Abstract
Cetuximab, an antibody against the Epidermal Growth Factor Receptor (EGFR) has shown efficacy in treating head and neck squamous cell carcinoma (HNSCC), metastatic colorectal cancer and non-small cell lung cancer (NSCLC). Despite the clinical success of cetuximab, many patients do not respond to cetuximab. Furthermore, virtually all patients who do initially respond become refractory, highlighting both intrinsic and acquired resistance to cetuximab as significant clinical problems. To understand mechanistically how cancerous cells acquire resistance, we previously developed models of acquired resistance using the H226 NSCLC and UM-SCC1 HNSCC cell lines. Cetuximab-resistant clones showed a robust upregulation and dependency on the HER family receptors EGFR, HER2 and HER3. Here, we examined Pan-HER, a mixture of six antibodies targeting these receptors on cetuximab-resistant clones. In cells exhibiting acquired or intrinsic resistance to cetuximab, Pan-HER treatment decreased all three receptors’ protein levels and down-stream activation of AKT and MAPK. This correlated with decreased cell proliferation in cetuximab-resistant clones. To determine whether Pan-HER had a therapeutic benefit in vivo, we established de novo cetuximab-resistant mouse xenografts and treated resistant tumors with Pan-HER. This regimen resulted in a superior growth delay of cetuximab-resistant xenografts compared to mice continued on cetuximab. Furthermore, intrinsically cetuximab-resistant HNSCC patient-derived xenograft tumors treated with Pan-HER exhibited significant growth delay compared to vehicle/cetuximab controls. These results suggest that targeting HER family receptors simultaneously with Pan-HER is a promising treatment strategy for tumors displaying intrinsic or acquired resistance to cetuximab.
Keywords: HER family, Pan-HER, antibody mixture, resistance to cetuximab
Introduction
The HER family of receptor tyrosine kinases (RTK) play a prominent role in cell physiology, development, and cancer pathophysiology. This family consists of four members: EGFR, HER2, HER3, and HER4. These receptors are activated on the cell membrane by the binding of specific ligands, which leads to receptor homo- and hetero-dimerization with other HER family members. Dimerization of HER family receptors results in the activation of each receptor’s tyrosine kinases, and subsequently the activation of multiple downstream effector molecules (1, 2). Specifically, EGFR regulates the MAPK and PI3K/AKT signaling pathways, both of which have been associated with increased cellular proliferation, survival, angiogenesis, and invasion (3).
Overexpression or activation of the EGFR has been linked to poor prognosis in several cancers including metastatic colorectal cancer (mCRC), head and neck squamous cell carcinoma (HNSCC), non-small cell lung cancer (NSCLC), and brain cancer (4–6). Therefore, EGFR has been pursued as a molecular target over the last three decades in many cancer treatment strategies. One approach uses monoclonal antibodies (mAbs) to target the extracellular domain of the EGFR to block natural ligand binding. Cetuximab (ICM-225, Erbitux) is a human:murine chimeric mAb that binds to the EGFR. Cetuximab is approved for treatment of patients with mCRC and HNSCC (7, 8), and more recent reports have indicated that it may additionally have clinical applications in the treatment of NSCLC (9, 10). Unfortunately, clinical data suggests that the majority of patients who initially respond to cetuximab eventually acquire resistance (11, 12).
To understand the mechanisms of acquired resistance to cetuximab, we developed models of cetuximab-resistance by treating the cetuximab-sensitive NSCLC line H226 and HNSCC line UM-SCC1 with increasing concentrations of cetuximab until single cell resistant clones emerged (13). Detailed exploration of these model systems revealed that cetuximab-resistant clones have increased steady-state expression and activation of HER family receptors (EGFR, HER2, and HER3) due to impaired internalization and degradation (13). It was also demonstrated that the activation of HER3 is dependent upon activation of EGFR and HER2, and this promotes survival in cetuximab-resistant clones (13).
In accordance with shown HER family interdependency, it has also been demonstrated that targeting both the EGFR (with cetuximab) and the HER3 (with U3-1287) signaling axes is necessary to achieve a significant anti-tumor response in tumors refractory to cetuximab therapy (14). This indicates the importance of inhibiting more than one HER family receptor to maximally block the signaling network emanating from the HER family (14). Similar patterns of HER family interdependency have also been demonstrated in studies of combination antibody therapies for other cancers and found to elicit anti-tumor response. Acquired resistance to trastuzumab in breast cancer cell lines was correlated with increased expression levels of EGFR and HER3. These cells could be sensitized with combined treatment of gefitinib and cetuximab or U3-1287 (15). Yonesaka et al. demonstrated that subsequent depletion of HER2 in resistant A431 cells restored sensitivity to cetuximab (16). Extensive preclinical studies and initial clinical data also demonstrated that combination inhibitory EGFR and HER2 mAbs had additive or even synergistic antitumor activity (review see (17, 18)). Collectively, these findings suggest that molecular therapeutics only targeting one receptor may not have suitable anti-tumor effect, rather, a combination antibody against multiple receptors is necessary.
These findings have led to the development of therapeutics that target multiple members of the HER family. Pan-HER is a mixture of six monoclonal antibodies targeting EGFR, HER2 and HER3 (19). In this study, we hypothesized that NSCLC and HNSCC cell-based models and tumors with intrinsic or acquired cetuximab-resistance may have extensive response to Pan-HER. We found that proliferation in both intrinsic and acquired cetuximab-resistant NSCLC and HNSCC cells was effectively inhibited by Pan-HER treatment. In addition, consistent attenuation of downstream signaling of both cellular proliferation and survival pathways was observed. Analysis of Pan-HER treated acquired cetuximab-resistant NSCLC xenograft tumors as well as intrinsically cetuximab-resistant HNSCC PDX tumors showed reduction of EGFR, HER2, and HER3 expression with tumor growth delay. These observations suggest that using Pan-HER may be an effective approach for overcoming both intrinsic and acquired resistance to cetuximab.
Materials and Methods
Cell Lines
The human NSCLC cell line H226 was provided by Drs J. Minna and A. Gazdar (University of Texas Southwestern Medical School, Dallas, TX). The human NSCLC cell line H358 was purchased from ATCC. The H226 and H358 cells were maintained in 10% FBS in RPMI-1640 (Mediatech, Inc, Manassas, VA) with 1% penicillin and streptomycin. The HNSCC cell lines UM-SCC1, UM-SCC6, UM-SCC4 and UM-SCC11A were provided by Dr. Thomas E. Carey (University of Michigan, Ann Harbor, MI) and maintained in 10% FBS in Dulbecco’s Modified Eagle Medium (DMEM) with 1% penicillin and streptomycin. The development of cetuximab-resistant cells has been previously described (13, 20, 21). The authenticity of these cell lines was regularly verified on the basis of cell morphology and genomic short tandem repeat (STR) profile of each cell line. All cell lines were tested for authenticity in accordance with ATCC guidelines 4 to 6 months prior to the initiation of our investigation.
Materials
Cetuximab (IMC-225, Erbitux) was purchased from the University of Wisconsin Pharmacy. Pan-HER was generously provided by Symphogen A/S (Ballerup, Denmark).
Antibodies
All antibodies were purchased from commercial sources as indicated below: EGFR, HER2, HER3, and HRP-conjugated goat anti-rabbit IgG and goat anti-mouse IgG were obtained from Santa Cruz Biotechnology, Inc (Dallas, TX). pMAPK (T202/Y204), pAKT(S473), AKT, p-rpS6 (S235/236), rpS6, and Ki67 were obtained from Cell Signaling Technology (Danvers, MA). α-Tubulin was purchased from Calbiochem (Billerica, MA).
Cell Proliferation Assay
This assay was performed as previously described (22). All treatments were performed in quadruplicate.
Immunoblot Analysis
Whole-cell protein lysate was obtained using Tween-20 lysis buffer (50 mM Hepes, pH 7.4, 150 mM NaCl, 0.1% Tween-20, 10% glycerol, 2.5 mM EGTA, 1 mM EDTA, 1 mM DTT, 1 mM Na3VO4, 1 mM PMSF, 1 mM beta-glycerophosphate (BGP), and 10 μg/ml leupeptin and aprotinin). Immunoblot analysis was conducted as previously described (14).
Bromodeoxyuridine (BrdU) Cell Cycle Distribution Analysis
Cells were plated at a density of 800,000 per 100 mm2 plate and allowed to adhere overnight. The cells were treated with vehicle, 20 μg/ml cetuximab, or 20 μg/ml Pan-HER for 24 hours. BrdU cell distribution analysis was performed as previously described (20).
