Abstract
Background
Protracted methamphetamine (MA) use is associated with decreased control over drug craving and altered brain volume in the frontostriatal network. However, the nature of volumetric changes following a course of psychological intervention for MA use is not yet known.
Methods
66 males (41 MA patients, 25 healthy controls, HC) between the ages of 18–50 were recruited, the MA patients from new admissions to an in-patient drug rehabilitation centre and the HC via public advertisement, both in Cape Town, South Africa. 17 MA patients received 4 weeks of treatment as usual (TAU), and 24 MA patients completed TAU plus daily 30-minute cognitive training (CT) using an N-back working memory task. Magnetic resonance imaging (MRI) at baseline and 4-week follow-up was acquired and voxel-based morphometry (VBM) was used for analysis.
Results
TAU was associated with larger bilateral striatum (caudate/putamen) volume, whereas CT was associated with more widespread increases of the bilateral basal ganglia (incorporating the amygdala and hippocampus) and reduced bilateral cerebellum volume coinciding with improvements in impulsivity scores.
Conclusions
While psychological intervention is associated with larger volume in mesolimbic reward regions, the utilisation of additional working memory training as an adjunct to treatment may further normalize frontostriatal structure and function.
Highlights
-
•
Working memory training over 4 weeks is associated with larger basal ganglia volume in methamphetamine users.
-
•
Treatment as usual is associated with larger bilateral putamen and smaller cerebellar volumes.
-
•
Working memory training coincides with improvements in self-reported impulsivity and self-regulation.
1. Introduction
Protracted methamphetamine (MA) use is associated with craving, risky behaviour and executive dysfunction (Dean et al., 2015, Mahoney et al., 2015, Semple et al., 2011) as well as deficits in self-regulatory control (Baicy and London, 2007, Morales et al., 2015). However, little is known about the structural brain changes associated with psychological interventions and adjuncts to treatment such as working memory (WM) training that together aim to improve neuropsychological deficits in those with MA use (Brooks, 2015). The frontostriatal circuitry is associated with WM function (Brooks, 2015, Ersche et al., 2012, Dahlbom et al., 2009, Groman et al., 2013) and is impaired following MA exposure in prenatally exposed children (Kwiatkowski et al., 2014), adolescents (Lyoo et al., 2015) and adults (Morales et al., 2015). MA adult users typically have smaller prefrontal cortex and larger striatal volumes (Morales et al., 2012, London et al., 2014), which may reflect dopamine-related neurotoxicity (Morales et al., 2015). In line with this, MA use is associated with reduced striatal dopamine transporter (DAT) and receptor availability (Morales et al., 2015, Ballard et al., 2015, Yuan et al., 2015). There is also some evidence that molecular alterations in the striatum involving inhibited expression of brain derived neurotrophic factor [BDNF] and dopamine D2 receptor levels may occur following MA use (Thompson et al., 2015). Such molecular alterations may present as altered brain volume, which in turn may be associated with difficulties faced by standard psychological interventions to curtail prevailing high rates of attrition and relapse (London et al., 2014, Plüddemann and C.D.H, 2012, Panenka et al., 2013).
Abstinence from MA acutely increases caudate and putamen and decreases prefrontal cortex volumes in MA dependent individuals (Morales et al., 2012, London et al., 2014), which could be associated with microglial and other neural processes involved in rapid reorganisation prior to neurogenesis (Nixon et al., 2008), and also with the risk of relapse. However, the influence of psychological intervention on brain processes in contrast to abstinence alone may differentially alter brain volume, but this is not yet known. For example, it is not known whether there is larger or smaller volume in the frontostriatal circuitry following treatment to reflect alterations in neurotoxicity, DA transporter (DAT) levels, receptor regulation or reorganisation of regional brain networks. Thus, by examining how psychological intervention and adjunctive WM training (associated with frontostriatal function (Brooks, 2015, Ersche et al., 2012, Dahlbom et al., 2009, Groman et al., 2013)) alters brain volume it might be possible to isolate the neurobiological markers associated with treatment efficacy. Psychological interventions aim to alter neural processes and enhance problem-solving, self-representation and affect regulation. For example, greater prefrontal cortex and lesser limbic activation has been reported following cognitive behavioural therapy treatment for anxiety disorders (Brooks and Stein, 2015), which are often comorbid with SUD (Harro, 2015). It is pertinent to consider here that the most common factors for relapse and attrition in those who use MA are poor attention and risky decision making (Chen et al., 2015), which is associated, in part, with dysfunction in the frontostriatal network (Kohno et al., 2015) and concomitantly deficits in WM.
Against this background, our group has recently shown that cognitive training (CT) with a WM task improves self-reported impulsivity and self-regulation in those with MA use (Brooks et al., n.d.). To progress this work, here we examine whether the same CT as an adjunct to treatment as usual (TAU) alters brain volume in patients receiving treatment for MA use. Additionally, we aim to examine how brain changes are associated with improvements in impulsivity and self-regulation.
To aid the formulation of our hypotheses we referred to a recent meta-analysis of WM training in both HC and patients with schizophrenia that demonstrated that greater activation incorporating fronto-parietal networks, the DLPFC and anterior cingulate (ACC), as well as the striatum, are associated with neuroplasticity changes (Li et al., 2015). Furthermore, CT is consistently reported to improve cognitive function in those with psychosis (Keshavan et al., 2014) and attention deficit hyperactivity disorder (ADHD) (Klingberg, 2010, Shinaver et al., 2014, Spencer-Smith and Klingberg, 2015), which are highly comorbid with regular MA use (Harro, 2015, Hides et al., 2015) and so CT is relevant for our study population. While the transferability of CT to general cognitive improvement is debated, specific training that targets localised brain regions and functions might be most effective for those with MA dependence (Karbach and Unger, 2014). Moreover, frontostriatal circuitry, as well as parietal, insula and cerebellar activation is associated with WM function, as demonstrated in a term-based search (“working memory”) of the ‘neurosynth’ database (http://www.neurosynth.org/analyses/terms/), yielding over 900 fMRI studies of WM, which additionally aided the formulation of our hypotheses. WM supports the management of distracting internal representations (Brooks, 2015, Chudasama and Robbins, 2006), such as drug craving and attention to drug paraphernalia. Thus, specifically utilising a WM task as an adjunct to treatment has the potential to strengthen neural processes involved in self-regulation in the presence of distractors in those being treated for MA use.
WM training lowers impulsivity in those with substance use disorders (Brooks, 2015, Brooks et al., n.d, Bickel et al., 2011), and improves attention in those with attentional deficits and the general public, with the current leader in the field of attentional deficits being CogMed™ (Klingberg, 2010, Spencer-Smith and Klingberg, 2015). However, the CogMed™ package was not implemented during this study because it utilises a selection of WM tasks, whereas our task utilises one task, and we considered that it may be more beneficial, manageable within treatment schedules and less anxiety-provoking for the patients to focus on one WM task that activates a specific brain region. For example, in a meta-analysis of 24 functional magnetic resonance imaging (fMRI) studies using the N-back task, the frontostriatal circuitry is typically activated (Owen et al., 2005), whereas it is not yet entirely clear which distinct brain regions are activated by CogMed. Therefore, for this study we have used our own modified WM training based on the N-back task called ‘Curb Your Addiction (C-Ya)’for CT intervention during TAU. Finally, while fMRI studies have demonstrated that WM training alters brain function in the prefrontal cortex corresponding to occupational changes after 6 months in adults with schizophrenia for example (Subramaniam et al., 2014), with one fMRI study underway in 7 year-old children born preterm using CogMed™ (Pascoe et al., 2013), there has been no evidence to date regarding potential structural brain changes associated with WM training in adults who use MA.
Thus, as well as measuring the effects of abstinence during standard psychological intervention on brain volume in patients being treated for MA dependence we have additionally examined the effects of adjunctive CT using an N-back WM task. Our aim was to measure how brain volume is altered by standard psychological TAU, and whether adjunctive CT is associated with additional brain changes. We also explored whether brain changes are related to changes in impulsivity, self-regulation and mood. Thus, against the research background presented above, our hypotheses are that: a) smaller frontal and larger striatal volumes in MA using patients at baseline (e.g. at the beginning of treatment) will correspond with higher impulsivity and lower self-regulation scores; b) by comparison to TAU, the CT group at 4-weeks' follow-up will have altered frontostriatal volumes corresponding to greater improvements on impulsivity and self-regulation measures.
2. Methods and materials
2.1. Participants
66 males between the ages of 18–50 were recruited for the study from January 2013 to September 2014 in Cape Town, South Africa. In-patients had a history of MA use (n = 41) and attended a local rehabilitation clinic. SUD by way of MA use was measured firstly at clinical interview by qualified psychologists, and secondly during the study phase by a qualified psychiatrist who administered the Structured Clinical Interview for Diagnosis (SCID) [see below]. Healthy controls (HC, n = 25) were local members of the public matched by age and gender. Selection of the MA use group was conducted via admission lists by clinicians in the second week of admittance to the in-patient facility. Most commonly in-patients were polysubstance users, or other primary substance users such as heroin or cocaine, and so researchers were required to wait for a potential participant whose primary substance of use was MA, identified by the clinical staff. Upon identification of a potential participant, the study was summarized to the patient by the lead clinician based on an information leaflet provided by the research team. Following this a researcher took informed consent and the study procedures commenced. The study for both MA users and HC began with a SCID interview by a qualified clinical researcher to confirm primary drug use, other comorbidities (e.g. anxiety, depression) and smoking status. Participants were excluded from further study procedures at this stage if they did not meet the inclusion/exclusion criteria as described below. The average duration of MA use in our participants prior to admission was 9.69 (s.d. 3.8) years – although an accurate average amount of drug taking could not be ascertained as most patients did not know exactly when they started consuming MA. All in-patients, while recent users of MA, were abstinent for two weeks (confirmed by clinicians via urine sampling at the clinic) when commencing our study. The MA group at baseline was divided (alternated in the order that they were admitted to the clinic) into two groups by the researcher: those who would receive TAU (n = 17) and those who would additionally to TAU receive a CT WM intervention (n = 24) as described below. At baseline, participants completed a battery of validated psychological questionnaires to determine levels of self-reported impulsivity, self-regulation, anxiety, depression, happiness, desire for MA and feelings of self-control: at the clinic if in the MA group, and at the university research offices if in the HC group. At a 4-week follow-up session the TAU and CT groups repeated the same questionnaire battery.
Of these participants, several were excluded prior to analyses due to failure to meet inclusion/exclusion criteria, inadequate scan quality, participant drop-out prior to follow-up and equipment failure at the scanner to record the log file. See Supplementary CONSORT diagram.
Inclusion/exclusion criteria for the MA group were: a) MA was the primary substance of use; b) no history of alcohol use/dependence, although participants were permitted to have concomitant cannabis/methaquolone use and/or infrequent alcohol use (as determined by clinical screening); c) no current or previous history of psychosis as confirmed by clinical staff at an admission interview and by researcher interview; d) no prescribed medication during the study.
Inclusion/exclusion criteria for the HC group were: a) no history of substance or alcohol use disorder, b) no history of an Axis I DSM-IV psychiatric diagnosis, c) no previous neurological condition.
All participants were required to be fluent in English, to be left-handed and to have a negative HIV diagnosis, as clarified by clinical staff. At the end of their participation, all participants at baseline received R150 (South African currency, approximately equivalent to $10) in food vouchers and the MA group who completed the 4-week follow-up (e.g. TAU or CT) received an additional R150 food vouchers. The study adhered to guidelines as set out in the Declaration of Helsinki, and was approved locally by the University of Cape Town Human Research Ethics Committee (Ref: 554/2012).
2.2. Clinical setting
Patients were recruited from an in-patient rehabilitation clinic in the Cape Town area that houses a maximum of 40 patients (male and female). The programme at the clinic ran over 8 weeks, during which time patients were provided with 6 meals a day up to 3500 cal, consisting of a large meal at breakfast, supper, lunch and 3 snacks. TAU at the clinic involved 1 h sessions (on each weekday) of dialectical behavioural therapy (DBT) for 6 weeks/30 h at the clinic. DBT is a form of cognitive-behavioural therapy with more emphasis on addressing maladaptive affect regulation, and has demonstrated success in treating substance use disorder (Shearin and Linehan, 1994). Typically, DBT provides skills training in a group, during individual therapy, via telephone coaching and as part of a therapist consultation team. There are normally 4 sets of behavioural skills taught during DBT, namely a) mindfulness, b) distress tolerance, c) interpersonal effectiveness and d) emotion regulation. Greater WM capacity is associated with heightened cognitive control and affect regulation and/or suppression (Brooks, 2015) and therefore WM training is a useful adjunct to DBT that attempts to improve such skills. Additionally, patients attended daily group sessions, psychotherapy, basic skills development and both physical and leisure activities.
