Abstract
We previously identified osteopontin (OPN) as a promising marker for the early detection of hepatocellular carcinoma (HCC). In this study, we investigated the association between pre-diagnostic circulating OPN levels and HCC incidence in a large population-based cohort. A nested-case control study was conducted within the EPIC cohort. During a mean follow-up of 4.8 years, 100 HCC cases were identified. Each case was matched to two controls and OPN levels were measured in baseline plasma samples. Viral hepatitis, liver function and alpha-fetoprotein (AFP) tests were also conducted. Conditional logistic regression models were used to calculate multivariable odds ratio (OR) and 95% confidence intervals (95%CI) for OPN levels in relation to HCC. Receiver operating characteristics curves were constructed to determine the discriminatory accuracy of OPN alone or in combination with other liver biomarkers in the prediction of HCC. OPN levels were positively associated with HCC risk (per 10% increment, ORmultivariable=1.30; 95%CI:1.14–1.48). The association was stronger among cases diagnosed within two years of follow-up. Adding liver function tests to OPN improved the discriminatory performance for subjects who developed HCC (AUC=0.86). For cases diagnosed within two years, the combination of OPN and AFP was best able to predict HCC risk (AUC=0.88). The best predictive model for HCC in this low-risk population is OPN in combination with liver function tests. Within two years of diagnosis, the combination of OPN and AFP best predicted HCC development, suggesting that measuring OPN and AFP could identify high-risk groups independently of a liver disease diagnosis.
Keywords: Liver Cancer, Risk prediction, Biomarker, Cohort study, Osteopontin
Introduction
Liver cancer is the sixth most commonly diagnosed cancer and the second leading cause of cancer death worldwide (1). Hepatocellular carcinoma (HCC), the most common type of liver cancer (2), is primarily associated with chronic hepatitis B and C virus (HBV/HCV) infections, heavy alcohol drinking, smoking, non-alcoholic steatohepatitis (NASH) and, in high incidence areas, dietary exposure to aflatoxin (3–5). HCC incidence rates have increased over the past 20 years in Western Europe and the United States (2). The aging HCV infected population and the growing pandemic of diabetes and obesity causing NASH are thought to be largely responsible for the observed surge in HCC incidence. HCC is often diagnosed at a late stage and has poor prognosis due to limited treatment options. Because mainly small tumors are accessible to curative treatments and such tumors are asymptomatic, identification of high risk individuals that would benefit from surveillance and novel biomarkers for early detection of this highly lethal disease are urgently needed. For the last 40 years, α-fetoprotein (AFP) has been the only serum marker routinely used by clinicians together with ultrasound for the detection and surveillance of HCC, despite its low sensitivity (ranging from 41 to 65%) for the detection of early-stage HCC (6, 7).
We have previously identified osteopontin (OPN) as an early stage HCC biomarker with greater performance than AFP as well as complementary properties to AFP in discriminating HCC patients in a population already at high risk for HCC development (8, 9). Furthermore, we showed that the performance of OPN remained intact a year prior to HCC diagnosis in this high risk group (8, 9). The performance of OPN for the early detection of HCC was further validated in independent studies (10–12). OPN is an extracellular matrix protein that has been implicated in several carcinogenic and angiogenic processes, such as cell invasion, inflammation, tumor progression, and metastasis (13, 14). High OPN levels have also been associated with reduced survival in patients with lung, prostate, breast or liver cancers (15, 16).
The aim of this study was to investigate the behaviour of circulating OPN in periods preceding HCC diagnosis in the general population, taking advantage of the European Prospective Investigation into Cancer and Nutrition (EPIC) cohort, a large heterogeneous cohort of Europeans, with a nested case-control subset for which measurements of HBV/HCV infection status and liver function biomarkers were conducted. EPIC is a large prospective cohort of >520,000 participants from 10 Western European countries, designed to investigate the association between diet, lifestyle and environmental factors and the incidence of cancers and other chronic diseases (17, 18). In EPIC, it was reported that smoking contributed to more HCCs (47.6%) than chronic HBV (13.2%) and HCV (20.9%) infections. Heavy alcohol consumption (10.2%) and obesity (16.1%) also contributed to sizeable fractions of this disease burden. Over one-third of HCCs could not be accounted for by exposure to at least one of the documented risk factors (19). In follow-up studies, associations with diet and vitamin D levels were reported (20, 21). The present study is the first to evaluate a novel biomarker for early detection of HCC and its behaviour in relation to time to diagnosis in EPIC.
Materials and methods
Study Population and Follow-up for Cancer Incidence
Detailed information on the study design, rationale and methods of the EPIC study, including assessment of diet and lifestyle factors, has been described previously (17, 18). Briefly, between 1991 and 2000 more than 520,000 men and women aged 20–85 years were recruited in 23 centres throughout 10 European countries (Denmark, France, Germany, Greece, Italy, the Netherlands, Norway, Spain, Sweden, and the United Kingdom). At recruitment, standardised dietary, lifestyle and socio-demographic questionnaires including information on physical activity, education, smoking, medical history and anthropometric data were collected. Blood samples were collected from participants at recruitment, immediately processed and fractionated into plasma, serum, white blood cells and red blood cells. These bio-samples are stored under liquid N2 at the International Agency for Research on Cancer (IARC, Lyon, France) for all countries except Denmark and Sweden. All cohort members provided written informed consent. Ethical approval for this study was obtained from the IARC ethical review board (Lyon, France) and participating centres.
