Abstract
The literature contains research regarding how trust is formed in healthcare settings but rarely discusses trust formation in an emergent care population. A literature review was conducted to determine which of the trust determinants are important for this process as well as how to develop a scale to measure trust. A search generated a total of 155 articles, 65 of which met eligibility criteria. Determinants that were important included the following: honesty, confidentiality, dependability, communication, competency, fiduciary responsibility, fidelity, and agency. The process of developing a scale includes the following: a literature review, qualitative analysis, piloting, and survey validation. Results suggest that physician behaviors are important in influencing trust in patients and should be included in scales measuring trust. Next steps consist of interviewing emergent care patients to commence the process of developing a scale.
Keywords: Trust, healthcare, scale development, emergent care, literature review
Introduction
Trust is defined as “an expectation that the other person will behave in a way that is beneficial, or at least not harmful, and allows for risks to be taken based on this expectation.”1 In an emergency department (ED), trust is defined as “the patient’s confidence that the physician and the emergency department staff will do what is in the patients’ best interests.”2 There are four elements that comprise trust: (1) it develops from past experiences and prior interactions; (2) the partner is regarded as reliable, dependable, and concerned with providing expected rewards; (3) it involves putting oneself at risk, through disclosure of information, reliance on another, or sacrificing the present in order to see benefits later; and (4) it requires having confidence and security in the caring responses of the partner and the strength of the relationship.3
Trust is associated with improved patient outcomes when examining medical populations. Patients who hold more favorable attitudes toward their physicians are more likely to use services on a regular basis,4,5 and there is more continuity of care, delivery of preventive care, adherence, and satisfaction.6–13 Furthermore, the existence of trust in the patient–physician relationship creates an overall positive psychological impact, which may decrease anxiety, increase feelings of well-being, and promote recovery from illness.14,15 Conversely, lower levels of trust are associated with lower rates of preventive services,13,16,17 lower adherence to physician recommendations,6,18–20 and an increased likelihood of switching physicians.21
Trust literature in healthcare has predominately studied patients in a primary-care setting; however, a few studies have measured trust in additional medical populations. Hupcey22 determined trust to be an important aspect in developing the nurse–family relationship in the intensive care unit and found it served as a fundamental part of the strategies that increased this relationship. For parents of hospitalized children, Price23 found trust was an important part of the process in establishing positive relationships with nurses. Thorne and Robinson24 interviewed patients with chronic illnesses and found reciprocal trust to be an important foundation in the patient–provider relationship. Cancer patients reported high levels of trust in the Hillen et al.25 study, presumably because of the serious implications of the diagnosis. Cancer patients in this study25 reported an even higher level of trust compared to trust reported in primary-care patients.10,19,26,27 Since vulnerability is an important aspect in the development of the physician–patient relationship,28–30 it seems intuitive that complex life-threatening illnesses increase physician dependency and trust levels.
To date, there are no scales in existence measuring immediate patient trust in an emergent care population. Given the emergent care population is unique compared to the medical care population (e.g. patients do not know the physician prior to entering into the ED, they did not choose their physician, and follow-up occurs with a different physician), understanding how trust forms can help physicians better serve their patients may lead to increased treatment adherence and improved outcomes. The purpose of this review seeks an understanding of how to develop a trust scale in order to measure the level of trust emergent care patients have in their emergent care providers. By reviewing trust determinants from other healthcare settings, this can help inform the initial steps needed to create a scale in an emergent care population. Specific questions included the following:
What are the determinants of trust in healthcare populations?
Which of the identified determinants are most important?
What methodological steps need to be taken in order to develop and implement a scale?
The information garnered from this review will help instruct the methodological process of scale development lacking in this patient population. The results will ultimately lead to an increase in knowledge regarding what factors make an emergent care population unique and how to better serve this population while increasing their trust.
Methods
A general and methodological review using PubMed® and Google Scholar™ was conducted. The goal of the general review was to identify determinants of trust and determine what aspects of trust are important. Determinants were deemed important if they were discussed in at least four separate articles. To identify the determinants of trust, global indicators that encompass trust formation were chosen. The goal of the methodological review was to identify a process in order to develop and implement a scale measuring trust in an emergent care population. To understand methodology, articles discussing the steps taken to develop a scale were located.
The following search teams were used for the general review: (“trust” AND “healthcare”) and (“trust” AND “physicians”). The following search terms were used for the methodological review: (“trust” AND “measure” AND “scale”), (“development of a scale”), and (“development of a scale to measure trust in physicians”). Further articles were found by searching citations. The search included articles from 1973 to July 2014. Only articles written in English were included.
