Abstract
While brainstem cavernous malformations were once considered inoperable, improvements in patient selection, surgical exposures, intraoperative MRI-guidance, MR tractography, and neurophysiologic monitoring have resulted in good outcomes in the majority of operated patients. In a consecutive series of 104 patients with brainstem cavernous malformations, only 14% of patients experienced cranial nerve or motor dysfunction that was worse at late follow-up, relative to their preoperative condition. Outcomes were predicted by several factors, including larger lesion size, lesions that crossed midline, the presence of a developmental venous anomaly, older age, and greater time interval from lesion hemorrhage to surgery. The 14% of patients who experienced a persistent neurological deficit as a result of surgery, while substantial from any perspective, compares favorably with the risks of observation based on a meta-analysis published by Horne et al. 2016. Curative resection is a safe and effective treatment for brainstem cavernous malformations that will prevent re-hemorrhage in symptomatic patients.
Keywords: Brainstem, Cavernoma, Cavernous malformation, Hemorrhage, Stroke, Surgery
1. Introduction
Horne et al. make a very important contribution to our knowledge of the natural history of cavernous malformations1, providing robust evidence for long-held suspicions that brainstem location and hemorrhagic lesions portend a more aggressive clinical course. When observed together, these lesions have an estimated 5-year recurrent hemorrhage risk of 30.8%, with a 50.7% risk of developing either a recurrent hemorrhage or a new neurological deficit not related to hemorrhage. Interestingly, the risk of events in the follow-up period was not uniform, and decreased with time. In this analysis, the median age of patients presenting with hemorrhage was 41, and we suspect that their cumulative risk over many decades of remaining life is higher than the 5-year estimates reported. These natural history data will undoubtedly inform management decisions. These data are especially useful when stakes are highest, with hemorrhagic lesions in the brainstem, as both the natural history and treatment risks are unique from other brain locations and presentations.
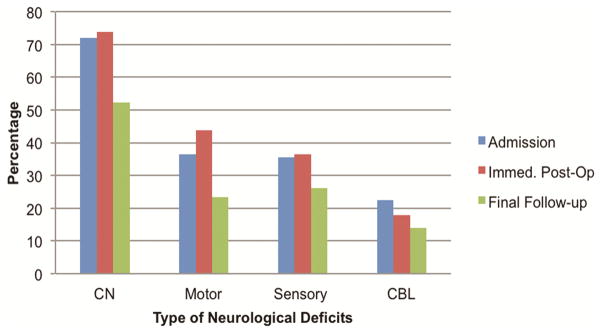
While brainstem cavernous malformations were once considered inoperable, improvements in patient selection, surgical exposures, intraoperative MRI-guidance, MR tractography, and neurophysiologic monitoring have resulted in good outcomes in the majority of operated patients.2–5 In our series of 104 patients with brainstem cavernous malformations, only 14% of patients experienced cranial nerve or motor dysfunction that was worse at late follow-up, relative to their preoperative condition.3 Outcomes were predicted by several factors, including larger lesion size, lesions that crossed midline, the presence of a developmental venous anomaly, older age, and greater time interval from lesion hemorrhage to surgery. It is important to note that most of the neurological deficits after brainstem cavernous malformation surgery are transient, and ultimately improve in the long term. [Figure 1] The 14% of patients who experienced a persistent neurological deficit as a result of surgery, while substantial from any perspective, compares favorably with the risks of observation based on these new data.
Figure 1.
In a retrospective, single center series at the University of California San Francisco, patients undergoing surgery for brainstem cavernous malformations were examined before surgery, immediately after surgery, and at final follow-up. A greater percentage of patients experienced neurological deficits immediately postoperatively compared to preoperatively. However, the percentage decreased to the lowest levels at the time of last clinical follow-up, suggesting that any neurological worsening following surgery is temporary in most cases. Abbreviations: CN (cranial nerve), CBL (cerebellar)
2. Conclusion
We anticipate that meta-analysis of patient level data from surgical series at high-volume neurovascular centers will validate curative resection as a safe and effective treatment for brainstem cavernous malformations that will prevent re-hemorrhage in symptomatic patients.
Footnotes
Conflicts of Interest/Disclosures
The authors declare that they have no financial or other conflicts of interest in relation to this research and its publication.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Horne MA, Flemming KD, Su I-C, et al. Clinical course of untreated cerebral cavernous malformations: a meta-analysis of individual patient data. The Lancet Neurology. 2015 doi: 10.1016/S1474-4422(15)00303-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Abla AA, Lekovic GP, Turner JD, de Oliveira JG, Porter R, Spetzler RF. Advances in the treatment and outcome of brainstem cavernous malformation surgery: a single-center case series of 300 surgically treated patients. Neurosurgery. 2011;68(2):403–15. doi: 10.1227/NEU.0b013e3181ff9cde. [DOI] [PubMed] [Google Scholar]
- 3.Garcia RM, Ivan ME, Lawton MT. Brainstem Cavernous Malformations: Surgical Results in 104 Patients and a Proposed Grading System to Predict Neurological Outcomes. Neurosurgery. 2015;76(3):265–78. doi: 10.1227/NEU.0000000000000602. [DOI] [PubMed] [Google Scholar]
- 4.Pandey P, Westbroek EM, Gooderham PA, Steinberg GK. Cavernous malformation of brainstem, thalamus, and basal ganglia: a series of 176 patients. Neurosurgery. 2013;72(4):573–89. doi: 10.1227/NEU.0b013e318283c9c2. [DOI] [PubMed] [Google Scholar]
- 5.Gross BA, Batjer HH, Awad IA, Bendok BR, Du R. Brainstem cavernous malformations: 1390 surgical cases from the literature. World neurosurgery. 2013;80(1):89–93. doi: 10.1016/j.wneu.2012.04.002. [DOI] [PubMed] [Google Scholar]