Abstract
Purpose
Chronic kidney disease (CKD) patients tend to have higher serum magnesium values than healthy population due to their positive balance of magnesium in kidney. Recent studies found that magnesium level is positively correlated with endothelial function. Therefore, this study was conducted to define the relationship between magnesium level and endothelial dysfunction in end stage renal disease (ESRD) patients on hemodialysis (HD).
Materials and Methods
A total of 27 patients were included in this cross-sectional study. Iontophoresis with laser-Doppler flowmetry, flow mediated dilation (FMD), and carotid intima-media thickness were measured. Patients' average serum magnesium levels were measured over previous three months, including the examination month. Pearson's correlation coefficient analysis and multivariate regression model were used to define the association between magnesium and endothelial function.
Results
In the univariate analysis, higher magnesium levels were associated with better endothelium-dependent vasodilation (EDV) of the FMD in ESRD patients on HD (r=0.516, p=0.007). When the participants were divided into two groups according to the median magnesium level (3.47 mg/dL), there was a significant difference in EDV of FMD (less than 3.47 mg/dL, 2.8±1.7%; more than 3.47 mg/dL, 5.1±2.0%, p=0.004). In multivariate analysis, magnesium and albumin were identified as independent factors for FMD (β=1.794, p=0.030 for serum magnesium; β=3.642, p=0.012 for albumin).
Conclusion
This study demonstrated that higher serum magnesium level may be associated with better endothelial function in ESRD patients on HD. In the future, a large, prospective study is needed to elucidate optimal range of serum magnesium levels in ESRD on HD patients.
Keywords: Magnesium, hemodialysis, microcirculation, endothelium
INTRODUCTION
Magnesium is the most abundant intracellular bivalent cation. It plays a major role in overall cell functions, including DNA and protein synthesis, glucose and fat metabolism, oxidative phosphorylation, neuromuscular excitability, and enzyme activity.1 Magnesium is also well known for its important roles in maintaining mineral bone metabolism and regulating vascular tone. Several studies have reported that magnesium deficiency is associated with the development of atherosclerosis and vascular diseases.2,3 Other studies in animals and humans have demonstrated that magnesium supplementation can limit atherosclerosis and decrease the intima-media thickness.4,5 Atherosclerosis can be attributed to endothelial dysfunction, which was demonstrated by several studies that endothelial dysfunction is present in the preclinical stage of atherosclerosis.6
Most of magnesium contents in human body is deposited in intracellular compartment (bone, 85%, soft tissue and liver, 14%), with only 1% present in the extracellular compartment. A trace amount of magnesium is absorbed from the intestine. However, this absorbed magnesium is mostly excreted through the kidney or/and intestine itself in order to maintain its proper magnesium balance. Excreted magnesium accounts for less than 1% of the total stores.7 For chronic kidney disease (CKD), urinary magnesium excretion may be normal or even increased until the glomerular filtration rate falls to ≤30 mL/min. As CKD progresses (<30 mL/min), urinary magnesium excretion is inadequate to balance intestinal magnesium absorption, at which dietary magnesium intake becomes a major determinant of serum and total body magnesium levels.8 In the case of patients receiving hemodialysis (HD), administration of magnesium-containing medication and high magnesium content of the dialysate are largely contributable for magnesium balance.9 Consequently, they are more likely to have elevated serum magnesium concentration and to be at risk for magnesium overload than are patients with functioning kidneys.8
To our knowledge, there are few prior studies that addressed the relationship between the serum magnesium level and endothelial dysfunction in patients with end-stage renal disease (ESRD) undergoing HD. Therefore, the aim of this study was to define this relationship using flow mediated dilation (FMD) and iontophoresis with laser-Doppler flowmetry (LDF), and carotid intima-media thickness (cIMT).
MATERIALS AND METHODS
Subjects and study design
A total of 27 HD patients from Ewha Womans University Mokdong Hospital Dialysis Center between February 2011 and September 2012 were enrolled. The participants who were undergoing HD for at least three months were between 18 and 65 years of age. They were medically stable (without any acute illnesses, significant infections, inflammation, or malignancies) and anuric with urine output of <100 mL/day, which can be seen as loss of residual renal function. HD was maintained using bicarbonate dialysate with the following electrolyte concentration: sodium 140 mEq/L, potassium 2.0 mEq/L, chloride 120 mEq/L, calcium 3.0 mEq/L, phosphate 0 mEq/L, magnesium 1.0 mEq/L (1.2 mg/dL), and bicarbonate 30 mEq/L. Data were collected from the medical record, including enrollment information and previous medical history. To evaluate endothelial function and atherosclerosis, FMD, iontophoresis with LDF, and cIMT were measured prior to starting a dialysis session after the patients had fasted for at least 8 hours. Each subject avoided food, drugs, tobacco, alcohol, coffee, or tea 10 hours prior to the test and had 20 minutes of acclimation in supine position before the test.
This protocol was approved by the hospital's ethics committee. All patients gave written informed consent before participating.