Vital status follow-up (98.5% complete) is collected by record linkage with regional and/or national mortality registries in all countries except Germany and Greece, where follow-up is based on active follow-up through study subjects or their next-of-kin. Cancer incidence is determined through record linkage with population-based regional cancer registries (Denmark, Italy, the Netherlands, Norway, Spain, Sweden, and the United Kingdom) or via a combination of methods, including the use of health insurance records, contacts with cancer and pathology registries, and active follow-up through study subjects and their next-of-kin (France, Germany, Greece). For HCC, our definition is based on site C22.0 (with morphology codes 8170/3, 8171/3 and 8180/3). For our study, the bases of diagnosis for definition of HCC cases were as follows: Clinical observation/investigation (n=5), laboratory/biochemical examination (n=12), radiological examination, computerized tomography scan, magnetic resonance scan (n=10), cytology/hematology, histology of primary tumor (n=71) and autopsy report (n=2). For this study, the latest date of complete information for cancer incidence and vital status ranged from December 2002 to December 2006.
Ascertainment of HCC and Nested Case-control Study Design
HCC was the primary outcome of interest in this study. HCC was defined as first incident tumor in the liver (C22.0 as per the 10th Revision of the International Statistical Classification of Diseases, Injury and Causes of Death [ICD-10]). For each identified case, the histology and the methods used to diagnose the cancer were reviewed to exclude metastatic cases or other types of liver cancers.
The design of the nested case-control study has been previously described (19). A total of 125 HCC cases with available blood samples at baseline were identified between participants’ recruitment and 2006. For each case, two controls were selected by incidence density sampling from all cohort members alive and free of cancer (except non-melanoma skin cancer). The controls were matched by age at blood collection (±1 year), sex, study center, date (±2 months) and time of the day (±3 hours) at blood collection, and by fasting status (<3/3–6/>6 hours) at blood collection. Women were additionally matched by menopausal status (pre-/peri-/postmenopausal) and hormone replacement therapy use at time of blood collection (yes/no). Participants with insufficient blood sample were excluded (Ncases = 25 and Ncontrols = 56). For six cases, only one eligible matched control was available. Therefore, the final sample size for the present analysis included 100 HCC cases and 194 controls. The number of HCC cases per recruitment center is Denmark (N = 24), Germany (N = 20), Greece (N = 9), Italy (N = 14), Spain (N = 4), Sweden (N = 19), the Netherlands (N = 3), United Kingdom (N = 7).
Serum Biomarkers
Data for HBV and HCV seropositivity, for AFP and C-reactive protein (CRP) levels and for liver function tests, alanine aminotransferase (ALT), aspartate aminotransferase (AST), gamma-glutamyltransferase (GGT), alkaline phosphatase (ALP), albumin and total bilirubin were available and measured as previously described (20). In addition, the ratio of AST/ALT and BARD score were calculated and used as markers of liver fibrosis (22). BARD score, a non-invasive scoring system used to predict fibrosis severity in patients with non-alcoholic fatty liver disease, was calculated as the sum of BMI >28 = 1 point, AST/ALT >0.8 = 2 points and diabetes = 1 point. Plasma concentrations of OPN were measured using a commercial ELISA kit from R&D Systems (Minneapolis, MN) as previously described (8). Briefly, 50 μl of diluted (1:100) plasma samples were added to the ELISA plates pre-coated with a capture OPN antibody.
Statistical Analysis
Relevant baseline lifestyle and socio-demographic characteristics were described among cancer cases and matched controls. To assess correlations between OPN and liver function tests and other relevant variables, spearman partial correlation coefficients adjusted for age at recruitment and sex were estimated in cases and controls. Conditional logistic regression models were used to estimate odds ratios (OR) and 95% confidence intervals (CI) for associations between OPN levels and HCC risk. OPN was analyzed as continuous and categorical variables based on tertiles of the distribution among controls. Tests for linear trend were performed by assigning the median values of each tertile of OPN. For continuous analyses, OPN was log transformed for normalization and a unit of 10% increase in circulating OPN levels was used as the exposure variable in linear models.
For all analyses, both crude and multivariable models were run. Crude models were conditioned on the matching factors while multivariable models were additionally adjusted for the following relevant confounding factors: baseline alcohol intake at recruitment (g/d), pattern of lifetime alcohol intake (never drinker, former light drinker, former heavy drinker, light drinker, never heavy drinker, periodically heavy drinker, always heavy drinker, unknown), body mass index (BMI; kg/m2), and smoking status (never, former, current, and not specified). Other factors (height, weight, waist circumference, waist-to-hip ratio, education, physical activity, self-reported diabetes, and dietary intake of energy, fiber, tea, coffee, red and processed meats, fish, fruits and vegetables) were tested as potential confounders, but were excluded from final models for parsimony, as they did not affect the observed risk estimates (change-in-estimate <10%).
Potential effect modifications of the association between OPN levels and HCC risk by sex, age at recruitment, years of follow-up, baseline and lifetime alcohol consumption, and smoking status were evaluated in separate analyses by including interaction terms formed by the product of modifying variable categories and the values of OPN. The statistical models were adjusted for alcohol using a combination variable of alcohol intake at baseline (i.e. recruitment into the cohort) and alcohol drinking throughout life periods (at 20, 30, 40, 50 years of age). These data were derived from standardized/validated dietary and lifestyle questionnaires (17). Participants classified as never drinkers indicated no alcohol intake at baseline, and no past alcohol intake. Former drinkers indicated no alcohol intake at baseline, but did have past alcohol intake. Drinkers at recruitment indicated alcohol intake at baseline, but did not have past alcohol intake. Lifetime drinkers were defined as those who indicated alcohol intake at both baseline and prior. All the categories of alcohol exposures assessed are mutually exclusive.
Statistical significance of interactions (p<0.05) was assessed using likelihood ratio tests based on the models with and without the interaction terms. Sensitivity analyses were performed including additional adjustment and/or stratification by hepatitis status, AFP, BARD score, liver function tests, sex, years of follow-up and diabetes. P-values<0.05 were considered statistically significant. Analyses were performed using Stata version 11 (StataCorp, College Station, Texas) and R software, version 3.0.2 (R Foundation for Statistical Computing, Vienna, Austria).
