Abstract
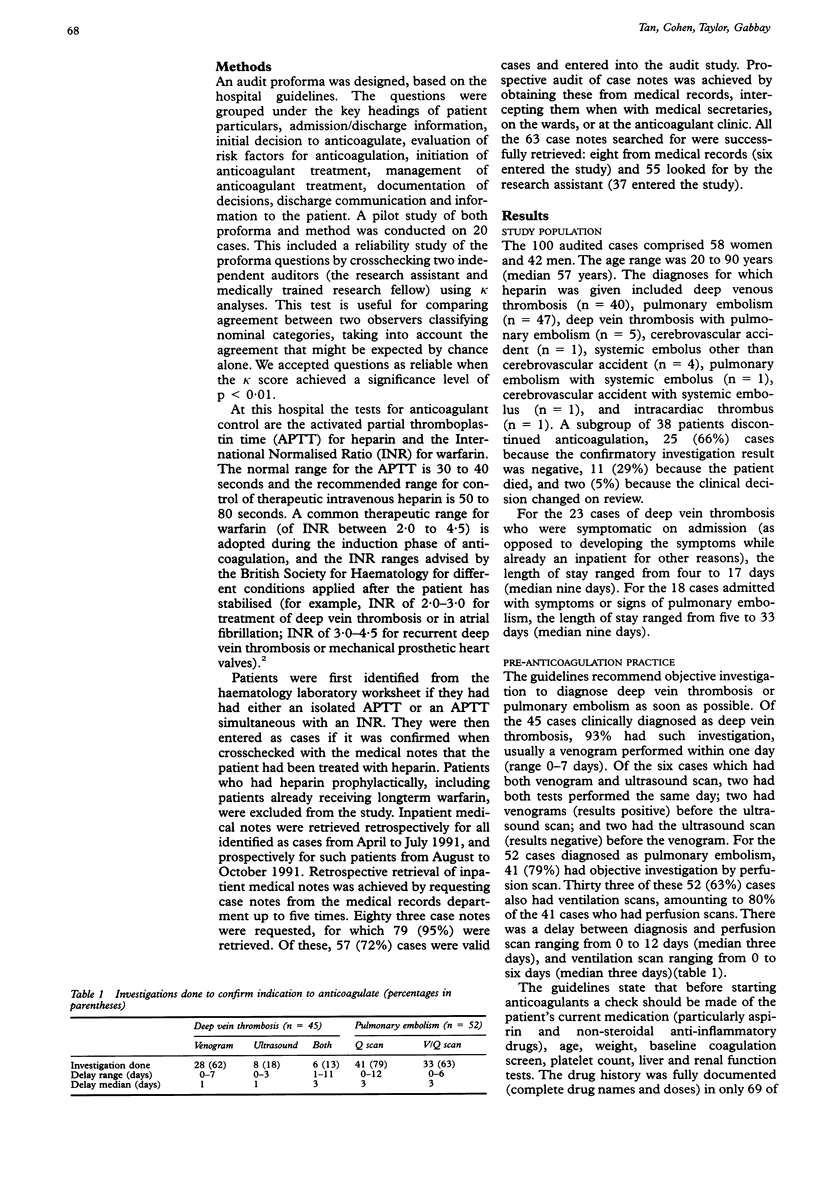
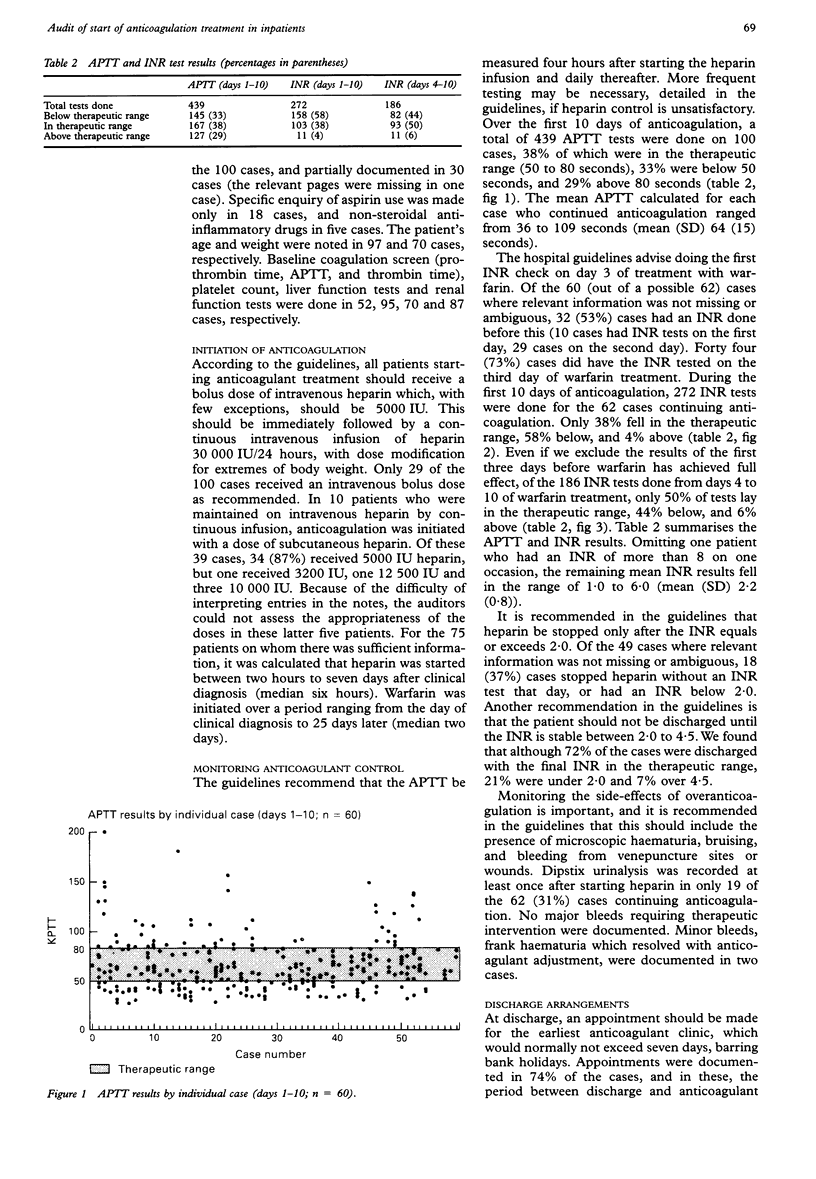
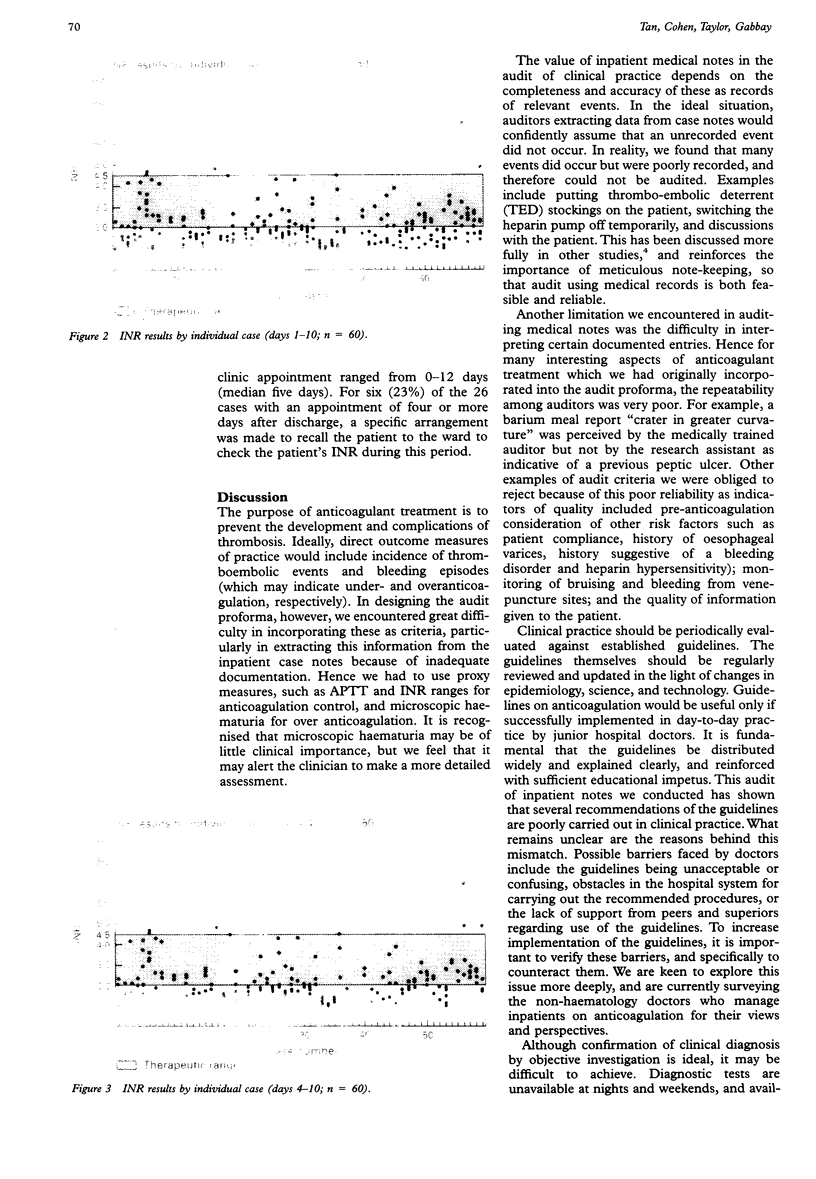
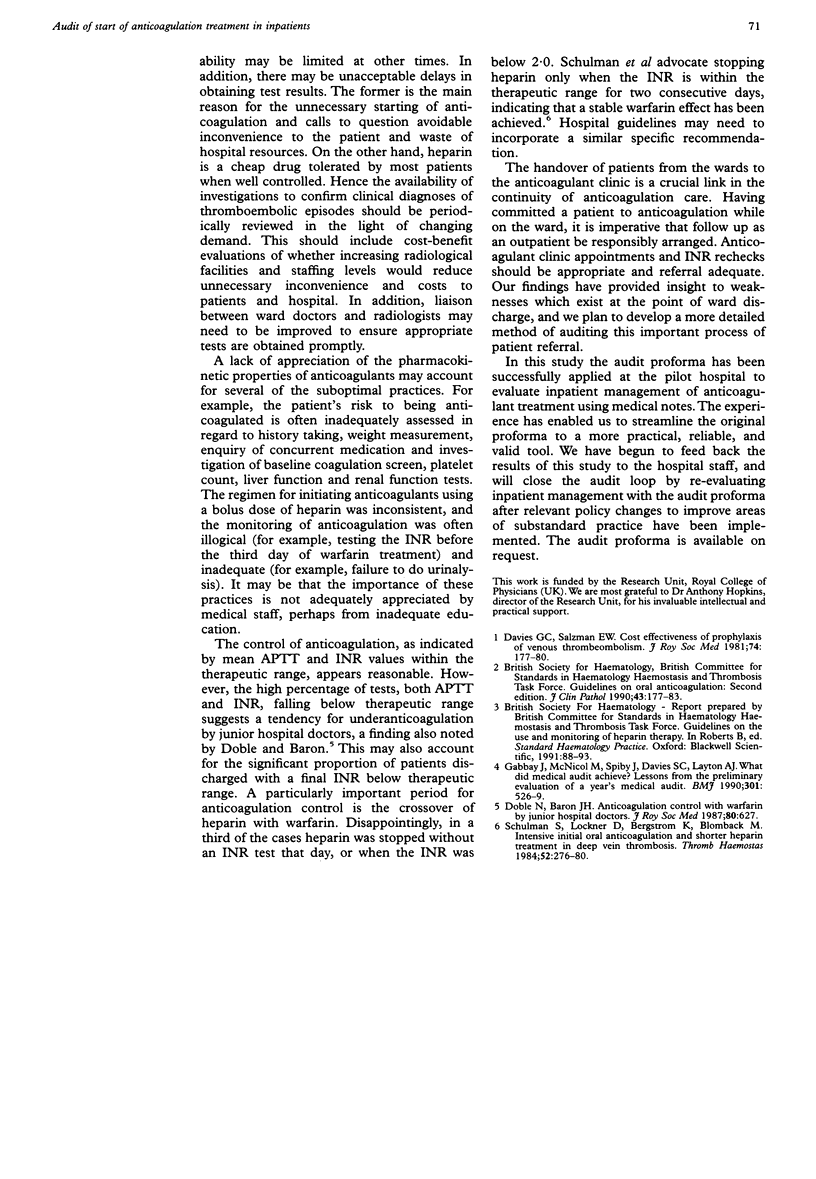
AIMS: To develop a method for evaluating the start of anticoagulation treatment in inpatients. METHODS: One hundred case notes were audited using a proforma based on local guidelines in accordance with British Society for Haematology recommendations. RESULTS: Confirmatory investigations were done in 93% and 79% of patients with symptomatic deep venous thrombosis and pulmonary embolism, respectively. Identification of patients' risk factors for anticoagulation by history taking and laboratory tests was often inadequate: baseline coagulation screen, platelet count, liver function