Mouse Xenograft Model and Patient-Derived Xenograft (PDX)
Athymic nude mice (4- to 6-week-old males or females) were obtained from Harlan Laboratories. All animal procedures and maintenance were conducted in accordance with the institutional guidelines of the University of Wisconsin. Mice were randomized into treatment or control groups. H226 or UW-SCC1 cells were injected in the dorsal flank of the mouse at respective day 0 (2 x 106 cells). Once tumors reached 200 mm3, mice were started on their respective treatments (IgG, cetuximab, Pan-HER). The dose of cetuximab and Pan-HER for the experiment was 50 mg/kg and twice a week by i.p. injection. Tumor volume measurements were evaluated by digital calipers and calculated by the formula (p)/6 x (large diameter) x (small diameter)2. The patient-derived xenograft (PDX) model was established as previously described (23).
Mouse Cetuximab-Resistant Human Tumor Xenografts
Mice were injected with H226 (2 x 106 cells), and tumors were allowed to grow to 100 mm3. All mice were randomized to treatment or control groups and treated with 50 mg/kg of either cetuximab or IgG i.p. twice weekly. Tumors were monitored for cetuximab resistance that was defined as marked tumor growth in the presence of continued cetuximab therapy. Once cetuximab-resistant tumors reached a volume of ~800 mm3, mice were grouped according to similar time points of resistance. At this point, each mouse was treated with either cetuximab or Pan-HER (50 mg/kg) i.p. twice weekly. Tumor volume measurements were evaluated by digital calipers and calculated by the formula (p)/6 x (large diameter) x (small diameter)2.
Mouse Tumor Collection and Protein Isolation
Tumors were collected 24 hours after the last cetuximab or Pan-HER treatment. Details of tumor collection and protein isolation were described previously (20). Protein quantitation and immunoblot analysis were performed as stated above.
Immunohistochemistry
Tumor tissue samples were collected from xenograft tumors, fixed in 10% neutral buffered formalin, paraffin-embedded, and cut into sections. The sections were heated in 10 mM citrate buffer (pH 6.0) for EGFR, HER2, and Ki67 or in EDTA buffer (pH 8.0) for HER3 with a Decloaking Chamber. Samples were incubated with rabbit anti-EGFR (Abcam; ab52894, 1:200), anti-HER2 (Cell Signaling; cs4290, 1:200), anti-HER3 (Cell Signaling; cs12708, 1:50), or anti-Ki67 (Cell Signaling; cs9027, 1:800). Sections were stained by VECTASTAIN universal kit/HRP (Vector Lab, Burlingame, CA). Antibody binding was revealed by addition of 3,3′-diaminobenzidine substrate. Tissues were counterstained with Mayer’s hematoxylin (Thermo Fisher Scientific, Waltham, MA) and were examined using an Olympus BX51 microscope.
Statistical Analysis
Student’s t-test was used to calculate the statistical significance of values provided by the different assay as described above. A p-value ≤0.05 was considered as statistically significant. Paired t-test analysis was performed for in vivo study and P≤0.01 was considered significant at the 99% confidence level as shown by the asterisks (**).
Results
Pan-HER Inhibits Proliferation of Cetuximab-Resistant NSCLC Clones
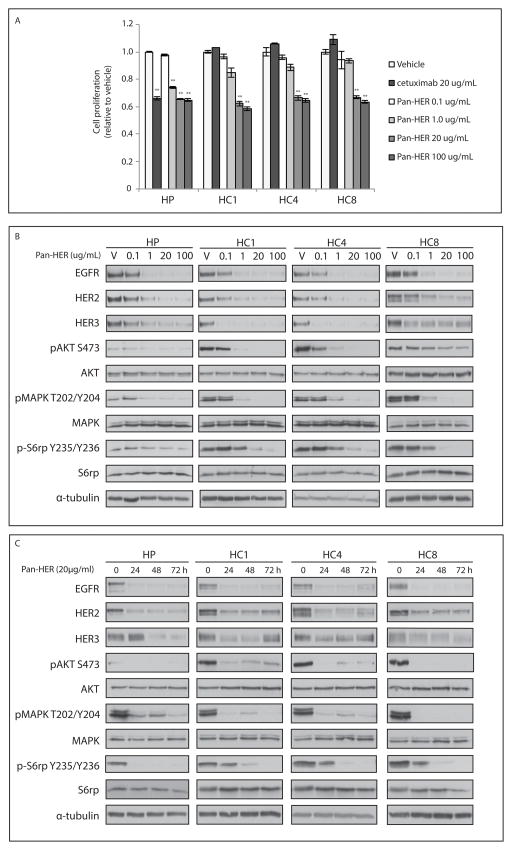
We previously reported the development of a model of acquired cetuximab resistance using the cell line H226. Analysis of individual clones with acquired resistance to cetuximab (HC1, HC4, and HC8) indicated increased expression, activity and dependency of the HER family relative to the cetuximab-sensitive parental control (HP) (13, 14). We have also demonstrated that EGFR has increased association with HER2 and HER3. Simultaneous inhibition of EGFR and HER2 decreased of HER3 activation as well as inhibited cell proliferation (13). Furthermore, dual knockdown of EGFR and HER3 by siRNA led to potent anti-proliferative effects in cetuximab-resistant clones (14). From these results, we hypothesized that Pan-HER, a mixture of six antibodies targeting each of EGFR, HER2, and HER3, would provide an anti-proliferative response in cetuximab-resistant clones. Cell proliferation analysis was performed after treatment with either cetuximab or with increasing concentrations of Pan-HER for 72 hours (Figure 1A). All cetuximab-resistant clones demonstrated statistically significant and dose-dependent growth inhibition upon treatment with Pan-HER. Treatment with 20 μg/mL Pan-HER reduced proliferation rate by ~40% compared to the vehicle control. To determine the efficacy of Pan-HER on targeting the HER family of receptors, cetuximab-resistant clones were treated with Pan-HER (0.1, 1, 20, 100 μg/ml) for 24 hours and the expression levels of HER family receptors were examined. Total protein levels of EGFR, HER2, and HER3 were effectively decreased by Pan-HER treatment at concentrations from 1 μg/ml in all cetuximab-resistant clones tested (Figure 1B). In addition, phosphorylation levels of AKT, S6rp, and MAPK were robustly decreased with increasing doses of Pan-HER. In a time course experiment, cetuximab-resistant clones were treated with Pan-HER (20 μg/mL) for 24, 48, or 72 hours (Figure 1C). The expression levels of HER family receptors were down-modulated by Pan-HER as early as 24 hours after treatment onset, with maintained down regulation observed out to the 72 hour time point. Overall, these findings indicated that Pan-HER can 1) effectively target HER family receptors in cetuximab-resistant clones for prolonged periods of time and 2) significantly impact downstream signaling, which may explain the observed decrease in proliferation, in cetuximab-resistant clones.
Figure 1. Pan-HER inhibits the proliferation of cetuximab-resistant cells.
(A) Pan-HER inhibits the proliferation of cetuximab-resistant clones. Cetuximab-sensitive cells HP and cetuximab-resistant clones (HC1, HC4, and HC8) were plated and treated with vehicle, cetuximab (20 μg/ml) or Pan-HER (0.1, 1, 20, or 100 μg/ml) for 72 hours prior to measuring the proliferation by CCK8 assay. Data points are represented as means ± SEM (n=4) **p≤0.001. (B) Pan-HER down-regulates HER family receptors and decreases downstream AKT and MAPK signalling. Cells were treated with vehicle or Pan-HER (0.1, 1, 20, or 100 μg/ml) for 24 hours. (C) HER family receptors remain down-regulated in cetuximab-resistant clones at 72 hours following Pan-HER treatment. Cells were treated with vehicle or Pan-HER (20 μg/ml) for 24, 48, or 72 hours. Cells were lysed and fractionated on SDS-PAGE, followed by immunoblotting for the indicated proteins. α-Tubulin was used as a loading control.