2.3. CT group – working memory (WM) training using “Curb Your Addiction (C-Ya)”computerized task
In addition to TAU, the CT group received training in a classroom at the clinic, using a computer based WM task called “Curb Your Addiction (C-Ya)” that was developed by the authors with Fontera Digital Works (www.fontera.com). Copies of the software are available upon request (http://www.drsamanthabrooks.com). C-Ya is a modified version of the N-back task (the modification being a distracting peripheral mosaic to mimic peripheral distraction in real life), and for the training in the present study we used standard levels 0-back through to 3-back. The N-back task was originally introduced by Kirchner (1958) and requires a response to a specified target letter as single letters appear on the screen consecutively. In the present study the letter ‘X’ was the target for ‘0-back’; the target for ‘1-back’ was when the current letter was the same as the ‘1 before’; the target for ‘2-back’ was when the current letter was the same as ‘2 before’ and ‘3 before’ for ‘3-back’. Targets were identified by pressing the space bar on the computer keyboard. During our standard version of the C-Ya task participants begin by completing 30 min of 0-back and they progress the next day on to the consecutively higher level after achieving at least 80% accuracy on the prior level. An 80% threshold was set for our study because in a previous publication that documented the effects of WM training on neural function the highest level of accuracy attained was 80%. Therefore, we decided to use this as a guideline for participant progression through the levels in our study (Olesen and Westerberg, 2003). Accuracy was calculated using the following algorithm:
[1 − ((number of commissions + number of omissions) / total possible correct)] × 100 (Miller et al., 2009), where commissions were responses to non-target letters; omissions were failures to respond to a target, and total possible correct were the total target letters.
Participants in this study were required to engage in the task 5 times a week for 4 weeks (maximum 20 sessions). WM accuracy on the first and last CT day before the baseline and follow-up scan respectively was recorded to link WM function to brain volume changes during analyses as described below.
2.4. Questionnaire measures
2.4.1. Structured clinical interview for diagnosis of Axis I DSM-IV disorders (SCID-IV, (First et al., 2002)– patient version with psychotic screen, and non-patient version)
We selected patients who were identified by clinical staff to attend an interview with a researcher using the SCID for DSM-IV, which was conducted at the clinic by a qualified research scientist. For the HC group the SCID was conducted at the university research offices. The SCID included screening questions for substance abuse (including alcohol and other drugs), mood, thought, anxiety and general screening questions.
2.4.2. Hospital anxiety and depression scale (HADS)
The HADS is a 14-item questionnaire used to assess patients' levels of anxiety and depression (Zigmond and Snaith, 1983). 7 of the items relate to depression, 7 to anxiety. Items are rated on a 4 point scale, with a maximum score of 21 for both anxiety and depression. A score of 0–7 is ‘normal’, 8–10 is ‘borderline’ and 11 or higher is considered significant.
2.4.3. Barratt impulsivity scale (BIS)
The BIS is a 30-item questionnaire designed to assess an individual's impulsiveness (Patton et al., 1995). Items are scored on a four-point scale (rarely/never, occasionally, often, almost always/always) to give 6 first order factors (attention, motor, self-control, cognitive complexity, perseverance and cognitive instability) and 3-second order factors (attentional, motor and non-planning).
2.4.4. Self-Regulation Questionnaire (SRQ)
The SRQ is a 63-item questionnaire designed to assess an individual's self-regulatory processes (Brown et al., 1999), measuring 7 factors of self-regulation: a) receiving relevant information, b) evaluating information and comparing it to norms, c) triggering change, d) searching for options, e) formatting a plan, f) implementing the plan and g) assessing the plan's effectiveness. Items are scored on a 5-point scale (strongly disagree, disagree, unsure, agree, strongly agree) and participants are asked to respond based on how well each statement describes them. It has been verified to give good internal consistency and reliability in a sample of young adults (Carey et al., 2004).
2.4.5. Visual analogue scale (VAS)
The VAS is a psychometric response scale, used to assess subjective feelings (Tombaugh, 2004). In this study mood, desire for drug and feelings of self-control were assessed. Participants responded by placing a mark on a horizontal line to indicate their current feelings. The left end point of the line represents low mood, no desire for drug and no feelings of self-control, and the right end point represents high mood, high desire for drug and high feelings of self-control respectively. The position of the mark on the line was measured and transformed into a percentage for analysis purposes.
2.4.6. Trail making test (TMT)
The TMT is a paper-based neuropsychological measure of an individual's speed of processing, mental flexibility, executive function (e.g. working memory) visual searching and scanning abilities (Reips and Funke, 2008). The TMT consists of two parts; TMT-A and TMT-B. TMT-A requires participants to draw a line between 25 numbers evenly distributed on a piece of paper. TMT B instead requires participants to alternatively join numbers with letters (e.g. 1, A, 2, B, 3, C). The time taken to complete the task and the number of errors are recorded. To account for dexterity the results from TMT-A are subtracted from the results of TMT-B to produce a final score. We used this task to examine near transfer effects of WM training during the study.
2.4.7. Working memory accuracy
Each participant played Curb Your Addiction (www.drsamanthabrooks.com) for 12 min (alternating between 6 min of 0-back and 6 min of 1-back) to gauge basic competency on the task during the experimental procedures. Commission and omission errors were recorded to a log file and accuracy was calculated according to the algorithm described above.
2.5. MRI data acquisition and pre-processing
For the MRI scans a 1.5 Tesla Siemens Magnetom Allegra scanner with a 4-channel SENSE head coil was used. Subjects were imaged with a sagittal T1 weighted image, with 3.82 ms repetition time (TR), 4.74 ms echo time (ET), 90° flip angle, acquisition matrix size 200 × 200 × 200, 3 mm acquisition voxel size, 36 contiguous slices and slice thickness 3.5 mm. The nifti-converted T1-weighted images were first manually reoriented along the AC-PC plane and examined for adequate scan quality. Two participant scans were excluded for poor quality.
For cross-sectional (HC versus MA baseline) and the longitudinal (repeated measures baseline versus follow-up in the TAU and CT group) analyses, we used the VBM-8 module of the Statistical Parametric Mapping software package SPM (http://www.fil.ion.ucl.ac.uk/~john/misc/VBMclass10.pdf). For the cross-sectional analyses, individual T1 images were first aligned to a T1 template in Montreal Neurological Institute (MNI) space and subsequently segmented into grey matter, white matter and cerebro-spinal fluid. The grey matter images were normalized using the diffeomorphic image registration algorithm (DARTEL) (Ashburner, 2007) and modulated with the nonlinear transformation parameters as computed during the normalization procedures. Subsequent images contain the volume proportion of probabilistically assigned grey matter tissue for each voxel. These grey matter probability maps were visually inspected using the display function in SPM8 and finally smoothed with an 8-mm Gaussian kernel. Note that each image of the regional grey matter volume was corrected for individual brain size as per the VBM8 toolbox pipeline.
For the repeated measures analyses (baseline and follow-up in TAU and CT groups), MRI data processing was performed using the VBM8 longitudinal batch, which has specific preprocessing steps for repeated measures data. These steps are summarized below. Firstly, the follow-up image was registered to the baseline image for each participant in each group (TAU, CT). Secondly, the mean image was calculated from the realigned images for each participant, and this was used as a reference image for the subsequent spatial alignment. Thirdly, the realigned images were corrected for field inhomogeneity in relation to the reference mean image. Fourthly, tissue segmentation was performed in the bias-corrected mean reference image and the bias-corrected realigned images using the default MNI template. Fifthly, DARTEL spatial normalization parameters were estimated using the tissue segments (grey matter and white matter) of the bias-corrected mean reference image. Sixthly, normalization parameters were applied to the tissue segments of the bias-corrected realigned images. Finally, the resulting normalized tissue segments for each time point of each participant were smoothed with an 8-mm Gaussian kernel. To avoid possible edge effects between grey and white matter, all voxels with grey matter values < 0.1 were excluded using the absolute threshold masking option available in SPM8.
2.6. Statistical analyses
Normal distribution was examined with Shapiro-Wilks test and by examining boxplots. Parametric or non-parametric analyses were applied accordingly. The assumption of homogeneity of variance was assessed using Levene's test, and the Welch-Satterthwaite method was used for all measures where equal variances were not assumed in order to adjust the t-score and p-value.
2.7. t-Tests with demographic data
Data analyses were performed using IBM SPSS Software (www.ibm.com/software/analytics/spss) and Bonferroni corrected for multiple comparisons. Demographic data was assessed using t-tests and Chi-squared tests of frequency distribution. All questionnaire measures were assessed using student t-tests, and for all non-normally distributed data a Mann Whitney non-parametric t-test was performed. These were performed between the following groups: HC vs MA baseline, TAU baseline vs CT baseline, HC vs TAU follow-up, HC vs CT follow-up, TAU follow-up vs CT follow-up. Further paired sample t-tests were performed on the TAU and CT group between baseline and follow-up to determine the effects of 4 weeks of standard treatment. A Wilcoxon Signed Ranks test was performed on all non-normally distributed data. All measures were Bonferroni corrected according to each individual questionnaire.
2.8. VBM analyses
All analyses were deemed significant at the whole brain, cluster threshold Family Wise Error (FWE) level. First, a full factorial 2 × 2 ANCOVA (Group × WM Accuracy) was conducted in the total cohort to examine the main effect of group (HC and MA) and the main effect of WM accuracy (dichotomised by high/low, split by mean of each group). Covariates of no interest were age and depression score (due to its statistically significant difference between the groups). We chose to run the ANCOVA between HC and MA baseline separately, so as to examine baseline differences, and also given that the HC group was only scanned once as a normative comparison group. The next repeated measures ANCOVA was done to examine how TAU and CT alter brain volume in association to baseline MA.
A second full factorial 3 × 2 ANCOVA (Group × WM Accuracy) was conducted in all methamphetamine users to examine the main effect of group (MA, TAU and CT) and main effect of WM accuracy. Covariates of no interest were age and duration of drug taking (there was no significant difference in depression in the MA groups).
Finally, we conducted a 2 × 2 repeated measures ANCOVA to examine the interaction between group (TAU, CT) and timeline (baseline, follow-up).
3. Results
3.1. Demographic data
See Table 1 for demographic data. There was no significant difference in age between the HC (mean 27.67 years, s.d. 8.714) and total MA group (mean 28.42 years, s.d. 6.129). However, there were significant differences in education (Chi-squared = 48.891, p ≤ 0.001), with the HC group reaching graduate level education and the MA group reaching a highest qualification level of matriculation (e.g. University entrance level). There were also significant differences in ethnicity (Chi-squared = 41.155, p ≤ 0.001), with the HC group being mostly Caucasian, whereas the MA group were predominantly of mixed ancestry. There was no significant difference in age, duration drug taking, education or ethnicity between the baseline and follow-up groups and between the TAU and CT groups. Thus, the baseline MA group was a robust control group to measure any potential differences at follow-up, although we included the HC group for measures related to non-SUD status.
Table 1.
Demographic variables.
| Demographic variables | Groups |
Statistic (p-value) (d = Cohen's effect size) |
||||
|---|---|---|---|---|---|---|
| Healthy control (n = 21) | All baseline MA (n = 36) | Baseline TAU (n = 15) | Baseline CT (n = 21) | HC vs. all baseline MA | Baseline TAU vs. baseline CT | |
| Age (mean, s.d.) | 27.67 (8.714) | 28.42 (6.129) | 29.00 (6.291) | 28.00 (6.132) | 0.381 (0.705) | 0.477 (0.636) |
| Type of drug taken (%) | ||||||
| Methamphetamine | – | 36 (100) | 15 (100) | 21 (100) | – | – |
| Mandrax/dagga/marijuana/nicotine | 36 (100) | 15 (100) | 21 (100) | |||
| Duration drug taking (yrs) | – | 9.69 (3.8) | 10.73 (3.955) | 8.95 (3.556) | – | 1.414 (0.166) |
| Ethnicity, n (%) | ⁎⁎ | ⁎⁎ | ||||
| Black | 7 (33) | 1 (3) | 1 (6.5) | 0 (0) | 41.155 | 2.965 |
| Mixed-race | 2 (10) | 34 (94) | 13 (87) | 21 (100) | (< 0.001) | (0.227) |
| White | 12 (57) | 1 (3) | 1 (6.5) | 0 (0) | ||
| Education, n (%) | ⁎⁎ | ⁎⁎ | ||||
| No matric | 1 (5) | 23 (64) | 9 (60) | 14 (67) | 48.891 | 0.169 |
| Matric | 1 (5) | 13 (36) | 6 (40) | 7 (33) | (< 0.001) | (0.681) |
| Undergraduate | 12 (57) | 0 | 0 | 0 | ||
| Honours | 4 (19) | 0 | 0 | 0 | ||
| PhD | 3 (14) | 0 | 0 | 0 | ||
HC = healthy controls; MA = baseline methamphetamine dependent group; TAU = treatment as usual; CT = cognitive training; p-value = probability value; n = number.