Assessment of endothelial function
Flow-mediated dilation (FMD)
Measurements were made by a single observer using a SONOS 5500 ultrasound system (Philips North America Corporation, Andover, MA, USA) with a 11-MHz probe. Brachial FMD was assessed using methods described previously by Celermajer, et al.10 Briefly, after 20 minutes of resting in the supine position in a temperature controlled room (22–24℃), the patient's study arm was extended and comfortably immobilized throughout the measurement. Changes in the luminal diameter of the brachial were measured during the reactive hyperemia phase in order to assess endothelium-dependent vasodilation. After the subjects had been lying down for 15 minutes, endothelium-independent vasodilation was measured based on the change in the luminal diameter of the brachial artery in response to 0.6 mg nitroglycerine. The lag times from the baseline to the initial reaction and peak reaction were defined as the initial reaction time and peak reaction time, respectively.
Iontophoresis with laser-Doppler flowmetry (LDF)
Iontophoresis employs electrically repulsive forces to deliver locally applied drug across the skin for therapeutic and diagnostic purposes. It is a non-invasive and proper tool to determine endothelial dysfunction.11 LDF measures cutaneous blood perfusion using the principle of the Doppler shift for lasers; it provides a linear relationship with the velocity of red blood cells.12
During the acclimation period, subjects sat in a comfortable chair for 20 minutes in a temperature-controlled room (22–24℃). Alcohol-soaked cotton was used to clean the skin of the forearm. Two drug delivery chamber electrodes (PF 383; Perimed, Järfälla, Sweden) were used for delivering acetylcholine (Ach) and sodium nitroprusside (SNP) on the skin. The drug delivery electrode were attached to the volar aspect of the forearm at a distance of 10 cm. Indifferent electrodes (PF 384, Perimed, Järfälla, Sweden) were attached to the forearm at a distance of 10 mm from paired drug delivery electrodes and provided the current needed for Ach and SNP delivery. Next, 0.05 mL of 1% solutions of Ach and sodium SNP were injected into the anodal and cathodal chambers to measure the endothelial-dependent and endothelial-independent responses, respectively. 13 The laser-Doppler probe (PF 408, Perimed, Järfälla, Sweden), connected to the LDF (PF 4001, Perimed, Järfälla, Sweden) was fixed within the drug chamber in order to explore the same small area of the skin. The laser Doppler outputs were recorded continuously using an interfaced computer equipped with acquisition software as arbitrary units (perfusion units, PU). After recording five minutes of stable baseline perfusion, dose-response curves to Ach and SNP were obtained with stepwise current applications.14 Ach was delivered in six doses (0.1 mA for 20 seconds each), followed by another two doses (0.2 mA for 20 seconds each) with 180 seconds in interval between the two successive doses. The absolute maximal response was defined as the flow rate reached after the last drug delivery. In order to eliminate the baseline variability, the blood flow responses to locally delivered Ach and SNP were expressed as ratios of response PU to baseline PU.11
Intima-media thickness of the common carotid artery (cIMT)
Carotid ultrasonography was performed using a 10-MHz scanning frequency in B mode. The carotid IMT was analyzed using a computer-based software called Intimascope® (Media Cross Co. Ltd., Tokyo, Japan).15 With the subject in the supine position, one skillful observer scanned the vessel in transverse planes. Images were obtained 20 mm proximal to the origin of the bulb at the far wall of the right common carotid artery. The computer-based IMT was evaluated by three methods, including 3-point, maximal, and average evaluations. Three-point evaluation refers to the average value of 3-point IMT, including two end points and the middle point in the >2 cm region. Maximal evaluation was obtained by the IMT value at the region's maximal point. Average IMT was the average value of 250 computer-based points in the region. In this study, average IMT was used because the computer-automated average IMT evaluations was thought to be more reliable indices for atherosclerosis rather than 3-point evaluation.15
Biochemical analyses
Venous blood was sampled just before the start of a dialysis session after 8 hour of fasting. Routine laboratory methods were used to measure serum albumin, total calcium, phosphate, total cholesterol, triglycerides, high-density lipoprotein, low-density lipoprotein and intact parathyroid hormone (PTH) in the blood. Serum magnesium was measured using the Xylene blue method (Clinimate MG kit, Sekisui Medical Co. Ltd., Tokyo, Japan). In healthy subjects, serum magnesium ranges between 1.9 and 3.1 mg/dL (0.79–1.29 mmol/L). The laboratory data (except magnesium) was taken from those at the beginning of the month, on which the endothelial function tests were carried out.
Statistical analyses
All data are expressed as means±SDs. Student's t-tests were used to assess differences in the means between two groups. Pearson's rank correlation was used to determine correlations between paired variables. Stepwise multivariate regression analysis was used to assess the predictors for FMD. p values<0.05 were considered statistically significant. All calculations were performed using SPSS 18.0 (SPSS Inc., Chicago, IL, USA).
RESULTS
Baseline characteristics
A total of 27 patients between 33 and 64 years old were included (12 men, 15 women). The baseline demographic and clinical characteristics are shown in Table 1. The etiology of CKD in this study included diabetes mellitus, hypertension, glomerulonephritis, and trauma, in order of decreasing frequency. All patients with cardiovascular disease were being treated for diabetes mellitus. One patient with cerebrovascular disease was not diagnosed with diabetes mellitus. There were no patients with peripheral vascular disease. Two patients (on male and one female) were current smokers.