Pan-HER Effectively Down-modulates HER Family Receptors and Inhibits the Proliferation of Cetuximab-Resistant Clones as Compared to Cetuximab
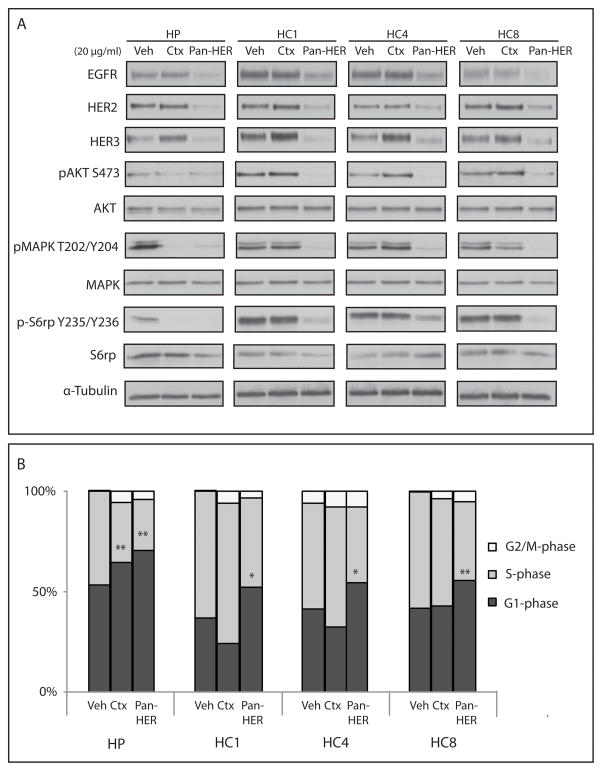
To investigate the impacts of concurrent targeting of HER family receptors in cetuximab-resistant NSCLC clones by cetuximab compared to Pan-HER, we compared the expression levels of EGFR, HER2, and HER3 as well as the phosphorylation levels of downstream signaling molecules in cells treated with 20 μg/mL cetuximab or Pan-HER for 24 hours (Figure 2A). Pan-HER treatment resulted in the down-modulation of EGFR, HER2 and HER3, whereas cetuximab treatment had no effect on HER family levels in cetuximab-resistant clones. Furthermore, the phosphorylation level of AKT, S6rp, and MAPK was significantly diminished after Pan-HER treatment in all cetuximab-resistant NSCLC clones, whereas cetuximab treatment had little inhibitory effect on inhibiting these signaling pathways.
Figure 2. Pan-HER effectively down-modulate HER family receptors in cetuximab-resistant clones compared with cetuximab and enhance to cell cycle arrest.
(A) Pan-HER, but not cetuximab, treatment leads to decreased expression of HER family receptors and subsequent downstream AKT and MAPK signalling pathways. HP and cetuximab-resistant clones (HC1, HC4, and HC8) were treated with vehicle, cetuximab (20 μg/ml) or Pan-HER (20 μg/ml) for 24 hours. Cells were lysed and fractionated on SDS-PAGE, followed by immunoblotting for the indicated proteins. α-Tubulin was used as a loading control. (B) Pan-HER induces a G1-phase cell cycle arrest in cetuximab-resistant clones. Cells were treated with 20 μg/ml cetuximab or 20 μg/ml Pan-HER for 24 hours, and cell cycle phase distribution was analyzed as described in the Materials and Methods section. Data points are represented as means ± SEM (n=3) *p<0.05, **p≤0.001.
Pan-HER-treated cells also showed potent cell cycle inhibition in cetuximab-resistant clones post Pan-HER treatment, when compared to those treated with cetuximab (Figure 2B). In addition, Pan-HER-treated cells had a greater inhibition of S-phase than cetuximab treated cells in acquired cetuximab-resistant NSCLC cells. Interestingly, compared to cetuximab, Pan-HER induced more G1 arrest in HP cetuximab-sensitive cells.
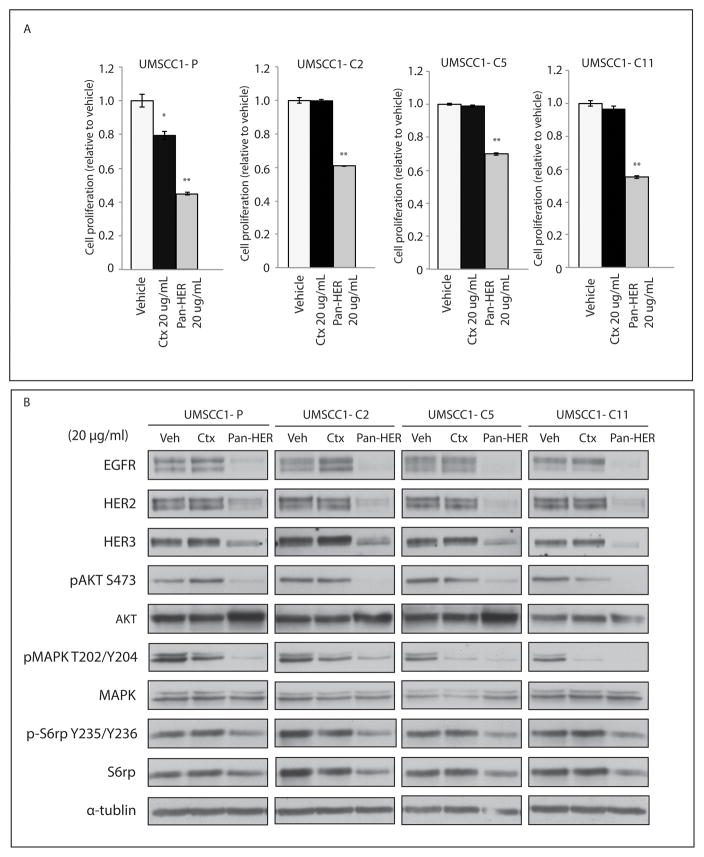
We utilized a second model of acquired resistance in HNSCC to further investigate whether Pan-HER would be effective in other models of acquired cetuximab-resistance (13). The proliferation of the parental UMSCC1 cell line (UMSCC1-P) was inhibited by treatment with 20 μg/mL cetuximab, while the three HNSCC cetuximab-resistant clones (C2, C5, and C11) were completely refractory to cetuximab (Figure 3A). Evaluation of cellular proliferation 72 hours post-treatment indicated statistically significant inhibition in HNSCC cetuximab-resistant clones by 20 μg/mL Pan-HER (Figure 3A). Immunoblot analysis mirrored the findings in the NSCLC acquired resistant model (Figure 1 and 2), showing that the expression of HER family members and activation of MAPK, AKT and S6rp signaling pathways were inhibited by Pan-HER treatment (Figure 3B). The fact that MAPK activity in the cetuximab-resistant HNSCC cells was blocked by cetuximab treatment suggests that MAPK plays a minor role in resistance. Collectively, these results suggest that Pan-HER can effectively overcome cetuximab resistance in two independent models of acquired resistance and impact this resistance by attenuating signaling cascades involving MAPK, AKT, and S6rp.
Figure 3. Pan-HER decreases HER family receptors in acquired cetuximab-resistant HNSCC.
(A) Cells were plated and treated with vehicle cetuximab (20 μg/ml) or Pan-HER (20 μg/ml) for 72 hours prior to measuring the proliferation by CCK8 assay. Data points are represented as means ± SEM (n= 4). *p<0.05, **p≤0.001. (B) Pan-HER decreased HER family receptors and inhibits downstream AKT and MAPK signalling. Cells were treated with vehicle, cetuximab (20 μg/ml) or Pan-HER (20 μg/ml) for 24 hours, after which the cell were lysed and fractionated on SDS-PAGE for the indicated proteins. α-Tubulin was used as a loading control.
