Abstract
Cone-rod degeneration (CRD) belongs to the disease spectrum of retinal degenerations, a group of hereditary disorders characterized by an extreme clinical and genetic heterogeneity. It mainly differentiates from other retinal dystrophies, and in particular from the more frequent disease retinitis pigmentosa, because cone photoreceptors degenerate at a higher rate than rod photoreceptors, causing severe deficiency of central vision. After exome analysis of a cohort of individuals with CRD, we identified biallelic mutations in the orphan gene CEP78 in three subjects from two families: one from Greece and another from Sweden. The Greek subject, from the island of Crete, was homozygous for the c.499+1G>T (IVS3+1G>T) mutation in intron 3. The Swedish subjects, two siblings, were compound heterozygotes for the nearby mutation c.499+5G>A (IVS3+5G>A) and for the frameshift-causing variant c.633delC (p.Trp212Glyfs∗18). In addition to CRD, these three individuals had hearing loss or hearing deficit. Immunostaining highlighted the presence of CEP78 in the inner segments of retinal photoreceptors, predominantly of cones, and at the base of the primary cilium of fibroblasts. Interaction studies also showed that CEP78 binds to FAM161A, another ciliary protein associated with retinal degeneration. Finally, analysis of skin fibroblasts derived from affected individuals revealed abnormal ciliary morphology, as compared to that of control cells. Altogether, our data strongly suggest that mutations in CEP78 cause a previously undescribed clinical entity of a ciliary nature characterized by blindness and deafness but clearly distinct from Usher syndrome, a condition for which visual impairment is due to retinitis pigmentosa.
Main Text
Cone-rod degeneration (CRD [MIM: 120970]) represents an extremely rare class of hereditary diseases that affect the light-sensing neurons of the retina, the cone and rod photoreceptors.1 Cones are involved in daytime vision, providing the brain with color information and central, precise visual input. Conversely, rods are active in very dim light conditions, are more abundant in the retinal periphery, and produce achromatic information, typical for instance of the visual stimulation provided by a landscape on a moonless night. Individuals with CRD experience initial loss of visual acuity (central vision) and aberrant color vision as a result of the prominent loss of cones, whereas rod functions remain relatively preserved.2 As the disease progresses, both cone and rod functions deteriorate and central vision is severely impaired or lost, but peripheral islands of the retina might retain some residual activity.3 On the basis of these clinical parameters, CRD can be distinguished from retinitis pigmentosa (RP [MIM: 26800], also called rod-cone degeneration), the most common form of hereditary retinal degeneration. In retinitis pigmentosa, rods are more severely affected than cones; initial symptoms include night blindness due to loss of rod function, and central vision (cone function) is often preserved until the very late stages of the disease.4 CRD is almost invariantly inherited as a Mendelian trait, predominantly according to a recessive pattern of transmission, and is characterized by an elevated genetic and allelic heterogeneity.5 Although as many as 33 CRD-associated genes have been identified to date (RetNet; see Web Resources), they are found to be mutated in only ∼25% of clinical cases, implying that a substantial percentage of affected people might carry mutations in yet-to-be-identified genes.6
According to this rationale, we performed whole-exome sequencing (WES) in 34 unrelated individuals with CRD (29 from Greece and five from Sweden). Genomic DNA was extracted from peripheral blood leukocytes according to standard procedures, and then exomic libraries (SureSelect V5 kit, Agilent) were sequenced on an Illumina HiSeq 2000. Raw sequence files were assessed, trimmed, and finally mapped back to the human genome reference sequence (build hg19); DNA variants were called and scored according to a specific in silico pipeline, described previously.7 Aggregate data analysis and variant filtering procedures (Tables S1 and S2 in the Supplemental Data available online) revealed biallelic mutations in two probands, one from Greece and another from Sweden, in CEP78 (centrosomal protein 78, composed of 16 exons for its longest coding isoform [GenBank: NM_001098802.1]). Both had classical signs and symptoms of CRD, clearly distinct from retinitis pigmentosa, as detailed below. Written informed consent was obtained from all individuals enrolled in this study, and approval for research on human subjects was obtained from the institutional review boards of all participating Institutions.