Table 1. Baseline Characteristics.
| Variables | n=27 |
|---|---|
| Age, yrs (range) | 52 (33–64) |
| Sex, M/F | 12/15 |
| Etiology of chronic kidney disease, number of patients | |
| Diabetes mellitus | 11 |
| Hypertension | 5 |
| Chronic glomerulonephritis | 3 |
| Trauma | 1 |
| Unknown | 7 |
| Current smoker | 2 |
| History, number of patients | |
| Cardiovascular disease | 3 |
| Cerebrovascular disease | 3 |
| Peripheral vascular disease | 0 |
Biochemical and vascular assessments
The biochemical and vascular assessments are presented in Table 2. The average serum magnesium concentration (3.43±0.46 mg/dL, range 2.47–4.5 mg/dL) was higher than the normal limit (1.9–3.1 mg/dL). Phosphorus, uric acid, and intact PTH were also higher than the references values. In the endothelial dysfunction test, FMD (3.9±2.2%) was lower than the nitroglycerin-mediated dilation (NMD, 11.7±6.7%). The response to Ach-induced iontophoresis (8.5±4.3), however, was greater than that of SNP-induced iontophoresis (7.5±4.5). The average cIMT of 18 subjects was <1 mm (0.80±0.10 mm).
Table 2. Biochemical and Vascular Assessment.
| Variables | Mean±standard deviation (n)* |
|---|---|
| Laboratory finding | |
| Magnesium (mg/dL) | 3.43±0.46 (27) |
| Hemoglobin (g/dL) | 10.27±0.61 (27) |
| Blood urea nitrogen (mg/dL) | 71.96±15.14 (27) |
| Creatinine (mg/dL) | 10.82±2.82 (27) |
| Albumin (g/dL) | 3.81±0.30 (27) |
| Total cholesterol (mg/dL) | 139.93±30.27 (27) |
| Triglycerides (mg/dL) | 112.81±69.23 (27) |
| Low density cholesterol (mg/dL) | 78.09±22.27 (11) |
| Total calcium (mg/dL) | 8.51±0.81 (27) |
| Phosphorus (mg/dL) | 5.31±1.00 (27) |
| Uric acid (mg/dL) | 7.77±0.93 (27) |
| Intact parathyroid hormone (pg/mL) | 154.86±148.32 (27) |
| Vascular assessment | |
| Flow-mediated dilation (%) | 3.9±2.2 (26) |
| Nitroglycerine-mediated dilation (%) | 11.7±6.7 (26) |
| Acetylcholine-induced iontophoresis (ratio of response to baseline) | 8.5±4.3 (27) |
| Nitropurusside-induced iontophoresis (ratio of response to baseline) | 7.5±4.5 (27) |
| Carotid intima media thickness (mm) | 0.80±0.10 (18) |
*Number of case.
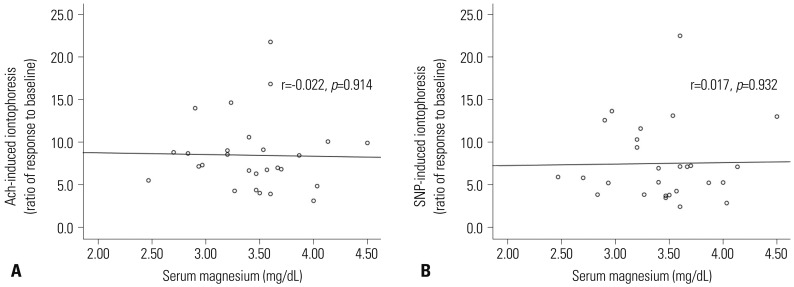
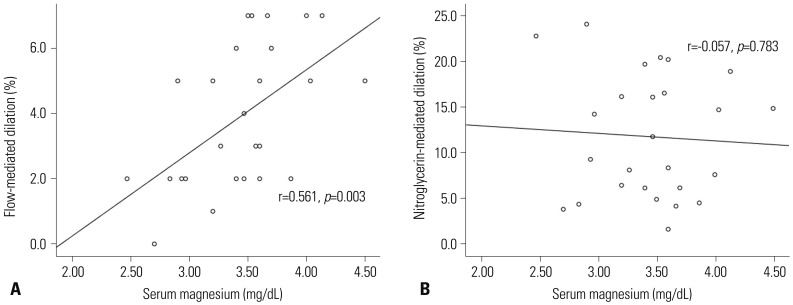
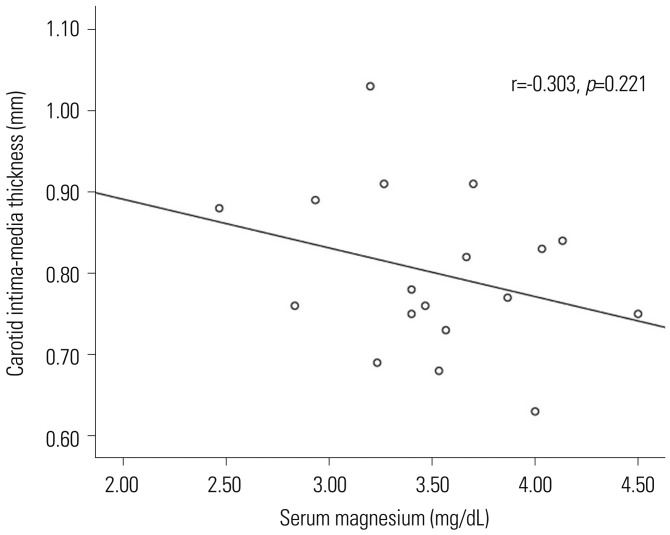
The relationship between the serum magnesium concentration and vascular parameters was evaluated (Figs. 1, 2, and 3). There was a strong positive relationship between FMD and the serum magnesium concentration (r=0.561, p=0.003) (Fig. 2A), in contrast to NMD (r=-0.057, p=0.783) (Fig. 2B). Both Ach-induced and SNP-induced ratio of response to baseline from iontophoresis with LDF had weak correlation with statistical insignificance (r=-0.022, p=0.914) (Fig. 1A) (r=0.017, p=0.932) (Fig. 1B).