Pan-HER Delays the Growth of Tumors with Acquired Cetuximab-Resistance
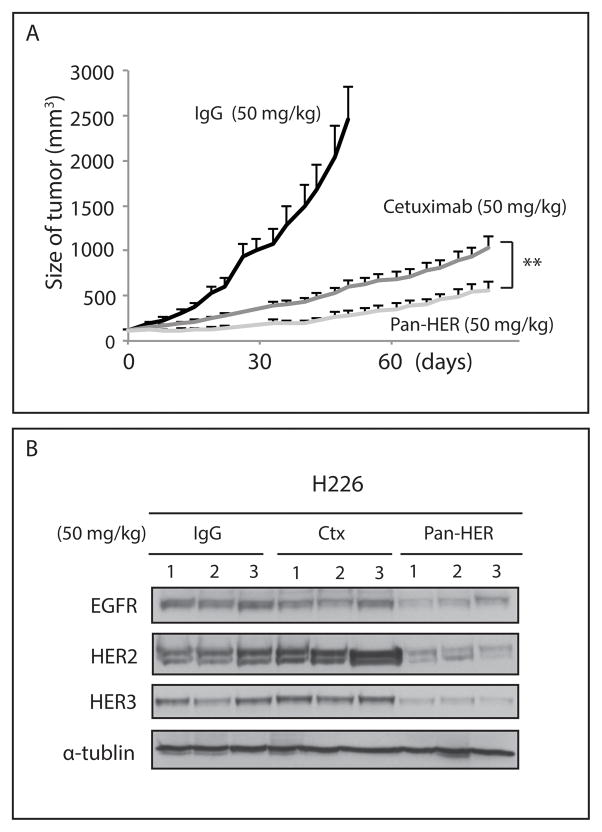
To expand our in vitro findings to the in vivo setting, Pan-HER was tested in a cell line-derived xenograft model with confirmed HER family dependence. Thirty mice were injected with the NSCLC H226 cells in the dorsal flank on day 0 (2x106 cells), and once tumors reached an average volume of 200 mm3 (~18 days), mice were randomized and treatment initiated. Cetuximab or Pan-HER was administered through i.p. injection at a dose of 50 mg/kg twice weekly for ten consecutive weeks. Mouse weight was measured weekly, and no discernible toxicity was observed in either the cetuximab or Pan-HER treatment group. Treatment with Pan-HER showed statistically significant tumor growth delay and exhibited superior antitumor activity compared to cetuximab treatment over 60 days (Figure 4A). Analysis of tumor lysates harvested from each treatment group indicated that expression levels of EGFR, HER2 and HER3 were strongly and uniformly reduced in all tumors from Pan-HER treated mice, whereas IgG- or cetuximab-treated tumors retained significant expression levels of HER family receptors (Figure 4B).
Figure 4. Pan-HER exhibits greater anti-tumor effects than cetuximab in lung tumors.
(A) Pan-HER shows anti-tumor activity and delayed tumor growth of H226 xenografts compared with the cetuximab treatment group. H226 cells were injected into mice and tumors were allowed to grow to 100 mm3. All mice were randomized to treatment or control groups and treated with cetuximab (50 mg/kg), Pan-HER (50 mg/kg), or IgG (50 mg/kg) i.p. twice weekly. (B) Pan-HER-induced HER family receptor down-modulation in vivo. Immunoblot analysis of total HER family receptors in xenograft tumors after IgG, cetuximab or Pan-HER treatment. α-Tubulin was used as a loading control.
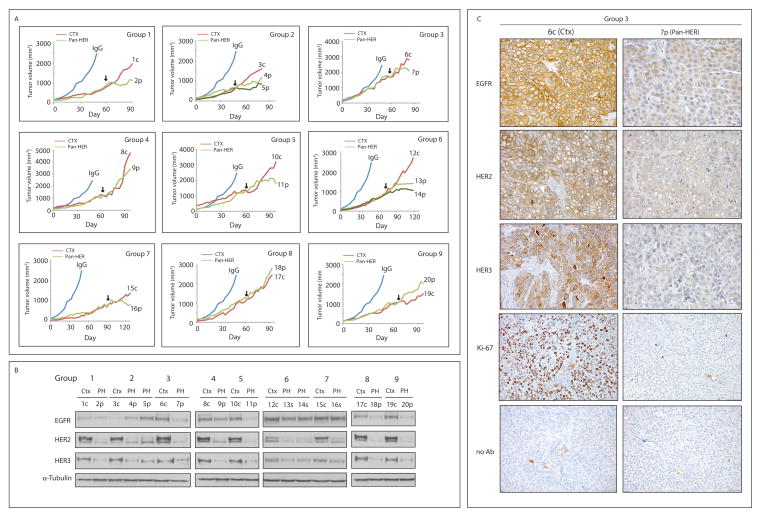
Next, a series of mouse xenograft studies of de novo acquired resistance to cetuximab were established to evaluate the efficacy of Pan-HER in overcoming acquired resistance to cetuximab in vivo. Fifty mice were inoculated with the NSCLC H226 cell line individually with 2x106 tumor cells in the dorsal flank. Tumors were allowed to grow to 100 mm3, at which time 40 mice were treated with cetuximab (50 mg/kg) and 10 mice were treated with IgG control (50 mg/kg) twice weekly by i.p. injection. IgG-treated tumors grew rapidly, whereas cetuximab-treated tumors showed delayed growth. Tumors were monitored for the development of cetuximab resistance, defined as marked tumor growth in the presence of continued cetuximab therapy. Once cetuximab-resistant tumors reached a volume of ~800 mm3, mice were grouped according to tumor size at the time of resistance. Cetuximab-resistant tumors were observed in 28 of 40 mice (70 %), which is in line with previous studies (14, 20, 21). Mice were then randomly subdivided into 13 cetuximab-resistant xenograft groups (28 mice in total), nine of which are shown in Figure 5A. One mouse per group was maintained on cetuximab therapy, while the other mouse (or mice) was removed from cetuximab treatment and started on 50 mg/kg Pan-HER (i.p. twice weekly). Fifteen mice were treated with Pan-HER and 13 mice were maintained on cetuximab therapy. The average tumor volume of mice treated with IgG alone is included in all groups for comparison purposes. Eleven of 15 (73%) cetuximab-resistant tumors treated with Pan-HER demonstrated an anti-tumor response compared to the cetuximab-treated group, whereas 4 of 15 (27%) tumors showed limited response to Pan-HER treatment. In Figure 5A, mice treated with Pan-HER in Groups 1, 2, 5, and 6 demonstrated more pronounced anti-proliferative responses than those maintained on cetuximab. Additionally, this anti-tumor response was maintained for more than 30 days in the Pan-HER treated mice. Mice treated with Pan-HER in Groups 3, 4, and 7 showed anti-proliferative response after 15–20 days of Pan-HER treatment. In contrast, tumors treated with Pan-HER in Group 8 and 9 did not exhibit delayed tumor growth compared to the tumor treated with cetuximab.
Figure 5. Pan-HER treatment delays the growth of tumors with acquired cetuximab-resistance.
(A) Growth-inhibitory effects of Pan-HER on cetuximab-resistant tumors in vivo. Acquired cetuximab-resistance tumors were established and evaluated for Pan-HER response as described in Materials and Methods. The black arrows indicate initiation of Pan-HER treatment. The average tumor volume in mice treated with IgG is included in all groups for comparison purposes. Tumor number is indicated for correlation with Figure 5B. (B) Pan-HER-induced HER family receptor down-modulation in vivo. Immunoblot analysis of total HER family receptors in cetuximab-resistant xenograft tumors after cetuximab or Pan-HER treatment. α-Tubulin was used as a loading control. (C) Down-modulation of HER family receptors in cetuximab-resistant tumors corresponds with loss of proliferation. Cetuximab-resistant tumor samples after cetuximab or Pan-HER treatments in vivo were prepared and analyzed for EGFR, HER2, HER3, and proliferation (Ki67) immunohistochemistry.
To determine whether Pan-HER effectively down-regulated the HER family of receptors in vivo, receptor levels in harvested tumors were investigated by immunoblot analysis (Figure 5B). Analysis of tumor lysates harvested from each treatment group indicated that Pan-HER-treated cetuximab-resistant tumors had low or undetectable levels of EGFR, HER2, or HER3. Cetuximab-treated cetuximab-resistant tumors, however, retained significant expression levels of the HER family receptors. These findings were similar to the results presented in Figure 2A. Interestingly, examination of Pan-HER treated tumors in Group 8 and 9 indicated that HER family receptors were effectively down-modulated upon treatment despite a minimal decrease in tumor growth. In a complementary approach, we verified these findings in tissue sections of the tumors by immunohistochemical analysis of EGFR, HER2, and HER3 as well as measurement of markers for cell proliferation (Ki67) (Figure 5C). Strong membrane and intracellular HER family member staining was observed in cetuximab-treated cetuximab-resistant tumors (6c from group 3). In contrast, Pan-HER-treated cetuximab-resistant tumors showed moderate intracellular HER family member staining, and limited to no membrane staining in the majority of tumors (7p from group 3). Furthermore, Pan-HER treated cetuximab-resistant tumors had lower expression of Ki67 than cetuximab treatment groups (Figure 5C). Collectively, these findings show that Pan-HER can effectively and consistently target the HER family of receptors in tumors that acquire resistance in vitro or in vivo and significantly impact tumor growth.
