Heart failure (HF) is a chronic condition in which active patient engagement in self-care is essential to achieve optimal outcomes.1–3 Self-care is a naturalistic decision-making process involving self-care maintenance, defined as activities to maintain physiological stability (e.g., low sodium diet) and self-care management, defined as recognizing altered health status, responding to it in a timely manner, and evaluating the effectiveness of the response undertaken.1 Self-care confidence is a critical component influencing patients’ self-care maintenance and management behaviors.1
Adequate self-care contributes to improving health status and decreasing hospitalizations and mortality.1 However, most patients’ self-care is sub-optimal.4,5 Jaarsma and colleagues reported that less than half of patients with HF in 15 countries worldwide followed recommended self-care maintenance activities, such as following a low-sodium diet and regular weight monitoring.5
It is challenging for patients with HF to become competent in self-care because performing self-care entails following therapeutic regimens that require constantly engaging in decision-making and problem-solving.1,6 The presence of depressive symptoms may limit the ability to adequately perform self-care even when patients have adequate self-care knowledge and skills.7 According to Johansson and colleagues, patients with HF and depressive symptoms were 1.5 times more likely to wait longer than 72 hours before seeking treatment from health care providers after the onset of worsening HF symptoms than those without depressive symptoms.8
Social support is identified as a facilitator of successful self-care for patients with chronic illnesses (e.g., HF, diabetes, and arthritis).1,6,9–14 There are four types of social supports: emotional support providing caring, empathy, and love; instrumental support providing tangible services and goods, informational support assisting a problem-solving process, and appraisal support providing assistance with self-evaluation and affirmation of one’s action and statements by others.15
Social support is conveyed through members in the individual’s social network, which is defined as the web of relationships around an individual (e.g., number of co-habitants or friends).15 Social support is the function of social network, a structure of social ties around an individual.15 According to a recent systematic review on contributions of social support to HF self-care,16 main sources of social support among patients with HF were their spouses (62%) and adult children (32%), and relatives or friends (6%).
There are two different ways to conceptualize social support, which are received and perceived social support. Received social support refers to actual receipt of social support, while perceived social support refers to potential access to social support.17 Patients with HF often receive various types of social support from their informal caregivers (e.g., monitoring HF symptoms and arranging clinical appointments) and perceive high levels of social support, which helps to enhance their engagement in self-care.16,18 Received and perceived social support and structure of social ties (social network) also contributes to relieving psychological distress by fulfilling a sense of coherence and belonging.19 In a study in which patients with HF without depressive symptoms were followed for one year, patients who lived alone were 2.6 times more likely to develop depressive symptoms than those who lived with someone at baseline.20
Given the positive relationships of social support with better self-care and fewer negative emotions (e.g., depressive symptoms) in patients with HF, it can be hypothesized that social support may counteract the impact of depressive symptoms on self-care. However, few studies have investigated if social support plays a role in the relationship between depressive symptoms and self-care in patients with HF.
Living arrangements are considered as one of the most salient indicators of social support as living arrangements is a channel which social support is provided through.10 Information about whether patients live with others in a shared space is an indication of the availability of informal care provided within the household and the possibility of frequent assessment of the patient’s health status and self-care behaviors.21 Living alone is identified as a risk factor for poor self-and mortality in patients with chronic illness13,22,23 and nursing home admission and hospitalizations in older adults.24,25 Therefore, the purpose of this study was to examine the potential buffering effect of living arrangements, as an indicator of social support, on the relationship between depressive symptoms and self-care in patients with HF. The specific aim was to determine whether depressive symptoms had direct and/or indirect effects on self-care constructs proposed by Riegel and colleagues (i.e., self-care maintains, self-care management, and self-care confidence)1,26 in HF patients living alone and those living with others.
Methods
This study was a secondary analysis of cross-sectional data collected on stable HF patients recruited from ambulatory HF clinics affiliated with large community hospitals and academic medical centers in the United States. Data included in this analysis were collected at baseline of two large studies. One study was a randomized-controlled trial to test whether the combined biofeedback and cognitive therapy is effective to improve HF outcomes (National Institutes of Health/National Institutes of Nursing Research R01 NR 008567). The other study was a longitudinal observational study aimed at examining the relationship between sodium intake and HF outcomes.27 Those two parent studies had a similar participant eligibility and shared recruitment sites. The institutional review board was approved for each study site where patients were recruited. All participants gave written, signed informed consent.
Sample
Potential participants referred to study staff by cardiology providers in HF clinics. All patients had a cardiologist confirmed diagnosis of HF with either preserved or reduced ejection fraction. Patients were excluded for any of the following criteria: (1) age of < 21 years; (2) recent myocardial infarction within 3 months prior to the enrollment; (3) referral for heart transplant; (4) non-cardiac serious or life-threatening comorbid conditions (e.g., end-stage renal or active cancer treatment); (5) obvious cognitive impairments that hindered providing informed consent; or (6) non-English speaking. In this analysis a total of 206 patients who had variables of interest, such as three constructs of self-care and depressive symptoms, were included.