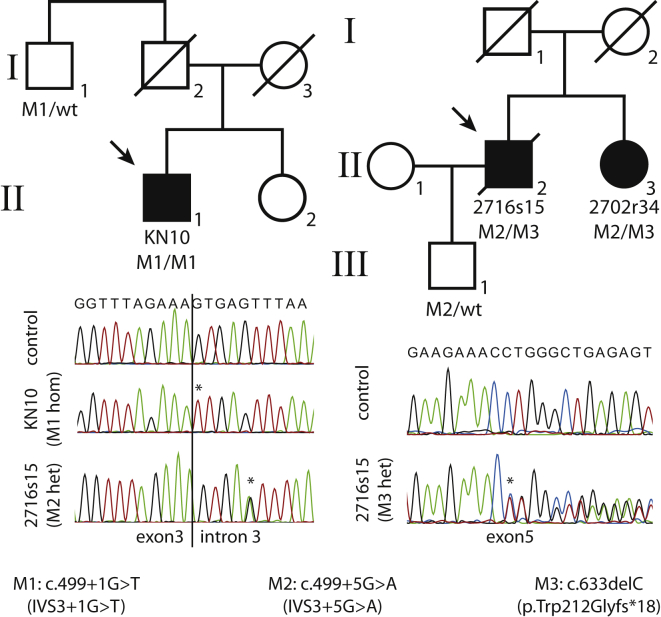
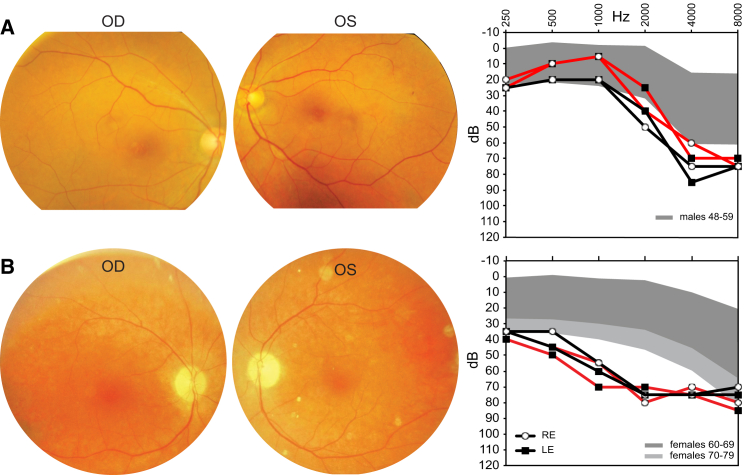
The Greek subject (KN10, individual II-1 on the left pedigree in Figure 1) was a 59-year-old male from the island of Crete and the eldest of two siblings of a non-consanguineous family. His sister was unaffected, and the family reported no history of retinal degeneration. Clinical history indicated hemarelopia since early adulthood (18–20 years of age); the condition progressed to severe central vision loss at the age of 35–40 years and evolved into severe visual impairment, nystagmus, and photophobia. Dyschromatopsia was also reported. Fundus examination at first visit showed normal color and normal vessels but a small atrophic foveal area with subjacent ring-like glistening in one eye and bull’s-eye maculopathy in the other eye. A few atrophic lesions were present in the inferior periphery in one eye (Figure 2). The 30° static automated perimetry revealed a diffuse suppression of the visual field in both eyes and a relative conservation of the peripapillary and superior periphery. Full-field electroretinography (ERG) showed flat cone responses but still some residual rod-mediated signals in the left eye. This person also complained about minor hearing problems, and his audiogram exhibited relatively mild deficit; nonetheless, such deficit was clearly distinct and more severe than natural age-related hearing loss (presbycusis)9 (Figure 2). KN10 carried a homozygous substitution in the first invariant base of intron 3 splice donor site c.499+1G>T (IVS3+1G>T) (Figure 1). This variant was located within a very small stretch of homozygosity that was not statistically significant for autozygosity, possibly indicating a mutational founder effect of geographic origin (not shown). The only relative who could be tested was his paternal uncle (individual I-1, left pedigree), who carried this DNA change heterozygously (Figure 1).
Figure 1.
CEP78 Mutations
Pedigrees and electropherograms of the identified DNA changes. Asterisks indicate the site of mutations. Abbreviations are as follows: Mx, mutant alleles; wt, wild-type allele.
Figure 2.
Clinical Features of the Analyzed Subjects
(A) Individual KN10. Fundus pictures (at age 53 years) reveal macular coalescent hypochromatic lesions in the right eye and minor macular changes in the left eye. Pure tone audiograms at age 57 years (black lines) and 59 years (red lines) show mild hearing impairment at higher frequencies compared to the normal range for gender and age, indicated by the shaded area.8
(B) Individual 2702r34. Fundus examination at age 65 years highlights attenuated vessels and degenerative changes in the posterior pole. Audiograms at age 66 years (black lines) and 77 years (red lines) show clear hearing loss at most frequencies. Abbreviations are as follows: OD, right eye; OS, left eye; RE, right ear; and LE, left ear.
The Swedish proband (2716s15, individual II-2 on the right pedigree in Figure 1), now deceased, was last examined at 69 years of age. He was born from unaffected parents and was the first child of a kindred of two. His sister (2702r34, individual II-3, right pedigree), examined at age 65, also had retinal degeneration. Both had visual problems, including loss of color sensitivity and central vision, since childhood. Both also reported a hearing deficit since they were young, and both had hearing aids. Audiogram of the living Swedish subject at age 66 years revealed substantial sensorineural hearing loss, which did not seem to progress substantially over the following 11 years (Figure 2). Hospital records containing information on the hearing status of her deceased brother were destroyed upon his death. Fundus examination showed degenerative changes for both siblings in the macular region and some spicular pigment in the mid-periphery but fewer changes in the periphery (Figure 2). Progressive deterioration of the visual field was reported and documented as expanding from the center to the periphery. At last examinations, both siblings retained some residual vision at the periphery of the visual field, especially in dim-light conditions. Similar to the situation for the Greek subject, full-field ERG of both individuals highlighted almost no residual cone activity but still revealed some rod-mediated responses, even at these late ages. These siblings were compound heterozygotes for two CEP78 mutations: a frameshift-causing single-nucleotide deletion (c.633delC; p.Trp212Glyfs∗18) in exon 5 and an intronic base substitution (c.499+5G>A; IVS3+5G>A) in the vicinity of the donor site for intron 3, just four nucleotides away from the mutation identified in the Greek subject. Genetic examination of the proband’s son (individual III-1, right pedigree) uncovered the presence of this latter mutation in heterozygosis, confirming the biallelic nature of the changes detected in his father and his aunt (Figure 1).