Titles and abstracts were screened for inclusion and exclusion criteria. For the general review, articles were selected if they discussed determinants of trust, types of trust, outcomes, and/or predictors in healthcare. For the methodological review, articles were selected if they discussed the development of a scale, re-validated an existing scale, or shortened an existing scale. All scales measured trust, mistrust, or distrust in physicians and healthcare. Articles were excluded if they discussed trust conceptually and did not mention a methodological approach for scale development.
Methodological analysis included scanning qualitative and quantitative information from the articles. Data selected included the following: author information, year of publication, study population, creation of scale items, number of initial questions, pilot, survey administration, scoring, measures of reliability/validity, and the final number of scale items. To minimize risk of bias, 23 articles that did not discuss trust were reviewed for methodological comparison. This showed a similar process to scale development in a healthcare setting, indicating methodology is comparable across domains.
Results
General review: determinants of trust
The search generated a total of 65 articles in PubMed® and Google Scholar™, including instrument development. Although all articles were reviewed to understand trust determinants, 32 (49%) discussed trust in the healthcare field. Out of the 32 articles, 12 (37%) broadly discussed determinants of trust. These determinants included the following: honesty, confidentiality, dependability, communication, competency, fiduciary responsibility, fidelity, agency, respect, caring, privacy, and global. Determinants that are discussed most frequently can be found in Table 1.
Table 1.
Determinants of trust.
| Author (year) | Honesty | Confidentiality | Dependability | Communication | Competency | Fiduciary responsibility | Fidelity | Agency |
|---|---|---|---|---|---|---|---|---|
| Armstrong et al. (2008) | X | X | X | X | X | X | ||
| Hall et al. (2001) | X | X | X | X | X | |||
| Katapodi et al. (2010) | X | |||||||
| Mechanic et al. (2000) | X | X | X | X | X | |||
| Ozawa et al. (2013) | X | X | X | X | X | |||
| Thom et al. (1997) | X | X | ||||||
| Thom and The Stanford Trust Study Physicians (2001) | X | |||||||
| Lynn-McHale et al. (2001) | X | X | X | |||||
| Mechanic et al. (1996) | X | X | X | X | X | |||
| Thom et al. (2002) | X | X | X | X | ||||
| Thom et al. (2004) | X | X | X | X | X | X | ||
| Pearson et al. (2000) | X | X | X | X |
Patient trust has been examined predominately in outpatient settings via physicians, medical care/healthcare, insurer/method of payment, and healthcare staff (Table 2). The purpose of studying trust varied within the articles. Researcher aims included the following: how trust was related to or differed by demographic variables, how health outcomes and behaviors differed when patients had trust, examining factors that increased or predicted trust, examining high versus low trust, developing a concept analysis of trust, and meta-analyses or reviews of the trust literature (Table 3).
Table 2.
How trust was examined.
| Author (year) | Physicians | Medical care/healthcare | Insurer/method of payment | Healthcare staff |
|---|---|---|---|---|
| Altice et al. (2001) | X | X | ||
| Armstrong et al. (2008) | X | |||
| Balkrishnan et al. (2003) | X | X | X | |
| Benin et al. (2006) | X | |||
| Berrios-Rivera et al. (2006) | X | |||
| Boulware et al. (2003) | X | X | X | |
| Caterinicchio (1979) | X | |||
| Halbert et al. (2006) | X | |||
| Hall et al. (1988) | X | |||
| Hall et al. (2001) | X | X | ||
| Kao et al. (1998) | X | |||
| Kao et al. (1998) | X | |||
| Katapodi et al. (2010) | X | |||
| Keating et al. (2002) | X | |||
| LaVeist et al. (2000) | X | |||
| Lynn-McHale (2000) | X | |||
| Mechanic et al. (1996) | X | X | ||
| Mechanic et al. (2000) | X | |||
| O’Malley et al. (2004) | X | |||
| Ozawa et al. (2011) | X | |||
| Ozawa et al. (2013) | X | |||
| Pearson et al. (2001) | X | |||
| Piette et al. (2005) | X | |||
| Russell (2005) | X | |||
| Thom et al. (1997) | X | |||
| Thom and The Stanford Trust Study Physician (2001) | X | |||
| Thom et al. (2002) | X | |||
| Thom et al. (2004) | X | |||
| Thorne et al. (1988) | X | |||
| Whetten et al. (2006) | X | |||
| Wiltshire et al. (2011) | X |
Table 3.