Measures
HF self-care
The Self-Care of Heart Failure Index (SCHFI) was used to measure self-care.28 This instrument consists of a total of 17 items measuring three constructs of self-care: self-care maintenance (5 items about monitoring signs and symptoms of HF exacerbation and adhering to therapeutic regimens), self-care management (8 items about ability to recognize and react appropriately to changes in symptoms), and self-care confidence (4 items about perceived confidence to perform the specific tasks of self-care). Patients are asked to rate each item on a 4-point Likert scale from 1 to 4. Items in the subscale of self-care management are answered only by patients who had dyspnea or lower-extremity edema past three months. Scores of each construct were summed and standardized to 100 with higher scores indicating better self-care. A score of ≥70 is used as a cut-off point to define adequacy of self-care.29 The reliability and validity of the SCHFI were demonstrated.28
Depressive symptoms
Depressive symptoms were measured with the self-administered Patient Health Questionnaire nine-item depression scale (PHQ-9), which has been widely validated.30 The PHQ-9 consists of the nine criteria for depression from the Diagnostic and Statistical Manual of Mental Disorders, fourth edition (DSM-IV). Each item is assigned points from 0 to 3 (0=not at all and 3=nearly every day). Scores for each item are summed to yield a total score with higher scores indicating a greater level of depressive symptoms. A total score of 5 to 9 represents mild depressive symptoms; 10 to 14, moderate; 15 to 19, moderately severe; and 20 to 27, severe. The PHQ-9 scores of ≥ 10 suggest clinical depression with a sensitivity of 88% and a specificity of 88% for detecting clinical depression in the primary care setting.31
Living arrangements
Patients’ report of whether or not they were living with someone was used to determine their living arrangements.
Socio-demographic and clinical characteristics
Self-report was used to collect information regarding the patients’ socio-demographic characteristics (e.g., age, gender, ethnicity, and education). Most information on the patients’ clinical characteristics (e.g., HF etiology) was abstracted by trained research nurses from medical records. Information about New York Heart Association (NYHA) functional class was determined by trained research nurses using structured interviews.
Data analysis
Demographic and clinical differences by living arrangement (i.e., living alone vs. living with someone) were tested with chi-square test or independent t-test using SAS 9.3 (SAS Institute Inc., Cary, NC). The strength of the associations among depressive symptoms and three self-care constructs (i.e., self-care maintenance, self-management, and self-care confidence) was evaluated with Spearman’s correlation coefficients (ρ).
In this study we only included patients who had scores of all three subscales of SCHFI (n=206) in order to include all three self-care constructs in the structural equation modeling. Structural equation modeling was used to conduct path analyses using Mplus version 7.0 (Muthen and Muthen). NYHA functional class was used as a covariate throughout the path analyses because NYHA functional class is related to self-care.32–35 We first examined the relationship between depressive symptoms and three self-care constructs. The first series of paths corresponded to the relationship among the three constructs based on the conceptual framework by Riegel and colleagues in which self-care maintenance leads to self-care management, and self-care confidence influences both self-care maintenance and management.26 A second series of paths corresponded to the association between depressive symptoms as an independent variable and the three self-care constructs, as dependent variables. Next, we compared the series of paths examined above between patients living alone and those living with someone. The overall model fit was judged to be adequate if the p-value of the chi-square test was below 0.05, Comparative Fit Index (CFI) values were above 0.90 and Standardized Root Mean Square Residual (SMSR) values were below 0.08.36
Results
Sample characteristics
The majority of the patients were male (66.5%) and white (77.2%) with an average age of 60 years (range: 32–87 years) (Table 1). More than half of the patients were married or co-habitating with a partner (52.4%) and in NYHA functional class III/IV (55.8%). On average, patients had poor self-care maintenance and management according to the cut-off score of 70 suggested by Riegel and colleagues.29 Patients having PHQ-9 scores of ≥ 10 were 29.6% (61/206) of the total sample, who had probable clinical depression. (Figure 1)
Table 1.