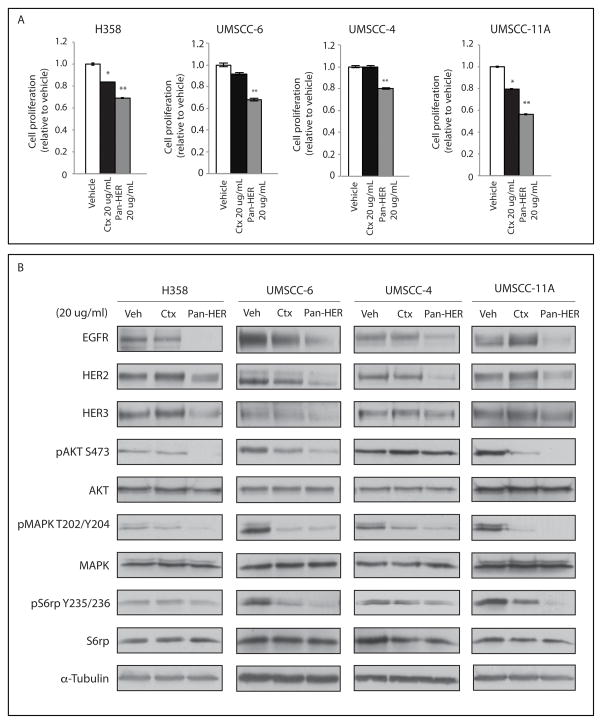
Pan-HER Effectively Decreased HER Family Receptors in Intrinsically Cetuximab-Resistant NSCLC and HNSCC Cell Lines
The data presented strongly suggests that Pan-HER can effectively overcome cetuximab resistance in several models of acquired resistance to cetuximab. Intrinsic resistance to cetuximab, however, in NSCLC and HNSCC remains a major clinical hurdle. To determine whether Pan-HER can overcome intrinsic resistance to cetuximab, intrinsically resistant NSCLC (H358) and HNSCC (UMSCC-6, UMSCC-4 and UMSCC-11A) cell lines were treated with 20 μg/mL of cetuximab or Pan-HER for 72 hours (Figure 6A). Pan-HER treatment resulted in statistically significant cell growth inhibition while cetuximab treatment had little effect. In addition, while cetuximab treatment exhibited mild inhibition of proliferation in H358 and UMSCC11A, Pan-HER treatment showed comparatively greater inhibition. After the establishment of these data, we investigated which pathways were inhibited by Pan-HER in those cell lines. Four intrinsically cetuximab-resistant NSCLC and HNSCC cell lines were treated with vehicle, cetuximab or Pan-HER for 24 hours. Expression levels of HER family receptors as well as AKT, MAPK, and S6rp phosphorylation levels were decreased by Pan-HER treatment compared to vehicle or cetuximab treatment (Figure 6B). Total HER3 levels in three UMSCC cell lines did not show superior down-modulation after Pan-HER treatment due to low total HER3 expressions. Overall, these data suggest that Pan-HER treatment impacts proliferation in intrinsically cetuximab-resistant NSCLC and HNSCC cell lines by reducing HER family receptor expression. Additionally, these data show that Pan-HER could significantly and consistently decreases activation of prominent downstream signaling pathways such as AKT, S6rp, and MAPK.
Figure 6. Pan-HER effectively decreases HER family receptors in intrinsic cetuximab-resistant lung and HNSCC cell lines.
(A) Cells were plated and allowed to adhere for 24 hours prior to vehicle, cetuximab (20 μg/mL) or Pan-HER (20 μg/mL) treatment. Cell proliferation assay were described as Materials and Methods. Data points are represented as mean ± SEM (n=6). **p≤0.001. (B) Pan-HER degrades HER family receptors and inhibits downstream AKT and MAPK signalling. Cells were treated with vehicle, cetuximab (20 μg/ml) or Pan-HER (20 μg/ml) for 24 hours. The cells were then lysed and fractionated on SDS-PAGE for the indicated proteins. α-Tubulin was used as a loading control.
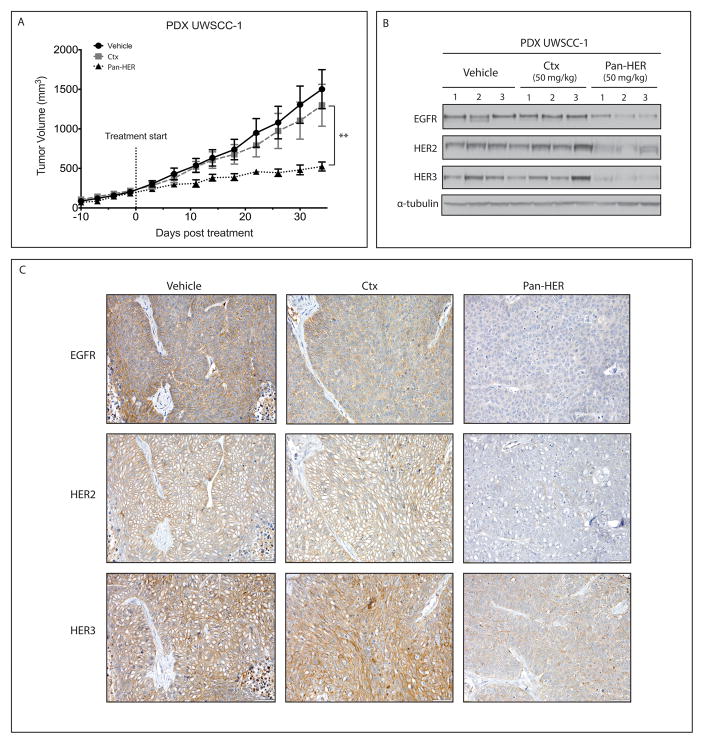
Pan-HER Treatment Leads to Decreased Tumor Growth in an Intrinsically Resistant Patient-Derived Xenograft Model
To expand these findings to a clinically more relevant model system, the effects of Pan-HER treatment were assessed in a PDX model established directly from a HNSCC patient (UW-SCC1). Previous analysis indicated that UW-SCC1 was resistant to cetuximab therapy (24, 25). Twelve mice were then injected with UWSCC-1 PDX in the flank and tumors were allowed grow to 200 mm3. All mice were randomized to treatment or control groups and treated with either vehicle, cetuximab, or Pan-HER by i.p. twice weekly. Mouse weight was measured weekly, and no discernible toxicity was observed in either the cetuximab or Pan-HER treatment group. Treatment with Pan-HER significantly delayed tumor growth of UWSCC-1 PDX compared to either vehicle or cetuximab treatment (Figure 7A). We examined expression levels of HER family members in individual tumors by immunoblot analysis to further investigate the potential of Pan-HER to effectively target HER family receptors in tumors in vivo (Figure 7B). Pan-HER-treated UWSCC-1 PDX tumors had essentially undetectable levels of EGFR, HER2, or HER3, whereas vehicle or cetuximab-treated UWSCC-1 PDX tumors retained significant levels of these receptors. These findings were consistent with the results presented in Figure 5B. Next, we verified these findings in tissue sections of the same tumors by immunohistochemical (IHC) analysis of EGFR, HER2, and HER3. IHC analysis confirmed the immunoblot results by demonstrating down-modulation of membrane and intracellular HER family receptor levels in Pan-HER-treated tumors (Figure 7C). Together, these data demonstrate that Pan-HER treatment resulted in an impactful and sustained antitumor effect in an intrinsically cetuximab resistant HNSCC PDX model through the targeting of multiple HER family members.
Figure 7. Pan-HER can overcome cetuximab-resistant in intrinsically resistant patient-derived xenografts.
(A) Mice were injected with HNSCC PDX cetuximab-resistant tumor (UWSCC-1) and tumors were allowed grow to 200 mm3. All mice were randomized to treatment or control groups and treated with either 50 mg/kg of cetuximab, Pan-HER, or vehicle i.p. twice weekly. The black dotted line designates the start of drug treatment (B) Pan-HER-induced HER family receptor down-modulation in PDX HNSCC tumor (UWSCC-1). Immunoblot analysis was performed of total HER family receptors in PDX HNSCC tumors after treatment. α-Tubulin was used as a loading control. (C) Reduction of HER family receptors in PDX HNSCC tumors. Cetuximab-resistant tumor samples after cetuximab or Pan-HER treatment in vivo were prepared and analyzed for EGFR, HER2, and HER3 immunohistochemistry.
Discussion
EGFR is one of the most highly targeted receptors in oncology due to its frequent overexpression and aberrant activation in numerous cancers (26). Cetuximab is a chimeric human-murine monoclonal IgG1 antibody that binds to the extracellular domain of EGFR and inhibits ligand binding, dimerization and ultimately its activation. Cetuximab has shown efficacy in treating HNSCC, mCRC and NSCLC however, several clinical studies have shown that intrinsic and acquired resistances are common (27–32). Determining why tumors are initially resistant to cetuximab or develop resistance during the course of therapy represents a major clinical challenge.