Chi-squared test of frequency distribution.
3.2. Questionnaire measures
See Table 2 for between group (HC, MA, TAU, CT) differences.
Table 2.
Neuropsychological variables between groups.
| Neuropsychological variables | Groups mean (s.d) |
T statistic (p-value) (d = Cohen's effect size) |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Healthy control (n = 21) | All baseline MA (n = 36) | Baseline TAU (n = 15) | Baseline CT (n = 21) | Follow-up TAU (n = 13) | Follow-up CT (n = 15) | HC vs. all baseline MA | Baseline TAU vs. baseline CT | HC vs. follow-up TAU | HC vs. follow-up CT | Follow-up TAU vs. follow-up CT | |
| Mood (%) | 63.9 (14.1) | 57.1 (26.7) | 55.5 (29.1) | 58.2 (25.5) | 60.1 (24.4) | 75.3 (20.4) | 1.267 (0.357⁎) (0.3) | 0.285 (0.704⁎) (0.1) |
0.583 (0.933⁎) (0.21) | 1.864 (0.119⁎) (0.69) | 1.795 (0.142⁎) (0.71) |
| Desire for drug (%) | 3.8 (6.7) | 15.3 (19.5) | 13.9 (22.6) | 16.3 (17.6) | 13.6 (15.8) | 9.6 (18.2) | 3.210 (0.001⁎) (0.73) | 0.360 (0.374⁎) (0.12) | 2.109 (0.038⁎) (0.92) | 1.343 (0.491⁎) (0.47) | 0.610 (0.339⁎) (0.24) |
| Feelings of self-control (%) | 83.7 (14.2) | 71.6 (19.9) | 69.9 (19.5) | 72.9 (20.5) | 76.7 (19.6) | 89.0 (12.7) | 2.433 (0.018) (0.68) | 0.429 (0.547⁎) (0.15) | 1.197 (0.240) (0.44) | 1.149 (0.161⁎) (0.4) | 1.929 (0.098⁎) (0.79) |
| Trail making errors (B-A) | 0.5 (0.6) | 0.6 (0.9) | 0.6 (1.0) | 0.5 (0.8) | 0.2 (0.7) | 0.5 (0.9) | 0.333 (0.741) (0.13) | 0.242 (0.811) (0.12) | 1.153 (0.258) (0.48) | 0.149 (0.882) (0) | 0.975 (0.339) (0.38) |
| Trail Making RT (B-A) | 32.9 (14.9) | 58.2 (37.4) | 54.7 (41.3) | 61.1 (35.0) | 37.8 (31.4) | 57.4 (24.4) | 3.296 (0.002) (0.83) | 0.452 (0.655) (0.17) | 0.520 (0.610) (0.22) | 3.260 (0.004) (1.3) | 1.783 (0.087) (0.73) |
| BIS total | 54.5 (8.1) | 67.7 (12.1) | 68.0 (11.4) | 67.4 (12.8) | 68.0 (11.2) | 60.2 (11.2) | 4.625 (< 0.001) (1.24) | 0.122 (0.903) (0.05) | 3.881 (0.001) (1.48) | 1.690 (0.101) (0.62) | 1.764 (0.091) (0.72) |
| BIS attention | 8.9 (2.4) | 10.4 (2.5) | 10.4 (2.7) | 10.5 (2.5) | 10.0 (3.1) | 9.4 (2.6) | 2.247 (0.029) (0.62) | 0.024 (0.796⁎) (0.04) | 1.187 (0.244) (0.42) | 0.605 (0.550) (0.21) | 0.555 (0.584) (0.22) |
| BIS motor | 14.0 (2.9) | 17.2 (4.4) | 17.0 (4.7) | 17.4 (4.2) | 17.4 (4.0) | 15.6 (2.2) | 3.364 (0.001) (0.83) | 0.259 (0.797) (0.09) | 2.916 (0.006) (1.04) | 1.864 (0.071) (0.62) | 1.493 (0.147) (0.59) |
| BIS self-control | 10.5 (2.8) | 13.5 (3.1) | 14.6 (2.6) | 12.7 (3.3) | 12.4 (3.0) | 11.0 (3.6) | 3.669 (0.001) (1.02) | 1.839 (0.075) (0.64) | 1.903 (0.066) (0.68) | 0.490 (0.628) (0.16) | 1.096 (0.284) (0.44) |
| BIS cognitive complexity | 9.3 (2.4) | 11.9 (2.8) | 11.9 (2.8) | 12.0 (3.0) | 11.6 (3.5) | 11.3 (2.3) | 3.479 (0.001) (0.99) | 0.085 (0.933) (0.04) | 2.283 (0.029) (0.83) | 2.552 (0.016) (0.87) | 0.257 (0.799) (0.11) |
| BIS perseverance | 6.7 (1.6) | 8.6 (2.3) | 8.7 (2.4) | 8.5 (2.2) | 7.9 (2.2) | 8.3 (3.3) | 3.310 (0.002) (0.93) | 0.268 (0.790) (0.09) | 1.821 (0.080⁎) (0.67) | 1.771 (0.093) (0.67) | 0.380 (0.905⁎) (0.15) |
| BIS cognitive instability | 5.0 (1.3) | 6.4 (1.5) | 6.4 (1.6) | 6.5 (1.6) | 7.6 (2.1) | 5.1 (1.4) | 3.465 (0.001) (1) | 0.171 (0.849⁎) (0.06) | 3.948 (0.001) (1.63) | 0.145 (0.658⁎) (0.08) | 3.787 (0.002⁎) (1.48) |
| BIS 2nd order attentional | 13.9 (2.3) | 16.9 (3.4) | 16.8 (3.5) | 16.9 (3.5) | 17.6 (4.2) | 14.5 (3.1) | 3.432 (0.001) (1) | 0.105 (0.813⁎) (0.03) | 2.928 (0.009) (1.21) | 0.675 (0.505) (0.23) | 2.275 (0.031) (0.88) |
| BIS 2nd order motor | 20.7 (3.7) | 25.8 (5.9) | 25.7 (6.3) | 25.9 (5.8) | 25.5 (5.0) | 23.9 (4.9) | 4.008 (< 0.001) (1) | 0.089 (0.930) (0.03) | 3.189 (0.003) (1.17) | 2.290 (0.028) (0.78) | 0.815 (0.423) (0.34) |
| BIS 2nd Order Non-planning | 19.8 (4.4) | 25.4 (5.2) | 26.5 (4.6) | 24.7 (5.6) | 24.0 (5.9) | 22.4 (5.4) | 4.119 (< 0.001) (1.16) | 1.029 (0.311) (0.36) | 2.366 (0.024) (0.86) | 1.589 (0.122) (0.55) | 0.724 (0.476) (0.29) |
| HADS anxiety | 6.5 (2.8) | 7.8 (2.8) | 8.5 (2.0) | 7.4 (3.3) | 6.4 (2.6) | 6.2 (2.2) | 1.693 (0.096) (0.47) | 1.235 (0.125⁎) (0.4) | 0.108 (0.929⁎) (0.04) | 0.346 (0.835⁎) (0.12) | 0.212 (0.980⁎) (0.76) |
| HADS depression | 2.4 (2.3) | 5.8 (3.3) | 5.5 (2.5) | 6.0 (3.8) | 4.3 (3.0) | 3.3 (2.7) | 4.640 (< 0.001) (1.16) | 0.419 (0.678) (0.15) | 2.095 (0.044) (0.76) | 1.144 (0.261) (0.76) | 0.908 (0.372) (0.37) |
| SRQ total | 239.8 (13.7) | 219.9 (27.8) | 214.2 (21.9) | 225.7 (32.5) | 219.2 (19.4) | 241.4 (27.1) | 3.084 (0.004) (0.86) | 1.062 (0.299) (0.23) | 3.172 (0.004) (1.32) | 0.195 (0.848) (0.08) | 2.164 (0.043) (0.97) |
| SRQ receiving | 35.4 (4.3) | 30.0 (6.2) | 29.4 (5.6) | 30.5 (6.6) | 30.85 (4.5) | 35.5 (6.6) | 3.439 (0.001) (0.98) | 0.494 (0.625) (0.18) | 2.907 (0.007) (1.07) | 0.063 (0.704⁎) (0.02) | 2.121 (0.019⁎) (0.84) |
| SRQ evaluating | 30.2 (3.4) | 28.8 (7.9) | 30.8 (10.9) | 27.2 (3.9) | 26.2 (4.0) | 26.3 (2.9) | 0.781 (0.022⁎) (0.22) | 1.353 (0.185) (0.49) | 3.062 (0.011⁎) (1.13) | 3.533 (0.001) (1.25) | 0.078 (0.938) (0.03) |
| SRQ triggering | 32.9 (3.1) | 31.3 (4.2) | 30.9 (3.7) | 31.6 (4.6) | 31.7 (2.6) | 31.4 (3.8) | 1.416 (0.163) (0.42) | 0.474 (0.931⁎) (0.17) | 1.039 (0.308) (0.42) | 1.219 (0.232) (0.45) | 0.195 (0.847) (0.09) |
| SRQ searching | 35.5 (3.8) | 36.2 (4.9) | 35.6 (4.6) | 36.7 (5.2) | 35.0 (5.1) | 39.4 (3.9) | 0.611 (0.544) (0.16) | 0.651 (0.520) (0.23) | 0.283 (0.779) (0.12) | 2.959 (0.005⁎) (1.04) | 2.508 (0.027⁎) (1.02) |
| SRQ planning | 36.2 (2.3) | 28.6 (6.1) | 27.5 (5.2) | 29.4 (6.7) | 30.8 (5.0) | 33.7 (7.8) | 6.297 (< 0.001) (1.53) | 0.827 (0.383⁎) (0.32) | 3.662 (0.002) (1.56) | 1.198 (0.248) (0.48) | 1.153 (0.259) (0.45) |
| SRQ implementing | 36.0 (3.0) | 31.5 (5.9) | 30.5 (4.9) | 32.2 (6.7) | 33.8 (4.8) | 35.7 (7.7) | 3.705 (0.001) (0.91) | 0.817 (0.420) (0.29) | 1.639 (0.120⁎) (0.6) | 0.127 (0.950⁎) (0.06) | 0.821 (0.413⁎) (0.3) |
| SRQ assessing | 35.5 (2.8) | 31.1 (5.7) | 30.6 (5.4) | 31.5 (6.0) | 31.5 (4.3) | 33.9 (4.1) | 3.901 (< 0.001) (0.92) | 0.452 (0.654) (0.16) | 3.325 (0.002) (1.2) | 1.403 (0.160⁎) (0.48) | 1.481 (0.155⁎) (0.59) |
| Accuracy (%) | 48.3 (15.7) | 67.1 (10.4) | |||||||||
HC = healthy controls; MA = baseline methamphetamine dependent group; TAU = treatment as usual; CT = cognitive training; p-value = probability value; n = number; BIS = Barratt impulsivity scale; HADS = hospital anxiety and depression scale; SRQ = self-regulation questionnaire.
Mann-Whitney non-parametric post-hoc t-tests were computed due to non-normally distributed data.
3.2.1. HC vs baseline MA group
Significant differences were found between the HC and Baseline MA group for the following measures: the MA group had a higher percentage desire for drug score (t = 3.210, p = 0.001, d = 0.73) a higher trail making response time (t = 3.296, p = 0.002, d = 0.83) and a higher HADS depression score (t = 4.640, p ≤ 0.001, d = 1.16). The MA group also scored higher on the BIS, including the total score (t = 4.625, p ≤ 0.001, d = 1.24), BIS motor (t = 3.364, p = 0.001, d = 1.02), BIS self-control (t = 3.669, p = 0.001, d = 1.02), BIS cognitive complexity (t = 3.479, p = 0.001, d = 0.99), BIS perseverance (t = 3.310, p = 0.002, d = 0.93), BIS cognitive instability (t = 3.465, p = 0.001, d = 1.00), BIS second order attentional (t = 3.432, p = 0.001, t = 1.00), BIS second order motor (t = 4.008, p ≤ 0.001, d = 1.00) and BIS second order non-planning (t = 4.119, p ≤ 0.001, d = 1.16). They also had lower self-regulation than the HC group on several subscales of the SRQ, specifically receiving (t = 3.439, p = 0.001, d = 0.98), planning (t = 6.297, p ≤ 0.001, d = 1.53), implementing (t = 3.705, p = 0.001, d = 0.91) and assessing (t = 3.901, p ≤ 0.001, d = 0.92).
3.2.2. TAU vs. CT at baseline
There were no significant differences in any questionnaire measure between the MA baseline group which became the TAU and CT groups at follow-up.