Sample Characteristics (N=206)
| Total (N = 206) | Living alone (n = 53) | Living with someone (N = 153) | p-value | |
|---|---|---|---|---|
| Age, years | 60 (11.6) | 61 (11.6) | 59 (11.6) | 0.187 |
|
| ||||
| Female | 69 (33.5%) | 23 (43.4%) | 46 (30.1%) | 0.076 |
|
| ||||
| Education level, years | 13 (3.3) | 13 (2.9) | 13 (3.4) | 0.614 |
|
| ||||
| Ethnicity | 0.427 | |||
| White | 159 (77.2%) | 43 (81.1%) | 116 (75.8%) | |
| Minority | 47 (22.8%) | 10 (18.9%) | 37 (24.2%) | |
|
| ||||
| NYHA class | 0.650 | |||
| I/II | 91 (44.2%) | 22 (41.5%) | 69 (45.1%) | |
| III/IV | 115 (55.8%) | 31 (58.5%) | 84 (54.9%) | |
|
| ||||
| Ischemic etiology of HF (n=197) | 139 (70.6%) | 39 (78.0%) | 100 (68.0%) | 0.027 |
|
| ||||
| Chalson Comorbidity Index | 3.3 (2.0) | 3.7 (2.2) | 3.2 (1.9) | 0.124 |
|
| ||||
| Self-care | ||||
| Maintenance | 49.6 (22.5) | 46.9 (21.5) | 50.5 (22.9) | 0.314 |
| Management | 54.7 (21.3) | 52.6 (20.9) | 55.5 (21.4) | 0.407 |
| Confidence | 56.5 (22.0) | 49.2 (18.7) | 59.0 (22.6) | 0.005 |
|
| ||||
| Depressive Symptoms | 6.9 (5.6) | 8.0 (5.5) | 6.5 (5.6) | 0.098 |
|
| ||||
| Medications | ||||
| ACEI or ARB (n=204) | 158 (77.5%) | 39 (73.6%) | 119 (78.8%) | 0.434 |
| Beta Blocker (n=203) | 177 (87.2%) | 46 (88.5%) | 131 (86.8%) | 0.751 |
| Diuretics (n=203) | 154 (75.9%) | 40 (75.5%) | 114 (76.0%) | 0.938 |
| Antidepressants (n=203) | 50 (24.6%) | 17 (32.1%) | 33 (22.0%) | 0.143 |
Note. Values are mean (SD) or n (%).
NYHA=New York Heart Association; HF= Heart Failure; ACEI = angiotensin converting enzyme inhibitor; ARB = angiotensin receptor blocker
Figure 1.
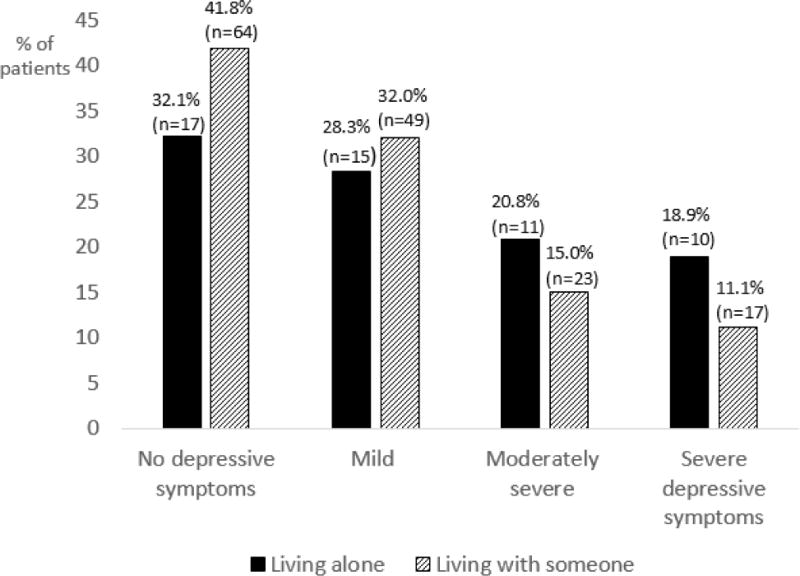
Depressive symptoms by living arrangements (n=206)
Note. There were no differences in proportion of patients living alone to those living with someone by each depressive symptom level (p=0.294).
Demographic and clinical characteristics between patients living alone vs. with someone were not significantly different except for marital status, etiology of HF, and self-care confidence (Table 1). Of patients living with someone more than two thirds of their informal caregivers (69.6%) were their spouses. Patients living with someone had higher scores on self-care confidence than patients living alone (p-value < 0.05). There were no significant differences in scores for depressive symptoms between patients living alone and patients living with someone.
Correlation among depressive symptoms and self-care
As shown in Table 2, there were weak negative correlations between scores for depressive symptoms and scores for self-care maintenance and confidence (ρ= −0.171 and −0.151, respectively). As depressive symptoms increased, self-care maintenance and confidence scores decreased. Scores for three self-care constructs were positively correlated with each other (ρ=0.242–0.360).
Table 2.
Correlation coefficients of variable of interest (N=206)
| Self-care maintenance | Self-care management | Self-care confidence | |
|---|---|---|---|
| Depressive symptoms | −0.171* | −0.071 | −0.151* |
| Self-care maintenance | 1.00 | 0.360‡ | 0.242‡ |
| Self-care management | 1.00 | 0.334‡ | |
| Self-care confidence | 1.00 |
Note.
=p-value <0.05;
= p-value <0.001
Patients living alone
Among patients who lived alone, depressive symptoms scores were moderately correlated with self-care maintenance and management scores (ρ=−0.364, p-value<0.001; and ρ= −0.388, p-value<0.001, respectively). The positive correlation between self-care maintenance and management scores indicates better self-care maintenance was associated with higher self-care management (ρ= 0.300, p-value<0.05). Self-care management scores were moderately positively correlated with self-care confidence (ρ= 0.421, p-value<0.001).
