% |
| 0 | 99.5% | 66.4% | 73.2% | 80.9% | 21.9% | 7.9% |
| < 1 | 100% | 68.1% | 77.3% | 75.7% | 23.9% | 13.8% |
| ≥ 1 | 99.4% | 72.3% | 84.9% | 76.5% | 21.0% | 10.0% |
Chi squared tests used to calculate p-values
All three comparisons (MML Status, Duration MML, and Dispensary) for that method were significant (p<0.01)
Among those who had ever used that method of administration
3.2.1. Ever Use of Method
The prevalence of ever use of cannabis via vaping or edibles was significantly higher among respondents in MML states compared to respondents in non-MML states (χ2=65.0, p<0.001; χ2=33.00, p<0.001, respectively). Significant differences in ever use of vaping and edibles were observed across the four duration categories of MML status (χ2=72.0, p<0.001; χ2 =68.6, p<0.001, respectively), and across the density of dispensaries categories (χ2=69.5, p<0.001; χ2=54.3, p<0.001 respectively), with the percentage of ever use increasing incrementally with higher density of dispensaries.
3.2.2. Preferences for Method
A higher proportion of respondents from non-MML states preferred smoking (χ2=13.6, p<0.001). Significant variation was observed across durations of MML status and dispensary density categories in preference for smoking (χ2=16.8, p=0.001; χ2=18.7, p<0.001 respectively) but not for vaping, and edibles. The percentage who preferred smoking decreased with higher density of dispensaries.
3.2.3. Age of Initiation
No significant differences in age of onset of smoking, vaping, or edibles were observed between respondents from MML and non-MML states, across durations of MML status, or across dispensary density categories.
3.3. Multivariable Logistic Regression Analyses
3.3.1. Ever Use of a Method of Administration
Table 3 presents odds ratios (OR) and 99% confidence intervals from the imputed logistic regression analyses of likelihood of ever use of methods of administration controlling for age, gender, education, race, age of cannabis use onset, and total days of lifetime cannabis use. Similar to univariate findings, the likelihood of ever using cannabis via vaping and edibles was significantly higher among respondents from MML states compared to non-MML states. This finding held when separate comparisons of respondents from each MML duration category (0-5 years, 6-10 years, and >10 years) were made to respondents from non-MML states (Table 3). Ever use among respondents from the three duration categories (MML states only) was significant for vaping and edibles (OR: 1.21, 99% CI: 1.01-1.45, p=0.007; OR: 1.70, 99% CI: 1.38-2.10, p<0.001 respectively). Respondents from states with a longer duration (>10 years) had a significantly higher likelihood of ever use of vaping than those from states with a shorter duration (0-5 years) (OR: 1.48, 99% CI: 1.03-2.14, p=0.005). Respondents from states with moderate (6-10 years) and longer duration had significantly higher likelihoods of ever use of edibles than respondents from states with shorter duration (OR: 2.00, 99% CI: 1.00-3.98, p<0.01; OR: 2.86, 99% CI: 1.87-4.36, p<0.001 respectively).
Table 3. Ever Use of Alternate Method - Adjusted Logistic Regression Results.