3.2.3. HC vs. TAU follow-up
The TAU group had significantly higher scores compared to the HC group on the total BIS (t = 3.881, p = 0.001, d = 1.48), BIS cognitive instability (t = 3.948, p = 0.001, d = 1.63) and BIS second order motor (t = 3.189, p = 0.003, d = 1.17). The TAU group also scored lower than the HC group on several subscales of the SRQ, including total SRQ (t = 3.172, p = 0.004, d = 1.32), SRQ receiving (t = 2.907, p = 0.007, d = 1.07), SRQ planning (t = 3.662, p = 0.002, d = 1.56) and SRQ assessing (t = 3.325, p = 0.002, d = 1.2).
3.2.4. HC vs. CT follow-up
The CT group had significantly longer trail making response times compared to the HC group (t = 3.260, p = 0.004, d = 1.3). They also scored significantly lower on several subscales of the SRQ, including SRQ evaluating (t = 3.533, p = 0.001, d = 1.25) and SRQ searching (t = 2.959, p = 0.005, d = 1.04). There were no significant differences on any other measures.
3.2.5. Baseline vs. follow-up repeated measures within-group analyses (TAU and CT)
See Table 3 for difference between baseline and follow-up measures.
Table 3.
Baseline vs. follow-up repeated measures within MA group (TAU and CT).
| Demographic and psychological variables | T statistic (p values) (d = Cohen's effect size) |
|
|---|---|---|
| Baseline TAU vs. Follow-up TAU (n = 13) |
Baseline CT vs. follow-up CT (n = 15) |
|
| Cognitive training accuracy (%) |
4.833 (< 0.001) (d = 1.46) |
|
| Mood (%) | 0.852 (0.311⁎) (d = 0.18) |
2.205 (0.047⁎) (d = 0.77) |
| Desire for drug (%) | 0.078 (0.939) (d = 0.02) |
1.622 (0.155⁎) (d = 0.39) |
| Feelings of self-control | 1.025 (0.456⁎) (d = 0.36) |
3.607 (0.003⁎) (d = 0.98) |
| Trail making errors (B-A) | 1.915 (0.082) (d = 0.48) |
0.318 (0.758) (d = 0) |
| Trail making RT (B-A) | 2.403 (0.033) (d = 0.48) |
0.257 (0.803) (d = 0.13) |
| BIS total | 0.781 (0.458) (d = 0) |
2.872 (0.013) (d = 0.62) |
| BIS attention |
0.356 (0.002⁎) (d = 0.14) |
1.927 (0.099⁎) (d = 0.45) |
| BIS motor | 0.000 (1.000) (d = 0.1) |
1.822 (d = 0.092) (d = 0.56) |
| BIS self-control | 2.332 (0.038) (d = 0.82) |
2.071 (0.059) (d = 0.51) |
| BIS cognitive complexity | 0.090 (0.930) (d = 0.1) |
0.633 (0.538) (d = 0.27) |
| BIS perseverance | 1.340 (0.179⁎) (d = 0.36) |
0.438 (0.669) (d = 0.07) |
| BIS cognitive instability | 2.028 (0.067) (d = 0.67) |
2.259 (0.046⁎) (d = 0.96) |
| BIS 2nd order attentional | 0.285 (0.781) (d = 0.34) |
2.439 (0.045⁎) (d = 0.75) |
| BIS 2nd order motor | 0.493 (0.632) (d = 0.04) |
1.558 (0.143) (d = 0.39) |
| BIS 2nd order non-planning | 1.700 (0.115) (d = 0.49) |
1.750 (0.104) (d = 0.43) |
| HADS anxiety | 1.758 (0.105⁎) (d = 0.94) |
1.046 (0.344⁎) (d = 0.44) |
| HADS depression | 1.385 (0.194) (d = 0.45) |
2.559 (0.023) (d = 0.85) |
| SRQ total | 0.121 (0.907) (d = 0.25) |
1.794 (0.116) (d = 0.54) |
| SRQ receiving | 1.044 (0.317) (d = 0.3) |
2.066 (0.068⁎) (d = 0.78) |
| SRQ evaluating | 1.705 (0.114) (d = 0.58) |
0.351 (0.732) (d = 0.27) |
| SRQ triggering | 0.559 (0.475) (d = 0.26) |
0.311 (0.761) (d = 0.05) |
| SRQ searching | 1.424 (0.185) (d = 0.13) |
2.302 (0.059⁎) (d = 0.61) |
| SRQ planning | 2.709 (0.022) (d = 0.67) |
2.096 (0.078⁎) (d = 0.61) |
| SRQ implementing | 2.598 (0.023⁎) (d = 0.71) |
1.981 (0.061⁎) (d = 0.5) |
| SRQ assessing | 0.386 (0.707) (d = 0.19) |
1.609 (0.194⁎) (d = 0.48) |
HC = healthy controls; MA = baseline methamphetamine dependent group; TAU = treatment as usual; CT = cognitive training; p-value = probability value; n = number; BIS = Barratt impulsivity scale; HADS = hospital anxiety and depression scale; SRQ = self-regulation questionnaire;
Wilcoxon Signed Ranks non parametric post-hoc t-tests were computed due to non-normally distributed data.
There were no significant differences between baseline and follow-up in the TAU group at the Bonferroni level. In the CT group, however, there were improvements in working memory accuracy (t = 4.833, p ≤ 0.001, d = 1.41), self-reported feelings of self-control (t = 3.607, p = 0.003, d = 0.98) and HADS depression (t = 2.559, p = 0.023, d = 0.85). There were no significant improvements on any other measures.
3.3. VBM analyses
See Table 4a, Table 4b for details of all VBM analyses, which were FWE corrected (besides two findings which were significant at the FDR and uncorrected level respectively, but which we deemed were important to mention).
Table 4a.
3 × 2 ANCOVA group (MA, TAU and CT) × working memory accuracy (high, low), with age and duration drug taking as covariates of no interest.
| Brain region | MNI coordinates |
|||||
|---|---|---|---|---|---|---|
| x | y | z | Cluster size (Voxels) | Z statistic | p-Value (FWE clust) | |
| Interaction | ||||||
| Right putamen (extending to the amygdala/hippocampus) | 27 | − 16 | 10 | 457 | 5.73 | 0.001 |
| Left putamen (extending to the amygdala/hippocampus) | − 18 | 11 | − 9 | 880 | 5.21 | 0.004 |
| Right cerebellum | 30 | − 85 | − 35 | 6111 | 5.04 | 0.009 |
| Left cerebellum | − 29 | − 54 | − 44 | 3560 | 4.96 | 0.013 |
| Main effect of group | ||||||
| Right putamen (extending to the amygdala/hippocampus) | 27 | − 16 | 10 | 487 | 5.61 | 0.001 |
| Left putamen (extending to the amygdala/hippocampus) | − 18 | 11 | − 9 | 1415 | 5.46 | 0.001 |
| Left cerebellum | − 29 | − 54 | − 44 | 3912 | 5.02 | 0.010 |
| Right cerebellum | 30 | − 85 | − 35 | 6023 | 4.96 | 0.012 |
| Main effect of working memory accuracy | ||||||
| Right orbitofrontal cortex (Brodmann area 11) | 30 | 56 | − 21 | 54 | 3.63 | 0.001 |
| MA ≥ TAU | ||||||
| Mid orbitofrontal cortex (Brodmann area 11) | − 2 | 66 | − 11 | 1221 | 4.07 | 0.02 |
| Right cerebellum | 21 | − 87 | − 30 | 1592 | 3.99 | 0.007 |
| MA ≥ CT | ||||||
| Right cerebellum | 30 | − 85 | − 35 | 7516 | 5.06 | < 0.001 |
| Left cerebellum | − 36 | − 82 | − 30 | 6056 | 4.81 | < 0.001 |
| Left orbitofrontal cortex (Brodmann area 11) | − 29 | 63 | 3 | 3701 | 4.27 | < 0.001 |
| TAU ≥ MA | ||||||
| Right putamen | 27 | − 16 | 10 | 510 | 5.73 | < 0.001 |
| Left putamen | − 18 | 9 | − 9 | 713 | 4.58 | 0.05 |
| CT ≥ MA | ||||||
| Left putamen (extending to the amygdala/hippocampus) | − 18 | 11 | − 9 | 1867 | 5.26 | 0.003 |
| Right Thalamus (extending to the amygdala/hippocampus) | 21 | − 18 | 10 | 376 | 4.76 | 0.02 |
| Left Thalamus (extending to the amygdala/hippocampus) | − 15 | − 15 | 7 | 1278 | 4.12 | 0.02 |
| Right putamen (extending to the amygdala/hippocampus) | 21 | 6 | − 9 | 1227 | 4.62 | 0.02 |
| Left cerebellum | − 21 | − 97 | − 24 | 929 | 4.32 | 0.05 |
| Right cerebellum | 8 | − 102 | − 6 | 1053 | 4.12 | 0.03 |
| CT ≥ TAU | ||||||
| Left midfrontal gyrus (Brodmann area 6) | − 24 | 9 | 43 | 206 | 4.29 | < 0.001 |
| High working memory accuracy ≥ low working memory accuracy | ||||||
| Right orbitofrontal cortex (Brodmann area 11) | 30 | 56 | − 21 | 90 | 3.81 | < 0.001 |
| High accuracy MA ≥ TAU | ||||||
| Left cerebellum | − 50 | − 63 | − 47 | 1150 | 3.97 | 0.03 |
| Right cerebellum | 42 | − 75 | − 42 | 3288 | 3.90 | < 0.001 |
| High accuracy MA ≥ CT | ||||||
| Right cerebellum | 30 | − 81 | − 38 | 1998 | 3.92 | 0.002 |
| High accuracy TAU ≥ MA | ||||||
| Right putamen (extending to the amygdala/hippocampus) | 27 | − 16 | 10 | 1845 | 6.26 | 0.003 |
| Left putamen (extending to the amygdala/hippocampus) | − 20 | 11 | − 6 | 1565 | 4.47 | 0.007 |
| CT high ≥ low accuracy | ||||||
| Right orbitofrontal cortex (Brodmann area 11) | 29 | 57 | − 18 | 438 | 4.24 | 0.023 |
MNI = Montreal Neurological Institute; FWE = family wise error; TAU = treatment as usual; CT = cognitive training; MA = methamphetamine baseline;
Table 4b.
2 × 2 ANCOVA group (TAU v CT) and time point (baseline, follow-up).
| Brain region | MNI coordinates |
|||||
|---|---|---|---|---|---|---|
| x | y | z | Cluster size (Voxels) | Z statistic | p-Value (FWE clust) |
|
| Interaction | ||||||
| Right putamen (extending to the amygdala) | 24 | − 16 | 12 | 1319 | 7.22 | < 0.001 |
| Left cerebellum | − 29 | − 54 | − 44 | 25,009 | 5.75 | < 0.001 |
| Left putamen (extending to the amygdala) | − 18 | 9 | − 9 | 3129 | 5.70 | < 0.001 |
| Right middle frontal gyrus (Brodmann area 6) | 30 | 2 | 57 | 585 | 4.93 | 0.05 |
| Main effect of group | ||||||
| Right middle frontal gyrus (Brodmann area 6) | 30 | 0 | 57 | 923 | 5.20 | 0.01 |
| Main effect of time point | ||||||
| Right putamen (extending to the amygdala) | 24 | − 16 | 12 | 1738 | 7.41 | < 0.001 |
| Left cerebellum | − 29 | − 54 | − 44 | 30,060 | 6.07 | < 0.001 |
| Left putamen (extending to the amygdala) | − 18 | 9 | − 9 | 4706 | 6.02 | < 0.001 |
| Right putamen (extending to the amygdala) | 20 | 3 | − 9 | 1683 | 5.17 | 0.014 |
| TAU ≥ CT (regardless of timepoint) | ||||||
| Right middle frontal gyrus (Brodmann area 6) | 30 | 0 | 57 | 1135 | 5.32 | 0.021 |
| Left superior frontal gyrus/SMA (Brodmann area 6) | − 17 | − 12 | 63 | 1079 | 4.38 | 0.026 |
| CT ≥ TAU (regardless of timepoint) | ||||||
| Left occipital lobe (Brodmann area 18) | − 6 | − 88 | 7 | 1252 | 4.12 | 0.013 |
| Baseline ≥ follow-up (regardless of group) | ||||||
| Left cerebellum | − 29 | − 54 | − 44 | 35,738 | 7.23 | < 0.001 |
| Left middle frontal gyrus (Brodmann area 6) | − 6 | 44 | − 9 | 1343 | 4.02 | 0.009 |
| Right middle frontal gyrus (Brodmann area 6) | 8 | 69 | − 11 | 2644 | 4.02 | < 0.001 |
| Follow-up ≥ baseline (regardless of group) | ||||||
| Right putamen (extending to the amygdala) | 24 | − 16 | 12 | 9715 | 7.50 | < 0.001 |
| Right cerebellum | 6 | − 102 | − 6 | 3243 | 4.81 | < 0.001 |
| Left cerebellum | − 23 | − 100 | − 21 | 1117 | 4.31 | 0.023 |
| TAU: baseline ≥ follow-up | ||||||
| Left cerebellum | − 50 | − 61 | − 45 | 7875 | 5.56 | < 0.001 |
| Right cerebellum | 32 | − 84 | − 35 | 8478 | 4.44 | < 0.001 |
| TAU: follow-up ≥ baseline | ||||||
| Right putamen | 26 | − 15 | 13 | 966 | 6.26 | 0.04 |
| CT: baseline ≥ follow-up | ||||||
| Right cerebellum | 32 | − 85 | − 36 | 6756 | 4.87 | < 0.001 |
| Left cerebellum | − 51 | − 64 | − 35 | 4747 | 4.57 | < 0.001 |
| CT: follow-up ≥ baseline | ||||||
| Right putamen (extending to the amygdala/hippocampus) | 22 | − 18 | 12 | 1023 | 5.69 | 0.003 |
| Left putamen (extending to the amygdala/hippocampus) | − 16 | 6 | − 9 | 3033 | 4.90 | < 0.001 |
| Right caudate (extending to the amygdala/hippocampus) | 20 | 2 | − 9 | 1132 | 4.36 | 0.021 |
| Baseline: TAU ≥ CT | ||||||
| No significant volume difference | ||||||
| Baseline: CT ≥ TAU | ||||||
| No significant volume difference | ||||||
| Follow-up: TAU ≥ CT | ||||||
| No significant volume difference | ||||||
| Follow-up: CT ≥ TAU | ||||||
| No significant volume difference | ||||||
MNI = Montreal Neurological Institute; FWE = family wise error; TAU = treatment as usual; CT = cognitive training; SMA = supplementary motor area.