Patients living with someone
Among patients who lived with someone, depressive symptoms scores were not correlated with any of the self-care constructs. The scores for self-care maintenance were moderately correlated with the scores for self-care management and confidence (ρ= 0.377, p-value<0.001; and ρ= 0.244, p-value<0.001, respectively). The scores for self-care management were positively correlated with the scores for self-care confidence (ρ= 0.304, p-value<0.001).
Path analyses
The path diagrams with standardized coefficients are presented in Figures 2 and 3.
Figure 2.
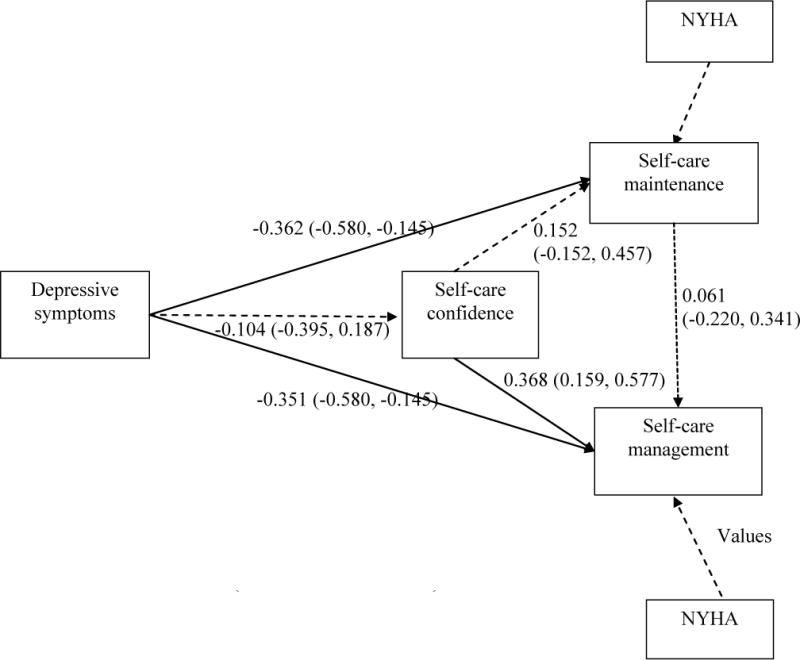
Path model with patients living alone (n=53)
Note. Solid lines indicate significant paths dotted lines indicate insignificant paths. Values are standardized coefficients (95% confidence interval).
Model fit indices: X2 = 31.971 (df = 9, p < 0.001), Comparative Fit Index = 0.859, Standardized Root Mean Square Residual =0.062.
NYHA= New York Heart Association functional class
Figure 3.
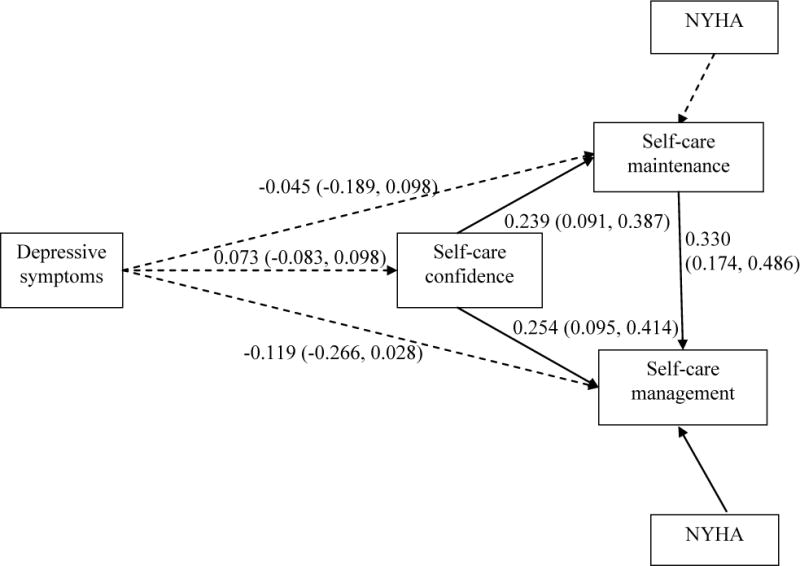
Path model with patients living with someone (n=153)
Note. Solid lines indicate significant paths dotted lines indicate insignificant paths. Values are standardized coefficients (95% confidence interval).
Model fit indices: X2 = 51.500 (df = 9, p value < 0.001), Comparative Fit Index = 1.000, Standardized Root Mean Square Residual <0.0001.
NYHA= New York Heart Association functional class
Patients living alone
Depressive symptoms had direct effects on self-care maintenance and management (standardized β= −0.362 and −0.351, respectively) after controlling for NYHA functional class, indicating that higher levels of depressive symptoms were related to poorer self-care maintenance and management (Figure 2). However, there was no significant direct effect of depressive symptoms on self-care confidence. There were also no indirect effects of depressive symptoms on self-care maintenance and management via self-care confidence.
Patients living with someone
Depressive symptoms did not have any significant direct effects on self-care maintenance, management, or confidence after controlling for NYHA functional class (Figure 3). Similarly, there were no indirect effects of depressive symptoms on self-care maintenance and management through self-care confidence.