|
Vape (model n=2838) |
Edible ((model n=2838) |
|
|---|---|---|
| OR (99% CI) | OR (99% CI) | |
| MML Status | ||
| No | ref | ref |
| Yes | 2.04 (1.62, 2.58) | 1.78 (1.39, 2.26) |
|
| ||
| Duration of MML | ||
| No MML | ref | ref |
| 0-5 years | 1.82 (1.38, 2.39) | 1.23 (0.93, 1.62) |
| 6-10 years | 1.51 (0.86, 2.66) | 2.50 (1.28, 4.89) |
| >10 years | 2.68 (1.92, 3.75) | 3.43 (2.32, 5.08) |
|
| ||
| Dispensary (per 100k people) | ||
| No MML | ref | ref |
| 0 | 1.79 (1.36, 2.34) | 1.34 (1.02, 1.76) |
| < 1 | 2.11 (1.22, 3.68) | 1.83 (1.01, 3.29) |
| ≥ 1 | 2.57 (1.82, 3.62) | 3.21 (2.16, 4.76) |
Results are from multiple imputation analysis
Adjusted for age, gender, education, race, age of onset of cannabis use, lifetime days of cannabis use
OR = “Odds Ratio” & CI = “Confidence Interval”
OR that are bold indicate p<0.01
Parallel analyses among dispensary density categories revealed that respondents from MML states without dispensaries, with lower dispensary density, and with higher dispensary density, each had significantly higher likelihoods of ever using vaping and edibles than non-MML states (Table 3). Ever use also significantly differed among the three dispensary density categories (MML states only) for vaping and edibles (OR: 1.22, 99% CI: 1.01-1.46, p=0.007; OR: 1.56, 99% CI: 1.27-1.93, p<0.001, respectively). Compared to respondents from MML states with no dispensaries, respondents from MML states with the highest dispensary density (≥1 per 100,000) had a significantly greater likelihood of ever use of vaping and edibles (OR: 1.48, 99% CI: 1.02-2.15, p=0.007; OR: 2.48, 99% CI: 1.61-3.80, p<0.001 respectively).
3.3.2. Preferences for Method of Administration
Also similar to results from the univariate analysis, persons living in MML states were less likely to prefer smoking (OR: 0.71, 99% CI: 0.55-0.92, p<0.001). There were no differences in preference for vaping or edibles between those living in MML states and those living in non-MML states. Respondents from MML states in the shortest and the longest MML duration categories had a significantly lower likelihood of preferring smoking (OR: 0.70, 99% CI: 0.52-0.94, p=0.002; OR: 0.66, 99% CI: 0.47-0.93, p=0.002 respectively). Respondents from states with higher density of dispensaries had a significantly lower likelihood of preferring smoking compared to respondents from non-MML states (OR: 0.62, 99% CI: 0.44-0.88, p<0.001).
3.3.3. Age of Initiation of Method of Administration
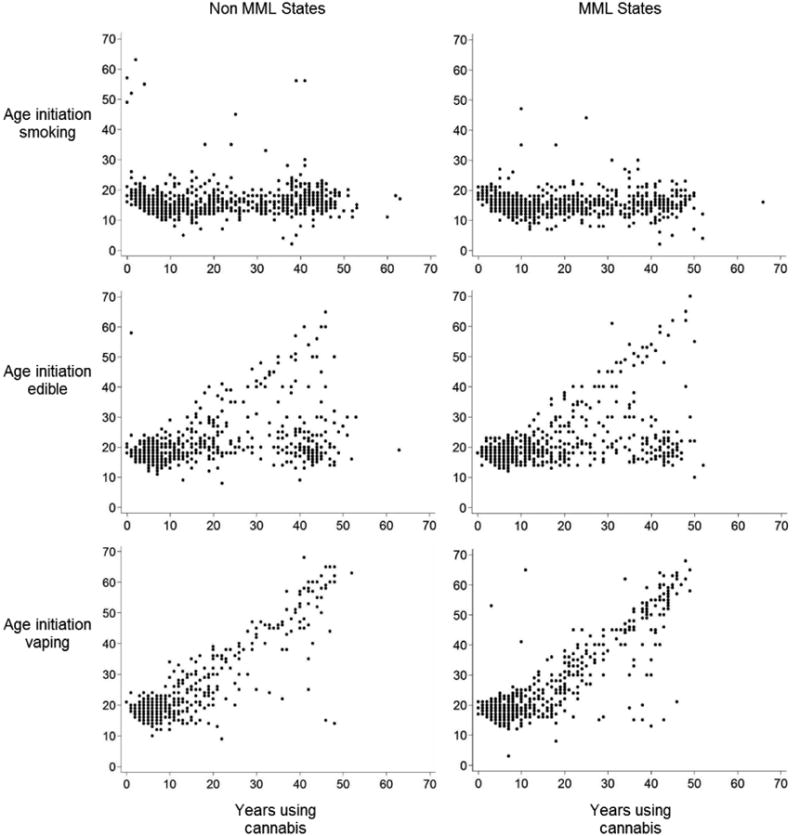
Among those who had ever used each of the three different methods of administration, no differences in age of onset of each method were observed in relation to MML status, duration, or dispensary density. Subsequent exploratory linear regression analyses demonstrated that regardless of MML status, the age of onset of vaping and edible use was positively related to duration of any cannabis use (longer duration of use, later onset of vaping and edibles; shorter duration of vaping and edible use, earlier onset of use of these methods) (β=0.83, 99% CI: 0.80-0.87, p<0.001; β=0.26, 99% CI: 0.23-0.30, p<0.001 respectively) (Figure 1).