Researcher aims in understanding trust.
| Author (year) | Demographics | Health outcomes and behaviors | Factors that increase or predict trust | High versus low trust | Concept analysis | Meta analysis/review |
|---|---|---|---|---|---|---|
| Altice et al. (2001) | X | |||||
| Armstrong et al. (2008) | X | |||||
| Balkrishnan et al. (2003) | X | |||||
| Benin et al. (2006) | X | |||||
| Berrios-Rivera et al. (2006) | X | X | ||||
| Boulware et al. (2003) | X | |||||
| Halbert et al. (2006) | X | |||||
| Hall et al. (1988) | X | |||||
| Hall et al. (2001) | X | |||||
| Johns (1996) | X | |||||
| Kao et al. (1998) | X | |||||
| Kao et al. (1998) | X | |||||
| Katapodi et al. (2010) | X | |||||
| Keating et al. (2002) | X | |||||
| LaVeist et al. (2000) | X | |||||
| Lynn-McHale (2000) | X | |||||
| Mechanic et al. (1996) | X | |||||
| Mechanic et al. (2000) | X | |||||
| O’Malley et al. (2004) | X | X | ||||
| Ozawa et al. (2011) | X | |||||
| Ozawa et al. (2013) | X | |||||
| Pearson et al. (2001) | X | |||||
| Piette et al. (2005) | X | |||||
| Russell (2005) | X | |||||
| Thom et al. (1997) | X | |||||
| Thom and The Stanford Trust Study Physicians (2001) | X | |||||
| Thom et al. (2002) | X | |||||
| Thom et al. (2004) | X | |||||
| Thorne et al. (1988) | X | |||||
| Whetten et al. (2006) | X | |||||
| Wiltshire et al. (2011) | X |
Methodological review: general characteristics
The search for scale development methodology resulted in a total of 90 articles in PubMed® and Google Scholar™. After eligibility review, 33 articles remained. A total of 27 (81%) of the scales were created after 2000. To create the scale items, most studies followed a pattern of qualitative methods, piloting, surveying, and validation testing. In all, 42% conducted either focus groups or individual interviews, 30% completed a review of the literature, 27% extracted items from other surveys/scales, and 24% re-validated or re-created a scale with another population. Most studies (64%) relied on at least two forms of data collection (e.g. focus groups and a pilot sample). A total of 67% of the studies completed a pilot survey before administering their scale with a larger population. Of those who completed a pilot, 59% surveyed 10–50 respondents, while 41% surveyed 55–290 respondents. Validity and reliability checks were conducted with 94% of the scales created. A comprehensive breakdown of these characteristics can be found in Tables 4 and 5.
Table 4.
Methodological process of scale development.
| Author (year) | Population | Initial scale creation | Number of initial questions | Pilot | Survey administration | Scoring |
|---|---|---|---|---|---|---|
| Anderson and Dedrick (1990) | Regional sample of VA outpatients | Looked at other instruments and interviews with patients and healthcare providers | 25 | None | N = 160 (initial) N = 106 (follow-up) |
5-point Likert scale |
| Bova et al. (2006) | HIV-infected adults | Three focus groups/individual interviews (if preferred) | 58 | N = 10 for instrument pilot N = 99 for instrument development |
None | 5-point Likert scale |
| Bova et al. (2012) | HIV-infected adults | None-revising original scale | 15 | N = 30 | N = 431 | 5-point Likert scale |
| Corbie-Smith et al. (2002) | General population (predominately African American) | Items came from other surveys | 42 | None | N = 909 | N/A |
| Doescher et al. (2009) | General population | Items extracted from another survey | 7 | None | N = 32,929 | 5-point Likert scale |
| Dugan et al. (2005) | General population (National) and insured (HMO sample) | Items came from other scales | 5 | None | N = 1064 (National) N = 1045 (HMO) |
5-point Likert scale; Yes/No |
| Egede and Ellis (2008) | Patients recruited from a primary-care clinic | Nine focus groups and items were pulled from other scales | 70 | N = 257 | N = 301 | 5-point Likert scale |
| Goold et al. (2005) | Members of a managed care plan | Interviews and other studies | 117 | N = 21 | N = 400 | 5-point Likert scale |
| Hall et al. (2002) | National (HMO) and regional (HMO) | Items extracted from other scales and new items were generated from experts in the field | 78 | N = 21 | N = 959 (National) N = 1199 (Regional) |
5-point Likert scale |
| Hall et al. (2002) | General population | Items extracted from other scales and new items were generated from experts in the field | N/A | N = 21 | N = 502 | N/A |
| Hall et al. (2006) | General population (adults with asthma and diabetes) | Sixteen focus groups and previous measures of trust were reviewed | 30 | N = 61 initial N = 63 revised |
N = 3623 | 5-point Likert scale |
| Hillen et al. (2012) | Cancer patients recruited from three departments in an academic hospital | Open-ended interviews | 33 | N = 12 | N = 423 | 5-point Likert scale |
| Jones and Barry (2011) | Health promotion partners in various realms of work | Five focus groups | 14 | None | N = 337 | 5-point Likert scale |