Discussion
In this study we addressed whether the relationship between depressive symptoms and self-care differed by living arrangement as a proxy of social support in patients with HF. Depressive symptoms were negatively related to self-care behaviors among patients living alone, but were not associated with self-care behaviors among patients living with someone. Our results suggest that the negative effect of depressive symptoms on self-care is buffered by the presence of others living in a shared household.
Depressive symptoms have been shown to be a determinant of poor self-care in patients with HF. For example, patients with depressive symptoms are less likely to follow recommended therapeutic regimens such as a low-sodium diet.9,32,37,38 Similarly, we also found the negative relationship between depressive symptoms and self-care maintenance (ρ=−0.171). Although the mechanism underlying the association between depressive symptoms and self-care is not clearly understood, motivation and cognitive function are two plausible mechanisms that could explain the relationship. In the general population, individuals with depression had a shift in cost/benefit gradients of behaviors, such as over-estimating costs of obtaining rewards or under-estimating expected benefits compared with individuals without depression.39 This inaccurate cost/benefit evaluation of activities contributes to diminishing motivation to pursue activities.39–41 Thus, depressed patients with HF may perceive self-care activities as burdensome compared to potential positive outcomes and be less likely to exert efforts to follow recommended self-care behaviors. In a meta-analysis of depression and cognitive function,42 depression negatively affected cognitive function in the domains of episodic memory, executive function, and processing speed. Given that self-care is a priority setting and decision-making process, poor cognitive function can negatively impact self-care in patients with HF.9,43
When the relationship between depressive symptoms and the three self-care constructs (i.e., self-care maintenance, management, and confidence) was examined in our study, the association among these constructs proposed by Riegel and colleagues1 (i.e., self-care maintenance leads to self-care management, and self-care confidence influences both self-care maintenance and management) was found only in patients who lived with someone, but not in patients who lived alone. This discrepancy might be related to the strong direct effects of depressive symptoms on self-care maintenance and management in patients living alone.
In an intervention study in which the effect of the cognitive behavioral therapy (CBT) aimed at decreasing depression on smoking cessation was examined in post-myocardial infarction patients, the CBT intervention was only effective to decrease depression and increase rates of smoking cessation only in the group of the patients who were depressed and had adequate social support.44 This result indicates that social support contributes to patients with depression engaging in healthy behaviors. Thus, this finding demonstrates that depressive symptoms play a more substantial role in self-care in HF patients living alone than in those living with someone.
It may be that those patients who live with someone have the advantage of assistance from their co-habitants, which results in increased adherence to self-care and negating the observation that depressed patients with HF are less likely to engage in self-care.9,32,37,38 Potential sources of support within the household include companionship, emotional support, and regular instrumental, and informational assistance.21 Such social support systems may positively contribute to self-care in patients experiencing depressive symptoms. High levels of social network systems (defined as being married, living with others, having face-to-face or telephone contacts with family members living away daily or almost daily, and being at home alone for < 2 hours a day) were associated with decrease in rehospitalizations among HF patients living in Spain.45
An informal caregiver’s contribution to the patient’s day-to-day self-care can be substantial. For example, approximately 80% of patients with HF living in Netherlands reported that they received emotional and practical support in their medical care from informal caregivers defined as a partner.18 Spousal caregivers’ confidence in their contribution to the patients’ self-care was positively associated with patients’ self-care according to a study conducted in Italy.46 Patients’ self-care confidence was also related to spousal caregivers’ contribution to self-care.46 A study conducted in the United States by Artinian and colleagues22 provides further insight in terms of the benefits of co-residence. They found that living arrangements made a larger contribution to self-care activities than did marital status. Thus, having someone living in the same household regardless of relationship may have a positive impact on self-care and buffer the negative effect of depressive symptoms in patients with HF.
According to Riegel and colleagues self-care confidence influences both self-care maintenance and management.1 Interestingly, for patients living alone, the indirect paths from depressive symptoms to self-care maintenance and managements via self-care confidence were not significant in our study. This result suggests that improving self-care confidence does not result in promoting self-care maintenance and management among depressed patients who live alone. Therefore, arranging resources that can provide practical support might be an effective way to improve self-care maintenance and management in depressed patients who live alone, instead of efforts focusing on promoting self-care confidence alone.
Limitations
Several limitations of this study are recognized. Because this was a cross-sectional design, we cannot draw causal relationships among living arrangements, depressive symptoms, and self-care. In this study we used living arrangements as a proxy of social support, which is the availability of support through one’s living circumstances. However, we did not collect the number of informal caregivers within the household and actual or perceived social support (e.g., emotional and instrumental support), which limits our understanding of the role of social support on the relationship between depressive symptoms and self-care in patients with HF. The information about reasons for living alone was not asked in this study although it might be possible that people who chose to live alone are more likely to be capable of performing activities of daily living and have different levels of self-care confidence compared to those who are subject to living alone due to a lack of social ties. Among people aged above 80 years who are at risk of or with atherothrombosis, living alone was not associated with mortality.23 Future studies addressing this additional information are needed.