Figure 1. Relationships between Age of Onset of Methods of Administration and Years of Cannabis Use across MML Status.
3.3.4. Impact of Recreational Marijuana Laws
To determine if recreational marijuana laws affected our findings, we conducted multiple sensitivity analyses. Imputed multiple logistic regressions simultaneously adjusting for recreational law status (yes/no), MML status (yes/no), and dispensary status (yes/no) (in addition to age, gender, race, education, lifetime days of cannabis use, and age of onset of cannabis use) were used to predict ever use of vaping and ever use of edibles. In the vaping model, MML status was a significant predictor (OR: 1.77, 99% CI: 1.35-2.33, p<0.001), but neither recreational legalization status nor dispensary status were significant predictors (OR: 1.65, 99% CI: 0.95-2.87, p=0.02; OR: 1.17, 99% CI: 0.81-1.71, p=0.27 respectively). In the edible model both MML status and dispensary status were significant predictors (OR: 1.33, 99% CI: 1.01-1.76, p=0.007; OR: 1.88, 99% CI: 1.25-2.84, p<0.001) while recreational legalization status was not (OR: 1.39, 99% CI: 0.74-2.62, p=0.18). These results indicate that MML status is a robust and significant predictor of ever use of alternative methods of administration even after the effect of recreationally legal states has been accounted for.
4. Discussion
Findings from this convenience sample of cannabis users support the hypotheses that vaping and use of edible marijuana appear more prevalent in states with MMLs, in states that have had MMLs in place for a longer time, and in MML states with a higher per capita density of cannabis dispensaries. If future investigations find these relationships to be causal, that is, MMLs do change how cannabis is used, then legislators and policy makers in the United States and other countries should be aware of the potential impact, pro or con, of alternative methods of cannabis consumption on public health.
The positive relationship between the duration an MML is in place and ever use of vaping or edibles suggests that implementation of MMLs is closely related to increased use of alternate methods. However the parallel observation that the existence and density of cannabis dispensaries were positively related to ever use of both vaping and edibles suggests that it may not be the mere presence of an MML, but other components of MML implementation (e.g., dispensary regulations) that influence methods and patterns of cannabis use. Discrepancies in regulatory policy related to dispensaries (e.g. quotas) may have important implications in this regard (Pacula, Powell, Heaton, & Sevigny, 2015). The popularity and utilization of less traditional methods of cannabis administration such as edibles and vaping, is likely to be a function of the availability and marketing of such products. A prior report indicated that dispensaries package and sell a variety of attractive and high potency edible cannabis products not readily available elsewhere (MacCoun & Mello, 2015), likely contributing to the greater prevalence of use of edibles. The proliferation of dispensaries that sell vaping products or the emergence of independent vaping shops may also contribute to the association between MML status and use of vaping methods, but to our knowledge, no data on the prevalence of vaping retail stores are available.