Results
Participants Characteristics and Baseline Circulating Osteopontin Levels
Baseline characteristics of the study participants (Ncases = 100 and Ncontrols = 194) and p values for differences are presented in Table 1. HCC cases were diagnosed on average 4.8 (±2.9) years after recruitment and baseline blood collection. They were more likely to be men, and compared with controls, they were more likely to be current smokers, to have higher BMI and to have diabetes. They were also more likely to present at recruitment with higher alcohol intake and with chronic HBV or HCV infection. Baseline AFP levels and markers of liver function are also presented in Table 1. Compared to controls, HCC cases had higher levels of AFP (6.4 vs. 3.9 ng/ml), CRP (2 vs. 1 mg/l) and liver enzymes (ALT: 33 vs. 7 U/l; AST: 44.5 vs. 19 U/l; GGT: 87 vs. 22.5 U/l; ALP: 85 vs. 59 U/l). No difference in the ratio AST/ALT was observed. Overall, 42.0% of HCC cases had BARD scores of 3 or 4, predictive of severe fibrosis, compared to 25.3% in controls.
Table 1.
Characteristics of EPIC cohort subjects with incident HCC (Cases) and matched controls (Controls) selected for the nested case-control study.
| Baseline characteristics | HCC cases (n=100) | Matched controls (n=194) | p-value |
|---|---|---|---|
| Men, N (%) | 70 (70.0) | 136 (70.1) | matching criteria |
| Age at recruitment (y), mean (SD) | 60.6 (6.6) | 60.6 (6.7) | matching criteria |
| Follow-up from blood collection (y), mean (SD) | 4.8 (2.9) | -- | -- |
| Smoking status, N (%) | <0.001 | ||
| Never smoker | 25 (25.0) | 79 (40.7) | |
| Former smoker | 37 (37.0) | 83 (42.8) | |
| Current smoker | 36 (36.0) | 31 (16.0) | |
| With diabetes, N (%)a | 14 (14.0) | 10 (5.2) | 0.024 |
| Body Mass Index (kg/m2), mean (SD) | 27.9 (5.3) | 26.5 (3.6) | 0.004 |
| Physical activity, N (%)b | 0.230 | ||
| Inactive | 4 (4.0) | 24 (12.4) | |
| Moderately inactive | 31 (31.0) | 58 (30.0) | |
| Moderately active | 50 (50.0) | 87 (44.9) | |
| Active | 10 (10.0) | 18 (9.3) | |
| Lifetime pattern of alcohol intake, N (%) | <0.001 | ||
| Never drinkers | 10 (10.0) | 6 (3.1) | |
| Former drinkers | 13 (13.0) | 4 (2.1) | |
| Drinkers only at recruitment | 17 (17.0) | 43 (22.2) | |
| Lifetime drinkers | 60 (30.0) | 141 (72.7) | |
| Alcohol intake at recruitment (g/d), mean (SD) | 19.7 (28.1) | 15.2 (18.6) | 0.063 |
| Viral Hepatitis status, N (%) | |||
| Hepatitis B virus (HBV) positive | 12 (12.0) | 5 (2.6) | 0.001 |
| Hepatitis C virus (HCV) positive | 18 (18.0) | 4 (2.1) | <0.001 |
| HBV or HCV positive | 27 (27.0) | 8 (4.2) | <0.001 |
| Baseline serum biomarkers, median (5th–95th percentile) | |||
| α-fetoprotein (AFP), ng/ml | 6.4 (2.5–744.6) | 3.9 (1.9–9.0) | 0.014 |
| C reactive protein (CRP), mg/l | 2 (1–29.5) | 1 (1–7) | <0.001 |
| Liver function tests | |||
| Alanineaminotransferase (ALT), U/l | 33 (10–139.5) | 7 (9–45) | <0.001 |
| Aspartateaminotransferase (AST), U/l | 45 (15–147) | 19 (13–33) | <0.001 |
| Gamma-glutamyltransferase (GGT), U/l | 87 (13–705) | 23 (10–75) | <0.001 |
| Alkaline phosphatase (ALP), U/l | 85 (44–177.5) | 59 (38–100) | <0.001 |
| Albumin, g/l | 39 (31–46.5) | 42 (37–48) | <0.001 |
| Total bilirubin, μmol/l | 10 (4–33) | 8 (4–16) | <0.001 |
| AST/ALT ratio | 1.1 (0.6–2.5) | 1.1 (0.6–1.9) | 0.0214 |
| BARD score,N (%) | 0.002 | ||
| 0–1 | 19 (19.0) | 29 (15.0) | |
| 2 | 39 (39.0) | 116 (59.8) | |
| 3–4 | 42 (42.0) | 49 (25.3) | |
| Osteopontin (OPN), ng/ml | 67.4 (29.1–167.3) | 53.7 (27.1–93.6) | <0.001 |
SD, standard deviation. Missing values were not excluded from percentage calculations; therefore the sum of percent across subgroups may not add up to 100%. Categorical variables are presented as numbers and percentages; continuous variables are presented as mean and standard deviations. Case-control differences were assessed using Student’s paired t-test, Wilcoxon’s signed rank test or McNemar’s test where appropriate.
Self-reported data. Number of cases and controls with missing data on diabetes status = 24.
Total physical activity categories were sex-specific. Number of cases and controls with missing data on physical activity = 12.
OPN levels at baseline were significantly higher in HCC cases than in controls (67.4 vs. 53.7 ng/ml, p<0.0001) (Table 1 and Supplementary Figure S1). Spearman correlations between OPN levels and AFP, CRP or liver function tests among HCC cases and controls were calculated (Supplementary Table S1). Among controls, a significant negative correlation was observed between OPN and ALT (R=−0.21; p=0.004) or albumin (R=−0.37; p<0.0001). Among HCC cases, a positive correlation was observed between OPN and AFP (R=0.24; p=0.022), CRP (R=0.38; p<0.0001), AST (R=0.21; p =0.039), GGT (R=0.25; p=0.014) and ALP (R=0.36; p <0.0001) and a negative correlation was observed between OPN and albumin (R=−0.48; p<0.0001).