Conclusions
An emphasis on self-care increases in HF management because of its pivotal role in preventing poor outcomes. Depressive symptoms hinder patients with HF from actively engaging in self-care. However, our findings suggest that the potential availability of support in a shared household can offset the negative impact of depressive symptoms on self-care in patients with HF. Patients with depressive symptoms who live alone lack support and may be more vulnerable to poor self-care than those who live with someone. Therefore, clinicians should pay particular attention to assessment and management of depressive symptoms in patients living alone who may be most vulnerable to poor self-care.
Acknowledgments
Funding: NIH # R01 NR008567 from the National Institute of Nursing Research and a Center grant from NIH National Institute of Nursing Research # 1P20NR010679. Research funding from Chungnam National University (Kyoung Suk Lee, principal investigator)
Footnotes
Conflicts of interest: No Disclosures to Report
Contributor Information
Kyoung Suk Lee, Assistant Professor, Chungnam National University, College of Nursing, Dea Jeon, South Korea.
Terry A. Lennie, Professor, and Associate Dean, PhD Studies University of Kentucky, College of Nursing, USA.
Ju Young Yoon, Assistant Professor, University of Wisconsin-Madison, School of Nursing, USA.
Jia-Rong Wu, Assistant Professor, The University of North Carolina at Chapel Hill, School of Nursing, USA.
Debra K. Moser, Professor and Gill Endowed Chair of Nursing, Co-Director RICH Heart Program, University of Kentucky, College of Nursing, USA.
References
- 1.Riegel B, Lee CS, Dickson VV. Self care in patients with chronic heart failure. Nature reviews. Cardiology. 2011 Nov;8(11):644–654. doi: 10.1038/nrcardio.2011.95. [DOI] [PubMed] [Google Scholar]
- 2.Lee KS, Lennie TA, Warden S, Jacobs-Lawson JM, Moser DK. A comprehensive symptom diary intervention to improve outcomes in patients with HF: a pilot study. Journal of cardiac failure. 2013 Sep;19(9):647–654. doi: 10.1016/j.cardfail.2013.07.001. [DOI] [PubMed] [Google Scholar]
- 3.Dracup K, Moser DK, Pelter MM, et al. Randomized, controlled trial to improve self-care in patients with heart failure living in rural areas. Circulation. 2014 Jul 15;130(3):256–264. doi: 10.1161/CIRCULATIONAHA.113.003542. [DOI] [PubMed] [Google Scholar]
- 4.Lee KS, Lennie TA, Dunbar SB, et al. The Association Between Regular Symptom Monitoring and Self-care Management in Patients With Heart Failure. The Journal of cardiovascular nursing. 2015 Mar-Apr;30(2):145–151. doi: 10.1097/JCN.0000000000000128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jaarsma T, Stromberg A, Ben Gal T, et al. Comparison of self-care behaviors of heart failure patients in 15 countries worldwide. Patient education and counseling. 2013 Jul;92(1):114–120. doi: 10.1016/j.pec.2013.02.017. [DOI] [PubMed] [Google Scholar]
- 6.Moser DK, Watkins JF. Conceptualizing self-care in heart failure: a life course model of patient characteristics. The Journal of cardiovascular nursing. 2008 May-Jun;23(3):205–218. doi: 10.1097/01.JCN.0000305097.09710.a5. [DOI] [PubMed] [Google Scholar]
- 7.Hwang B, Moser DK, Dracup K. Knowledge is insufficient for self-care among heart failure patients with psychological distress. Health Psychol. 2014 Jul;33(7):588–596. doi: 10.1037/a0033419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Johansson P, Nieuwenhuis M, Lesman-Leegte I, van Veldhuisen DJ, Jaarsma T. Depression and the delay between symptom onset and hospitalization in heart failure patients. European journal of heart failure. 2011 Feb;13(2):214–219. doi: 10.1093/eurjhf/hfq200. [DOI] [PubMed] [Google Scholar]
- 9.Riegel B, Vaughan Dickson V, Goldberg LR, Deatrick JA. Factors associated with the development of expertise in heart failure self-care. Nursing research. 2007 Jul-Aug;56(4):235–243. doi: 10.1097/01.NNR.0000280615.75447.f7. [DOI] [PubMed] [Google Scholar]
- 10.Graven LJ, Grant JS. Social support and self-care behaviors in individuals with heart failure: an integrative review. International journal of nursing studies. 2014 Feb;51(2):320–333. doi: 10.1016/j.ijnurstu.2013.06.013. [DOI] [PubMed] [Google Scholar]
- 11.Jerant AF, von Friederichs-Fitzwater MM, Moore M. Patients’ perceived barriers to active self-management of chronic conditions. Patient education and counseling. 2005 Jun;57(3):300–307. doi: 10.1016/j.pec.2004.08.004. [DOI] [PubMed] [Google Scholar]