The 2 × 2 ANCOVA examining group (HC and baseline MA) and WM accuracy revealed no significant differences in brain volume.
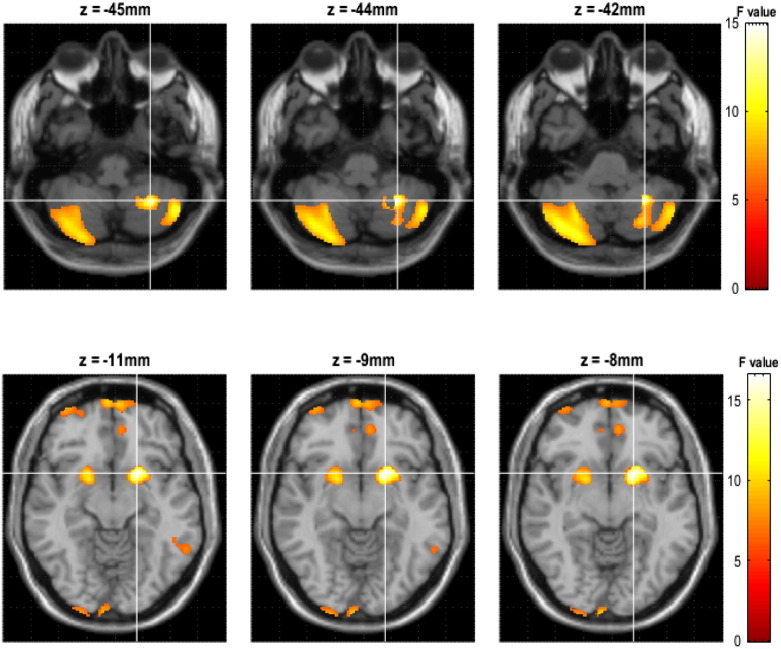
A 3 × 2 ANCOVA examined interactions and any main effect of patient group (MA, TAU, CT) and of WM accuracy (high, low), correcting for age and duration of drug taking, Family Wise Error (FWE) corrected. See Fig. 1. An interaction in the bilateral putamen extending to the hippocampus (x = 27/− 15, y = − 16/9, z = 10/− 11; cluster size = 801/1705 voxels; Z statistic = 5.62/5.50; p = 0.001/0.002) and right cerebellum (x = 29, y = − 85/, z = − 33, cluster size = 4172 voxels, Z statistic = 4.64, p < 0.001) was observed. A main effect of group was observed in the bilateral putamen extending to the hippocampus (x = − 15/27, y = 9/− 16, z = − 11/10, cluster size = 2375/845 voxels, Z statistic = 5.75/5.42, p < 0.001/0.002) and the right caudate (x = 20, y = 5, z = − 11, cluster size = 1301 voxels, Z statistic = 4.69, p = 0.049), left thalamus (x = − 17, y-15, z = 10, cluster size = 529 voxels, Z statistic = 4.60, p = 0.05), bilateral cerebellum (x = 29/− 36, y = − 85/− 82, z = − 33/− 30, cluster size = 3314/789 voxels, Z statistic = 4.35/3.84, p < 0.001/0.01) and left occipital lobe (x = − 23, y = − 97, z = − 17, cluster size = 935 voxels, Z statistic = 4.11, p = 0.004). A main effect of WM accuracy was observed (although it was a preliminary finding as it was only significant without FWE correction) in the right dorsolateral prefrontal cortex (DLPFC) (x = 30, y = 56, z = − 20, cluster size = 155 voxels, Z statistic = 4.10, p = 0.001).
Fig. 1.
Interaction in the bilateral striatum and cerebellum.
Z = axial plane, colour-bar represents the F-statistic. Top row illustrates bilateral cerebellar differences. Bottom row illustrates bilateral putamen differences.
Post-hoc t-tests (all FWE corrected) revealed that the TAU follow-up group in comparison to baseline MA group had larger volumes in the bilateral putamen extending to the amygdala/hippocampus (x = 27/− 15, y = − 16/9, z = 10/− 11, cluster size = 851/1085 voxels, Z statistic = 5.56/4.72, p = 0.025/0.009), and the left thalamus (x = − 17, y = − 15, z = 10, cluster size = 648 voxels, Z statistic = 4.45, p = 0.036), but no smaller volumes. The CT follow-up group in comparison to the MA baseline group had larger volumes in the bilateral putamen extending to the hippocampus/amygdala (x = 20/− 15, y = 5/9, z = − 11/− 11, cluster size = 2134/3619 voxels, Z statistic = 5.66/4.82, p < 0.001/<0.001), right thalamus (x = 21, y = − 18, z = 12, cluster size = 746 voxels, Z statistic = 4.68, p = 0.041) and left cerebellum (x = − 23, y = − 96, z = − 24, cluster size = 3841 voxels, Z statistic = 4.40, p < 0.001), but also smaller volumes in discretely different areas of the bilateral cerebellum (x = 30/− 36, y = − 85/− 82, z = − 35/− 30, cluster size = 5135/2649 voxels, Z statistic = 4.57/4.34, p < 0.001/<0.001).
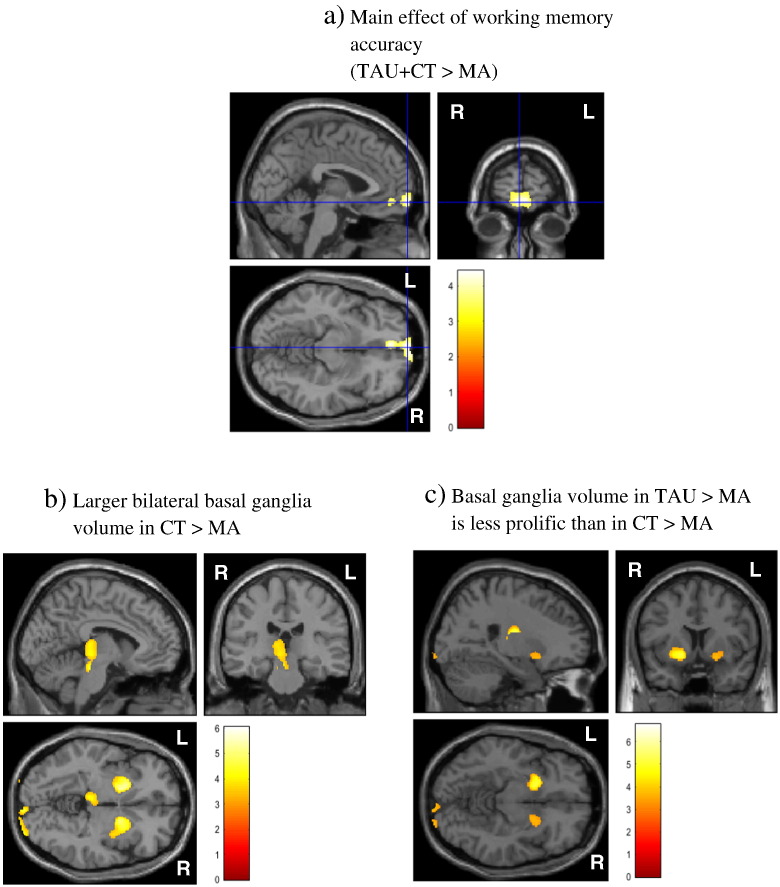
3.4. WM accuracy (see Fig. 2)
Fig. 2.
High working memory accuracy in the right middle frontal cortex. a) Higher working memory accuracy during the experimental procedure in both the TAU and CT groups compared to baseline MA revealed larger middle frontal cortex volume; b) Larger bilateral basal ganglia volume associated with higher working memory accuracy in the CT > MA group; c) larger bilateral basal ganglia volume is also observed in the TAU > MA group but the effects are less significant than in the previous CT > MA contrast.
Post-hoc t-tests revealed a preliminary finding (significant only when not FWE corrected) for larger brain volume in the right DLPFC in the high versus low WM accuracy condition regardless of group status (x = 30, y = 56, z = − 20, cluster size = 221 voxels, Z statistic = 4.25, p < 0.001). Further post-hoc t-tests revealed that high WM accuracy during the scan, after 4 weeks of TAU compared to baseline MA was associated with smaller bilateral cerebellar volume (x = 51/− 50, y = − 47/− 63, z = − 44/− 47, cluster size = 2789/855 voxels, Z statistic = 4.01/3.90, p < 0.001/0.025) and larger bilateral putamen volume extending to the amygdala/hippocampus (x = − 35/27, y = − 7/− 16, z = − 3/10, cluster size = 2527/2757 voxels, Z statistic = 6.32/4.51, p < 0.001). High WM accuracy in those patients who additionally completed WM training was associated with significantly reduced right cerebellum volume (x = 30, y = − 81, z = − 38, cluster size = 776 voxels, Z statistic = 3.87, p = 0.035) and larger left putamen (extending to the amygdala/hippocampus) (x = − 14, y = 6, z = − 14, cluster size = 1727 voxels, Z statistic = 4.61, p = 0.001). Finally, in the CT group only, there is preliminary evidence (significant without FWE correction) that high WM accuracy is associated with larger volume in the right DLPFC (x = 29, y = 57, z = − 18, cluster size = 438 voxels, Z statistic = 4.24, p = 0.023).