Sanger sequencing of the entire reading frame of CEP78 in a cohort of 99 unrelated CRD-affected individuals of Swedish, Swiss, Dutch, and Pakistani ethnic background failed to identify any additional causative variants. The three mutations present in our two families were not detected in the genome of an internal control cohort of 350 unrelated individuals or in any other public database, including the 1000 Genomes Project, the Exome Variant Server (EVS), and the Exome Aggregation Consortium (ExAC) Browser, which reports sequencing data from more than 61,000 unrelated individuals. In addition, in silico assessment of the c.499+1G>T and c.499+5G>A mutations via two distinct web-based platforms, NNSPLICE 0.910 and Human Splicing Finder,11 predicted for both variants the abolishment of the donor splicing site for intron 3.
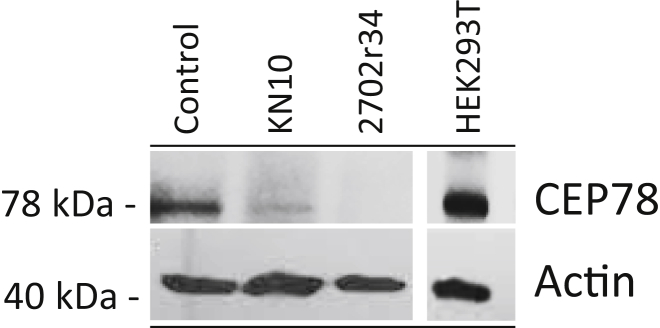
To analyze the functional consequences of the three mutations, we obtained fresh blood samples and skin biopsies from the Greek proband and the living Swedish subject and performed the following experiments. We first retrotranscribed total RNA from immortalized lymphoblasts (GoScript Reverse Transcriptase, Promega). Then, after performing saturating RT-PCR of the region spanning all mutations (primers: 5′-TTTTGCAGAAGTCGTGTTCCT-3′ and 5′-TTCAAGGGCCTCTAGCAAAG-3′), we cloned the amplified products in E. coli (Zero Blunt PCR Cloning Kits, Invitrogen) and performed colony PCRs and capillary electrophoresis on 96 clones (48 clones per affected individual). Representative samples were Sanger sequenced, and relative numbers of splicing events were assessed and quantified. The c.499+1G>T mutation resulted invariantly in the skipping of exon 3, leading to the production of an aberrant isoform, never reported in genomic databases, for which exons 2 and 4 were joined together. This event ablated 24 codons and altered the reading frame of CEP78, leading to the formation of a premature termination codon at nucleotides 16–18 of exon 4. Therefore, this non-canonical transcript was predicted to trigger nonsense-mediated mRNA decay (NMD)12 and result in no viable mRNA. The same exon-skipping occurrence was observed for the other, nearby mutation, c.499+5G>A, that was present in the Swedish subjects. Finally, the frameshift mutation c.633delC resulted in reduced mRNA amounts, as deduced by the low number of E. coli colonies carrying this cDNA clone (4 out of 48), again, probably as a result of the action of NMD. Immunoblot analysis in fibroblasts’ extracts (antibodies: A301-799A, Bethyl Laboratories, epitope between residues 550 and 600 and A2066, Sigma, for beta actin) revealed the presence of CEP78 in very reduced amounts in the Greek subject and the absence of any detectable band in the Swedish subject, in agreement with the mRNA findings described above (Figure 3). More specifically, the homozygous c.499+1G>T mutation probably resulted in a few canonical mRNA forms not detected by our cloning experiments, in turn producing small amounts of CEP78. Concerning the Swedish subject, it is likely that both the c.633delC and the c.499+5G>A alleles produced mostly non-viable mRNA and minimal quantities of wild-type mRNA and protein. In fact, overexposed films showed a faint band corresponding to CEP78, indicating that the protein was present in trace amounts (not shown).
Figure 3.
Immunoblot Analysis of Endogenous CEP78 in Fibroblasts from Affected Individuals
Numbers on the left refer to molecular-size markers. Control indicates human fibroblasts from a control individual; HEK293T indicates HEK293 cells containing SV40 large T antigen as a control for specificity of the anti-CEP78 antibody.