Association Between Circulating OPN Levels and HCC risk
A statistically significant positive association was observed between circulating OPN levels and HCC risk. In analyses by tertiles of OPN concentrations, a strong, positive dose-response association was observed between HCC risk and OPN levels; multivariable OR (ORmultivariable) was 3.87 [95% CI: 1.27–11.78] and 13.76 [95% CI: 4.21–44.98] for second (OPN: 49.1–58.6 ng/ml) and third (OPN: >58.6 ng/ml) tertiles vs. first (OPN: <49.1 ng/ml) tertile, respectively (p-trend<0.0001) (Table 2). Additionally, ORs for 10% increment in OPN level in crude and multivariable adjusted models were 1.33 [95% CI: 1.19–1.49] and 1.30 [95% CI: 1.14–1.48], respectively (Table 2). The association between circulating OPN levels and HCC risk was stronger than the association between AFP levels and HCC risk; although circulating AFP level at baseline was also associated with higher HCC risk when analysed continuously or in tertiles, ORmultivariable for 10% increment in AFP level was 1.17 [95% CI: 1.09–1.25] and ORsmultivariable for second and third tertiles vs. first tertile were 1.97 [95% CI: 0.72–5.41] and 9.97 [95% CI: 3.70–26.86], respectively (p-trend<0.0001) (Table 2). Finally, cubic spline representation showed that the association between OPN levels and HCC increased linearly when OPN level was above 47.15 ng/ml (Supplementary Figure S2).
Table 2.
Odds ratios and 95% confidence intervals for HCC by tertiles of circulating OPN and AFP levels in the EPIC nested case-control study.
| Tertiles | Continuously, | |||||
|---|---|---|---|---|---|---|
| 1 | 2 | 3 | Ptrend | per increasea | 10% | |
| OPN | ||||||
| Tertile range, (ng/ml) | <49.1 | 49.1–58.6 | >58.6 | |||
| No of cases/controls | 14/65 | 24/65 | 62/64 | |||
| Matching factors onlyb | 1.00 | 3.09 [1.17–8.13] | 12.26 [4.40–34.10] | <0.0001 | 1.33 [1.19–1.49] | |
| Multivariablec | 1.00 | 3.87 [1.27–11.78] | 13.76 [4.21–44.98] | <0.0001 | 1.30 [1.14–1.48] | |
| AFP | ||||||
| Tertile range, (ng/ml) | <3.3 | 3.3–4.6 | >4.6 | |||
| No of cases/controls | 9/67 | 15/63 | 76/64 | |||
| Matching factors onlyb | 1.00 | 2.02 [0.78–5.28] | 12.48 [4.87–32.02] | <0.0001 | 1.18 [1.11–1.25] | |
| Multivariablec | 1.00 | 1.97 [0.72–5.41] | 9.97 [3.70–26.86] | <0.0001 | 1.17 [1.09–1.25] | |
OPN and AFP levels correspond to a 10% increment after log transformation.
Odds ratios and 95% confidence intervals estimated by conditional logistic regression conditioned on the matching factors.
Additionally adjusted for body mass index (kg/m2, continuous), smoking status (never, former, current, unknown), baseline alcohol intake (g/d, continuous), and lifetime alcohol intake pattern (never drinkers, former drinkers, drinkers only at recruitment, lifetime drinkers, unknown).
In separate models, we evaluated potential interactions of the association between OPN levels and HCC risk by sex, age at recruitment, baseline and lifetime alcohol consumption and smoking status. We did not observe any statistically significant effect modifications (all P for interaction > 0.05). Additional adjustment for AFP, BARD score, AST/ALT ratio, liver function tests and HBV/HCV status did not alter the findings for OPN (Supplementary Table S2). The association between circulating OPN levels and HCC risk was stronger among men than women (ORmultivariable per 10% increase: 1.44 [95% CI: 1.19–1.74] and 1.07 [95% CI: 0.87–1.32], respectively) (Supplementary Table S2). The association between circulating OPN levels and HCC risk was also stronger for cases diagnosed during the first 2 years (n=21) or from 2 to 6 years (n=40) of follow-up (ORmultivariable: 2.51 [95% CI: 1.06–5.95] and 1.45 [95% CI: 1.13–1.85], respectively) compared to cases diagnosed after 6 years or more (n=39) of follow-up (ORmultivariable: 1.05 [95% CI: 0.89–1.24]) (Supplementary Table S2). However, the associations did not differ significantly by sex or years of follow-up (all P-values for heterogeneity>0.10). Models stratified by viral hepatitis status showed that while circulating OPN levels were significantly associated with higher HCC risk in both HBV/HCV positive and negative subjects, the association was stronger in HBV/HCV positive subjects (ncases=27; ORmultivariable: 2.45 [95% CI: 1.24–4.83]) than in negative subjects (ncases=70; 1.19 [95% CI: 1.05–1.34]) (Supplementary Table S2). Finally, the association between OPN levels and HCC risk did not change substantially after excluding participants with AFP levels ≥ 20 or ≥ 10 ng/ml and after exclusion of participants that self-reported type 2 diabetes at baseline (Supplementary Table S2).