To elucidate potential mechanisms of resistance to cetuximab in NSCLC and HNSCC, we developed models of cetuximab resistance using the cetuximab-sensitive NSCLC line H226 and HNSCC line UM-SCC1 (13). In these models, we found that cetuximab-resistant clones had increased expression and activity of the HER family, including EGFR, HER2, and HER3, compared to cetuximab-sensitive HP cell line. These findings suggested that cetuximab resistance could manifest by constitutive overexpression and activity of the HER family (13). We previously found that cetuximab-resistant clones had dependency on EGFR for enhanced proliferative potential when EGFR was targeted genetically (21, 33). To investigate whether cetuximab resistant tumors would be sensitive to different EGFR antibody, Sym004, a mixture of two anti-EGFR monoclonal antibodies that leads to EGFR degradation, was tested. Sym004 led to rapid internalization and degradation of EGFR in cetuximab-resistant H226 clones with subsequent loss of proliferative effects (20). In line with these data, Pedersen et al. reported that Sym004 synergistically inhibited skin, lung and HNSCC cell growth through efficient target internalization and degradation (34). Huang et al. also utilized lung and HNSCC tumors and demonstrated that Sym004 inhibited DNA damage repair as well as augment radiation response in these cancers (35). Furthermore, Ferraro et al. showed that the combination of non-competitive anti-EGFR antibodies (panitumumab + mAb111) accelerated receptor endocytosis, enhanced receptor internalization and impaired recycling in triple-negative breast cancer (TNBC) cells. This mixture of mAbs showed strong G1 arrest in TNBC cells and inhibited these tumor growths, better than either antibody alone (36). Perera et al. demonstrated that two EGFR-targeted antibodies (mAbs 806 and 528) showed synergistic anti-tumor activity in glioma and squamous cell cancer xenograft models (37).
Given the robust expression of EGFR, HER2, and HER3 in cetuximab-resistant clones, we targeted EGFR and HER3 genetically or with the combination of cetuximab and U3-1287, a monoclonal antibody directed against HER3 in cetuximab-resistant clones (14). Abrogation of HER3 activity, either by genetic approaches or U3-1287, led to diminished cell proliferation accompanied by impaired MAPK and AKT signaling (14). Interestingly, HER2 was also strongly inactivated by dual mAb therapy, suggesting that this treatment regimen could block signaling from all three HER family receptors. These studies demonstrate that targeting HER family receptors with antibody-based combinatorial therapies can overcome acquired resistance to cetuximab. Similar findings have been made by other groups in the field (18, 38, 39). Thus, targeting multiple HER family receptors is necessary for complete inhibition of the HER family signaling network. In this study, we took a systematic approach, using an innovative antibody combination called Pan-HER. Pan-HER is a mixture of six monoclonal antibodies targeting EGFR, HER2, and HER3 simultaneously. It inhibits receptor phosphorylation not only by preventing ligand binding, but also by inducing receptor internalization and degradation. The effects of Pan-HER in decreasing cell proliferation and tumor growth was determined in several models of intrinsic and acquired resistance to cetuximab.
We found that Pan-HER inhibited proliferation in NSCLC and HNSCC cell lines with both intrinsic and acquired cetuximab-resistance (Figure 1A, 3A and 6A). Similar findings were reported by Jacobsen et al., where Pan-HER was tested on various cancer cell lines such as lung, breast, or pancreatic with a known dependency on EGFR, HER2, or HER3. Challenging these cell lines with Pan-HER broadly inhibited signaling from the HER family, resulting in abrogated cell proliferation (19). Furthermore, Mancini et al. reported that simultaneous targeting of EGFR (mAb565 or cetuximab), HER2 (mAb12 or trastuzumab), and HER3 (mAb33) was very effective for inhibition of T790M+ erlotinib-resistant NSCLC cells (40). We also found that Pan-HER antibody mixture resulted in a decrease of all three receptors as well as reduced cell proliferation pathway activation compared to cetuximab alone (Figure 2A, 3B, and 6B). Similarly, Mancini et al. showed that triple combination of mAbs targeting EGFR, HER2 and HER3 reduced the detection of all three on the surface of NSCLC cells and prevented increased MAPK activation (40). Francis et al. also demonstrated that Pan-HER might be more efficacious in cell lines that overexpress EGFR, HER2, and/or HER3 in NSCLC, HNSCC or colorectal cancer cell lines (41).
The inhibition of proliferation by Pan-HER was demonstrated using several mouse models. Pan-HER exhibited superior tumor growth delay in H226 lung xenograft models with down-modulation of three HER family receptors as compared to cetuximab (Figure 4A, 4B). Our data is consistent with other investigators indicating that Pan-HER is an effective treatment for pancreatic, squamous, and gastric tumors (19, 42). Next, we utilized two different model systems; de novo acquired cetuximab-resistant and intrinsically cetuximab-resistant PDX xenograft models (Figure 5A, 7A). Both de novo and PDX models are clinically relevant systems and offer a platform for the investigation of novel therapeutics. In the de novo resistant model, acquired cetuximab-resistant xenograft tumors showed significant growth delay (73%) post Pan-HER treatment compared to cetuximab-resistant tumors that were continued on cetuximab treatment (Figure 5A). In an intrinsically cetuximab-resistant HNSCC PDX model, Pan-HER strongly suppressed tumor growth (Figure 7A). Jacobsen et al. also showed a strong effect of Pan-HER treatment in a panel of PDX models, including ovarian, colorectal, lung and pancreatic (19). Furthermore, Pan-HER could augment radiation response in HNSCC PDX tumors (41). Recently, there are a few reports, in which targeting the HER family receptors, rather than any one receptor, in various cancers corroborated with our data. The four-in-one antibody FL518 as potent inhibitors of EGFR, HER2, HER3, and VEGF inhibited their receptor phosphorylation and had superior antitumor activity in colorectal, breast or gastric cancer (43). Pre-clinical data suggested that inhibition of EGFR, HER2, and HER3 by combined treatment with lapatinib, trastuzumab and U3-1287 showed maximum effect in trastuzumab-resistant HER2-overexpressing breast cancer (44). Mancini et al. showed strong inhibitory effect on tumor growth in erlotinib-resistant NSCLC cells (H1975) by triple combinatorial treatment with ant-EGFR, anti-HER2, and anti-HER3 antibodies (40). Notably, treatment with Pan-HER clearly decreased the expression of all three receptors in both de novo and PDX cetuximab-resistant NSCLC and HNSCC tumors by Immunoblot and IHC analyses (Figure 5B, 5C, 7B and 7C). Jacobsen et al. confirmed that Pan-HER treatment induced simultaneous down-modulation of all three receptors in BxPC3 tumors by Western analysis and IHC analysis (19). Nielsen et al. demonstrated that HER family receptors were down-regulated in BxPC3 xenograft model by only a single dose of Pan-HER treatment using IHC analysis (42). Interestingly, Pan-HER treated cetuximab-resistant tumors in Group 8 and 9 showed superior HER family down-modulation, however, Pan-HER treatment did not show any growth delay in these tumors (Figure 5A). It has been exhibited that cetuximab-resistant clones have increased not only EGFR, HER2, HER3, and HER4, but also other receptor tyrosine kinases (RTKs) such as cMET, AXL, and IGF1R (13, 45, 46). Recently, mutations in the genes encoding other RTKs, such as FGFR1 or PDGFRA were found in CRC PDX models with intrinsic resistance to cetuximab (47). Nakamura et al also found HER4 mutation in cetuximab-resistant ESCC or HNSCC cells (48). These RTK crosstalk mechanisms associated with resistance have also been reported in other tumors such as NSCLC, breast cancer or melanoma (49). These data may explain why some of the cetuximab-resistant tumors did not respond to Pan-HER treatment. It is also notable that many other RTK crosstalks may be involved in the mechanisms of drug resistance and a detailed investigation is necessary. Accordingly, combination of other RTK antibodies/inhibitors with Pan-HER could be powerful combination treatment in an antitumor effect for tumors with acquired resistance to cetuximab.