Fig. 1. Scatter plot of the relationships between serum magnesium concentration and endothelial function using iontophoresis with laser-Doppler flowmetry. Neither endothelium-dependent vascular dilation (A) nor endothelium-independent vascular dilation (B) was significantly related to serum magnesium. Ach, acetylcholine; SNP, sodium nitroprusside.
Fig. 2. Scatter plot of the relationships between serum magnesium concentration and endothelial function, measured by flow mediated dilation. Endothelium-dependent vasodilation (A) is significantly associated with serum magnesium. There is no significant trend in endothelium-independent vasodilatation (B).
Fig. 3. Negative relationship between serum magnesium concentration and carotid intima-media thickness (p=0.221).
The cIMT decreased with increasing serum magnesium concentration, which was not statistically significant (p=0.221).
Measurements comparisons based on the median magnesium concentration
We compared the laboratory parameters and vascular assessments of patients with magnesium levels above and below the median value (3.47 mg/dL), shown in Table 3. One group (n=14 patients) had serum magnesium levels below the median value, and other group (with 13 patients) had the levels above the median value. The FMD was significantly different between the two groups (2.8±1.7% below vs. 5.1±2.0% above, p=0.004). However, there were inconsistent values between the two groups with regard to the other endothelial dysfunction, measured by iontophoresis with LDF and cIMT.
Table 3. Measurement Comparisons Based on the Median Magnesium Value.
| Mg<3.47 mg/dL (n=14) | Mg≥3.47 mg/dL (n=13) | p value | |
|---|---|---|---|
| Laboratory findings | |||
| Hemoglobin (g/dL) | 10.27±0.78 | 10.26±0.37 | 0.985 |
| Blood urea nitrogen (mg/dL) | 70.69±16.17 | 73.33±14.47 | 0.659 |
| Creatinine (mg/dL) | 10.33±3.38 | 11.35±2.05 | 0.350 |
| Albumin (g/dL) | 3.72±0.32 | 3.90±0.24 | 0.119 |
| Total cholesterol (mg/dL) | 132.64±28.62 | 147.77±31.13 | 0.200 |
| Triglycerides (mg/dL) | 107.14±67.34 | 118.92±73.43 | 0.667 |
| Low density cholesterol (mg/dL) | 65.25±14.17 | 56.00±33.67 | 0.619 |
| Total calcium (mg/dL) | 8.60±0.74 | 8.42±0.89 | 0.569 |
| Phosphorus (mg/dL) | 5.42±0.97 | 5.18±1.06 | 0.534 |
| Uric acid (mg/dL) | 7.87±0.99 | 7.66±0.90 | 0.568 |
| Intact parathyroid hormone (pg/mL) | 158.47±111.63 | 150.97±184.74 | 0.889 |
| Vascular assessment | |||
| Ach-induced iontophoresis (ratio of response to baseline) | 8.3±3.1 | 8.7±5.3 | 0.819 |
| SNP-induced iontophoresis (ratio of response to baseline) | 7.2±3.6 | 7.8±5.5 | 0.773 |
| Flow-mediated dilatation (%) | 2.8±1.7 | 5.1±2.0 | 0.004 |
| Nitroglycerine-mediated dilatation (%) | 12.5±6.9 | 11.0±6.8 | 0.571 |
| Carotid intima-media thickness (mm) | 0.83±0.11 | 0.77±0.09 | 0.252 |
Ach, acetylcholine; SNP, sodium nitroprusside.
Factors associated with flow-mediated dilation
There was a significant correlation between FMD and serum magnesium levels. Multivariate analysis was performed in order to determine the factors associated with FMD. Variables that were significant in univariate analysis were included in the multivariate regression analysis. These included age, gender, diabetes mellitus, history of cerebrovascular disease, albumin, calcium, phosphorus, and intact PTH. Serum magnesium and albumin were found to be independent factors for FMD (β=1.794, p=0.030 for serum magnesium; β=3.642, p=0.012 for albumin) (Table 4).
Table 4. Univariate and Multivariate Analysis of the Factors Associated with FMD.
| Univariate* | Multivariate | |||
|---|---|---|---|---|
| r | p value | β | p value | |
| Age | NS | - | ||
| Female | 0.468 | 0.016 | 0.801 | 0.292 |
| Diabetes mellitus | NS | - | ||
| Cerebrovascular disease | -0.390 | 0.049 | -0.918 | 0.284 |
| Albumin (g/dL) | 0.550 | 0.004 | 3.642 | 0.012 |
| Total calcium (mg/dL) | NS | - | ||
| Phosphorus (mg/dL) | NS | - | ||
| Intact PTH (pg/mL) | NS | - | ||
| Magnesium (mg/dL) | 0.549 | 0.004 | 1.794 | 0.030 |
FMD, flow-mediated dilation; PTH, parathyroid hormone.