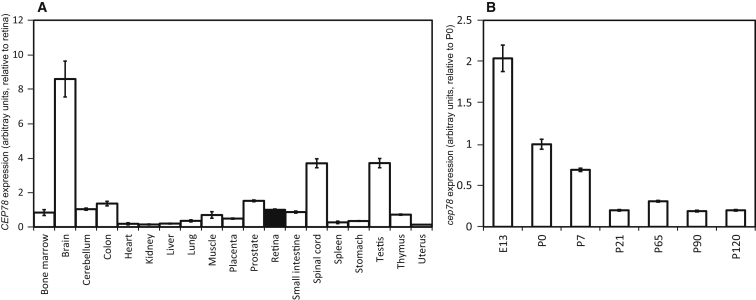
To gain insights into the relationship between vision and CEP78, we analyzed its expression in a panel of human tissues of cadaveric origin (Human Total RNA Master Panel II, Takara, primers 5′-GTTTCCCATTAATCAAAACACG-3′ and 5′-TCAACTTCAGAGGATGAAGGACT-3′ for CEP78 and 5′-AGAGTGGTGCTGAGGATTGG-3′ and 5′-CCCTCATGCTCTAGCGTGTC-3′ for the housekeeping gene GUSB). Although the number of CEP78 transcripts in the retina was higher than in many other tissues and organs, retinal CEP78 mRNA did not display the highest expression level (Figure 4). A time-course experiment on eyes of developing and postnatal mice (primers 5′-CTTCAGAAAGTGTCCAGGAAGC-3′ and 5′-GATCACTCTCTCCTCCTTCAGC-3′ for Cep78 and 5′-CCTAAGATGAGCGCAAGTTGAA-3′ and 5′-CCACAGGACTAGAACACCTGCTAA-3′ for the housekeeping gene Hprt1) revealed high expression at embryonic stages, followed by a progressive decrease at perinatal stages and by a plateau at adulthood (Figure 4). This pattern is reminiscent of the expression of other genes involved in retinal degenerations and in early biogenesis and homeostasis of the centriole, notably CEP76, CEP110, CEP164 (MIM: 614848), RAB8A (MIM: 165040), BBS4 (MIM: 600374), and RPGR (MIM: 312610).13 Although we could not obtain primary data on CEP78 expression in human cochlea, we assessed its RNaseq values from the only comprehensive transcriptome repository currently available for the inner ear.14 CEP78 displayed a FPKM (fragments per kilobase of exon per million reads mapped) value of 4.53 (average from three human cochleae), indicating moderate expression in this structure. Importantly, this FPKM value for CEP78 appeared to be higher than that of most genes already known to be associated with hereditary deafness (40 out of 70, or 57%), as assessed in the same organs and in the same conditions (Table S3).
Figure 4.
CEP78 mRNA Expression in Various Human Tissues and Organs and in the Developing Murine Eye
Data are from real-time PCR relative expression analysis, for which GUSB and Hprt1 were used as normalizing genes for (A) and (B), respectively.
Little is known about the function of CEP78. Identified as a component of the centrosome by two independent proteomic screenings,15, 16 CEP78 is composed of five leucine-rich repeats located at the N-terminal half of the protein, as well as a coiled-coil domain at the C terminus. An important study using Planaria as the main experimental model revealed that miRNA-based knockdown of CEP78 resulted in defective primary cilia assembly in flatworms and human RPE1 cells.17 Intriguingly, CEP78 was also found upregulated more than 5-fold by noise stress in rat cochlea.18 The function and impact of CEP78 in human physiology, however, remain largely elusive.
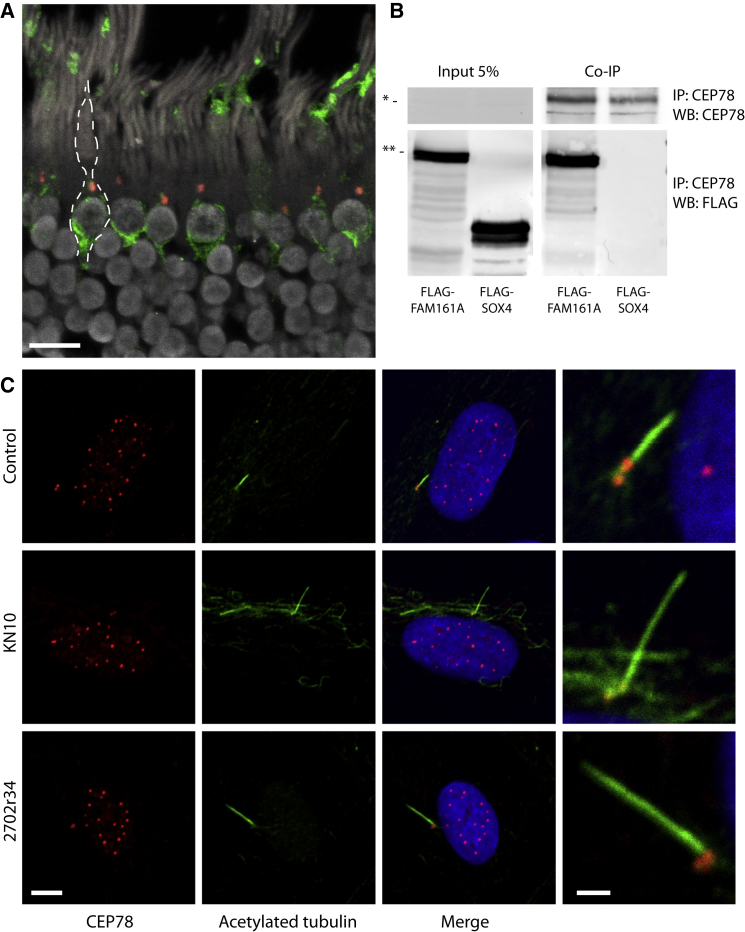
The reported centrosomal localization of CEP78 prompted us to investigate a possible role in relationship to the photoreceptor primary cilium. Immunofluorescence of human retinal sections with anti-CEP78 antibody (IHC-00364, Bethyl Laboratories, epitope between residues 550 and 600) and anti-cone arrestin (SC-54355, Santa Cruz) showed that CEP78 is present in dot-shaped foci in the inner segments, probably at the base of the primary cilium in retinal photoreceptors, predominantly cones (Figure 5 and Figure S1). This observation was confirmed when CEP78 was labeled together with acetylated tubulin, staining the primary cilium of human skin fibroblasts (Figure 5). Interestingly, positive staining was observed in fibroblasts from KN10 and 2702r34 as well, confirming that CEP78 was in fact expressed at the protein level in these individuals, as inferred (Figure 5). The mild differences between these experiments and the protein-expression observations might be due to different sensitivities of the two analytical tools and the use of distinct antibodies (A301-799A for immunoblot and IHC-00364 for immunofluorescence). No specific differences concerning CEP78 subcellular localization were observed in cells from affected individuals versus cells from controls.