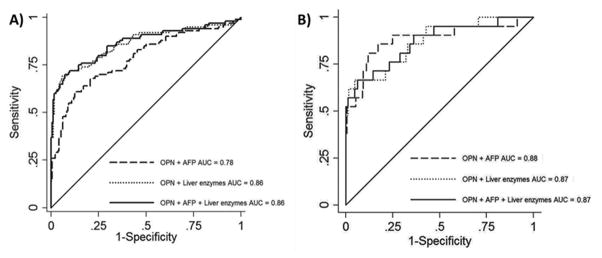
Diagnostic Performance of OPN for HCC Risk
Receiver operating characteristics (ROC) curves were constructed to evaluate OPN performance as a marker for HCC risk in all participants and among cases diagnosed within two years of follow-up. ROC curves were also used to assess whether the addition of AFP or liver enzymes AST, GGT and ALP improved the model. The performance of OPN alone or in combination with AFP or liver enzymes, in discriminating HCC cases from controls are presented in Figure 1. When including all HCC cases (Figure 1A), the AUC for OPN (0.71 [95% CI: 0.64–0.77] was lower than for AFP (0.76 [95% CI: 0.70–0.82]) or for liver enzymes GGT, ALP and AST (0.84 [95% CI: 0.78–0.89]). AUC increased to 0.86 [95% CI: 0.81–0.91] when both liver enzymes and OPN were included in the model and further addition of AFP did not improve the performance. To further validate the performance of OPN alone or in combination with AFP and liver enzymes, we performed a 5-fold cross-validation analysis. The average from 5 runs showed similar AUC averages on classifier calibration and classifier validation (Supplementary Table S3). At 90% specificity, sensitivity was 72% for the model with OPN and liver enzymes in detecting HCC.
Fig. 1. Discriminatory accuracy of the models for predicting the development of HCC.
Receiver operating characteristics (ROC) curves for OPN, AFP and liver enzymes in the diagnosis of hepatocellular carcinoma in the EPIC nested case-control study in (A) all cases (HCC cases=100) and (B) in cases diagnosed during the first 2 years of follow-up (HCC cases=21). The area under the curve (AUC) is shown with 95% CIs.
When OPN performance was evaluated specifically for HCC cases diagnosed during the first 2 years of follow-up (Figure 1B), the AUC for OPN (0.82 [95% CI: 0.72–0.91]) was higher than for AFP (0.79 [95% CI: 0.67–0.92] or for liver enzymes (0.79 [95% CI: 0.66–0.92]), respectively). AUC increased to 0.88 [95% CI: 0.78–0.98] when OPN and AFP were combined in the model. Similarly, when OPN and liver enzymes were combined in the model, the AUC increased to 0.87 [95% CI: 0.78–0.96]. However, a combination of OPN, AFP and liver enzymes did not improve the performance (AUC=0.87 [95% CI: 0.77–0.96]). At 85% specificity, sensitivity was 85% for the model with OPN and AFP in detecting HCC within 2 years of HCC diagnosis.
Discussion
In this study, we observed a statistically significant positive association between plasma OPN levels and risk of first incident HCC. The results were stronger among cases diagnosed during the first years of follow-up, and did not change substantially after excluding hepatitis positive participants, or after adjustment for biomarkers of liver function. Also, among cases diagnosed during the first two years of follow-up, OPN alone or in combination with AFP showed better diagnostic performance of HCC compared to AFP alone.
Most HCC cases are diagnosed at a late stage when curative treatments are not applicable. A recent multi-regional retrospective study showed that survival from first HCC treatment varied significantly by region, with median overall survival of 60, 33, 31, 24 and 23 months for Japan, North America, South Korea, Europe and China, respectively (P<0.0001), underscoring the need for earlier HCC diagnosis worldwide (23). Given the rising incidence of this cancer in developed countries, it is critically important to identify those at high risk for HCC and institute effective surveillance strategies for early diagnosis. HCC is a cancer well suited for screening given its occurrence in identifiable high risk populations such as patients with liver cirrhosis or chronic HBV infection status. While surveillance for HCC in patients with cirrhosis is recommended, the uptake of HCC surveillance by the medical community has been poor. Better assessment of an individual’s risk of HCC could help clinicians increase adherence to screening programs. Most prediction models for HCC have been developed in high risk groups such as patients with liver cirrhosis or chronic HBV or HCV infection (24–32) and most models included age and levels of transaminases. Only two studies on HCC risk prediction models have been performed on the general population and both of them were performed in large cohorts from Taiwan (33, 34).
In the first Taiwanese population cohort study, transaminase levels were shown to be predictive of HCC development within 10 years independently of known HCV or HBV infection status (33). In that cohort the average of follow-up for HCC incidence was 8.5 years. In the second Taiwanese population cohort study, family history of HCC and cumulative smoking improved a model based on transaminases alone (34). All these models, whether they were developed on high risk groups or in general populations, used only a combination of readily available parameters and liver function tests such as liver transaminase or albumin. Our study is the first to include a novel HCC biomarker. While we also found that liver function tests indicative of liver injury, could predict HCC development in the EPIC cohort independently of HCV or HBV infection status, we showed that a model based on liver function can be moderately improved by the addition of OPN. We have previously identified OPN as an early stage HCC biomarker in patients with liver cirrhosis or chronic hepatitis and showed that OPN is already elevated a year prior to diagnosis (8). We also reported that OPN and AFP are complementary for the detection of HCC. In the EPIC pre-diagnosis samples, addition of AFP did not further improve the OPN-based prediction model.
Most remarkably, the performance and the composition of the OPN prediction model changed in relation to time to HCC diagnosis. Within two years of diagnosis, the combination of OPN and AFP best predicted HCC development and liver function tests did not improve the model, suggesting that measuring OPN and AFP could identify high risk groups independently of a cirrhosis diagnosis. In most studies, the clinical utility of HCC risk models has not been evaluated. At the population level, an ideal model is an easy-to-use model that should encourage at-risk people to be screened. Information provided by the OPN-AFP prediction model could allow the clinician to identify patients at high risk of developing HCC within two years and requiring HCC surveillance with imaging modalities such as MRI or CT that are highly sensitive for the detection of small HCCs.