*Statistically significant (p<0.05) p values as assessed by Pearson's correlation, as well as β estimates and p values from multivariate regression models. The r2 of the multivariate model was 0.638. Variables known to influence FMD (age, sex, diabetes mellitus, history of cerebrovascular disease, albumin, calcium, phosphorus, intact PTH) were included in the multivariate analyses.
The relationship between intact PTH and magnesium
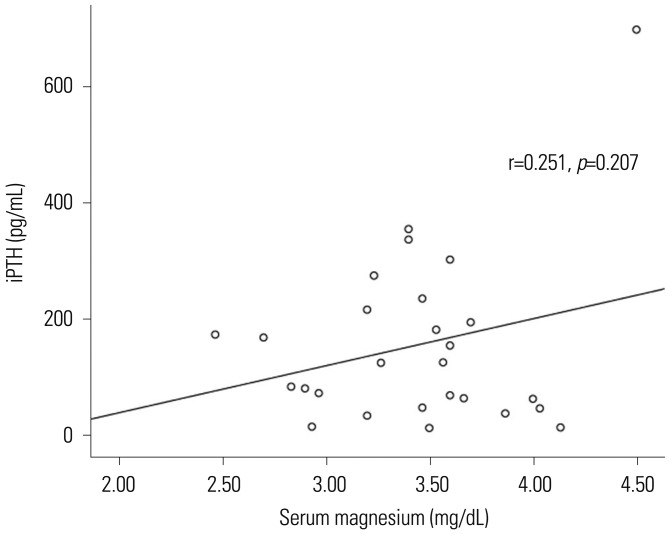
As shown in Fig. 4, the univariate analysis showed positive correlation (r=0.251) between intact PTH and magnesium, although it was not statistically significant (p=0.207).
Fig. 4. Positive relationship between serum magnesium concentration and iPTH (p=0.207). iPTH, intact parathyroid hormone.
DISCUSSION
Systemic endothelial dysfunction is an early triggering event in the pathogenesis of atherosclerosis, hypertension and cardiovascular disease.16 A loss of endothelium-dependent vasodilation precedes structural atherosclerotic lesions.6,17 Endothelial dysfunction was identified in a child with known risk factors for later cardiovascular disease.18,19 Therefore, evaluating the function of the vascular endothelium allows detection and prevention of cardiovascular diseases.
Hypomagnesemia is believed to play a significant role in the development of cardiovascular disease, hypertension, and thrombosis in the general population.20,21 Magnesium is well known to modulate vascular tone and response, and act as a cofactor for Ach-induced endothelium-dependent relaxation.1 Magnesium deficiency promotes oxidative stress in various cell types, including endothelial cells.22,23 In addition, oral magnesium therapy is associated with significant improvement in endothelial function in patients with coronary artery disease.24 Baseline serum magnesium levels are higher in patients with CKD than those in healthy population due to their positive balance of magnesium in kidney.25 Thus, it is important to define the relationship between serum magnesium levels and endothelial dysfunction in CKD patients on HD because cardiovascular complications are the most common cause of death among dialysis patients.
Our present data demonstrated that macrovascular endothelial function is significantly correlated with serum magnesium levels in patients on HD, whereas microvascular endothelial function (presented as iontophoresis with LDF) was not significantly related to serum magnesium values. Although not significant, there was also positive correlation between cIMT and serum magnesium level.
FMD has been established as valid method of assessing macrovascular endothelial function in patients at risk for atherosclerosis and other cardiovascular diseases. We found that FMD was positively correlated with serum magnesium. This suggests that higher magnesium values may actually improve macrovascular endothelial function in patients undergoing HD. The reactive hyperemia during FMD measurement produces a shear stress stimulus that induces the endothelium to release nitric oxide (NO), a vasodilator.26 Endothelial dysfunction refers to a worsening in endothelium-dependent relaxation. Endothelial dysfunction is normally mediated by compounds including NO, prostacyclin, and endothelium-derived hyperpolarizing factors (EDHFs), which directly facilitate vascular smooth muscle cell relaxation.27 Magnesium is thought to modify the vascular tone not only by regulating the endothelial and smooth muscle cell functions, but also by playing a role in the classical pathway of NO release. One animal experiment demonstrated that magnesium increases the production of prostacyclin and NO, which ultimately promote endothelium-independent and endothelium-dependent vasodilation, respectively.28 Similarly, our study confirmed this positive relationship between serum magnesium and FMD, especially in patients on HD. In addition, serum magnesium levels may actually be protective against macrovascular disease.