Figure 5.
CEP78 in Human Cells and Its Interaction with FAM161A
(A) Immunostaining of CEP78 (red dots) and of cone arrestin (green) in a section of human retina. Margins of a cone photoreceptor are highlighted by a dotted line. The scale bar represents 10 μm.
(B). Co-immunoprecipitation of endogenous CEP78 and FLAG-tagged FAM161A in HEK293T cells. FLAG-SOX4 is a negative control. Abbreviations are as follows: IP:x, protein targeted by the antibody used in immunoprecipitation; and WB:x, protein or peptide targeted by the antibody used in immunoblots. The single and double asterisks indicate the expected molecular sizes for CEP78 (78 kDa) and the FLAG-FAM161A construct (90 kDa), respectively.
(C) Staining of CEP78 (red) and acetylated tubulin (green) in fibroblasts from a control individual, KN10, and 2702r34. CEP78 localizes at the centrioles and at the base of the induced primary cilium. The scale bars represent 5 and 1 μm for regular and magnification panels, respectively.
Presence at the base of the connecting cilium is a characteristic that is shared by other proteins associated with retinal degeneration, and in particular by FAM161A, the deficiency of which causes the RP28 form of retinitis pigmentosa (MIM: 606068).19, 20, 21 Indeed, tandem-affinity purification analysis performed with full-length FAM161A showed a positive interaction with CEP78,22 and co-immunoprecipitation with an anti-CEP78 antibody (A301-800A, Bethyl Laboratories, epitope between residues 639 and 689) in HEK293T cells transfected with full-length FLAG-FAM161A revealed direct binding between these two ciliary proteins (Figure 5).
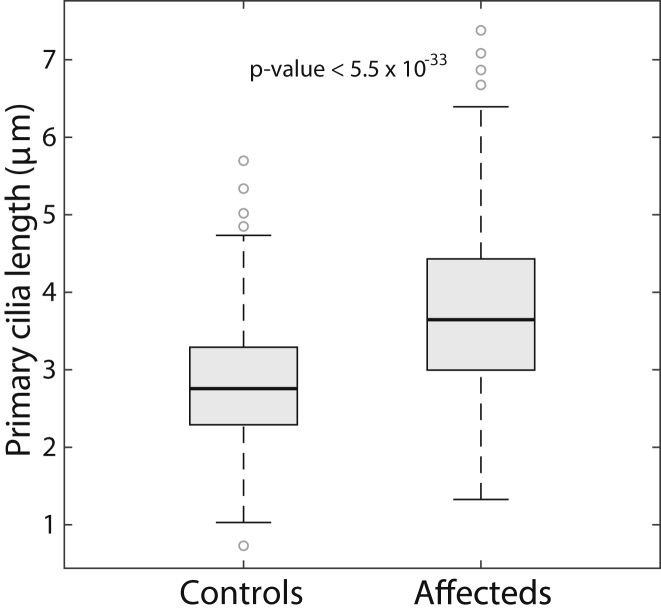
On the basis of these findings, we speculated that CRD due to mutations in CEP78 could be a consequence of hindered ciliary function, similar to what occurs in many other retinal degenerations.23 To test this hypothesis, we analyzed the morphology of primary cilia in fibroblasts derived from KN10 and 2702r34, with respect to four controls, after serum starvation. Unsupervised counting of at least 82 events per sample (207 events in affected individuals and 430 in controls) revealed that induced cilia in fibroblasts from KN10 and 2702r34 were significantly longer than those from control cells (Figure 6 and Figure S2), a phenomenon that has been previously associated with impaired function of this organelle. For instance, mutations in murine orthologs of BBS4, ICK, and TSC1, linked with ciliopathies such as Bardet-Biedl syndrome, endocrine-cerebro-osteodysplasia, and tuberous sclerosis, respectively, display kidney cells with elongated primary cilia.24, 25, 26
Figure 6.
Analysis of Ciliary Lengths
Fibroblasts from affected subjects display significantly longer primary cilia than those from four unaffected controls, suggesting impaired functionality.
