Abstract
As anatomical reduction of the articular surface of femoral head fractures and restoration of damaged cartilage are essential for good long-term results, many treatment options have been suggested, including fixation of the fracture using various surgical exposures and implants, as well as arthroscopic irrigation and debridement, bone marrow stimulating techniques, osteochondral allograft, autograft, and autogenous chondrocyte implantation. We report a case of osteochondral autograft harvested from its own femoral articular surface through surgical hip dislocation. The osteochondral graft was harvested from the inferior non-weight-bearing articular surface and grafted to the osteochondral defect. One year later, the clinical and radiological results were good, without the collapse of the femoral head or arthritic change. This procedure introduced in our case is considered convenient and able to lessen surgical time without morbidity of the donor site associated with the harvest.
Keywords: Femoral head, hip dislocation, autograft transplant, fractures cartilage
INTRODUCTION
Dashboard injury is the most common mechanism of femoral head fractures, commonly known as Pipkin fractures, and associated hip dislocation; the type of Pipkin fracture is determined by the orientation of the leg when the accident occurred.1,2 Pipkin type II fractures, in which the fracture line extends cephalad to the fovea into the weight-bearing surface of the femoral head, specifically require accurate alignment. Anatomical reduction of the fracture and restoration of injured cartilage generally yield good long-term results.3,4 All procedures should therefore focus on restoration of joint congruency and cartilage. Several treatment options such as arthroscopic lavage and debridement, marrow stimulation, osteochondral allograft, autograft, and autogenous chondrocyte implantation have been proposed for restoration of damaged cartilage and chondral defects.3,4,5,6,7 Hangody and Karpati introduced osteochondral autologous graft transplantation surgery (OATS) in the 1990s, and OATS remains a popular technique.7 We report a case of OATS for femoral head fracture with dislocation harvested from its own femoral articular surface through surgical hip dislocation. The osteochondral graft was harvested from the inferior non-weight-bearing articular surface and grafted to the osteochondral defect.
CASE REPORT
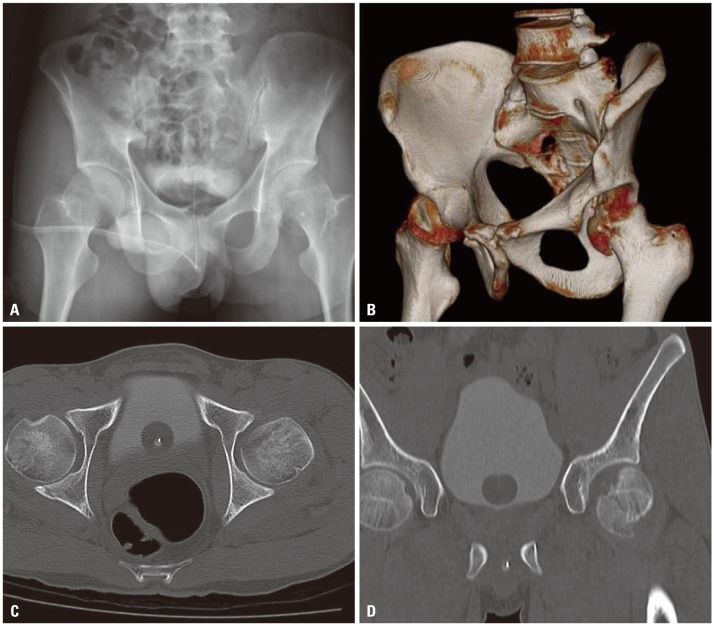
A 31-year-old healthy man presented after a fall during a soccer game that resulted in dislocated right posterior hip with fracture and acetabular wall fracture. In the emergency department, he was diagnosed with right posterior hip dislocation and Pipkin type II femoral head fracture with intra-articular bony fragments. Plain radiographs and a computed tomography scan confirmed the cephalad direction of the femoral head fracture extending around the fovea in the coronal plane, with bony fragments in the postero-superior and postero-inferior aspects of the joint (Fig. 1). One day after the accident, he underwent open reduction and internal fixation and OATS on his right hip and pelvis (Fig. 2).
Fig. 1. (A) Plain radiograph showing femoral head fracture. (B and C) CT scan showing Pipkin type II femoral head fracture. (D) CT sagittal scan show femoral defect of weight bearing portion.
Fig. 2. (A) 2.5×1 cm femoral head defect is visible after fixation of the main fragment. (B) OATS was performed with a bone plug harvested from the inferior non-weight bearing portion of the affected femoral head. (C) OATS was performed using a headless 3.5 mm compression screw. OATS, osteochondral autologous graft transplantation surgery.