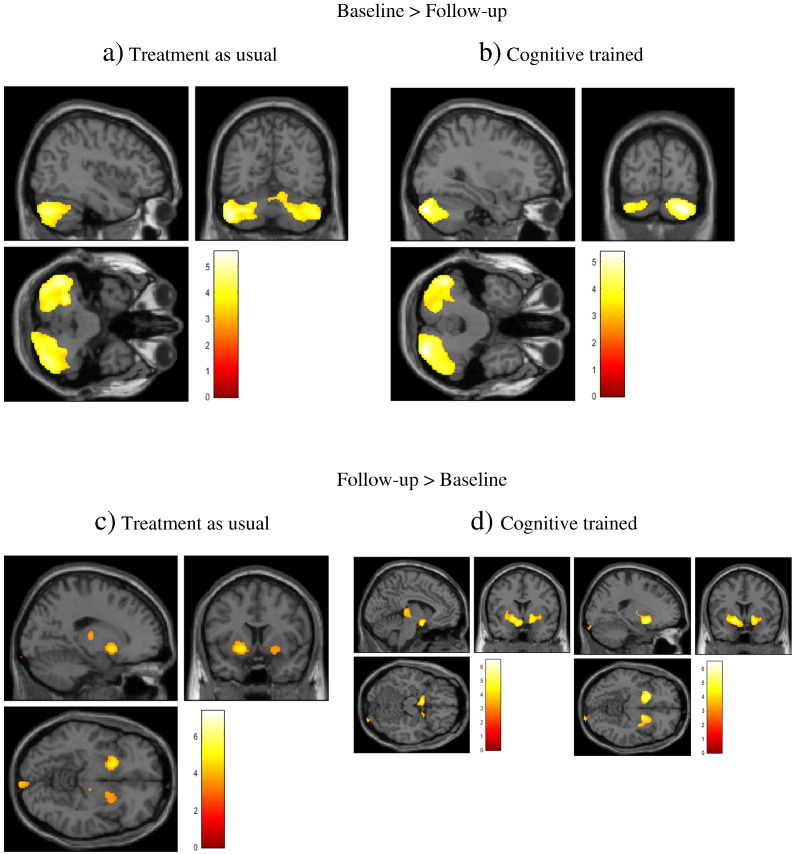
A 2 × 2 repeated measures ANCOVA examined interactions and any main effect of patient group (TAU, CT) and of time point (baseline, follow-up) Family Wise Error (FWE) corrected. See Fig. 3 and Table 4b. Significant interactions were found in the bilateral putamen (extending to the amygdala) (x = 24/− 18, y = − 16/9, z = 12/− 9, cluster size = 1319/3129 voxels, Z statistic = 7.22/5.70, p < 0.001), the left cerebellum (x = − 29, y = − 54, z = − 44, cluster size = 25,009 voxels, Z statistic = 5.75, p < 0.001) and the right middle frontal gyrus, Brodmann area 6 (x = 30, y = 2, z = 57, cluster size = 585 voxels, Z statistic = 4.93, p = 0.05). A main effect of patient group was observed, in the right middle frontal gyrus (x = 30, y = 0, z = 57, cluster size 923 voxels, Z statistic = 5.20, p = 0.01) and a main effect of time point was observed in the bilateral putamen (x = 24/20/− 18, y = − 16/3/9, z = 12/− 9/− 9, cluster size = 1738/1683/4706 voxels, Z statistic = 7.41/5.17/6.02, p < 0.001/0.014) and the left cerebellum (x = − 29, y = − 54, z = − 44, cluster size = 30,060 voxels, Z statistic = 6.07, p < 0.001). Subsequent post-hoc t-tests revealed that TAU (regardless of time point) had larger volume than CT in right middle frontal gyrus, Brodmann area 6 (x = 30, y = 0, z = 57, cluster size = 1135 voxels, Z statistic = 5.32, p = 0.021) and left superior frontal gyrus/supplementary motor area (x = − 17, y = − 12, z = 63, cluster size = 1079 voxels, Z statistic = 4.38, p = 0.026). By contrast the CT group (regardless of time point) had larger volume than the TAU group in the left occipital lobe (x = − 6, y = − 88, z = 7, cluster size = 1252 voxels, Z statistic = 4.12, p = 0.013). There was greater volume at baseline compared to follow-up regardless of group, in the left cerebellum (x = − 29, y = − 54, z = − 44, cluster size = 35,738 voxels, Z statistic = 7.23, p < 0.001) and the bilateral middle frontal gyrus (x = − 6/8, y = 44/69, z = − 9/− 11, cluster size = 1343/2644 voxels, Z statistic = 4.02, p = 0.009/<0.001). Conversely, in the follow-up time point regardless of group, larger volume compared to baseline was observed in the right putamen extending to the amygdala (x = 24, y = − 16, z = 12, cluster size = 9715 voxels, Z statistic = 7.50, p < 0.001) and the bilateral cerebellum (x = − 23/6, y = − 102/− 100, z = − 6/− 21, cluster size = 3243/1117 voxels, Z statistic = 4.81/4.31, p < 0.001/0.023).
Fig. 3.
Repeated measures effects. a) In TAU, baseline > follow-up there was larger bilateral cerebellar volume; b) in the CT baseline > follow-up there was also larger bilateral cerebellar volume; c) in the TAU group at follow-up > baseline there was larger bilateral putamen volume; d) however, in the CT group at follow-up > baseline there were more significant larger volumes in the bilateral basal ganglia, extending to amygdala/hippocampus.
In terms of repeated measures group differences, in the TAU group, we observed larger bilateral cerebellar volumes at baseline compared to follow-up (x = − 50/32, y = − 61/− 84, z = − 45/− 35, cluster size = 7875/8478 voxels, Z statistic = 5.56/4.44, p < 0.001), whereas at the follow-up timepoint compared to baseline the TAU group had larger right putamen volume (x = 26, y = − 15, z = 13, cluster size = 966 voxels, Z statistic = 6.26, p = 0.04).
In the CT group at baseline compared to follow-up, we again observed larger bilateral cerebellar volumes (x = 32/− 51, y = − 85/− 64, z = − 36/− 35, cluster size = 6756/4747 voxels, Z statistic = 4.87/4.57, p < 0.001). However, in the follow-up versus baseline time point there were more protracted larger volumes in the CT group than were observed in the TAU group, in bilateral putamen (extending to the amygdala/hippocampus) (x = 22/− 16, y = − 18/6, z = 12/− 9, cluster size = 1023/3033 voxels, Z statistic = 5.69/4.90, p = 0.003/<0.001) and the right caudate (extending to the amygdala/hippocampus) (x = 20, y = 2, z = − 9, cluster size = 1132 voxels, Z statistic = 4.36, p = 0.021). No other volumetric differences were observed.
4. Discussion
This voxel-based morphometry (VBM) study is the first to examine whether 4 weeks of standard psychological intervention with additional adjunctive working memory (WM) training can alter brain volume in male in-patients being treated for methamphetamine (MA) use. Additionally, we sought to link volumetric brain changes to improvements in subjective self-report measures of impulse control, self-regulation and WM accuracy. It must be noted that changes in self-report measures while intriguing may not transfer to actual changes in clinical measures. Nevertheless, after 4 weeks of psychological TAU, MA using males exhibited larger volume in the bilateral putamen (extending to the hippocampus) and reduced left middle temporal gyrus, right post-central gyrus and left insula cortex volume. Further, those who had additional cognitive training (CT) demonstrated more pronounced increases in volume that extended across large areas of the bilateral basal ganglia, as well as reduced bilateral cerebellar volume. While no significant correlations between questionnaire measures of impulsivity, self-regulation and changes in brain volume were observed, greater improvements/normalization in impulsivity and self-regulation scores were found in the CT compared to the TAU group. This may suggest that the brain volumetric differences observed may be attributable to clinical improvements rather than self-reports in the CT group, although there are likely also other variables at play, such as molecular mechanisms and genetic susceptibility associated with impulsivity. Finally, we presented some preliminary evidence that greater WM accuracy at follow-up in the CT group was associated with larger volume in the right middle frontal cortex and orbitofrontal cortex, regions associated with executive functioning, WM ability and impulse control (Brooks, 2015). We suggest that with no medications known to improve MA use disorder reliably and no psychological interventions yet able to effectively reduce relapse rates, it is important to explore the neurobiological effects of adjunctive behavioural interventions such as WM training, and so our study provides a useful progression to the field.
A recent meta-analysis of WM training in both HC and patients with schizophrenia demonstrates that greater activation incorporating frontoparietal networks, the DLPFC and anterior cingulate, as well as the striatum, are associated with neuroplasticity changes (Li et al., 2015). Additionally, previous studies have shown that cerebellar (Ding et al., 2012), striatum, lateral prefrontal and frontoparietal grey matter volume alterations are associated with WM capacity (Ruge and Wolfensteller, 2015), and that larger volume in the lateral prefrontal cortex is particularly susceptible to variations in WM capacity (Reid et al., 2015). Furthermore, training using a WM task has been associated with reductions in frontoparietal network volume (Takeuchi et al., 2011), although there is some indication that basal ganglia networks are more susceptible to WM training (Klingberg, 2014). Thus, in line with previous research, we find increases in volume following WM training that are most significant in the basal ganglia, and we show this for the first time in male patients being treated for MA use.
The effects of CT on brain volume may have been confounded by the neurotoxic effects of MA exposure, suggesting that longitudinal studies using CT may be more beneficial to clinical advances. Neurotoxic effects of MA exposure have been shown by animal models to be associated with reductions in dopamine, serotonin and associated dopamine transporter (DAT) systems, as well as greater expression of brain derived neurotrophic factor (BDNF) in frontal, parietal, and basal ganglia areas (Braun et al., 2011). DAT is reduced in rats exposed to MA for 10 days, particularly in the striatum, orbitofrontal cortex, dorsolateral prefrontal cortex and amygdala, persisting after abstinence (Hong et al., 2015). Furthermore, animal models have demonstrated that MA exposure impairs spatial learning and memory, (Bigdeli et al., 2015), but that proactive interference (the tendency to repeat previous responses) to WM can be ameliorated with a dopamine D1 receptor antagonist (Macaskill et al., 2015). Additionally, impaired memory in mice that have been exposed to MA is associated with dysfunction in dopamine D1 receptor-extracellular signal-regulated kinase 1/2 (ERK1/2) pathway in the prefrontal cortex, striatum and hippocampus (Nagai and Yamada, 2010). Thus, animal models of MA exposure and concomitant WM deficits consistently report the involvement of disrupted dopamine activity in the frontostriatal neural circuitry, which is associated with WM. It might therefore be useful to study the effects of WM training on neurochemistry in animal models.
Animal studies of WM training support the hypothesis that frontostriatal circuitry changes coincide with learning and memory. For example, volume change in the medial striatum in mice is implicated in spatial WM training (Pooters et al., 2015), and studies have shown epigenetic effects in the dorsal and medial striatum in mice after WM training (Cassanelli et al., 2015). Additionally, methylation sequences in prefrontal cortex neurons of mice are shown to be susceptible to WM training effects (Jakovcevski et al., 2015). Furthermore, cerebellar volume (which was shown to be reduced following WM training in our human cohort) is associated with plasticity-related volume increases during motor WM learning in mice (Yamazaki et al., 2015). Similarly, activation of dopaminergic circuits (associated with the basal ganglia in humans) are shown to mediate short and long term memory formation associated with reward reinforcement in Drosophila melanogaster (Yamagata et al., 2015). Moreover, the role of greater DLPFC activation in delaying the application of recently learned visual information and of concurrently regulating tactile stimuli is demonstrated in a recent study of monkeys completing a uni- and cross-modal visual and haptic perception task (Wang et al., 2015). Thus, animal models help to understand the observations of volumetric brain differences in patients with MA dependence undergoing CT in our study.
Studies of CT using WM tasks in humans have highlighted that efficiency within neural system operations can be achieved by potentially fostering inherent plasticity processes (Keshavan et al., 2014, Subramaniam et al., 2014), particularly in the frontostriatal circuitry (Haut et al., 2010). This coincides with improved cognitive functioning in people with ADHD; (Klingberg, 2010, Spencer-Smith and Klingberg, 2015), schizophrenia (Li et al., 2015) and some evidence in those with substance use disorder (Brooks et al., n.d, Bickel et al., 2015, Wesley and Bickel, 2014). For example, computerized WM training has been shown to reduce impulsivity and delay discounting (lowering the preference for immediate over delayed rewards) among stimulant users (Bickel et al., 2011). Additionally, WM tasks have been shown in a meta-analysis to activate DLPFC with reduced activation coinciding with reduced temporal discounting, a measure of impulsivity, in those with stimulant use disorder (Wesley and Bickel, 2014). However, until now there has been no brain imaging studies to show that WM training alters brain volume associated with underlying functional mechanisms, in the frontostriatal circuitry in MA dependent individuals.
It is intriguing to consider findings that abstinence from MA acutely increases striatal volume, and may be a reflection of compensatory cognitions that maintain optimal functioning, greater glial activation or inflammation associated with MA-related injury (London et al., 2014, Ballard et al., 2015, Yuan et al., 2015, Nixon et al., 2008, Jernigan et al., 2005, Chang et al., 2005, Jan et al., 2012). Although longer term psychological intervention may differentially alter brain volume. It is not yet clear how interventions for MA use alter brain volume, for example, whether there is larger or smaller volume in the frontostriatal circuitry over a period of time to reflect alterations in neurotoxicity, DA transporter levels and receptor regulation or reorganisation of regional brain networks for example. It might be intuitive to expect a reduction in striatal brain volume following TAU or an adjunctive intervention, given that MA users generally exhibit larger striatal grey-matter volume than non-users (Berman et al., 2008). However, greater striatal activation associated with neuroplasticity changes have been shown after CT (Brooks et al., n.d.), which would support our observations here.
Nevertheless, the question remains, what else could underlie our observed increase in basal ganglia volume following WM training in male in-patients being treated for MA use? It might be that repetitive and increasingly difficult training over 4 weeks encourages inherent neural plasticity after the initial involvement of neuronal support systems (e.g. microglia) (Nixon et al., 2008), which forge more efficient communication along the frontostriatal circuitry. This in turn might lead the patient, during DBT treatment, to have better adherence to cognitive strategies while regulating affective (interoceptive) and environmental (exteroceptive) distractors. For example, blunting of negative affect and drug taking prior to treatment may coincide with a maladaptive coping approach that helps a person to limit the recollection of traumatic life experiences. However, the harnessing of daily and increasingly loaded WM training that fosters inherent neural plasticity (Keshavan et al., 2014, Subramaniam et al., 2014) associated with larger brain volumes may reflect enhanced basal ganglia connections and better affect regulation. In this vein, recent evidence in humans supports the view that greater brain volume after a course of WM training may be associated with myelination and related microstructural markers that underpin plasticity and improvements in clinical populations (Caeyenberghs et al., 2016). However, it is not yet clear that if WM training fosters such neuroplasticity benefits, whether the effects are longer term, and so more longitudinal studies are needed.