In recent years, a significant number of hereditary conditions have been recognized to be the consequence of abnormalities of the cellular cilium. These diseases, collectively called ciliopathies, form a genetically heterogeneous spectrum of disorders affecting various tissues and organs, for instance kidney, cochlea, brain, and retina.23, 27 Classical examples of ciliopathies involving retina and other tissues are Usher syndrome (MIM: 276900, blindness and deafness) and Bardet-Biedl syndrome (BBS [MIM: 209900], blindness and multi-organ defects) for both of which vision loss is due to retinitis pigmentosa.28 In addition, syndromic ciliopathies such as Senior–Løken syndrome (SLS [MIM: 266900]), Joubert syndrome (JBTS [MIM: 213300]), and Jeune syndrome (JATD [MIM: 616300]) can occasionally be accompanied by retinal dystrophy and, in particular, retinitis pigmentosa and/or Leber congenital amaurosis (LCA [MIM: 204000]).29, 30, 31, 32 Another multi-organ ciliopathy is Alström syndrome (ALMS [MIM: 203800]),33 caused by null mutations in the gene ALMS1 (MIM: 606844). This disease is characterized by cone-rod degeneration, dilated cardiomyopathy, obesity, type 2 diabetes, and short stature, which can be accompanied by hepatosteatosis and defects in the lungs, kidney, and bladder.33, 34 Most cases also display progressive sensorineural hearing loss.35 Of interest, mutations in ALMS1 have recently been suggested as being causative of non-syndromic CRD.36
In this study, we show that mutations in CEP78 result in cone-rod degeneration associated with hearing loss, another hallmark of ciliopathy, but no other syndromic features. Interestingly, the two Swedish affected individuals had declared hearing loss, and the Greek subject had borderline hearing impairment. An intriguing possibility involves the presence of a genotype-phenotype correlation between CEP78 alleles and hearing (but not vision), as it is the case for instance for mutations in USH2A and ALMS1.36, 37, 38 Taken together, our data indicate that genetic defects in CEP78 define a newly recognized ciliopathy, distinct from Usher and Alström syndromes, affecting both the visual and the hearing systems.
Acknowledgments
This work was supported by the Swiss National Science Foundation (grant #156260, to C.R.), by the European Community’s Seventh Framework Programmes FP7/2009 under grant agreement #241955 (SYSCILIA) to R.R. and M.U., by the Netherlands Organization for Scientific Research (NWO Vici-865.12.005 to R.R), and by the Rotterdamse Stichting Blindenbelangen, the Stichting Blindenhulp, the Stichting A.F. Deutman Researchfonds Oogheelkunde, and the Stichting voor Ooglijders (to F.P.M.C. and M.I.K.). F.P.M.C. and M.I.K. were also supported by the following foundations: the Algemene Nederlandse Vereniging ter Voorkoming van Blindheid, the Landelijke Stichting voor Blinden en Slechtzienden, the Stichting Retina Nederland Fonds, and the Novartis fund, contributed through UitZicht. We would also like to acknowledge Drs. Andrea Superti-Furga and Luisa Bonafé from the Center for Molecular Diseases of the Lausanne University Hospital, Dr. Frauke Coppieters from the Ghent University Hospital, Dr. Guy Van Camp from the University of Antwerp, and Dr. Isabelle Schrauwen from the Translational Genomics Research Institute in Phoenix.
Published: September 1, 2016
Footnotes
Supplemental Data include two figures and three tables and are available with this article online at http://dx.doi.org/10.1016/j.ajhg.2016.07.009.
Accession Numbers
The mutations reported in this paper have been deposited in the Leiden Open Variation Database (LOVD) under variant ID numbers 0000119260, 0000119261, and 0000119262.
Web Resources
1000 Genomes, http://browser.1000genomes.org
ExAC Browser, http://exac.broadinstitute.org/
GenBank, http://www.ncbi.nlm.nih.gov/genbank/
Leiden Open Variation Database (LOVD), http://www.lovd.nl/3.0/home
NHLBI Exome Sequencing Project (ESP) Exome Variant Server, http://evs.gs.washington.edu/EVS/
OMIM, http://www.omim.org/
RetNet, https://sph.uth.edu/retnet/
Supplemental Data
References
- 1.Hamel C.P. Cone rod dystrophies. Orphanet J. Rare Dis. 2007;2:7. doi: 10.1186/1750-1172-2-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Berson E.L., Gouras P., Gunkel R.D. Progressive cone-rod degeneration. Arch. Ophthalmol. 1968;80:68–76. doi: 10.1001/archopht.1968.00980050070010. [DOI] [PubMed] [Google Scholar]
- 3.Krauss H.R., Heckenlively J.R. Visual field changes in cone-rod degenerations. Arch. Ophthalmol. 1982;100:1784–1790. doi: 10.1001/archopht.1982.01030040764011. [DOI] [PubMed] [Google Scholar]
- 4.Berson E.L. Retinitis pigmentosa. The Friedenwald Lecture. Invest. Ophthalmol. Vis. Sci. 1993;34:1659–1676. [PubMed] [Google Scholar]