Unlike FMD of the brachial artery, there are no standardized assessments of endothelial function in the microvasculature. Iontophoresis with LDF is one of non-invasive methods to assess microvascular endothelial function. This technology uses transdermal delivery of selective endothelium-dependent vasodilators, such as Ach in this study. The non-NO dependent vasodilatory pathway is likely to play a more critical role in the peripheral microcirculation than it does in the macrocirculation. In other words, the contributions of recovered EDHF, which was suppressed by NO, or compensatorily enhanced prostanoid-dependent vasodilatory response is the determining factor for the preservation of endothelial function of microvessels. 29 EDHF is a non-characterized endothelial-factor that plays a role in non-NO, non-prostaglandin-mediated endothelium-dependent vasodilation. It ultimately causes hyperpolarization and relaxation of vascular smooth muscle cells.29 The EDHF contribution is inversely correlated with vessel size. The predominant EDHF activity occurs in resistance vessels. In smaller vessels, there is a compensatory upregulation of EDHF under conditions of reduced NO bioavailability. 29 In this study, exogenous transdermal Ach induced peripheral vasodilation through a non-NO dependent pathway. Ach has been shown to mediate cutaneous vasodilation through both prostanoid and non-NO, non-prostanoid-dependent pathways. This phenomenon suggests that there is no direct role for NO in vasodilation.30 These findings are supported by an in vitro study, which demonstrated that Ach relaxation is mainly dependent on a non-NO, non-prostanoid endothelium-dependent hyperpolarization.31 Studies that have used iontophoresis application of Ach have also demonstrated that NO plays a limited role in the cutaneous response to Ach.32,33 Other researchers have suggested that prostaglandins act in the late phase of Ach-induced iontophoresis.34 Ultimately, it appears that the NO contribution in the peripheral microcirculation is smaller than in the macrocirculation. In addition, cutaneous Ach-mediated iontophoresis is unresponsive regardless of the serum magnesium level. Consequently, the irrelevant response to Ach-mediated iontophoresis in the present study is expected.
cIMT assessment is an established tool for detecting and monitoring atherosclerosis progression.35 In this study, rising serum magnesium levels were associated with decreased cIMT, although the correlation was not statistically significant. Previously, HD patients were studied with regard to the relationship between magnesium level (intra- and extracellular) and atherosclerosis (as measured using the cIMT).36 HD patients were found to have significantly higher mean common cIMTs than controls patients, and their serum magnesium and intracellular magnesium were negatively associated with the common cIMT. This suggests that magnesium may play a protective role in the development and acceleration of atherosclerosis in patients with chronic renal insufficiency.
The interplay between intact PTH and magnesium is complicated. Several studies have reported that hypermagnesemia play a role for inhibition of PTH secretion, presenting a significant linear inverse correlation between PTH and magnesium in patients on peritoneal dialysis as well as HD.37 However, a linear correlation was statistically insignificant. PTH may be regulated by phosphorus and calcium rather than magnesium, and these factors are tied up for sustaining homeostasis. Baradaran and Nasri38 reported that magnesium was correlated with serum 25-OH Vit D level rather than PTH, concluding that factors such as serum 25-OH Vit D rather than serum magnesium might be more important for regulation of PTH secretion. Additionally, when we analyzed the relationship between PTH and endothelial function, there was no obvious correlation between them (not shown). Therefore, future studies are required to ascertain the relationship between magnesium and PTH.
This study has several limitations. Given its cross-sectional design, the case and effect relationships cannot be determined. Assessments were performed only one time and were not based on a time series. In addition, because the control group was not settled, these data cannot be generalized to all dialysis patients. Another limitation is that there is no objective reference to define endothelial dysfunction as assessed by iontophoresis with LDF. In order to describe the blood volume change, we used a ratio of response to baseline PU. However, there are no reference values of iontophoresis in HD patients. Finally, although each magnesium level ranged either above or within the upper limit of normal reference, the participants did not show any symptoms from hypermagnesemia. Furthermore, because there were no signs of toxicity, we could not propose the upper limit of magnesium concentration, which may positively affect the endothelial function. Regardless of despite these limitations, our study is the first to suggest that serum magnesium prevents endothelial dysfunction in HD patients.
In conclusion, higher serum magnesium levels in hemodilaysis patients may have a beneficial effect on endothelial dysfunction. In the future, a large prospective study of HD patients is needed to clarify the relationship between serum magnesium and endothelial function. Furthermore, it is important to define the optimal magnesium reference range in patients with end stage renal disease undergoing HD.
Footnotes
The authors have no financial conflicts of interest.