The somewhat counterintuitive observation that individuals in MML states are less likely to prefer smoking cannabis but not more likely to prefer vaping or edible use warrants note. The greater prevalence of vaping or edible use in MML states was associated with fewer participants in those states indicating they preferred smoking (because more preferred vaping or eating). Our comparative analyses of preference for vaping or edibles, however, only included those who ever vaped or used edibles, and here no differences were observed between MML and non-MML states. These observations suggest that the impact of MML status on preference likely relates to increased exposure to the method of use, that is, once people have tried varying methods, preference rates appear stable regardless of residence in an MML state or not.
The observation that cannabis users in MML states were more likely to have tried an alternative method of administration but not necessarily at a younger age merits comment. The positive relationship between years of cannabis use and the age of initiation of alternative methods regardless of MML status (Figure 1) suggests that alternative methods (vaping in particular) have become increasingly popular methods of administration in recent years (Budney et al., 2015), and thus both newer and more experienced cannabis users have both only recently initiated vaping.
Although recreational legalization status was not a significant predictor of increased use of alternative methods in our sensitivity analyses, the odds ratios associated with it were similar in size to the MML association. This finding warrants consideration as recreational legalization becomes more widely deliberated.
A number of important limitations of the present study warrant consideration and caution when interpreting our findings. Individuals who participated in this non-compensated Facebook survey reflect a convenience sample with associated potential selection biases and may differ from the general population of cannabis users. Indeed, as indicated above, this sample comprised a larger percentage of daily users than observed in a recent nationally representative sample of cannabis users. A recent study on the prevalence in the United States of various methods of administration of cannabis reported that smoking is the most commonly used method of administration (similar to our observed results), however, its reported prevalence of use of vaporization and edibles was lower than observed in our sample (Schauer et al., 2016). This may be due to differences in sampling strategies as Schauer et al. used a probability based sampling method. If vape and edible users in MML states were more likely to respond to the survey, this selection bias could account for at least some of the observed differences associated with MMLs.
The decisions on how to categorize MML duration and dispensary density were arbitrary, other strategies could yield different results. Also, dispensary density classification was limited by (a) an unknown number of dispensaries operating within each state that are not sanctioned or counted in state reports and (b) analyses did not account for potential clustering of dispensaries in large urban areas. While vaping and edible use appears to be strongly associated with MML status, it is important to note that these data reflect reports of lifetime, or ever use, so these results may include participants that vaped or used edibles prior to enactment of MMLs in their respective states. Future studies that collect longitudinal data before and after medical legalization are needed to more fully understand the relationship between MMLs and methods of cannabis use.
Continued vigilance and data collection concerning how individuals are using cannabis is essential in order to detect shifts in patterns of use both before and after the implementation of MMLs. Legalization may prompt a rapid escalation in marketing of cannabis products and devices to administer cannabis. The speed of this escalation may depend on legislative rules and regulations such as placing quotas on dispensaries. Moving forward, cannabis users will likely be administering cannabis in different ways and using different cannabis products than in the past. An important strength of this study and its methods (Facebook sampling) is that repeated and perhaps highly generalizable observations can be acquired relatively quickly and at low cost. As such, this methodology may be used to systematically monitor the rapidly changing patterns of cannabis use and methods of use pre and post legalization as these changes are likely to have important public health implications.
Acknowledgments
Funding: NIH 5T32DA037202-02 & 5R01DA032243-04
The funding sources had no involvement in the study design; collection, analysis and interpretation of data; writing of the report; or in the decision to submit the article for publication.
Footnotes
Portions of this work were previously presented at the College on Problems for Drug dependence conference in Phoenix Arizona, June 2015.