Current study clearly demonstrated that Pan-HER effectively targets the HER family receptors in models of intrinsic or acquired resistance to cetuximab and can overcome cetuximab resistance. Our previous reports and numerous examples from other investigators have demonstrated that treatment of tumors with single agents such as anti-RTK antibodies or TKIs frequently leads to rapid resistance [see review (50)]. Several mechanisms of resistance are associated with overexpression of HER family receptors. Recently, Mancini et al. demonstrated that the triple combination of mAbs could be a feasible pharmacological option for treating lung cancer patients who inevitably develop resistance to EGFR TKIs (40). Nakade et al. also reported that triple inhibition of EGFR, Met and angiogenesis by erlotinib plus TAS-115 efficiently controlled growth of HGF-triggered, EGFR-TKI resistant tumors harboring EGFR mutations (51). Collectively, these studies suggest that completely blocking the signaling of HER family receptors and RTK crosstalk should be a focus of future antibody development strategies. Synergistic antibody mixtures targeting the HER family and beyond are likely to show great promise for the future of RTK targeting in cancer.
Acknowledgments
Grant Support: This work was supported in part by research funding from Symphogen A/S (D.L. Wheeler).
Footnotes
Disclosure of Potential Conflicts of Interest: D.L. Wheeler holds a laboratory research agreement with Symphogen A/S. J. Lantto, I.D. Horak, and M. Kragh are employed by Symphogen A/S. No potential conflicts of interest were disclosed by other authors.
References
- 1.Yarden Y, Pines G. The ERBB network: at last, cancer therapy meets systems biology. Nat Rev Cancer. 2012;12:553–63. doi: 10.1038/nrc3309. [DOI] [PubMed] [Google Scholar]
- 2.Arteaga CL, Engelman JA. ERBB receptors: from oncogene discovery to basic science to mechanism-based cancer therapeutics. Cancer Cell. 2014;25:282–303. doi: 10.1016/j.ccr.2014.02.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Citri A, Yarden Y. EGF-ERBB signalling: towards the systems level. Nat Rev Mol Cell Biol. 2006;7:505–16. doi: 10.1038/nrm1962. [DOI] [PubMed] [Google Scholar]
- 4.Ang KK, Andratschke NH, Milas L. Epidermal growth factor receptor and response of head-and-neck carcinoma to therapy. Int J Radiat Oncol Biol Phys. 2004;58:959–65. doi: 10.1016/j.ijrobp.2003.07.010. [DOI] [PubMed] [Google Scholar]
- 5.Nicholson RI, Gee JM, Harper ME. EGFR and cancer prognosis. European journal of cancer. 2001;37(Suppl 4):S9–15. doi: 10.1016/s0959-8049(01)00231-3. [DOI] [PubMed] [Google Scholar]
- 6.Saito Y, Haendeler J, Hojo Y, Yamamoto K, Berk BC. Receptor heterodimerization: essential mechanism for platelet-derived growth factor-induced epidermal growth factor receptor transactivation. Mol Cell Biol. 2001;21:6387–94. doi: 10.1128/MCB.21.19.6387-6394.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Roskoski R., Jr The ErbB/HER family of protein-tyrosine kinases and cancer. Pharmacological research. 2014;79:34–74. doi: 10.1016/j.phrs.2013.11.002. [DOI] [PubMed] [Google Scholar]
- 8.Hynes NE, MacDonald G. ErbB receptors and signaling pathways in cancer. Current opinion in cell biology. 2009;21:177–84. doi: 10.1016/j.ceb.2008.12.010. [DOI] [PubMed] [Google Scholar]
- 9.Douillard JY, Pirker R, O’Byrne KJ, Kerr KM, Storkel S, von Heydebreck A, et al. Relationship between EGFR expression, EGFR mutation status, and the efficacy of chemotherapy plus cetuximab in FLEX study patients with advanced non-small-cell lung cancer. J Thorac Oncol. 2014;9:717–24. doi: 10.1097/JTO.0000000000000141. [DOI] [PubMed] [Google Scholar]
- 10.Pirker R. EGFR-directed monoclonal antibodies in non-small cell lung cancer. Targeted oncology. 2013;8:47–53. doi: 10.1007/s11523-012-0244-7. [DOI] [PubMed] [Google Scholar]
- 11.Brand TM, Iida M, Wheeler DL. Molecular mechanisms of resistance to the EGFR monoclonal antibody cetuximab. Cancer Biol Ther. 2011;11:777–92. doi: 10.4161/cbt.11.9.15050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Vlacich G, Coffey RJ. Resistance to EGFR-targeted therapy: a family affair. Cancer Cell. 2011;20:423–5. doi: 10.1016/j.ccr.2011.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wheeler DL, Huang S, Kruser TJ, Nechrebecki MM, Armstrong EA, Benavente S, et al. Mechanisms of acquired resistance to cetuximab: role of HER (ErbB) family members. Oncogene. 2008;27:3944–56. doi: 10.1038/onc.2008.19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Iida M, Brand TM, Starr MM, Huppert EJ, Luthar N, Bahrar H, et al. Overcoming acquired resistance to cetuximab by dual targeting HER family receptors with antibody-based therapy. Mol Cancer. 2014;13:242. doi: 10.1186/1476-4598-13-242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Narayan M, Wilken JA, Harris LN, Baron AT, Kimbler KD, Maihle NJ. Trastuzumab-induced HER reprogramming in “resistant” breast carcinoma cells. Cancer Res. 2009;69:2191–4. doi: 10.1158/0008-5472.CAN-08-1056. [DOI] [PubMed] [Google Scholar]
- 16.Yonesaka K, Zejnullahu K, Okamoto I, Satoh T, Cappuzzo F, Souglakos J, et al. Activation of ERBB2 signaling causes resistance to the EGFR-directed therapeutic antibody cetuximab. Science translational medicine. 2011;3:99ra86. doi: 10.1126/scitranslmed.3002442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Tebbutt N, Pedersen MW, Johns TG. Targeting the ERBB family in cancer: couples therapy. Nat Rev Cancer. 2013;13:663–73. doi: 10.1038/nrc3559. [DOI] [PubMed] [Google Scholar]
- 18.Demarest SJ, Hariharan K, Dong J. Emerging antibody combinations in oncology. mAbs. 2011;3:338–51. doi: 10.4161/mabs.3.4.16615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jacobsen HJ, Poulsen TT, Dahlman A, Kjaer I, Koefoed K, Sen JW, et al. Pan-HER, an Antibody Mixture Simultaneously Targeting EGFR, HER2, and HER3, Effectively Overcomes Tumor Heterogeneity and Plasticity. Clin Cancer Res. 2015;21:4110–22. doi: 10.1158/1078-0432.CCR-14-3312. [DOI] [PubMed] [Google Scholar]
- 20.Iida M, Brand TM, Starr MM, Li C, Huppert EJ, Luthar N, et al. Sym004, a Novel EGFR Antibody Mixture, Can Overcome Acquired Resistance to Cetuximab. Neoplasia. 2013;15:1196–206. doi: 10.1593/neo.131584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Brand TM, Dunn EF, Iida M, Myers RA, Kostopoulos KT, Li C, et al. Erlotinib is a viable treatment for tumors with acquired resistance to cetuximab. Cancer Biol Ther. 2011;12:436–46. doi: 10.4161/cbt.12.5.16394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Dunn EF, Iida M, Myers RA, Campbell DA, Hintz KA, Armstrong EA, et al. Dasatinib sensitizes KRAS mutant colorectal tumors to cetuximab. Oncogene. 2011;30:561–74. doi: 10.1038/onc.2010.430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kimple RJ, Harari PM, Torres AD, Yang RZ, Soriano BJ, Yu M, et al. Development and characterization of HPV-positive and HPV-negative head and neck squamous cell carcinoma tumorgrafts. Clin Cancer Res. 2013;19:855–64. doi: 10.1158/1078-0432.CCR-12-2746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Brand TM, Iida M, Stein AP, Corrigan KL, Braverman CM, Coan JP, et al. AXL Is a Logical Molecular Target in Head and Neck Squamous Cell Carcinoma. Clin Cancer Res. 2015;21:2601–12. doi: 10.1158/1078-0432.CCR-14-2648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Stein AP, Saha S, Liu CZ, Hartig GK, Lambert PF, Kimple RJ. Influence of handling conditions on the establishment and propagation of head and neck cancer patient derived xenografts. PLoS One. 2014;9:e100995. doi: 10.1371/journal.pone.0100995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ciardiello F, Tortora G. EGFR antagonists in cancer treatment. The New England journal of medicine. 2008;358:1160–74. doi: 10.1056/NEJMra0707704. [DOI] [PubMed] [Google Scholar]
