Abstract
Adrenocortical carcinoma (ACC) is a rare malignancy that is generally associated with a poor prognosis whose existence dictates the management of incidental renal masses. We report a case of ACC diagnosed and treated at its apparent inception in a patient undergoing close surveillance imaging of a prior malignancy. Despite timely detection and resection of a localized ACC this patient rapidly progressed to systemic disease. This case highlights the rapid growth kinetics of ACC and puts into perspective the challenges associated with the established treatment paradigm for patients diagnosed with an adrenal mass.
Keywords: Adrenocortical carcinoma, Adrenal cancer, Incidental adrenal mass, Incidentaloma
Introduction
Adrenocortical carcinoma (ACC) is an uncommon malignancy with an estimated incidence of 0.5–2 per million.1 Meanwhile, benign adrenal masses are present in >5% of the elderly population.2 Despite rarity of ACC, the possibility of its existence dictates the management of incidentally discovered adrenal lesions. Indeed, indications for surgical resection such as adrenal mass growth greater than 1 cm and tumor size greater than 4 cm aim to achieve ACC cure prior to metastatic progression.3 Here, we present a case of a 3.8 cm ACC that was diagnosed at its apparent inception in a patient with lung cancer who underwent frequent surveillance cross-sectional imaging, and despite timely treatment, rapidly progressed to systemic disease.
Case presentation
A 73-year-old woman with hypertension and history of non-small cell lung adenocarcinoma (T1bN0M0, Stage I), resected 2.5 years previously, was referred to the urologic oncology clinic with a rapidly growing, asymptomatic left adrenal mass. The initial concern was for a solitary metastasis of lung cancer to the adrenal gland. At the time of referral, the left adrenal mass measured 2.3 × 3 cm and exhibited attenuation of 35 HU on non-contrast imaging (Fig. 1). PET-CT demonstrated intense FDG avidity (11.3 SUV) within the corresponding lesion (Fig. 2). Otherwise, imaging of the brain, thorax, abdomen and pelvis were unremarkable. In retrospect, an adrenal mass was present on the patient's previous scan, 6-months prior, and measured 1.1 cm, demonstrating lipid-poor characteristics (Fig. 1). This same mass was detected at initial presentation, 3 years prior, was not FDG avid, and remained stable in size on numerous 6-month interval surveillance imaging studies. Adrenal metabolic work-up at the time of referral was significant for inappropriate suppression of serum cortisol on low-dose dexamethasone suppression test (8.74 mcg/dL, normal < 5 mcg/dL). Plasma free metanephrines, serum aldosterone, and adrenal sex steroid testing with dehydroepiandrosterone sulfate (DHEA-S), 17-hydroxyprogesterone, androstenedione, testosterone and 17-beta estradiol were unremarkable. The patient underwent an uneventful laparoscopic left adrenalectomy within 4 weeks of being seen in consultation. Pathologic examination revealed a high grade 3.8 cm adrenocortical carcinoma with venous invasion and negative surgical margins. As per the standard of care, the patient received adjuvant mitotane. After two months of adjuvant therapy, the patient was found to have progressive disease with extensive metastatic disease to the liver detected on cross-sectional imaging (Fig. 3) and confirmed on fine needle aspiration biopsy. The patient subsequently received two cycles of etoposide, cisplatin, doxorubicin (ECD) systemic chemotherapy. Due to rapid disease progression, treatment was suspended after two cycles, and the patient expired 10 months following adrenalectomy.
Figure 1.
Computed Tomography (CT) imaging of adrenal mass. (a) Axial contrast-enhanced image depicting 1.1 cm adrenal mass that had remained stable for several years on surveillance imaging. (b–c) Axial and coronal CT imaging at time of referral demonstrating a 2.3 × 3.3 cm lipid poor adrenal mass (non-contrast CT attenuation 35 HU).
Figure 2.