Conflict of interest: All authors have no conflicts of interest to report.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Abrams DI, Vizoso HP, Shade SB, Jay C, Kelly ME, Benowitz NL. Vaporization as a smokeless cannabis delivery system: a pilot study. Clin Pharmacol Ther. 2007;82(5):572–578. doi: 10.1038/sj.clpt.6100200. [DOI] [PubMed] [Google Scholar]
- Aggarwal SK, Kyashna-Tocha M, Carter GT. Dosing medical marijuana: rational guidelines on trial in Washington State. MedGenMed. 2007;9(3):52. [PMC free article] [PubMed] [Google Scholar]
- Aldington S, Williams M, Nowitz M, Weatherall M, Pritchard A, McNaughton A, et al. Beasley R. Effects of cannabis on pulmonary structure, function and symptoms. Thorax. 2007;62(12):1058–1063. doi: 10.1136/thx.2006.077081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baggio S, Deline S, Studer J, Mohler-Kuo M, Daeppen JB, Gmel G. Routes of administration of cannabis used for nonmedical purposes and associations with patterns of drug use. J Adolesc Health. 2014;54(2):235–240. doi: 10.1016/j.jadohealth.2013.08.013. [DOI] [PubMed] [Google Scholar]
- Budney AJ, Sargent JD, Lee DC. Vaping cannabis (marijuana): parallel concerns to e-cigs? Addiction. 2015;110(11):1699–1704. doi: 10.1111/add.13036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carter GT, Weydt P, Kyashna-Tocha M, Abrams DI. Medicinal cannabis: rational guidelines for dosing. IDrugs. 2004;7(5):464–470. [PubMed] [Google Scholar]
- Cerda M, Wall M, Keyes KM, Galea S, Hasin D. Medical marijuana laws in 50 states: investigating the relationship between state legalization of medical marijuana and marijuana use, abuse and dependence. Drug Alcohol Depend. 2012;120(1-3):22–27. doi: 10.1016/j.drugalcdep.2011.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chabrol H, Roura C, Armitage J. Bongs, a method of using cannabis linked to dependence. Can J Psychiatry. 2003;48(10):709. doi: 10.1177/070674370304801011. [DOI] [PubMed] [Google Scholar]
- Choo EK, Benz M, Zaller N, Warren O, Rising KL, McConnell KJ. The impact of state medical marijuana legislation on adolescent marijuana use. J Adolesc Health. 2014;55(2):160–166. doi: 10.1016/j.jadohealth.2014.02.018. [DOI] [PubMed] [Google Scholar]
- Colorado Department of Revenue Enforcement Division. Marijuana, Annual Update (2014) 2015 [Google Scholar]
- Ghosh TS, Van Dyke M, Maffey A, Whitley E, Erpelding D, Wolk L. Medical marijuana's public health lessons--implications for retail marijuana in Colorado. N Engl J Med. 2015;372(11):991–993. doi: 10.1056/NEJMp1500043. [DOI] [PubMed] [Google Scholar]
- Gieringer DH. Cannabis “Vaporization” A Promising Strategy for Smoke Harm Reduction. Journal of Cannabis Therapeutics. 2001;1(3-4):153–170. [Google Scholar]
- Hall W. The adverse health effects of cannabis use: What are they, and what are their implications for policy? International Journal of Drug Policy. 2009;20(6):458–466. doi: 10.1016/j.drugpo.2009.02.013. [DOI] [PubMed] [Google Scholar]
- Harper S, Strumpf EC, Kaufman JS. Do medical marijuana laws increase marijuana use? Replication study and extension. Ann Epidemiol. 2012;22(3):207–212. doi: 10.1016/j.annepidem.2011.12.002. [DOI] [PubMed] [Google Scholar]
- Hasin DS, Wall M, Keyes KM, Cerda M, Schulenberg J, O'Malley PM, et al. Feng TS. Medical marijuana laws and adolescent marijuana use in the USA from 1991 to 2014: results from annual, repeated cross-sectional surveys. Lancet Psychiatry. 2015;2(7):601–608. doi: 10.1016/S2215-0366(15)00217-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hazekamp A, Ruhaak R, Zuurman L, van Gerven J, Verpoorte R. Evaluation of a vaporizing device (Volcano) for the pulmonary administration of tetrahydrocannabinol. J Pharm Sci. 2006;95(6):1308–1317. doi: 10.1002/jps.20574. [DOI] [PubMed] [Google Scholar]
- Huestis MA, Henningfield JE, Cone EJ. Blood cannabinoids. I. Absorption of THC and formation of 11-OH-THC and THCCOOH during and after smoking marijuana. J Anal Toxicol. 1992;16(5):276–282. doi: 10.1093/jat/16.5.276. [DOI] [PubMed] [Google Scholar]
- Huestis MA, Sampson AH, Holicky BJ, Henningfield JE, Cone EJ. Characterization of the absorption phase of marijuana smoking. Clin Pharmacol Ther. 1992;52(1):31–41. doi: 10.1038/clpt.1992.100. [DOI] [PubMed] [Google Scholar]
- Julien RM. A primer of drug action: A concise, nontechnical guide to the actions, uses, and side effects of psychoactive drugs. WH Freeman/Times Books/Henry Holt & Co; 1995. [Google Scholar]
- Law Atlas The Policy Surveillance Portal. Medical Marijuana Laws for Patients Map. 2014 Retrieved 10/2/14, from http://lawatlas.org/query?dataset=medical-marijuana-patient-related-laws.