- 5.Berger W., Kloeckener-Gruissem B., Neidhardt J. The molecular basis of human retinal and vitreoretinal diseases. Prog. Retin. Eye Res. 2010;29:335–375. doi: 10.1016/j.preteyeres.2010.03.004. [DOI] [PubMed] [Google Scholar]
- 6.Roosing S., Thiadens A.A., Hoyng C.B., Klaver C.C., den Hollander A.I., Cremers F.P. Causes and consequences of inherited cone disorders. Prog. Retin. Eye Res. 2014;42:1–26. doi: 10.1016/j.preteyeres.2014.05.001. [DOI] [PubMed] [Google Scholar]
- 7.Royer-Bertrand B., Castillo-Taucher S., Moreno-Salinas R., Cho T.J., Chae J.H., Choi M., Kim O.H., Dikoglu E., Campos-Xavier B., Girardi E. Mutations in the heat-shock protein A9 (HSPA9) gene cause the EVEN-PLUS syndrome of congenital malformations and skeletal dysplasia. Sci. Rep. 2015;5:17154. doi: 10.1038/srep17154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cruickshanks K.J., Wiley T.L., Tweed T.S., Klein B.E., Klein R., Mares-Perlman J.A., Nondahl D.M., The Epidemiology of Hearing Loss Study Prevalence of hearing loss in older adults in Beaver Dam, Wisconsin. Am. J. Epidemiol. 1998;148:879–886. doi: 10.1093/oxfordjournals.aje.a009713. [DOI] [PubMed] [Google Scholar]
- 9.Jerger J., Chmiel R., Stach B., Spretnjak M. Gender affects audiometric shape in presbyacusis. J. Am. Acad. Audiol. 1993;4:42–49. [PubMed] [Google Scholar]
- 10.Reese M.G., Eeckman F.H., Kulp D., Haussler D. Improved splice site detection in Genie. J. Comput. Biol. 1997;4:311–323. doi: 10.1089/cmb.1997.4.311. [DOI] [PubMed] [Google Scholar]
- 11.Desmet F.O., Hamroun D., Lalande M., Collod-Béroud G., Claustres M., Béroud C. Human Splicing Finder: an online bioinformatics tool to predict splicing signals. Nucleic Acids Res. 2009;37:e67. doi: 10.1093/nar/gkp215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hentze M.W., Kulozik A.E. A perfect message: RNA surveillance and nonsense-mediated decay. Cell. 1999;96:307–310. doi: 10.1016/s0092-8674(00)80542-5. [DOI] [PubMed] [Google Scholar]
- 13.Zhang S.S., Xu X., Liu M.G., Zhao H., Soares M.B., Barnstable C.J., Fu X.Y. A biphasic pattern of gene expression during mouse retina development. BMC Dev. Biol. 2006;6:48. doi: 10.1186/1471-213X-6-48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Schrauwen I., Hasin-Brumshtein Y., Corneveaux J.J., Ohmen J., White C., Allen A.N., Lusis A.J., Van Camp G., Huentelman M.J., Friedman R.A. A comprehensive catalogue of the coding and non-coding transcripts of the human inner ear. Hear. Res. 2016;333:266–274. doi: 10.1016/j.heares.2015.08.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Andersen J.S., Wilkinson C.J., Mayor T., Mortensen P., Nigg E.A., Mann M. Proteomic characterization of the human centrosome by protein correlation profiling. Nature. 2003;426:570–574. doi: 10.1038/nature02166. [DOI] [PubMed] [Google Scholar]
- 16.Jakobsen L., Vanselow K., Skogs M., Toyoda Y., Lundberg E., Poser I., Falkenby L.G., Bennetzen M., Westendorf J., Nigg E.A. Novel asymmetrically localizing components of human centrosomes identified by complementary proteomics methods. EMBO J. 2011;30:1520–1535. doi: 10.1038/emboj.2011.63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Azimzadeh J., Wong M.L., Downhour D.M., Sánchez Alvarado A., Marshall W.F. Centrosome loss in the evolution of planarians. Science. 2012;335:461–463. doi: 10.1126/science.1214457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Han Y., Hong L., Zhong C., Chen Y., Wang Y., Mao X., Zhao D., Qiu J. Identification of new altered genes in rat cochleae with noise-induced hearing loss. Gene. 2012;499:318–322. doi: 10.1016/j.gene.2012.02.042. [DOI] [PubMed] [Google Scholar]
- 19.Bandah-Rozenfeld D., Mizrahi-Meissonnier L., Farhy C., Obolensky A., Chowers I., Pe’er J., Merin S., Ben-Yosef T., Ashery-Padan R., Banin E., Sharon D. Homozygosity mapping reveals null mutations in FAM161A as a cause of autosomal-recessive retinitis pigmentosa. Am. J. Hum. Genet. 2010;87:382–391. doi: 10.1016/j.ajhg.2010.07.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Langmann T., Di Gioia S.A., Rau I., Stöhr H., Maksimovic N.S., Corbo J.C., Renner A.B., Zrenner E., Kumaramanickavel G., Karlstetter M. Nonsense mutations in FAM161A cause RP28-associated recessive retinitis pigmentosa. Am. J. Hum. Genet. 2010;87:376–381. doi: 10.1016/j.ajhg.2010.07.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Di Gioia S.A., Letteboer S.J., Kostic C., Bandah-Rozenfeld D., Hetterschijt L., Sharon D., Arsenijevic Y., Roepman R., Rivolta C. FAM161A, associated with retinitis pigmentosa, is a component of the cilia-basal body complex and interacts with proteins involved in ciliopathies. Hum. Mol. Genet. 2012;21:5174–5184. doi: 10.1093/hmg/dds368. [DOI] [PubMed] [Google Scholar]
- 22.Di Gioia, S.A. (2013). Targeted sequence capture and ultra high throughput sequencing for gene discovery in inherited diseases. PhD Thesis (University of Lausanne, Lausanne, Switzerland).