- 27.Bonner JA, Harari PM, Giralt J, Azarnia N, Shin DM, Cohen RB, et al. Radiotherapy plus cetuximab for squamous-cell carcinoma of the head and neck. The New England journal of medicine. 2006;354:567–78. doi: 10.1056/NEJMoa053422. [DOI] [PubMed] [Google Scholar]
- 28.Pirker R, Pereira JR, Szczesna A, von Pawel J, Krzakowski M, Ramlau R, et al. Cetuximab plus chemotherapy in patients with advanced non-small-cell lung cancer (FLEX): an open-label randomised phase III trial. Lancet. 2009;373:1525–31. doi: 10.1016/S0140-6736(09)60569-9. [DOI] [PubMed] [Google Scholar]
- 29.Van Cutsem E, Kohne CH, Hitre E, Zaluski J, Chang Chien CR, Makhson A, et al. Cetuximab and chemotherapy as initial treatment for metastatic colorectal cancer. The New England journal of medicine. 2009;360:1408–17. doi: 10.1056/NEJMoa0805019. [DOI] [PubMed] [Google Scholar]
- 30.Khelwatty SA, Essapen S, Bagwan I, Green M, Seddon AM, Modjtahedi H. Co-expression of HER family members in patients with Dukes’ C and D colon cancer and their impacts on patient prognosis and survival. PLoS One. 2014;9:e91139. doi: 10.1371/journal.pone.0091139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lynch TJ, Patel T, Dreisbach L, McCleod M, Heim WJ, Hermann RC, et al. Cetuximab and first-line taxane/carboplatin chemotherapy in advanced non-small-cell lung cancer: results of the randomized multicenter phase III trial BMS099. Journal of clinical oncology : official journal of the American Society of Clinical Oncology. 2010;28:911–7. doi: 10.1200/JCO.2009.21.9618. [DOI] [PubMed] [Google Scholar]
- 32.Misale S, Di Nicolantonio F, Sartore-Bianchi A, Siena S, Bardelli A. Resistance to anti-EGFR therapy in colorectal cancer: from heterogeneity to convergent evolution. Cancer discovery. 2014;4:1269–80. doi: 10.1158/2159-8290.CD-14-0462. [DOI] [PubMed] [Google Scholar]
- 33.Wheeler DL, Iida M, Kruser TJ, Nechrebecki MM, Dunn EF, Armstrong EA, et al. Epidermal growth factor receptor cooperates with Src family kinases in acquired resistance to cetuximab. Cancer Biol Ther. 2009;8:696–703. doi: 10.4161/cbt.8.8.7903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Pedersen MW, Jacobsen HJ, Koefoed K, Hey A, Pyke C, Haurum JS, et al. Sym004: a novel synergistic anti-epidermal growth factor receptor antibody mixture with superior anticancer efficacy. Cancer Res. 2010;70:588–97. doi: 10.1158/0008-5472.CAN-09-1417. [DOI] [PubMed] [Google Scholar]
- 35.Huang S, Peet CR, Saker J, Li C, Armstrong EA, Kragh M, et al. Sym004, a novel anti-EGFR antibody mixture, augments radiation response in human lung and head and neck cancers. Mol Cancer Ther. 2013;12:2772–81. doi: 10.1158/1535-7163.MCT-13-0587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ferraro DA, Gaborit N, Maron R, Cohen-Dvashi H, Porat Z, Pareja F, et al. Inhibition of triple-negative breast cancer models by combinations of antibodies to EGFR. Proc Natl Acad Sci U S A. 2013;110:1815–20. doi: 10.1073/pnas.1220763110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Perera RM, Narita Y, Furnari FB, Gan HK, Murone C, Ahlkvist M, et al. Treatment of human tumor xenografts with monoclonal antibody 806 in combination with a prototypical epidermal growth factor receptor-specific antibody generates enhanced antitumor activity. Clin Cancer Res. 2005;11:6390–9. doi: 10.1158/1078-0432.CCR-04-2653. [DOI] [PubMed] [Google Scholar]
- 38.Zhang L, Castanaro C, Luan B, Yang K, Fan L, Fairhurst JL, et al. ERBB3/HER2 signaling promotes resistance to EGFR blockade in head and neck and colorectal cancer models. Mol Cancer Ther. 2014 doi: 10.1158/1535-7163.MCT-13-1033. [DOI] [PubMed] [Google Scholar]
- 39.Zheng L, Tan W, Zhang J, Yuan D, Yang J, Liu H. Combining trastuzumab and cetuximab combats trastuzumab-resistant gastric cancer by effective inhibition of EGFR/ErbB2 heterodimerization and signaling. Cancer immunology, immunotherapy : CII. 2014 doi: 10.1007/s00262-014-1541-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Mancini M, Gaborit N, Lindzen M, Salame TM, Dall’Ora M, Sevilla-Sharon M, et al. Combining three antibodies nullifies feedback-mediated resistance to erlotinib in lung cancer. Science signaling. 2015;8:ra53. doi: 10.1126/scisignal.aaa0725. [DOI] [PubMed] [Google Scholar]
- 41.Francis DM, Huang S, Armstrong EA, Werner LR, Hullett CR, Li C, et al. Pan-HER receptor inhibition augments radiation response in human lung and head and neck cancer models. Clin Cancer Res. 2015 doi: 10.1158/1078-0432.CCR-15-1664. [DOI] [PubMed] [Google Scholar]
- 42.Nielsen CH, Jensen MM, Kristensen LK, Dahlman A, Frohlich C, Jacobsen HJ, et al. In vivo imaging of therapy response to a novel Pan-HER antibody mixture using FDG and FLT positron emission tomography. Oncotarget. 2015 doi: 10.18632/oncotarget.6060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Hu S, Fu W, Xu W, Yang Y, Cruz M, Berezov SD, et al. Four-in-one antibodies have superior cancer inhibitory activity against EGFR, HER2, HER3, and VEGF through disruption of HER/MET crosstalk. Cancer Res. 2015;75:159–70. doi: 10.1158/0008-5472.CAN-14-1670. [DOI] [PubMed] [Google Scholar]
- 44.Garrett JT, Sutton CR, Kuba MG, Cook RS, Arteaga CL. Dual blockade of HER2 in HER2-overexpressing tumor cells does not completely eliminate HER3 function. Clin Cancer Res. 2013;19:610–9. doi: 10.1158/1078-0432.CCR-12-2024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Hatakeyama H, Cheng H, Wirth P, Counsell A, Marcrom SR, Wood CB, et al. Regulation of heparin-binding EGF-like growth factor by miR-212 and acquired cetuximab-resistance in head and neck squamous cell carcinoma. PLoS One. 2010;5:e12702. doi: 10.1371/journal.pone.0012702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Brand TM, Iida M, Stein AP, Corrigan KL, Braverman CM, Luthar N, et al. AXL mediates resistance to cetuximab therapy. Cancer Res. 2014;74:5152–64. doi: 10.1158/0008-5472.CAN-14-0294. [DOI] [PMC free article] [PubMed] [Google Scholar] [Research Misconduct Found]
- 47.Bertotti A, Papp E, Jones S, Adleff V, Anagnostou V, Lupo B, et al. The genomic landscape of response to EGFR blockade in colorectal cancer. Nature. 2015;526:263–7. doi: 10.1038/nature14969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Nakamura Y, Togashi Y, Nakahara H, Tomida S, Banno E, Terashima M, et al. Afatinib against esophageal or head-and-neck cell squamous carcinoma: significance of activating oncogenic HER4 mutations in HNSCC. Mol Cancer Ther. 2016 doi: 10.1158/1535-7163.MCT-15-0737. [DOI] [PubMed] [Google Scholar]
- 49.Sun C, Bernards R. Feedback and redundancy in receptor tyrosine kinase signaling: relevance to cancer therapies. Trends in biochemical sciences. 2014;39:465–74. doi: 10.1016/j.tibs.2014.08.010. [DOI] [PubMed] [Google Scholar]
- 50.Bertotti A, Sassi F. Molecular Pathways: Sensitivity and Resistance to Anti-EGFR Antibodies. Clin Cancer Res. 2015;21:3377–83. doi: 10.1158/1078-0432.CCR-14-0848. [DOI] [PubMed] [Google Scholar]
- 51.Nakade J, Takeuchi S, Nakagawa T, Ishikawa D, Sano T, Nanjo S, et al. Triple inhibition of EGFR, Met, and VEGF suppresses regrowth of HGF-triggered, erlotinib-resistant lung cancer harboring an EGFR mutation. J Thorac Oncol. 2014;9:775–83. doi: 10.1097/JTO.0000000000000170. [DOI] [PMC free article] [PubMed] [Google Scholar]