OPN is a secreted non-collagenous, matrix glycoprotein, implicated in the progression of fibrosis and cancer and an influential factor in the tumor microenvironment (35,36). In the liver, OPN has been shown to modulate regeneration, inflammation and fibrosis and more recently, to induce dedifferentiation of hepatocytes (37,38). Our group has also shown that OPN is necessary for the survival of CD24+ liver progenitor cells (39). Both dedifferentiation of hepatocytes and accumulation of CD24+ cells have been proposed as early events in HCC tumor initiation (40,41). The effect of OPN on hepatocyte dedifferentiation and accumulation of liver progenitor cells is also in agreement with the observed negative correlation between OPN and albumin, a marker of mature hepatocytes.
A strength of our study is its reliance on a prospective cohort design which allowed the estimation of OPN concentrations prior to cancer diagnosis, and the coverage of several European countries with variable prevalence patterns of exposures relevant to HCC risk. Other strengths of the study include the use of a uniform protocol and the centralized laboratory determinations of markers of HBV/HCV infections and liver function markers. The study has however several limitations. While the sample size can be considered adequate for a cohort study in Caucasians, among whom HCC is a relatively rare tumor, the study suffers from small sample size when focusing on subgroups. This is particularly the case for the analysis of OPN performance within 2 years prior to HCC diagnosis. The comparative estimation of HCC risk by OPN between subgroups, such as men and women, may also not reach statistical significance due to the small sample size. Another limitation of this study is the lack of information on the presence of fibrosis, cirrhosis or other chronic liver diseases. Although we were able to adjust for a number of important risk factors, liver function markers, and hepatitis infection status, the presence of possible residual confounding may not be ruled out.
In conclusion, this study has shown that higher pre-diagnostic OPN levels in plasma is associated with higher risk of first incident HCC among Europeans. Assessment of the risk of HCC development is essential for formulating personalized surveillance or for prevention strategies. We identified simple models using OPN circulating levels, for the identification of patients at high risk of developing HCC and for use as a decision rule for clinical action. Because these models are independent of known risk factor for HCC, they could have utility in assessing individual annual risk of developing HCC in subjects previously thought to be at low or average risk because of unknown risk factors or undiagnosed cirrhosis. Large prospective studies, and studies in other populations, are needed to further optimize the model in relation to time of diagnosis and to evaluate its utility as a decision rule for clinical action.
Supplementary Material
Acknowledgments
Financial Support: This work was supported by NIH R01 CA120719 to LB and by the French National Cancer Institute (Institut National du Cancer; INCA) grant number 2009-139 to MJ. The coordination of EPIC is financially supported by the European Commission (DG-SANCO); and the International Agency for Research on Cancer. The national cohorts are supported by Danish Cancer Society (Denmark); Ligue Contre le Cancer; Institut Gustave Roussy; Mutuelle Générale de l’Education Nationale; and Institut National de la Santé et de la Recherche Médicale (INSERM) (France); Deutsche Krebshilfe, Deutsches Krebsforschungszentrum (DKFZ); and Federal Ministry of Education and Research (Germany); Hellenic Health Foundation (Greece); Italian Association for Research on Cancer (AIRC); National Research Council; and AIRE-ONLUS Ragusa, AVIS Ragusa, Sicilian Government (Italy); Dutch Ministry of Public Health, Welfare and Sports (VWS); Netherlands Cancer Registry (NKR); LK Research Funds; Dutch Prevention Funds; Dutch ZON (Zorg Onderzoek Nederland); World Cancer Research Fund (WCRF); and Statistics Netherlands (the Netherlands); European Research Council (ERC) (grant number ERC-2009-AdG 232997) and Nordforsk; and Nordic Center of Excellence Programme on Food, Nutrition and Health (Norway); Health Research Fund (FIS); Regional Governments of Andalucía, Asturias, Basque Country, Murcia (No. 6236) and Navarra; and ISCIII RETIC (RD06/0020) (Spain); Swedish Cancer Society; Swedish Scientific Council; and Regional Government of Skåne and Västerbotten (Sweden); Cancer Research UK; Medical Research Council; Stroke Association; British Heart Foundation; Department of Health; Food Standards Agency; and Wellcome Trust (UK). Reagents for the hepatitis infection determinations were kindly provided by Abbott Diagnostics Division, Lyon, France.
Abbreviations
- HCC
hepatocellular carcinoma
- HBV
hepatitis B virus
- HCV
hepatitis C virus
- AFP
α-fetoprotein
- OPN
osteopontin
- EPIC
European Prospective Investigation into Cancer and Nutrition
- IARC
International Agency for Research on Cancer
- CRP
C-reactive protein
- ALT
alanine aminotransferase
- AST
aspartate aminotransferase
- GGT
gamma-glutamyl transferase
- ALP
alkaline phosphatase
- AUC
area under the curve
- BMI
Body mass index
- OR
Odds Ratio
- CI
confidence interval
- ROC
receiver operating characteristics curves
Footnotes
Conflict of interest: None declared.