References
- 1.Altura BM, Altura BT. New perspectives on the role of magnesium in the pathophysiology of the cardiovascular system. I. Clinical aspects. Magnesium. 1985;4:226–244. [PubMed] [Google Scholar]
- 2.Reffelmann T, Ittermann T, Dörr M, Völzke H, Reinthaler M, Petersmann A, et al. Low serum magnesium concentrations predict cardiovascular and all-cause mortality. Atherosclerosis. 2011;219:280–284. doi: 10.1016/j.atherosclerosis.2011.05.038. [DOI] [PubMed] [Google Scholar]
- 3.Amighi J, Sabeti S, Schlager O, Mlekusch W, Exner M, Lalouschek W, et al. Low serum magnesium predicts neurological events in patients with advanced atherosclerosis. Stroke. 2004;35:22–27. doi: 10.1161/01.STR.0000105928.95124.1F. [DOI] [PubMed] [Google Scholar]
- 4.Ouchi Y, Tabata RE, Stergiopoulos K, Sato F, Hattori A, Orimo H. Effect of dietary magnesium on development of atherosclerosis in cholesterol-fed rabbits. Arteriosclerosis. 1990;10:732–737. doi: 10.1161/01.atv.10.5.732. [DOI] [PubMed] [Google Scholar]
- 5.Turgut F, Kanbay M, Metin MR, Uz E, Akcay A, Covic A. Magnesium supplementation helps to improve carotid intima media thickness in patients on hemodialysis. Int Urol Nephrol. 2008;40:1075–1082. doi: 10.1007/s11255-008-9410-3. [DOI] [PubMed] [Google Scholar]
- 6.McLenachan JM, Williams JK, Fish RD, Ganz P, Selwyn AP. Loss of flow-mediated endothelium-dependent dilation occurs early in the development of atherosclerosis. Circulation. 1991;84:1273–1278. doi: 10.1161/01.cir.84.3.1273. [DOI] [PubMed] [Google Scholar]
- 7.Floege J, Johnson RJ, Feehally J. Comprehensive clinical nephrology. 4th ed. St. Louis: Elsevier Health Sciences; 2010. [Google Scholar]
- 8.Navarro-González JF, Mora-Fernández C, García-Pérez J. Clinical implications of disordered magnesium homeostasis in chronic renal failure and dialysis. Semin Dial. 2009;22:37–44. doi: 10.1111/j.1525-139X.2008.00530.x. [DOI] [PubMed] [Google Scholar]
- 9.Truttmann AC, Faraone R, Von Vigier RO, Nuoffer JM, Pfister R, Bianchetti MG. Maintenance hemodialysis and circulating ionized magnesium. Nephron. 2002;92:616–621. doi: 10.1159/000064109. [DOI] [PubMed] [Google Scholar]
- 10.Celermajer DS, Sorensen K, Ryalls M, Robinson J, Thomas O, Leonard JV, et al. Impaired endothelial function occurs in the systemic arteries of children with homozygous homocystinuria but not in their heterozygous parents. J Am Coll Cardiol. 1993;22:854–858. doi: 10.1016/0735-1097(93)90203-d. [DOI] [PubMed] [Google Scholar]
- 11.Cupisti A, Rossi M, Placidi S, Caprioli R, Morelli E, Vagheggini G, et al. Responses of the skin microcirculation to acetylcholine and to sodium nitroprusside in chronic uremic patients. Int J Clin Lab Res. 2000;30:157–162. doi: 10.1007/s005990070015. [DOI] [PubMed] [Google Scholar]
- 12.Niwayama J, Sanaka T. Development of a new method for monitoring blood purification: the blood flow analysis of the head and foot by laser Doppler blood flowmeter during hemodialysis. Hemodial Int. 2005;9:56–62. doi: 10.1111/j.1492-7535.2005.01118.x. [DOI] [PubMed] [Google Scholar]
- 13.Morris SJ, Shore AC, Tooke JE. Responses of the skin microcirculation to acetylcholine and sodium nitroprusside in patients with NIDDM. Diabetologia. 1995;38:1337–1344. doi: 10.1007/BF00401767. [DOI] [PubMed] [Google Scholar]
- 14.Davis KR, Ponnampalam J, Hayman R, Baker PN, Arulkumaran S, Donnelly R. Microvascular vasodilator response to acetylcholine is increased in women with pre-eclampsia. BJOG. 2001;108:610–614. doi: 10.1111/j.1471-0528.2001.00144.x. [DOI] [PubMed] [Google Scholar]
- 15.Yanase T, Nasu S, Mukuta Y, Shimizu Y, Nishihara T, Okabe T, et al. Evaluation of a new carotid intima-media thickness measurement by B-mode ultrasonography using an innovative measurement software, intimascope. Am J Hypertens. 2006;19:1206–1212. doi: 10.1016/j.amjhyper.2006.05.010. [DOI] [PubMed] [Google Scholar]
- 16.Verma S, Anderson TJ. Fundamentals of endothelial function for the clinical cardiologist. Circulation. 2002;105:546–549. doi: 10.1161/hc0502.104540. [DOI] [PubMed] [Google Scholar]
- 17.Celermajer DS, Sorensen KE, Bull C, Robinson J, Deanfield JE. Endothelium-dependent dilation in the systemic arteries of asymptomatic subjects relates to coronary risk factors and their interaction. J Am Coll Cardiol. 1994;24:1468–1474. doi: 10.1016/0735-1097(94)90141-4. [DOI] [PubMed] [Google Scholar]
- 18.Celermajer DS, Sorensen KE, Gooch VM, Spiegelhalter DJ, Miller OI, Sullivan ID, et al. Non-invasive detection of endothelial dysfunction in children and adults at risk of atherosclerosis. Lancet. 1992;340:1111–1115. doi: 10.1016/0140-6736(92)93147-f. [DOI] [PubMed] [Google Scholar]
- 19.Martin H, Hu J, Gennser G, Norman M. Impaired endothelial function and increased carotid stiffness in 9-year-old children with low birthweight. Circulation. 2000;102:2739–2744. doi: 10.1161/01.cir.102.22.2739. [DOI] [PubMed] [Google Scholar]