- 12.Searle A, Norman P, Thompson R, Vedhara K. Illness representations among patients with type 2 diabetes and their partners: relationships with self-management behaviors. J Psychosom Res. 2007 Aug;63(2):175–184. doi: 10.1016/j.jpsychores.2007.02.006. [DOI] [PubMed] [Google Scholar]
- 13.Toljamo M, Hentinen M. Adherence to self-care and glycaemic control among people with insulin-dependent diabetes mellitus. J Adv Nurs. 2001 Jun;34(6):780–786. doi: 10.1046/j.1365-2648.2001.01808.x. [DOI] [PubMed] [Google Scholar]
- 14.Trivedi RB, Bryson CL, Udris E, Au DH. The influence of informal caregivers on adherence in COPD patients. Annals of behavioral medicine: a publication of the Society of Behavioral Medicine. 2012 Aug;44(1):66–72. doi: 10.1007/s12160-012-9355-8. [DOI] [PubMed] [Google Scholar]
- 15.Langford CP, Bowsher J, Maloney JP, Lillis PP. Social support: a conceptual analysis. J Adv Nurs. 1997 Jan;25(1):95–100. doi: 10.1046/j.1365-2648.1997.1997025095.x. [DOI] [PubMed] [Google Scholar]
- 16.Buck HG, Harkness K, Wion R, et al. Caregivers’ contributions to heart failure self-care: a systematic review. European journal of cardiovascular nursing: journal of the Working Group on Cardiovascular Nursing of the European Society of Cardiology. 2015 Feb;14(1):79–89. doi: 10.1177/1474515113518434. [DOI] [PubMed] [Google Scholar]
- 17.Uchino BN. Understanding the Links Between Social Support and Physical Health: A Life-Span Perspective With Emphasis on the Separability of Perceived and Received Support. Perspectives on psychological science: a journal of the Association for Psychological Science. 2009 May;4(3):236–255. doi: 10.1111/j.1745-6924.2009.01122.x. [DOI] [PubMed] [Google Scholar]
- 18.Gallagher R, Luttik ML, Jaarsma T. Social support and self-care in heart failure. The Journal of cardiovascular nursing. 2011 Nov-Dec;26(6):439–445. doi: 10.1097/JCN.0b013e31820984e1. [DOI] [PubMed] [Google Scholar]
- 19.Bisschop MI, Kriegsman DM, Beekman AT, Deeg DJ. Chronic diseases and depression: the modifying role of psychosocial resources. Social science & medicine. 2004 Aug;59(4):721–733. doi: 10.1016/j.socscimed.2003.11.038. [DOI] [PubMed] [Google Scholar]
- 20.Havranek EP, Spertus JA, Masoudi FA, Jones PG, Rumsfeld JS. Predictors of the onset of depressive symptoms in patients with heart failure. Journal of the American College of Cardiology. 2004 Dec 21;44(12):2333–2338. doi: 10.1016/j.jacc.2004.09.034. [DOI] [PubMed] [Google Scholar]
- 21.Weaver FM, Weaver BA. Does availability of informal care within the household impact hospitalisation? Health Econ Policy Law. 2014 Jan;9(1):71–93. doi: 10.1017/S1744133113000169. [DOI] [PubMed] [Google Scholar]
- 22.Artinian NT, Magnan M, Sloan M, Lange MP. Self-care behaviors among patients with heart failure. Heart & Lung. 2002 May-Jun;31(3):161–172. doi: 10.1067/mhl.2002.123672. [DOI] [PubMed] [Google Scholar]
- 23.Udell JA, Steg PG, Scirica BM, et al. Living alone and cardiovascular risk in outpatients at risk of or with atherothrombosis. Arch Intern Med. 2012 Jul 23;172(14):1086–1095. doi: 10.1001/archinternmed.2012.2782. [DOI] [PubMed] [Google Scholar]
- 24.Gaugler JE, Duval S, Anderson KA, Kane RL. Predicting nursing home admission in the U.S: a meta-analysis. BMC geriatrics. 2007;7:13. doi: 10.1186/1471-2318-7-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mu C, Kecmanovic M, Hall J. Does Living Alone Confer a Higher Risk of Hospitalisation? Economic Record. 2015:n/a–n/a. [Google Scholar]
- 26.Riegel B, Dickson VV. A situation-specific theory of heart failure self-care. The Journal of cardiovascular nursing. 2008 May-Jun;23(3):190–196. doi: 10.1097/01.JCN.0000305091.35259.85. [DOI] [PubMed] [Google Scholar]
- 27.Lennie TA, Song EK, Wu JR, et al. Three gram sodium intake is associated with longer event-free survival only in patients with advanced heart failure. Journal of cardiac failure. 2011 Apr;17(4):325–330. doi: 10.1016/j.cardfail.2010.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Riegel B, Carlson B, Moser DK, Sebern M, Hicks FD, Roland V. Psychometric testing of the self-care of heart failure index. Journal of cardiac failure. 2004 Aug;10(4):350–360. doi: 10.1016/j.cardfail.2003.12.001. [DOI] [PubMed] [Google Scholar]