References
- 1.Ferlay J, SI, Ervik M, Dikshit R, Eser S, Mathers C, Rebelo M, Parkin DM, Forman D, Bray F. Cancer Incidence and Mortality Worldwide: IARC CancerBase No. 11. Globocan. 2013 doi: 10.1002/ijc.29210. Internet. cited 1.0 September 17, 2015; Available from: http://globocan.iarc.fr. [DOI] [PubMed]
- 2.Jemal A, Bray F, Center MM, Ferlay J, Ward E, Forman D. Global cancer statistics. CA: a cancer journal for clinicians. 2011;61:69–90. doi: 10.3322/caac.20107. [DOI] [PubMed] [Google Scholar]
- 3.El-Serag HB. Hepatocellular carcinoma. N Engl J Med. 2011;365:1118–27. doi: 10.1056/NEJMra1001683. [DOI] [PubMed] [Google Scholar]
- 4.Bosetti C, Turati F, La Vecchia C. Hepatocellular carcinoma epidemiology. Best Pract Res Clin Gastroenterol. 2014;28:753–70. doi: 10.1016/j.bpg.2014.08.007. [DOI] [PubMed] [Google Scholar]
- 5.Michelotti GA, Machado MV, Diehl AM. NAFLD, NASH and liver cancer. Nature reviews Gastroenterology & hepatology. 2013;10:656–65. doi: 10.1038/nrgastro.2013.183. [DOI] [PubMed] [Google Scholar]
- 6.Singal AG, Conjeevaram HS, Volk ML, Fu S, Fontana RJ, Askari F, et al. Effectiveness of hepatocellular carcinoma surveillance in patients with cirrhosis. Cancer Epidemiol Biomarkers Prev. 2012;21:793–9. doi: 10.1158/1055-9965.EPI-11-1005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.van Meer S, de Man RA, Siersema PD, van Erpecum KJ. Surveillance for hepatocellular carcinoma in chronic liver disease: evidence and controversies. World journal of gastroenterology : WJG. 2013;19:6744–56. doi: 10.3748/wjg.v19.i40.6744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Shang S, Plymoth A, Ge S, Feng Z, Rosen HR, Sangrajrang S, et al. Identification of osteopontin as a novel marker for early hepatocellular carcinoma. Hepatology. 2012;55:483–90. doi: 10.1002/hep.24703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.da Costa AN, Plymoth A, Santos-Silva D, Ortiz-Cuaran S, Camey S, Guilloreau P, et al. Osteopontin and latent-TGF beta binding-protein 2 as potential diagnostic markers for HBV-related hepatocellular carcinoma. International journal of cancer Journal international du cancer. 2015;136:172–81. doi: 10.1002/ijc.28953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nabih MI, Aref WM, Fathy MM. Significance of plasma osteopontin in diagnosis of hepatitis C virus-related hepatocellular carcinoma. Arab journal of gastroenterology : the official publication of the Pan-Arab Association of Gastroenterology. 2014;15:103–7. doi: 10.1016/j.ajg.2014.08.002. [DOI] [PubMed] [Google Scholar]
- 11.Wan HG, Xu H, Gu YM, Wang H, Xu W, Zu MH. Comparison osteopontin vs AFP for the diagnosis of HCC: a meta-analysis. Clinics and research in hepatology and gastroenterology. 2014;38:706–14. doi: 10.1016/j.clinre.2014.06.008. [DOI] [PubMed] [Google Scholar]
- 12.Ge T, Shen Q, Wang N, Zhang Y, Ge Z, Chu W, et al. Diagnostic values of alpha-fetoprotein, dickkopf-1, and osteopontin for hepatocellular carcinoma. Medical oncology. 2015;32:59. doi: 10.1007/s12032-014-0367-z. [DOI] [PubMed] [Google Scholar]
- 13.Rittling SR, Chambers AF. Role of osteopontin in tumour progression. Br J Cancer. 2004;90:1877–81. doi: 10.1038/sj.bjc.6601839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chakraborty G, Jain S, Behera R, Ahmed M, Sharma P, Kumar V, et al. The multifaceted roles of osteopontin in cell signaling, tumor progression and angiogenesis. Current molecular medicine. 2006;6:819–30. doi: 10.2174/156652406779010803. [DOI] [PubMed] [Google Scholar]
- 15.Weber GF, Lett GS, Haubein NC. Osteopontin is a marker for cancer aggressiveness and patient survival. Br J Cancer. 2010;103:861–9. doi: 10.1038/sj.bjc.6605834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zhang CH, Xu GL, Jia WD, Ge YS, Li JS, Ma JL, et al. Prognostic significance of osteopontin in hepatocellular carcinoma: a meta-analysis. International journal of cancer Journal international du cancer. 2012;130:2685–92. doi: 10.1002/ijc.26301. [DOI] [PubMed] [Google Scholar]
- 17.Riboli E, Kaaks R. The EPIC Project: rationale and study design. European Prospective Investigation into Cancer and Nutrition. International journal of epidemiology. 1997;26(Suppl 1):S6–14. doi: 10.1093/ije/26.suppl_1.s6. [DOI] [PubMed] [Google Scholar]
- 18.Riboli E, Hunt KJ, Slimani N, Ferrari P, Norat T, Fahey M, et al. European Prospective Investigation into Cancer and Nutrition (EPIC): study populations and data collection. Public health nutrition. 2002;5:1113–24. doi: 10.1079/PHN2002394. [DOI] [PubMed] [Google Scholar]
- 19.Trichopoulos D, Bamia C, Lagiou P, Fedirko V, Trepo E, Jenab M, et al. Hepatocellular carcinoma risk factors and disease burden in a European cohort: a nested case-control study. J Natl Cancer Inst. 2011;103:1686–95. doi: 10.1093/jnci/djr395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Fedirko V, Lukanova A, Bamia C, Trichopolou A, Trepo E, Nothlings U, et al. Glycemic index, glycemic load, dietary carbohydrate, and dietary fiber intake and risk of liver and biliary tract cancers in Western Europeans. Annals of oncology : official journal of the European Society for Medical Oncology / ESMO. 2013;24:543–53. doi: 10.1093/annonc/mds434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Fedirko V, Duarte-Salles T, Bamia C, Trichopoulou A, Aleksandrova K, Trichopoulos D, et al. Prediagnostic circulating vitamin D levels and risk of hepatocellular carcinoma in European populations: a nested case-control study. Hepatology. 2014;60:1222–30. doi: 10.1002/hep.27079. [DOI] [PubMed] [Google Scholar]