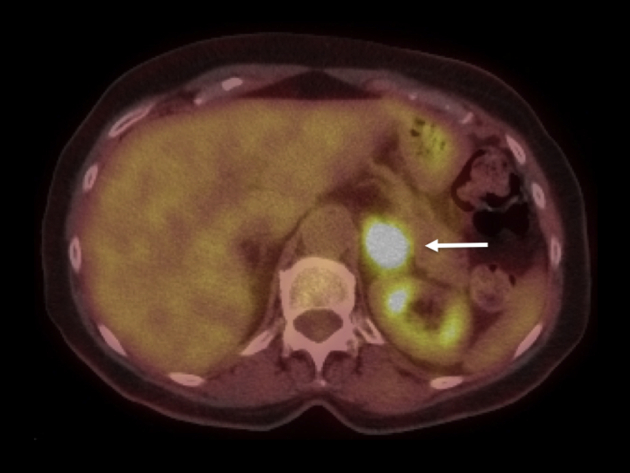
Positron Emission Tomography/CT imaging displaying avid FDG uptake (11.3 SUV) in the adrenal mass (arrows). No other pathologic FDG uptake was noted elsewhere in the body.
Figure 3.
Axial and coronal CT imaging demonstrates diffuse metastatic disease within the liver parenchyma (arrows).
Discussion
We report a unique case of an ACC that was detected and removed at its apparent inception. Although a stable ∼1 cm mass was present on the adrenal gland of our patient for several years, transformation of this lesion into a rapidly growing malignancy vs. development of a new adjacent aggressive lesion was noted on biannual cross-sectional imaging. Despite timely surgical intervention for clinically localized disease that measured <4 cm at resection, this patient's malignancy exhibited rapid systemic progression. This case underscores breakneck ACC disease progression kinetics and the short, and arguably in some cases non-existent, window of therapeutic opportunity in patients with this malignancy. Indeed, our case dovetails with previous reports from administrative datasets that have documented lack of both stage migration and absence of improvement in survival for patients with ACC over the last several decades despite advent of ubiquitous cross-sectional imaging.4
Since oncologic risks currently drive management decisions in patients with adrenal mass, this case highlights shortcomings of the current treatment paradigm.5 Indeed, thousands of patients are annually subjected to risks of adrenalectomy,6 based on current management guidelines, in order to potentially affect outcomes of less than 100 patients who present each year with small (<6 cm) ACC in the United States.7 This case highlights that favorable oncologic outcomes are elusive even in patients who receive timely surgical extirpation for localized ACC.
Conclusion
This is a rare case where inception of an adrenal cortical carcinoma was incidentally witnessed during close radiographic surveillance of another malignancy. Despite timely resection, this patient rapidly progressed to systemic disease and died from ACC within 1 year of surgery. This report underscores a need to better calibrate and balance risks of delaying ACC treatment against the burden of overtreatment of patients with benign adrenal mass.
References
- 1.Siegel R.L., Miller K.D., Jemal A. Cancer statistics, 2015. CA Cancer J Clin. 2015;65(1):5–29. doi: 10.3322/caac.21254. [DOI] [PubMed] [Google Scholar]
- 2.Young W.F. Clinical practice. The incidentally discovered adrenal mass. N Engl J Med. 2007;356(6):601–610. doi: 10.1056/NEJMcp065470. [DOI] [PubMed] [Google Scholar]
- 3.Kutikov A., Crispen P.L., Uzzo R.G. Pathophysiology, evaluation, and medical management of adrenal disorders. In: Wein A.J., editor. Campbell–Walsh Urology. 11th ed. Elsevier; Philadelphia: 2015. [Google Scholar]
- 4.Kutikov A., Mallin K., Canter D., Wong Y.-N., Uzzo R.G. Effects of increased cross-sectional imaging on the diagnosis and prognosis of adrenocortical carcinoma: analysis of the national cancer database. J Urol. 2011;186(3):805–810. doi: 10.1016/j.juro.2011.04.072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kutikov A., Mehrazin R., Uzzo R.G. Assessment and management of an adrenal mass in urological practice. AUA Update Ser. 2014;33:1–8. [Google Scholar]
- 6.Simhan J., Smaldone M.C., Canter D.J. Trends in regionalization of adrenalectomy to higher volume surgical centers. J Urol. 2012;188(2):377–382. doi: 10.1016/j.juro.2012.03.130. [DOI] [PubMed] [Google Scholar]
- 7.Canter J.D., Mallin K., Uzzo G.R. Association of tumor size with metastatic potential and survival in patients with adrenocortical carcinoma: an analysis of the national cancer database. Can J Urol. 2013;20(5):6915–6921. [PubMed] [Google Scholar]