- Lee DC, Crosier BS, Borodovsky JT, Sargent JD, Budney AJ. Online survey characterizing vaporizer use among cannabis users. Drug and Alcohol Dependence. 2015 doi: 10.1016/j.drugalcdep.2015.12.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lemberger L, Weiss JL, Watanabe AM, Galanter IM, Wyatt RJ, Cardon PV. Delta-9-tetrahydrocannabinol: temporal correlation of the psychologic effects and blood levels after various routes of administration. New England Journal of Medicine. 1972;286(13):685–688. doi: 10.1056/NEJM197203302861303. [DOI] [PubMed] [Google Scholar]
- Lynne-Landsman SD, Livingston MD, Wagenaar AC. Effects of state medical marijuana laws on adolescent marijuana use. Am J Public Health. 2013;103(8):1500–1506. doi: 10.2105/AJPH.2012.301117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacCoun RJ, Mello MM. Half-baked--the retail promotion of marijuana edibles. N Engl J Med. 2015;372(11):989–991. doi: 10.1056/NEJMp1416014. [DOI] [PubMed] [Google Scholar]
- Mair C, Freisthler B, Ponicki WR, Gaidus A. The impacts of marijuana dispensary density and neighborhood ecology on marijuana abuse and dependence. Drug Alcohol Depend. 2015;154:111–116. doi: 10.1016/j.drugalcdep.2015.06.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Malouff JM, Rooke SE, Copeland J. Experiences of marijuana-vaporizer users. Subst Abus. 2014;35(2):127–128. doi: 10.1080/08897077.2013.823902. [DOI] [PubMed] [Google Scholar]
- Marijuana Policy Project. State-By-State Medical Marijuana Laws. 2014 Retrieved 10/14/14, from https://www.mpp.org/issues/medical-marijuana/state-by-state-medical-marijuana-laws/
- National Conference of State Legislatures. State Medical Marijuana Laws. 2015 Retrieved 3/27/15, from http://www.ncsl.org/research/health/state-medical-marijuana-laws.aspx.
- Pacula RL, Powell D, Heaton P, Sevigny EL. Assessing the effects of medical marijuana laws on marijuana use: the devil is in the details. J Policy Anal Manage. 2015;34(1):7–31. doi: 10.1002/pam.21804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pomahacova B, Van der Kooy F, Verpoorte R. Cannabis smoke condensate III: the cannabinoid content of vaporised Cannabis sativa. Inhal Toxicol. 2009;21(13):1108–1112. doi: 10.3109/08958370902748559. [DOI] [PubMed] [Google Scholar]
- ProCon.org. 23 Legal Medical Marijuana States and DC. 2014 Retrieved 10/7/15, from Retrieved from http://medicalmarijuana.procon.org/view.resource.php?resourceID=000881.