- 22.Harrison SA, Oliver D, Arnold HL, Gogia S, Neuschwander-Tetri BA. Development and validation of a simple NAFLD clinical scoring system for identifying patients without advanced disease. Gut. 2008;57:1441–7. doi: 10.1136/gut.2007.146019. [DOI] [PubMed] [Google Scholar]
- 23.Park JW, Chen M, Colombo M, Roberts LR, Schwartz M, Chen PJ, et al. Global patterns of hepatocellular carcinoma management from diagnosis to death: the BRIDGE Study. Liver Int. 2015;35:2155–66. doi: 10.1111/liv.12818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Yuen MF, Tanaka Y, Fong DY, Fung J, Wong DK, Yuen JC, et al. Independent risk factors and predictive score for the development of hepatocellular carcinoma in chronic hepatitis B. Journal of hepatology. 2009;50:80–8. doi: 10.1016/j.jhep.2008.07.023. [DOI] [PubMed] [Google Scholar]
- 25.Lok AS, Seeff LB, Morgan TR, di Bisceglie AM, Sterling RK, Curto TM, et al. Incidence of hepatocellular carcinoma and associated risk factors in hepatitis C-related advanced liver disease. Gastroenterology. 2009;136:138–48. doi: 10.1053/j.gastro.2008.09.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Yang HI, Yuen MF, Chan HL, Han KH, Chen PJ, Kim DY, et al. Risk estimation for hepatocellular carcinoma in chronic hepatitis B (REACH-B): development and validation of a predictive score. The lancet oncology. 2011;12:568–74. doi: 10.1016/S1470-2045(11)70077-8. [DOI] [PubMed] [Google Scholar]
- 27.Michikawa T, Inoue M, Sawada N, Iwasaki M, Tanaka Y, Shimazu T, et al. Development of a prediction model for 10-year risk of hepatocellular carcinoma in middle-aged Japanese: the Japan Public Health Center-based Prospective Study Cohort II. Preventive medicine. 2012;55:137–43. doi: 10.1016/j.ypmed.2012.05.017. [DOI] [PubMed] [Google Scholar]
- 28.Kurosaki M, Hiramatsu N, Sakamoto M, Suzuki Y, Iwasaki M, Tamori A, et al. Data mining model using simple and readily available factors could identify patients at high risk for hepatocellular carcinoma in chronic hepatitis C. Journal of hepatology. 2012;56:602–8. doi: 10.1016/j.jhep.2011.09.011. [DOI] [PubMed] [Google Scholar]
- 29.Lee MH, Yang HI, Liu J, Batrla-Utermann R, Jen CL, Iloeje UH, et al. Prediction models of long-term cirrhosis and hepatocellular carcinoma risk in chronic hepatitis B patients: risk scores integrating host and virus profiles. Hepatology. 2013;58:546–54. doi: 10.1002/hep.26385. [DOI] [PubMed] [Google Scholar]
- 30.Lee MH, Lu SN, Yuan Y, Yang HI, Jen CL, You SL, et al. Development and validation of a clinical scoring system for predicting risk of HCC in asymptomatic individuals seropositive for anti-HCV antibodies. PLoS One. 2014;9:e94760. doi: 10.1371/journal.pone.0094760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Flemming JA, Yang JD, Vittinghoff E, Kim WR, Terrault NA. Risk prediction of hepatocellular carcinoma in patients with cirrhosis: the ADRESS-HCC risk model. Cancer. 2014;120:3485–93. doi: 10.1002/cncr.28832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.El-Serag HB, Kanwal F, Davila JA, Kramer J, Richardson P. A new laboratory-based algorithm to predict development of hepatocellular carcinoma in patients with hepatitis C and cirrhosis. Gastroenterology. 2014;146:1249–55. e1. doi: 10.1053/j.gastro.2014.01.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wen CP, Lin J, Yang YC, Tsai MK, Tsao CK, Etzel C, et al. Hepatocellular carcinoma risk prediction model for the general population: the predictive power of transaminases. J Natl Cancer Inst. 2012;104:1599–611. doi: 10.1093/jnci/djs372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hung YC, Lin CL, Liu CJ, Hung H, Lin SM, Lee SD, et al. Development of risk scoring system for stratifying population for hepatocellular carcinoma screening. Hepatology. 2015;61:1934–44. doi: 10.1002/hep.27610. [DOI] [PubMed] [Google Scholar]
- 35.Kothari AN, Arffa ML, Chang V, Blackwell RH, Syn WK, Zhang J, et al. Osteopontin-A master regulator of epithelial-mesenchymal transition. J Clin Med. 2016 doi: 10.3390/jcm5040039. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Shevde LA, Samant RS. Role of osteopontin in the pathophysiology of cancer. Matrix Biology. 2014;37:131–41. doi: 10.1016/j.matbio.2014.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Nagoshi S. Osteopontin: Versatile modulator of liver diseases. Hepatol Res. 2014;44:22–30. doi: 10.1111/hepr.12166. [DOI] [PubMed] [Google Scholar]
- 38.Yovchey MI, Locker J, Oertel M. Biliary fibrosis drives liver repopulation and phenotype transition of transplanted hepatocytes. J Hepatol. 2016 doi: 10.1016/j.jhep.2016.01.036. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Zhang J, Jiao J, Cermelli S, Muir K, Jung KH, Zou R, et al. miR-21 inhibition reduces liver fibrosis and prevents tumor development by inducing apoptosis of CD24+ progenitor cells. Cancer Res. 2015;75:1859–67. doi: 10.1158/0008-5472.CAN-14-1254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Mu X, Espanol-Suner R, Mederacke I, Affò S, Manco R, Sempoux C, et al. Hepatocellular carcinoma originates from hepatocytes and not from the progenitor/biliary compartment. J Clin Invest. 2015;125:3891–903. doi: 10.1172/JCI77995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Lee TK, Castilho A, Cheung VC, Tang KH, Ma S, Ng IO. CD24(+) liver tumor-initiating cells drive self-renewal and tumor initiation through STAT3-mediated NANOG regulation. Cell Stem Cell. 2011;9:50–63. doi: 10.1016/j.stem.2011.06.005. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.