Some limitations deserve consideration during the interpretation of our findings. Firstly, we did not observe greater striatal volume in the MA cohort at baseline, as is extensively reported in humans (London et al., 2014, Jan et al., 2012, Churchwell et al., 2012, Chang et al., 2007). However, our failure to replicate these well-reported findings could be due to our MA cohort being abstinent for at least two weeks at the start of the study and recovering from malnourishment, which can alter regional brain volume (Titova et al., 2013), due to re-feeding for two weeks. Therefore, neuronal re-wiring due to treatment and re-feeding effects may have already occurred and prevented our replication of greater striatal volume in MA compared to HC at baseline. Furthermore, we did not take measures of cytokines in blood that may differentiate larger brain volume due to neurotoxicity from larger volume due to neuroplasticity. Secondly, we did not contrast the CT group with a control MA group that also spent time on a computer and had regular contact with researchers but that did not receive the WM training intervention. This is pertinent as it could be that regular social interaction with researchers could have led to the volumetric changes we observed. Additionally, the sample was confounded by our inability to gauge an accurate duration of drug use and length of abstinence prior to treatment, although all in-patients were drug free for two weeks from the beginning of the study. Also, we only recruited males since the in-patient facility at the time of our study housed only males, preventing generalization to females. Finally, there was a significant difference in ethnicity and level of education between the HC and MA group, although we accounted for this by conducting analyses with the baseline MA group as the control condition for treatment effect, and also by conducting repeated measures analyses.
In summary, having previously observed that adjunctive WM training improves outcomes compared to TAU in MA using males (Brooks et al., n.d.), here we extend our work by investigating the potential involvement of specific brain regions in improved clinical outcomes, and discuss some possible molecular mechanisms associated with the dopaminergic reward circuitry. First, using voxel-based morphometry we demonstrate that daily adjunctive WM training is associated with greater increases in frontostriatal circuitry than is seen in TAU. Second, we report that in the CT group the neural alterations observed are associated with improvements in self-reported affect regulation and reduced impulsivity. While further work is needed to investigate the neurobiological mechanisms and molecular underpinnings responsible for these increases in volume, as well as potential longitudinal transfer, these data are important in buttressing our view that CT may be useful in those being treated for MA use. We further posit that our data provide a clear model of the relevant neurocircuitry that underlies the impact of CT.
Conflicts of interest
The Curb Your Addiction (C-Ya) App is currently being marketed online at $4.99, but free downloads are available to researchers who are interested to use the software, upon request (www.drsamanthabrooks.com).
Acknowledgements
We thank the clinical staff at Maitland Treatment Center for their help and support during our study. The study was financially supported by the Brain Behaviour Initiative (BBI), University of Cape Town, the Claude Leon Foundation, South Africa, the Medical Research Council (MRC) of South Africa and the National Institute of Health NIDA R21 DA040492.
Footnotes
Supplementary data to this article can be found online at http://dx.doi.org/10.1016/j.nicl.2016.08.019.
Contributor Information
S.J. Brooks, Email: drsamanthabrooks@gmail.com.
K.H. Burch, Email: mbykhbu@nottingham.ac.uk.
S.A. Maiorana, Email: stefanomaiorana@me.com.
E. Cocolas, Email: ecocolas@gmail.com.
H.B. Schioth, Email: helgi.schioth@neuro.uu.se.
E.K. Nilsson, Email: emil.nilsson@neuro.uu.se.
K. Kamaloodien, Email: kkamaloodien@uwc.ac.za.
D.J. Stein, Email: dan.stein@uct.ac.za.
Appendix A. Supplementary data
CONSORT Diagram.
References
- Ashburner J. A fast diffeomorphic image registration algorithm. NeuroImage. 2007;38(1):95–113. doi: 10.1016/j.neuroimage.2007.07.007. [DOI] [PubMed] [Google Scholar]
- Baicy K., London E.D. Corticolimbic dysregulation and chronic methamphetamine abuse. Addiction. 2007;102(Suppl 1):5–15. doi: 10.1111/j.1360-0443.2006.01777.x. [DOI] [PubMed] [Google Scholar]
- Ballard M.E., Mandelkern M.A., Monterosso J.R., Hsu E., Robertson C.L., Ishibashi K., Dean A.C., ED L. Low dopamine D2/D3 receptor availability is associated with steep discounting of delayed rewards in methamphetamine dependence. Int. J. Neuropsychopharmacol. 2015;18(7) doi: 10.1093/ijnp/pyu119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berman S., O'Neill J., Fears S., Bartzokis G., London E.D. Abuse of amphetamines and structural abnormalities in the brain. Ann. N. Y. Acad. Sci. 2008;1141:195–220. doi: 10.1196/annals.1441.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bickel W.K., Yi R., Landes R.D., Hill P.F., Baxter C. Remember the future: working 1140 memory training decreases delay discounting among stimulant addicts. Biol. Psychiatry. 2011;69(3):260–265. doi: 10.1016/j.biopsych.2010.08.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bickel W.K., Quisenberry A.J., Moody L., Wilson A.G. Therapeutic opportunities for self-control repair in addiction and related disorders: change and the limits of change in trans-disease processes. Clin. Psychol. Sci. 2015;3(1):140–153. doi: 10.1177/2167702614541260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bigdeli I., Asia M.N., Miladi-Gorji H., Fadaei A. The spatial learning and memory performance in methamphetamine-sensitized and withdrawn rats. Iran J. Basic Med. Sci. 2015 Mar;18(3):234–239. [PMC free article] [PubMed] [Google Scholar]
- Braun A.A., Herring N.R., Schaefer T.L., Hemmerle A.M., Dickerson J.W., Seroogy K.B., Vorhees C.V., Williams M.T. Neurotoxic (+)-methamphetamine treatment in rats increases brain-derived neurotrophic factor and tropomyosin receptor kinase B expression in multiple brain regions. Neuroscience. 2011;184:164–171. doi: 10.1016/j.neuroscience.2011.03.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brooks S.J. A debate on working memory and cognitive control: can we learn about the treatment of substance use disorders from the neural correlates of anorexia nervosa? BMC Psychiatry. 2015 doi: 10.1186/s12888-016-0714-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brooks S.J., Stein D.J. A systematic review of the neural bases of psychotherapy for anxiety and related disorders. Dialogues Clin. Neurosci. 2015;17(3):261–279. doi: 10.31887/DCNS.2015.17.3/sbrooks. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brooks SJ, Burch KH, Simon M, Nilsson EK, Schioth HB, Cocolas E, Kamaloodien K, Stein DJ. Working memory training as an adjunct to treatment as usual is associated with better impulse-control in self-selected methamphetamine dependent males (under review).
- Brown J.M., Miller W.R., Lawendowski L.A. The self-regulation questionnaire. In: VandeCreek L., Jackson T.L., editors. Innovations in Clinical Practice: A Source Book. Vol. 17. Professional Resource Press; Sarasota, FL: 1999. pp. 281–289. [Google Scholar]
- Caeyenberghs K., Metzler-Baddeley C., Foley S., Jones D.K. Dynamics of the human structural connectome underlying working memory training. J. Neurosci. 2016;36(14):4056–4066. doi: 10.1523/JNEUROSCI.1973-15.2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carey K.B., Neal D.J., Collins S.E. A psychometric analysis of the self-regulation questionnaire. Addict. Behav. 2004;29(2):253–260. doi: 10.1016/j.addbeh.2003.08.001. [DOI] [PubMed] [Google Scholar]
- Cassanelli P.M., Cladouchos M.L., Fernández Macedo G., Sifonios L., Giaccardi L.I., Gutiérrez M.L., Gravielle M.C., Wikinski S. Working memory training triggers delayed chromatin remodeling in the mouse corticostriatothalamic circuit. Prog. Neuro-Psychopharmacol. Biol. Psychiatry. 2015;60:93–103. doi: 10.1016/j.pnpbp.2015.02.011. [DOI] [PubMed] [Google Scholar]
- Chang L., Cloak C., Patterson K., Grob C., Miller E.N., Ernst T. Enlarged striatum in abstinent methamphetamine abusers: a possible compensatory response. Biol. Psychiatry. 2005;57(9):967–974. doi: 10.1016/j.biopsych.2005.01.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chang L., Alicata D., Ernst T., Volkow N. Structural and metabolic brain changes in the striatum associated with methamphetamine abuse. Addiction. 2007;102(Suppl 1):16–32. doi: 10.1111/j.1360-0443.2006.01782.x. [DOI] [PubMed] [Google Scholar]
- Chen Y.C., Chen C.K., Wang L.J. Predictors of relapse and dropout during a 12-week relapse prevention program for methamphetamine users. J. Psychoactive Drugs. 2015;47(4):317–324. doi: 10.1080/02791072.2015.1071447. [DOI] [PubMed] [Google Scholar]
- Chudasama Y., Robbins T.W. Functions of frontostriatal systems in cognition: comparative neuropsychopharmacological studies in rats, monkeys and humans. Biol. Psychol. 2006;73(1):19–38. doi: 10.1016/j.biopsycho.2006.01.005. [DOI] [PubMed] [Google Scholar]
- Churchwell J.C., Carey P.D., Ferrett H.L., Stein D.J., Yurgelun-Todd D.A. Abnormal striatal circuitry and intensified novelty seeking among adolescents who abuse methamphetamine and cannabis. Dev. Neurosci. 2012;34(4):310–317. doi: 10.1159/000337724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dahlbom M., Mukherjee J., Bilder R.M., Brody A.L., Mandelkern M.A. Striatal dopamine d2/d3 receptor availability is reduced in methamphetamine dependence and is link to impulsivity. J. Neurosci. 2009;29(47):14734–14740. doi: 10.1523/JNEUROSCI.3765-09.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dean A.C., Kohno M., Morales A.M., Ghahremani D.G., London E.D. Denial in methamphetamine users: associations with cognition and functional connectivity in brain. Drug Alcohol Depend. 2015 Jun 1;151:84–91. doi: 10.1016/j.drugalcdep.2015.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ding H., Qin W., Jiang T., Zhang Y., Yu C. Volumetric variation in subregions of the cerebellum correlates with working memory performance. Neurosci. Lett. 2012;508(1):47–51. doi: 10.1016/j.neulet.2011.12.016. [DOI] [PubMed] [Google Scholar]
- Ersche K.D., Jones P.S., Williams G.B., Turton A.J., Robbins T.W., Bullmore E.T. Abnormal brain structure implicated in stimulant drug addiction. Science. 2012;335(6068):601–604. doi: 10.1126/science.1214463. [DOI] [PubMed] [Google Scholar]
- First M.B., Spitzer R.L., Miriam G., Williams J.B.W. (SCID-I/NP) New York: Biometrics Research. New York State Psychiatric Institute; 2002. Structured clinical interview for DSM-IV-TR Axis I disorders, research version, non-patient edition. [Google Scholar]
- Groman S.M., Morales A.M., Lee B., London E.D., Jentsch J.D. Methamphetamine-induced increases in putamen gray matter associate with inhibitory control. Psychopharmacology. 2013;229(3):527–538. doi: 10.1007/s00213-013-3159-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harro J. Neuropsychiatric adverse effects of amphetamine and methamphetamine. Int. Rev. Neurobiol. 2015;120:179–204. doi: 10.1016/bs.irn.2015.02.004. [DOI] [PubMed] [Google Scholar]
- Haut K.M., Lim K.O., MacDonald A., 3rd. Prefrontal cortical changes following cognitive training in patients with chronic schizophrenia: effects of practice, generalization, and specificity. Neuropsychopharmacology. 2010;35(9):1850–1859. doi: 10.1038/npp.2010.52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hides L., Dawe S., McKetin R., Kavanagh D.J., Young R.M., Teesson M., Saunders J.B. Primary and substance-induced psychotic disorders in methamphetamine users. Psychiatry Res. 2015;226(1):91–96. doi: 10.1016/j.psychres.2014.11.077. [DOI] [PubMed] [Google Scholar]
- Hong S.J., Zhang D., Zhang L.H., Yang P., Wan J., Yu Y., Wang T.H., Feng Z.T., Li L.H., Yew D.T. Expression of dopamine transporter in the different cerebral regions of methamphetamine-dependent rats. Hum. Exp. Toxicol. 2015;34(7):707–717. doi: 10.1177/0960327114555929. [DOI] [PubMed] [Google Scholar]