- 29.Riegel B, Lee CS, Dickson VV, Carlson B. An update on the self-care of heart failure index. The Journal of cardiovascular nursing. 2009 Nov-Dec;24(6):485–497. doi: 10.1097/JCN.0b013e3181b4baa0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Spitzer RL, Kroenke K, Williams JB. Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study. Primary Care Evaluation of Mental Disorders. Patient Health Questionnaire. JAMA: the journal of the American Medical Association. 1999 Nov 10;282(18):1737–1744. doi: 10.1001/jama.282.18.1737. [DOI] [PubMed] [Google Scholar]
- 31.Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. Journal of general internal medicine. 2001 Sep;16(9):606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Cameron J, Worrall-Carter L, Page K, Riegel B, Lo SK, Stewart S. Does cognitive impairment predict poor self-care in patients with heart failure? European journal of heart failure. 2010 May;12(5):508–515. doi: 10.1093/eurjhf/hfq042. [DOI] [PubMed] [Google Scholar]
- 33.Suwanno J, Petpichetchian W, Riegel B, Issaramalai SA. A model predicting health status of patients with heart failure. J Cardiovasc Nurs. 2009 Mar-Apr;24(2):118–126. doi: 10.1097/JCN.0b013e318197a75c. [DOI] [PubMed] [Google Scholar]
- 34.Davis KK, Himmelfarb CR, Szanton SL, Hayat MJ, Allen JK. Predictors of heart failure self-care in patients who screened positive for mild cognitive impairment. The Journal of cardiovascular nursing. 2015 Mar-Apr;30(2):152–160. doi: 10.1097/JCN.0000000000000130. [DOI] [PubMed] [Google Scholar]
- 35.Lee CS, Riegel B, Driscoll A, et al. Gender differences in heart failure self-care: a multinational cross-sectional study. Int J Nurs Stud. 2009 Nov;46(11):1485–1495. doi: 10.1016/j.ijnurstu.2009.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hu LT, Bentler PM. Cutoff Criteria for Fit Indexes in Covariance Structure Analysis: Conventional Criteria Versus New Alternatives. Struct Equ Modeling. 1999;6(1):1–55. [Google Scholar]
- 37.Wu JR, Lennie TA, Dekker RL, Biddle MJ, Moser DK. Medication adherence, depressive symptoms, and cardiac event-free survival in patients with heart failure. Journal of cardiac failure. 2013 May;19(5):317–324. doi: 10.1016/j.cardfail.2013.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Luyster FS, Hughes JW, Gunstad J. Depression and anxiety symptoms are associated with reduced dietary adherence in heart failure patients treated with an implantable cardioverter defibrillator. The Journal of cardiovascular nursing. 2009 Jan-Feb;24(1):10–17. doi: 10.1097/01.JCN.0000317469.63886.24. [DOI] [PubMed] [Google Scholar]
- 39.Treadway MT, Bossaller NA, Shelton RC, Zald DH. Effort-based decision-making in major depressive disorder: a translational model of motivational anhedonia. Journal of abnormal psychology. 2012 Aug;121(3):553–558. doi: 10.1037/a0028813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Klein D. Depression and anhedonia. New York: PMA Publishing; 1987. [Google Scholar]
- 41.Sherdell L, Waugh CE, Gotlib IH. Anticipatory pleasure predicts motivation for reward in major depression. Journal of abnormal psychology. 2012 Feb;121(1):51–60. doi: 10.1037/a0024945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.McDermott LM, Ebmeier KP. A meta-analysis of depression severity and cognitive function. J Affect Disord. 2009 Dec;119(1–3):1–8. doi: 10.1016/j.jad.2009.04.022. [DOI] [PubMed] [Google Scholar]
- 43.Lee CS, Gelow JM, Bidwell JT, et al. Blunted Responses to Heart Failure Symptoms in Adults With Mild Cognitive Dysfunction. J Cardiovasc Nurs. 2012 Sep 25; doi: 10.1097/JCN.0b013e31826620fa. [DOI] [PubMed] [Google Scholar]
- 44.Trockel M, Burg M, Jaffe A, Barbour K, Taylor CB. Smoking behavior postmyocardial infarction among ENRICHD trial participants: cognitive behavior therapy intervention for depression and low perceived social support compared with care as usual. Psychosomatic medicine. 2008 Oct;70(8):875–882. doi: 10.1097/PSY.0b013e3181842897. [DOI] [PubMed] [Google Scholar]
- 45.Rodriguez-Artalejo F, Guallar-Castillon P, Herrera MC, et al. Social network as a predictor of hospital readmission and mortality among older patients with heart failure. Journal of cardiac failure. 2006 Oct;12(8):621–627. doi: 10.1016/j.cardfail.2006.06.471. [DOI] [PubMed] [Google Scholar]
- 46.Vellone E, Chung ML, Cocchieri A, Rocco G, Alvaro R, Riegel B. Effects of self-care on quality of life in adults with heart failure and their spousal caregivers: testing dyadic dynamics using the actor-partner interdependence model. J Fam Nurs. 2014 Feb;20(1):120–141. doi: 10.1177/1074840713510205. [DOI] [PubMed] [Google Scholar]