and renal function tests were done in 52%, 95%, 70% and 87% of cases, respectively. There was a tendency to undertreat patients: 33% of the activated partial thromboplastin times (APTT) and 58% of the International Normalised Ratios (INR) were subtherapeutic. The heparin-warfarin crossover period was particularly problematic: 37% stopped heparin without an INR that day, or had an INR of less than 2. Microscopic haematuria was monitored occasionally. Of the 62 patients continuing anticoagulation, 72% were discharged with the final INR in the therapeutic range. At discharge, only 74% of patients had documented appointments for the anticoagulant Clinic, the period between discharge and appointment ranging from 0 to 12 days. Of the 25 cases with an appointment exceeding four days after discharge, only six (24%) had arrangements for an interim INR check. CONCLUSIONS: The experience allowed the proforma to become streamlined to a more practical, reliable, and valid tool for use elsewhere. Findings will be fed back to the hospital staff to promote practice improvements before closing the audit loop by re-evaluating practice. Further studies are in progress to identify barriers experienced by doctors in implementing the guidelines and problems in the process of referral to the anticoagulant clinic.
Full text
PDF
Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Davies G. C., Salzman E. W. Cost effectiveness of prophylaxis of venous thromboembolism. J R Soc Med. 1981 Mar;74(3):177–180. doi: 10.1177/014107688107400302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Doble N., Baron J. H. Anticoagulation control with warfarin by junior hospital doctors. J R Soc Med. 1987 Oct;80(10):627–627. doi: 10.1177/014107688708001009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gabbay J., McNicol M. C., Spiby J., Davies S. C., Layton A. J. What did audit achieve? Lessons from preliminary evaluation of a year's medical audit. BMJ. 1990 Sep 15;301(6751):526–529. doi: 10.1136/bmj.301.6751.526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schulman S., Lockner D., Bergström K., Blombäck M. Intensive initial oral anticoagulation and shorter heparin treatment in deep vein thrombosis. Thromb Haemost. 1984 Dec 29;52(3):276–280. [PubMed] [Google Scholar]