- Jakovcevski M., Ruan H., Shen E.Y., Dincer A., Javidfar B., Ma Q., Peter C.J., Cheung I., Mitchell A.C., Jiang Y., Lin C.L., Pothula V., Stewart A.F., Ernst P., Yao W.D., Akbarian S. Neuronal Kmt2a/Mll1 histone methyltransferase is essential for prefrontal synaptic plasticity and working memory. J. Neurosci. 2015;35(13):5097–5108. doi: 10.1523/JNEUROSCI.3004-14.2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jan R.K., Lin J.C., Miles S.W., Kydd R.R., Russell B.R. Striatal volume increases in active methamphetamine-dependent individuals and correlation with cognitive performance. Brain Sci. 2012;2(4):553–572. doi: 10.3390/brainsci2040553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jernigan T.L., Gamst A.C., Archibald S.L., Fennema-Notestine C., Mindt M.R., Marcotte T.D., Heaton R.K., Ellis R.J., Grant I. Effects of methamphetamine dependence and HIV infection on cerebral morphology. Am. J. Psychiatry. 2005;162(8):1461–1472. doi: 10.1176/appi.ajp.162.8.1461. [DOI] [PubMed] [Google Scholar]
- Karbach J., Unger K. Executive control training from middle childhood to adolescence. Front. Psychol. 2014;5:390. doi: 10.3389/fpsyg.2014.00390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keshavan M.S., Vinogradov S., Rumsey J., Sherrill J., Wagner A. Cognitive training in mental disorders: update and future directions. Am. J. Psychiatry. 2014;171(5):510–522. doi: 10.1176/appi.ajp.2013.13081075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirchner W.K. Age differences in short-term retention of rapidly changing information. J. Exp. Psychol. 1958;55(4):352–358. doi: 10.1037/h0043688. [DOI] [PubMed] [Google Scholar]
- Klingberg T. Training and plasticity of working memory. Trends Cogn. Sci. 2010;1113(14):317–324. doi: 10.1016/j.tics.2010.05.002. [DOI] [PubMed] [Google Scholar]
- Klingberg T. Childhood cognitive development as a skill. Trends Cogn. Sci. 2014;18(11):573–579. doi: 10.1016/j.tics.2014.06.007. [DOI] [PubMed] [Google Scholar]
- Kohno M., Ghahremani D.G., Morales A.M., Robertson C.L., Ishibashi K., Morgan A.T., Mandelkern M.A., London E.D. Risk-taking behavior: dopamine D2/D3 receptors, feedback, and frontolimbic activity. Cereb. Cortex. 2015 Jan;25(1):236–245. doi: 10.1093/cercor/bht218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kwiatkowski M.A., Roos A., Stein D.J., Thomas K.G., Donald K. Effects of prenatal methamphetamine exposure: a review of cognitive and neuroimaging studies. Metab. Brain Dis. 2014;29(2):245–254. doi: 10.1007/s11011-013-9470-7. [DOI] [PubMed] [Google Scholar]
- Li X., Xiao Y.H., Zhao Q., Leung A.W., Cheung E.F., Chan R.C. The neuroplastic effect of working memory training in healthy volunteers and patients with schizophrenia: implications for cognitive rehabilitation. Neuropsychologia. 2015;75:149–162. doi: 10.1016/j.neuropsychologia.2015.05.029. [DOI] [PubMed] [Google Scholar]
- London E.D., Kohno M., Morales A.M., Ballard M.E. Chronic methamphetamine abuse and corticostriatal deficits revealed by neuroimaging. Brain Res. 2014;S0006-8993(14):01466–01468. doi: 10.1016/j.brainres.2014.10.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lyoo I.K., Yoon S., Kim T.S., Lim S.M., Choi Y., Kim J.E., Hwang J., Jeong H.S., HB C., YA C., PF R. Predisposition to and effects of methamphetamine use on the adolescent brain. Mol. Psychiatry. 2015 doi: 10.1038/mp.2014.191. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Macaskill A.C., Harrow C.C., Harper D.N. The disruptive effects of methamphetamine on delayed-matching-to-sample performance reflect proactive interference and are reduced by SCH23390. Pharmacol. Biochem. Behav. 2015;128:62–67. doi: 10.1016/j.pbb.2014.11.009. [DOI] [PubMed] [Google Scholar]
- Mahoney J.J., 3rd, Thompson-Lake D.G., Cooper K., Verrico C.D., Newton T.F., De La Garza R., 2nd A comparison of impulsivity, depressive symptoms, lifetime stress and sensation seeking in healthy controls versus participants with cocaine or methamphetamine use disorders. J. Psychopharmacol. 2015;29(1):50–56. doi: 10.1177/0269881114560182. [DOI] [PubMed] [Google Scholar]
- Miller K.M., Price C.C., Okun M.S., Montijo H., Bowers D. Is the N-back task a valid neuropsychological measure for assessing working memory. Arch. Clin. Neuropsychol. 2009;24(7):711–717. doi: 10.1093/arclin/acp063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morales A.M., Lee B., Hellemann G., O'Neill J., London E.D. Gray-matter volume in methamphetamine dependence: cigarette smoking and changes with abstinence from methamphetamine. Drug Alcohol Depend. 2012;125(3):230–238. doi: 10.1016/j.drugalcdep.2012.02.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morales A.M., Kohno M., Robertson C.L., Dean A.C., Mandelkern M.A., London E.D. Gray-matter volume, midbrain dopamine D2/D3 receptors and drug craving in methamphetamine users. Mol. Psychiatry. 2015;20(6):764–771. doi: 10.1038/mp.2015.47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nagai T., Yamada K. Molecular mechanism for methamphetamine-induced memory impairment. Nihon Arukoru Yakubutsu Igakkai Zasshi. 2010;45(2):81–91. [PubMed] [Google Scholar]
- Nixon K., Kim D.H., Potts E.N., He J., Crews F.T. Distinct cell proliferation events during abstinence after alcohol dependence: microglia proliferation precedes neurogenesis. Neurobiol. Dis. 2008;31(2):218–229. doi: 10.1016/j.nbd.2008.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olesen P.J., Westerberg H., Klingberg T. Increased prefrontal and parietal activity after training of working memory. Nat. Neurosci. 2003 doi: 10.1038/nn1165. [DOI] [PubMed] [Google Scholar]
- Owen A.M., McMillan K.M., Laird A.R., Bullmore E. N-back working memory paradigm: a meta-analysis of normative functional neuroimaging studies. Hum. Brain Mapp. 2005;25(1):46–59. doi: 10.1002/hbm.20131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Panenka W.J., Procyshyn R.M., Lecomte T., MacEwan G.W., Flynn S.W., Honer W.G., Barr A.M. Methamphetamine use: a comprehensive review of molecular, preclinical and clinical findings. Drug Alcohol Depend. 2013;129(3):167–179. doi: 10.1016/j.drugalcdep.2012.11.016. [DOI] [PubMed] [Google Scholar]
- Pascoe L., Roberts G., Doyle L.W., Lee K.J., Thompson D.K., Seal M.L., Josev E.K., Nosarti C., Gathercole S., Anderson P.J. Preventing academic difficulties in preterm children: a randomised controlled trial of an adaptive working memory training intervention — IMPRINT study. BMC Pediatr. 2013;13:144. doi: 10.1186/1471-2431-13-144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patton J.H., Stanford M.S., Barratt E.S. Factor structure of the Barratt impulsiveness scale. J. Clin. Psychol. 1995;51(6):768–774. doi: 10.1002/1097-4679(199511)51:6<768::aid-jclp2270510607>3.0.co;2-1. [DOI] [PubMed] [Google Scholar]
- Plüddemann A., C.D.H P. Policy Brief. South African Medical Research Council; Cape Town: 2012. Methamphetamine use and associated problems among adolescents in the Western Cape Province: A need for focused interventions. [Google Scholar]
- Pooters T., Gantois I., Vermaercke B., D'Hooge R. Inability to acquire spatial information and deploy spatial search strategies in mice with lesions in dorsomedial striatum. Behav. Brain Res. 2015;S0166-4328(15):30272. doi: 10.1016/j.bbr.2015.11.001. [DOI] [PubMed] [Google Scholar]
- Reid A.T., Bzdok D., Langner R., Fox P.T., Laird A.R., Amunts K., SB E., CR E. Multimodal connectivity mapping of the human left anterior and posterior lateral prefrontal cortex. Brain Struct. Funct. 2015 doi: 10.1007/s00429-015-1060-5. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reips U.D., Funke F. Interval-level measurement with visual analogue scales in internet-based research: VAS generator. Behav. Res. Methods. 2008;40(3):699–704. doi: 10.3758/brm.40.3.699. [DOI] [PubMed] [Google Scholar]
- Ruge H., Wolfensteller U. Distinct contributions of lateral orbito-frontal cortex, striatum, and fronto-parietal network regions for rule encoding and control of memory-based implementation during instructed reversal learning. NeuroImage. 2015;125:1–12. doi: 10.1016/j.neuroimage.2015.10.005. [DOI] [PubMed] [Google Scholar]
- Semple S.J., Strathdee S.A., Zians J., McQuaid J., Patterson T.L. Correlates of obsessive-compulsive disorder in a sample of HIV-positive, methamphetamine-using men who have sex with men. AIDS Behav. 2011 Aug;15(6):1153–1160. doi: 10.1007/s10461-010-9719-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shearin E.N., Linehan M.M. Dialectical behaviour therapy for borderline personality disorder: theoretical and empirical foundations. Acta Psychiatr. Scand. Suppl. 1994;379:61–68. doi: 10.1111/j.1600-0447.1994.tb05820.x. [DOI] [PubMed] [Google Scholar]
- Shinaver C.S., 3rd, Entwistle P.C., Söderqvist S. Cogmed WM training: reviewing the reviews. Appl. Neuropsychol. Child. 2014;3(3):163–172. doi: 10.1080/21622965.2013.875314. [DOI] [PubMed] [Google Scholar]
- Spencer-Smith M., Klingberg T. Benefits of a working memory training program for inattention in daily life: a systematic review and meta-analysis. PLoS One. 2015;10(3) doi: 10.1371/journal.pone.0119522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Subramaniam K., Luks T.L., Garrett C., Chung C., Fisher M., Nagarajan S., Vinogradov S. Intensive cognitive training in schizophrenia enhances working memory and associated prefrontal cortical efficiency in a manner that drives long-term functional gains. NeuroImage. 2014;1(99):281–292. doi: 10.1016/j.neuroimage.2014.05.057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Takeuchi H., Taki Y., Sassa Y., Hashizume H., Sekiguchi A., Fukushima A., Kawashima R. Working memory training using mental calculation impacts regional gray matter of the frontal and parietal regions. PLoS One. 2011;6(8) doi: 10.1371/journal.pone.0023175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thompson A.B., Stolyarova A., Ying Z., Zhuang Y., Gómez-Pinilla F., Izquierdo A. Methamphetamine blocks exercise effects on Bdnf and Drd2 gene expression in frontal cortex and striatum. Neuropharmacology. 2015 Aug. 31;99:658–664. doi: 10.1016/j.neuropharm.2015.08.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Titova O.E., Hjorth O.C., Schiöth H.B., Brooks S.J. Anorexia nervosa is linked to reduced brain structure in reward and somatosensory regions: a meta-analysis of VBM studies. BMC Psychiatry. 2013;13:110. doi: 10.1186/1471-244X-13-110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tombaugh T.N. Trail making test A and B: normative data stratified by age and education. Arch. Clin. Neuropsychol. 2004;19(2):203–214. doi: 10.1016/S0887-6177(03)00039-8. [DOI] [PubMed] [Google Scholar]
- Wang L., X L., SS H., FA L., Bodner M., YD Z., JM F. Differential roles of delay-period neural activity in the monkey dorsolateral prefrontal cortex in visual-haptic crossmodal working memory. Proc. Natl. Acad. Sci. U. S. A. 2015;112(2):E214–E219. doi: 10.1073/pnas.1410130112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wesley M.J., Bickel W.K. Remember the future II: meta-analyses and functional overlap of working memory and delay discounting. Biol. Psychiatry. 2014;75(6):435–448. doi: 10.1016/j.biopsych.2013.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yamagata N., Ichinose T., Aso Y., Plaçais P.Y., Friedrich A.B., Sima R.J., Preat T., Rubin G.M., Tanimoto H. Distinct dopamine neurons mediate reward signals for short- and long-term memories. Proc. Natl. Acad. Sci. U. S. A. 2015;112(2):578–583. doi: 10.1073/pnas.1421930112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yamazaki T., Nagao S., Lennon W., Tanaka S. Modeling memory consolidation during posttraining periods in cerebellovestibular learning. Proc. Natl. Acad. Sci. U. S. A. 2015;112(11):3541–3546. doi: 10.1073/pnas.1413798112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yuan J., Liu X.D., Han M., Lv R.B., YK W., GM Z., Y L. Comparison of striatal dopamine transporter levels in chronic heroin-dependent and methamphetamine-dependent subjects. Addict. Biol. 2015 doi: 10.1111/adb.12271. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- Zigmond A.S., Snaith R.P. The hospital anxiety and depression scale. Acta Psychiatr. Scand. 1983;67(6):361–370. doi: 10.1111/j.1600-0447.1983.tb09716.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
CONSORT Diagram.