A longitudinal incision was made distally from 5 cm above the tip of the greater trochanter, and the fascia lata was incised in line with the skin incision. An osteotomy that was introduced by Ganz, et al.8 was made on the lateral border of the femur after distal-to-proximal palpation of the vastus lateralis ridge. By gently externally rotating and flexing the leg, the vastus lateralis and intermedius were sharply dissected from the femur. A Z-type capsulotomy was made. In order to dislocate the hip, the leg was brought into further external rotation and flexed. By manipulating the leg, the femoral head and the acetabulum were exposed. The major fragment was reduced and fixed with three 3.5-mm cannulated screws (Fig. 2). Small fragments of the femoral head without capsular attachment could not be fixed. The cartilage defect was 2.5×1 cm and located vertically from the fovea to the proximal weight-bearing zone. The non-weight-bearing portion of cartilage was harvested. OATS was performed on the cartilage defect, and the harvested fragment was fixed with two 3.5-mm cannulated screws. The trochanteric osteotomy was reduced and fixed with three 3.5-mm screws. Weight bearing was prohibited for four weeks, followed by crutch ambulation for eight weeks.
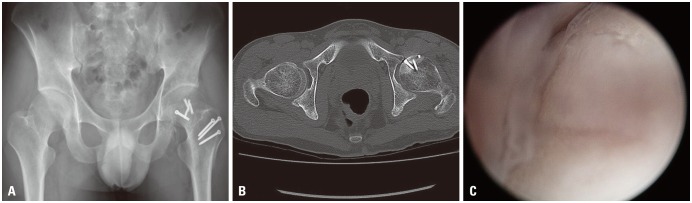
One year later, the surgical, clinical, and radiological results were good, without the collapse of the femoral head or arthritic change (Modified Harris Hip Score: 82 points). However, the patient had a decreased range of external hip rotation with 90 degrees of flexion. Adhesive capsulitis was suspected; thus, we performed arthroscopic capsulotomy (mainly posterior capsule), and the coexistent pathology was identified and addressed via labral debridement, synovectomy, and excision of fibrotic tissue from the acetabular fossa. The joint was accessed through a standard anterolateral portal and a mid-anterior portal, with direct visualization. The OATS site showed mild softening and fraying (Fig. 3). The overall surface of the OATS site was regenerated with fibrocartilage tissue and was otherwise normal. Before completing the operation, we performed brisement, resulting in 130 degrees of hip flexion on full external rotation.
Fig. 3. (A and B) One year after the operation, plain radiograph and CT scan shows good fixation and articulation. (C) Arthroscopic findings one year after the operation show mild fraying and softening, but the overall surface was regenerated with fibrocartilage tissue.
DISCUSSION
The good results of mosaicplasty when applied to the knee joint have led to its application to other joints, including the talus, tibial plateau, and humeral capitellum. Good clinical results of OATS for the knee joint were reported at 2-year follow-ups using clinical scores.9,10 Nam, et al.11 previously implemented OATS harvested from the non-weight-bearing knee joint for repair of a femoral head defect via arthrotomy in a 15-year-old boy. They fixed this portion with three bio-absorbable screws. Another case of OATS harvested from the lateral border of the lateral femoral condyle was performed on a 28-year-old man. Hart, et al.12 treated this case with posterior mosaicplasty of the osteochondral defect of the femoral head. In this report, we introduced and presented the initial clinical results of the use of an intact non-weight-bearing portion of the ipsilateral femoral articular cartilage to restore the osteochondral defect of the weight-bearing antero-superior articular surface of the femoral head. This procedure is considered to be convenient and is able to lessen surgical time without morbidity of the donor site associated with the harvest. However, compared to our case, harvest from other joints is likely to require more time and cost, and it may also increase the risk of surgical co-morbidity.
Utilization of the non-weight-bearing intact femoral surface was first reported in 1978 by Sugioka,13 and favorable results were reported. While scientific evidence to explain the relationship between transplantation and Sugioka's osteotomy is lacking, utilization of less-invasive methods such as OATS, compared to standard osteotomy and fixation, is expected to increase.
As Ganz, et al.8 described in 2001, surgical dislocation of the hip joint with osteotomy of the great trochanter of the femur can expose the acetabulum without the risk of avascular necrosis and avoid injury to the medial femoral circumflex artery. With this technique, we can access and handle the whole aspect of the femoral head in order to harvest the proper articular surface.
Among the indications for OATS, the recommended location and size of the graft differ among authors. In cases of osteonecrosis of a femoral head treated with OATS, outcomes of the large-sized pre-collapse stage are compared to those of the small- and medium-sized pre-collapse stages among cases with unsuccessful results.14 Under certain conditions, mosaicplasty can be used as a salvage procedure for defects as large as 8 to 9 cm2, although such extension of the indication can result in a higher rate of donor-site morbidity.15 Autogenous osteochondral mosaicplasty is an innovative and promising treatment for focal chondral and osteochondral articular surface defects that are between 1 and 4 cm2 in size. The success of the procedure depends largely on adherence to proper indications and caution regarding technical details.15
We believe that surgical dislocation combined with OATS harvested from the ipsilateral femoral head is a good option for osteochondral defects in femoral head fractures, as it offers sufficient exposure of the femoral head while preserving its vasculature and minimizes the damage to other joints and other complications, which enables proper restoration of the articular cartilage surface.