- 20.Ma J, Folsom AR, Melnick SL, Eckfeldt JH, Sharrett AR, Nabulsi AA, et al. Associations of serum and dietary magnesium with cardiovascular disease, hypertension, diabetes, insulin, and carotid arterial wall thickness: the ARIC study. Atherosclerosis Risk in Communities Study. J Clin Epidemiol. 1995;48:927–940. doi: 10.1016/0895-4356(94)00200-a. [DOI] [PubMed] [Google Scholar]
- 21.Liao F, Folsom AR, Brancati FL. Is low magnesium concentration a risk factor for coronary heart disease? The Atherosclerosis Risk in Communities (ARIC) Study. Am Heart J. 1998;136:480–490. doi: 10.1016/s0002-8703(98)70224-8. [DOI] [PubMed] [Google Scholar]
- 22.Wiles ME, Wagner TL, Weglicki WB. Effect of acute magnesium deficiency (MgD) on aortic endothelial cell (EC) oxidant production. Life Sci. 1997;60:221–236. doi: 10.1016/s0024-3205(96)00619-4. [DOI] [PubMed] [Google Scholar]
- 23.Dickens BF, Weglicki WB, Li YS, Mak IT. Magnesium deficiency in vitro enhances free radical-induced intracellular oxidation and cytotoxicity in endothelial cells. FEBS Lett. 1992;311:187–191. doi: 10.1016/0014-5793(92)81098-7. [DOI] [PubMed] [Google Scholar]
- 24.Shechter M, Sharir M, Labrador MJ, Forrester J, Silver B, Bairey Merz CN. Oral magnesium therapy improves endothelial function in patients with coronary artery disease. Circulation. 2000;102:2353–2358. doi: 10.1161/01.cir.102.19.2353. [DOI] [PubMed] [Google Scholar]
- 25.Mordes JP, Wacker WE. Excess magnesium. Pharmacol Rev. 1977;29:273–300. [PubMed] [Google Scholar]
- 26.Ras RT, Streppel MT, Draijer R, Zock PL. Flow-mediated dilation and cardiovascular risk prediction: a systematic review with meta-analysis. Int J Cardiol. 2013;168:344–351. doi: 10.1016/j.ijcard.2012.09.047. [DOI] [PubMed] [Google Scholar]
- 27.Cracowski JL, Minson CT, Salvat-Melis M, Halliwill JR. Methodological issues in the assessment of skin microvascular endothelial function in humans. Trends Pharmacol Sci. 2006;27:503–508. doi: 10.1016/j.tips.2006.07.008. [DOI] [PubMed] [Google Scholar]
- 28.Northcott CA, Watts SW. Low [Mg2+]e enhances arterial spontaneous tone via phosphatidylinositol 3-kinase in DOCA-salt hypertension. Hypertension. 2004;43:125–129. doi: 10.1161/01.HYP.0000103631.68328.03. [DOI] [PubMed] [Google Scholar]
- 29.Ozkor MA, Quyyumi AA. Endothelium-derived hyperpolarizing factor and vascular function. Cardiol Res Pract. 2011;2011:156146. doi: 10.4061/2011/156146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Holowatz LA, Thompson CS, Minson CT, Kenney WL. Mechanisms of acetylcholine-mediated vasodilatation in young and aged human skin. J Physiol. 2005;563(Pt 3):965–973. doi: 10.1113/jphysiol.2004.080952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Buus NH, Simonsen U, Pilegaard HK, Mulvany MJ. Nitric oxide, prostanoid and non-NO, non-prostanoid involvement in acetylcholine relaxation of isolated human small arteries. Br J Pharmacol. 2000;129:184–192. doi: 10.1038/sj.bjp.0703041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Noon JP, Walker BR, Hand MF, Webb DJ. Studies with iontophoretic administration of drugs to human dermal vessels in vivo: cholinergic vasodilatation is mediated by dilator prostanoids rather than nitric oxide. Br J Clin Pharmacol. 1998;45:545–550. doi: 10.1046/j.1365-2125.1998.00718.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Khan F, Davidson NC, Littleford RC, Litchfield SJ, Struthers AD, Belch JJ. Cutaneous vascular responses to acetylcholine are mediated by a prostanoid-dependent mechanism in man. Vasc Med. 1997;2:82–86. doi: 10.1177/1358863X9700200202. [DOI] [PubMed] [Google Scholar]
- 34.Durand S, Tartas M, Bouyé P, Koïtka A, Saumet JL, Abraham P. Prostaglandins participate in the late phase of the vascular response to acetylcholine iontophoresis in humans. J Physiol. 2004;561(Pt 3):811–819. doi: 10.1113/jphysiol.2004.069997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Pignoli P, Tremoli E, Poli A, Oreste P, Paoletti R. Intimal plus medial thickness of the arterial wall: a direct measurement with ultrasound imaging. Circulation. 1986;74:1399–1406. doi: 10.1161/01.cir.74.6.1399. [DOI] [PubMed] [Google Scholar]
- 36.Tzanakis I, Virvidakis K, Tsomi A, Mantakas E, Girousis N, Karefyllakis N, et al. Intra- and extracellular magnesium levels and atheromatosis in haemodialysis patients. Magnes Res. 2004;17:102–108. [PubMed] [Google Scholar]
- 37.Navarro JF, Macía ML, Gallego E, Méndez ML, Chahín J, García-Nieto V, et al. Serum magnesium concentration and PTH levels. Is long-term chronic hypermagnesemia a risk factor for adynamic bone disease? Scand J Urol Nephrol. 1997;31:275–280. doi: 10.3109/00365599709070348. [DOI] [PubMed] [Google Scholar]
- 38.Baradaran A, Nasri H. Correlation of serum magnesium with serum parathormone levels in patients on regular hemodialysis. Saudi J Kidney Dis Transpl. 2006;17:344–350. [PubMed] [Google Scholar]