- 23.Wright A.F., Chakarova C.F., Abd El-Aziz M.M., Bhattacharya S.S. Photoreceptor degeneration: Genetic and mechanistic dissection of a complex trait. Nat. Rev. Genet. 2010;11:273–284. doi: 10.1038/nrg2717. [DOI] [PubMed] [Google Scholar]
- 24.Armour E.A., Carson R.P., Ess K.C. Cystogenesis and elongated primary cilia in Tsc1-deficient distal convoluted tubules. Am. J. Physiol. Renal Physiol. 2012;303:F584–F592. doi: 10.1152/ajprenal.00141.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Moon H., Song J., Shin J.O., Lee H., Kim H.K., Eggenschwiller J.T., Bok J., Ko H.W. Intestinal cell kinase, a protein associated with endocrine-cerebro-osteodysplasia syndrome, is a key regulator of cilia length and Hedgehog signaling. Proc. Natl. Acad. Sci. USA. 2014;111:8541–8546. doi: 10.1073/pnas.1323161111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mokrzan E.M., Lewis J.S., Mykytyn K. Differences in renal tubule primary cilia length in a mouse model of Bardet-Biedl syndrome. Nephron, Exp. Nephrol. 2007;106:e88–e96. doi: 10.1159/000103021. [DOI] [PubMed] [Google Scholar]
- 27.Waters A.M., Beales P.L. Ciliopathies: An expanding disease spectrum. Pediatr. Nephrol. 2011;26:1039–1056. doi: 10.1007/s00467-010-1731-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Koenig R. Bardet-Biedl syndrome and Usher syndrome. Dev. Ophthalmol. 2003;37:126–140. doi: 10.1159/000072043. [DOI] [PubMed] [Google Scholar]
- 29.Bachmann-Gagescu R., Dempsey J.C., Phelps I.G., O’Roak B.J., Knutzen D.M., Rue T.C., Ishak G.E., Isabella C.R., Gorden N., Adkins J., University of Washington Center for Mendelian Genomics Joubert syndrome: a model for untangling recessive disorders with extreme genetic heterogeneity. J. Med. Genet. 2015;52:514–522. doi: 10.1136/jmedgenet-2015-103087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bard L.A., Bard P.A., Owens G.W., Hall B.D. Retinal involvement in thoracic-pelvic-phalangeal dystrophy. Arch. Ophthalmol. 1978;96:278–281. doi: 10.1001/archopht.1978.03910050146008. [DOI] [PubMed] [Google Scholar]
- 31.Wilson D.J., Weleber R.G., Beals R.K. Retinal dystrophy in Jeune’s syndrome. Arch. Ophthalmol. 1987;105:651–657. doi: 10.1001/archopht.1987.01060050069040. [DOI] [PubMed] [Google Scholar]
- 32.Hildebrandt F., Zhou W. Nephronophthisis-associated ciliopathies. J. Am. Soc. Nephrol. 2007;18:1855–1871. doi: 10.1681/ASN.2006121344. [DOI] [PubMed] [Google Scholar]
- 33.Marshall J.D., Muller J., Collin G.B., Milan G., Kingsmore S.F., Dinwiddie D., Farrow E.G., Miller N.A., Favaretto F., Maffei P. Alström syndrome: Mutation spectrum of ALMS1. Hum. Mutat. 2015;36:660–668. doi: 10.1002/humu.22796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Marshall J.D., Maffei P., Collin G.B., Naggert J.K. Alström syndrome: genetics and clinical overview. Curr. Genomics. 2011;12:225–235. doi: 10.2174/138920211795677912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Marshall J.D., Bronson R.T., Collin G.B., Nordstrom A.D., Maffei P., Paisey R.B., Carey C., Macdermott S., Russell-Eggitt I., Shea S.E. New Alström syndrome phenotypes based on the evaluation of 182 cases. Arch. Intern. Med. 2005;165:675–683. doi: 10.1001/archinte.165.6.675. [DOI] [PubMed] [Google Scholar]
- 36.Lazar C.H., Kimchi A., Namburi P., Mutsuddi M., Zelinger L., Beryozkin A., Ben-Simhon S., Obolensky A., Ben-Neriah Z., Argov Z. Nonsyndromic early-onset cone-rod dystrophy and limb-girdle muscular dystrophy in a consanguineous Israeli family are caused by two independent yet linked mutations in ALMS1 and DYSF. Hum. Mutat. 2015;36:836–841. doi: 10.1002/humu.22822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Rivolta C., Sweklo E.A., Berson E.L., Dryja T.P. Missense mutation in the USH2A gene: association with recessive retinitis pigmentosa without hearing loss. Am. J. Hum. Genet. 2000;66:1975–1978. doi: 10.1086/302926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Lenassi E., Vincent A., Li Z., Saihan Z., Coffey A.J., Steele-Stallard H.B., Moore A.T., Steel K.P., Luxon L.M., Héon E. A detailed clinical and molecular survey of subjects with nonsyndromic USH2A retinopathy reveals an allelic hierarchy of disease-causing variants. Eur. J. Hum. Genet. 2015;23:1318–1327. doi: 10.1038/ejhg.2014.283. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.