- ProCon.org. 9 States with Pending Legislation to Legalize Medical Marijuana. 2015a Retrieved 3/25/15, from Retrieved from http://medicalmarijuana.procon.org/view.resource.php?resourceID=000881.
- ProCon.org. 2015b 23 Legal Medical Marijuana States and DC. from Retrieved from http://medicalmarijuana.procon.org/view.resource.php?resourceID=000881.
- ProCon.org. Two States Considering the Legalization of Medical Marijuana. 2015c Retrieved 12/28/15, from Retrieved from http://medicalmarijuana.procon.org/view.resource.php?resourceID=002481.
- Schauer GL, King BA, Bunnell RE, Promoff G, McAfee TA. Toking, Vaping, and Eating for Health or Fun: Marijuana Use Patterns in Adults, U.S., 2014. Am J Prev Med. 2016;50(1):1–8. doi: 10.1016/j.amepre.2015.05.027. [DOI] [PubMed] [Google Scholar]
- Sevigny EL, Pacula RL, Heaton P. The effects of medical marijuana laws on potency. Int J Drug Policy. 2014;25(2):308–319. doi: 10.1016/j.drugpo.2014.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- State of New Jersey Department of Health. Medicinal Marijuana Program ATC FAQ's. Retrieved 10/7/14, from http://www.nj.gov/health/medicalmarijuana/atc_faqs.shtml.
- Tetrault JM, Crothers K, Moore BA, Mehra R, Concato J, Fiellin DA. Effects of marijuana smoking on pulmonary function and respiratory complications: a systematic review. Arch Intern Med. 2007;167(3):221–228. doi: 10.1001/archinte.167.3.221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- United States Census Bureau. Annual Estimates of the Resident Population for the United States, Regions, States, and Puerto Rico. April 1, 2010 to July 1, 2014 (NST-EST2014-01) from http://www.census.gov/popest/data/state/totals/2014/index.html.
- United States Department of, H., Human Services. Substance, A., Mental Health Services Administration. Center for Behavioral Health, S., & Quality. National Survey on Drug Use and Health, 2013. 2015 Retrieved from: http://doi.org/10.3886/ICPSR35509.v3.
- Van Dam NT, Earleywine M. Pulmonary function in cannabis users: Support for a clinical trial of the vaporizer. Int J Drug Policy. 2010;21(6):511–513. doi: 10.1016/j.drugpo.2010.04.001. [DOI] [PubMed] [Google Scholar]
- Vandrey R, Raber JC, Raber ME, Douglass B, Miller C, Bonn-Miller MO. Cannabinoid Dose and Label Accuracy in Edible Medical Cannabis Products. JAMA. 2015;313(24):2491–2493. doi: 10.1001/jama.2015.6613. [DOI] [PubMed] [Google Scholar]
- Wall MM, Poh E, Cerda M, Keyes KM, Galea S, Hasin DS. Adolescent marijuana use from 2002 to 2008: higher in states with medical marijuana laws, cause still unclear. Ann Epidemiol. 2011;21(9):714–716. doi: 10.1016/j.annepidem.2011.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang GS, Roosevelt G, Heard K. Pediatric marijuana exposures in a medical marijuana state. JAMA Pediatr. 2013;167(7):630–633. doi: 10.1001/jamapediatrics.2013.140. [DOI] [PubMed] [Google Scholar]
- Wang GS, Roosevelt G, Le Lait MC, Martinez EM, Bucher-Bartelson B, Bronstein AC, Heard K. Association of unintentional pediatric exposures with decriminalization of marijuana in the United States. Ann Emerg Med. 2014;63(6):684–689. doi: 10.1016/j.annemergmed.2014.01.017. [DOI] [PubMed] [Google Scholar]
- Wu TC, Tashkin DP, Djahed B, Rose JE. Pulmonary hazards of smoking marijuana as compared with tobacco. N Engl J Med. 1988;318(6):347–351. doi: 10.1056/NEJM198802113180603. [DOI] [PubMed] [Google Scholar]