Footnotes
The authors have no financial conflicts of interest.
References
- 1.Pipkin G. Treatment of grade IV fracture-dislocation of the hip. J Bone Joint Surg Am. 1957;39-A:1027–1042 passim. [PubMed] [Google Scholar]
- 2.Davis JB. Simultaneous femoral head fracture and traumatic hip dislocation. Am J Surg. 1950;80:893–895. doi: 10.1016/0002-9610(50)90473-9. [DOI] [PubMed] [Google Scholar]
- 3.Butler JE. Pipkin Type-II fractures of the femoral head. J Bone Joint Surg Am. 1981;63:1292–1296. [PubMed] [Google Scholar]
- 4.Henle P, Kloen P, Siebenrock KA. Femoral head injuries: which treatment strategy can be recommended? Injury. 2007;38:478–488. doi: 10.1016/j.injury.2007.01.023. [DOI] [PubMed] [Google Scholar]
- 5.Hougaard K, Thomsen PB. Traumatic posterior fracture-dislocation of the hip with fracture of the femoral head or neck, or both. J Bone Joint Surg Am. 1988;70:233–239. [PubMed] [Google Scholar]
- 6.Mowery C, Gershuni DH. Fracture dislocation of the femoral head treated by open reduction and internal fixation. J Trauma. 1986;26:1041–1044. doi: 10.1097/00005373-198611000-00014. [DOI] [PubMed] [Google Scholar]
- 7.Kish G, Módis L, Hangody L. Osteochondral mosaicplasty for the treatment of focal chondral and osteochondral lesions of the knee and talus in the athlete. Rationale, indications, techniques, and results. Clin Sports Med. 1999;18:45–66. vi. doi: 10.1016/s0278-5919(05)70129-0. [DOI] [PubMed] [Google Scholar]
- 8.Ganz R, Gill TJ, Gautier E, Ganz K, Krügel N, Berlemann U. Surgical dislocation of the adult hip a technique with full access to the femoral head and acetabulum without the risk of avascular necrosis. J Bone Joint Surg Br. 2001;83:1119–1124. doi: 10.1302/0301-620x.83b8.11964. [DOI] [PubMed] [Google Scholar]
- 9.Horas U, Pelinkovic D, Herr G, Aigner T, Schnettler R. Autologous chondrocyte implantation and osteochondral cylinder transplantation in cartilage repair of the knee joint. A prospective, comparative trial. J Bone Joint Surg Am. 2003;85-A:185–192. doi: 10.2106/00004623-200302000-00001. [DOI] [PubMed] [Google Scholar]
- 10.Smith GD, Richardson JB, Brittberg M, Erggelet C, Verdonk R, Knutsen G, et al. Autologous chondrocyte implantation and osteochondral cylinder transplantation in cartilage repair of the knee joint. J Bone Joint Surg Am. 2003;85-A:2487–2488. doi: 10.2106/00004623-200312000-00044. [DOI] [PubMed] [Google Scholar]
- 11.Nam D, Shindle MK, Buly RL, Kelly BT, Lorich DG. Traumatic osteochondral injury of the femoral head treated by mosaicplasty: a report of two cases. HSS J. 2010;6:228–234. doi: 10.1007/s11420-010-9159-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hart R, Janecek M, Visna P, Bucek P, Kocis J. Mosaicplasty for the treatment of femoral head defect after incorrect resorbable screw insertion. Arthroscopy. 2003;19:E1–E5. doi: 10.1016/j.arthro.2003.10.025. [DOI] [PubMed] [Google Scholar]
- 13.Sugioka Y. Transtrochanteric anterior rotational osteotomy of the femoral head in the treatment of osteonecrosis affecting the hip: a new osteotomy operation. Clin Orthop Relat Res. 1978:191–201. [PubMed] [Google Scholar]
- 14.Gagala J, Tarczyńska M, Gawęda K. Clinical and radiological outcomes of treatment of avascular necrosis of the femoral head using autologous osteochondral transfer (mosaicplasty): preliminary report. Int Orthop. 2013;37:1239–1244. doi: 10.1007/s00264-013-1893-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hangody L, Kish G, Kárpáti Z, Udvarhelyi I, Szigeti I, Bély M. Mosaicplasty for the treatment of articular cartilage defects: application in clinical practice. Orthopedics. 1998;21:751–756. doi: 10.3928/0147-7447-19980701-04. [DOI] [PubMed] [Google Scholar]