| Kelly et al. (2005) | Patients who received treatment in a regional ED | Literature review and focus groups | 42 | N = 238 initial N = 145 revised |
None | N/A |
| Kressin et al. (2002) | Patients at five VA medical centers who had coronary artery disease | Literature review and focus groups | 63 | None | None | N/A |
| LaVeist et al. (2009) | Regional sample of adults | Re-validated the Medical Mistrust Index (MMI) | 17 | None | N = 401 (initial) N = 327 (follow-up) |
4-point Likert scale |
| Leisen and Hyman (2001) | Regional sample of employees of a service organization | Based on other scales and physician suggestion | 51 | N = 40 | N = 241 | 7-point Likert scale |
| Mainous et al. (2006) | Regional sample of adults | Developed a conceptual model from the literature to create items | 29 | N = 25 | N = 496 | 5-point Likert scale |
| Moseley et al. (2005) | Regional sample of parents of pediatric patients | Modified the TiPS to apply to pediatric patients | 11 | None | N = 526(initial) N = 485 (final) |
5-point Likert scale |
| Radwin et al. (2005) | Regional sample of recently-hospitalized cancer patients | Literature review and a qualitative pilot | 18 | N = 66 | N = 66 | 6-point Likert scale |
| Radwin and Cabral (2010) | Regional sample of recently-hospitalized cancer patients | Assessing the Trust in Nurses Scale’s validity | 5 | None | N = 187 | 6-point Likert scale |
| Rose et al. (2004) | Regional sample of prospective jurors | Four focus groups and review of the literature | 15 | N = 55 | N = 400 | 5-point Likert scale |
| Safran et al. (1998) | Regional sample of Massachusetts state employees | Checking the validity and reliability of the Primary Care Assessment Survey (PCAS) | 51 | None | N = 6094 | 0–100 points |
| Shea et al. (2008) | Regional sample of adults who saw a PCP or ED within the last 3 years | 12 focus groups | 75 | N = 34 | N = 264 | 5-point Likert scale |
| Shelton et al. (2010) | Regional sample of African American males | Validated the Group-Based Medical Mistrust Scale (GBMMS) on a different sample | 12 | None | N = 201 | 5-point Likert scale |
| Stiggelbout et al. (2004) | A regional sample of aneurysm patients and a regional sample of surgeons and surgical residents | Used six moral concepts of patient autonomy from the literature | 55 | N/A Tested three groups |
N = 96 (patients) N = 58 (surgeons and residents) |
5-point Likert scale |
| Thom et al. (1999) | General population from community-based primary-care practices | Assessing the validity and reliability of the TiPS | 11 | None | N = 414 | 5-point Likert scale |
| Thom et al. (2011) | Clinicians, whose patients were participating in a pain study | Used prior focus groups data to identify items | 18 | N = 14 | N = 61 | 5-point Likert scale |
| Thompson et al. (2004) | Regional sample of adults (African American and Latina) | Items came from the literature and other scales | 12 | None | N = 168 | 5-point Likert scale |
| Wallston et al. (1973) | Regional samples of nurse’s at a VA | Interviews with nurses | 34 | N = 46 (senior nurses) N = 19 (graduate nursing students) |
N = 55 | 7-point Likert scale |
| Wallston and Wallston (1978) | Sample of adults waiting at an airport | Using the Health Locus of Control (HLC) scale to create the Multidimensional Health Locus of Control (MHLC) scale | 81 | None | N = 115 | 6-point Likert scale |
| Wolf et al. (1978) | Regional sample of patients at student-health and adult clinics | Interviews with patients, observations of consultations, and review of the literature | 63 | N = 50 | N = 100 (second field trial) N = 50 (third field trial) |
5-point Likert scale |
| Zheng et al. (2002) | General population (National) and regional sample (HMO) | Focus groups and items were extracted from other scales | 37 | N = 290 | N = 410 (National) N = 1152 (Regional) |
5-point Likert scale |
VA: Veterans Affairs; HMO: health maintenance organization; ED: emergency department; TiPS: Trust in Physician Scale PCP: primary care physician.
Table 5.
Validity and reliability of scale items.
| Author (year) | Validity | Reliability | Final number of items |
|---|---|---|---|
| Anderson and Dedrick (1990) | Construct (with other scales) | Cronbach’s α = .85 | 11 |
| Bova et al. (2006) | Concurrent (correlation with other scales) | Cronbach’s α = .92/.95 | 15 |
| Bova et al. (2012) | Criterion (with other scales) | Cronbach’s α = .96 | 13 |
| Construct (factor analysis) | |||
| Corbie-Smith et al. (2002) | Face validity (picked items based on validity) | N/A | 12 |
| Doescher, et al. (2009) | Convergent (correlation between scales) | Cronbach’s α = .62 | 7 |
| Dugan et al. (2005) | Construct (correlation) Concurrent (2-sample t-test) |
Cronbach’s α = .87 (National) .86 (Regional) |
5 |
| Egede and Ellis (2008) | Convergent (correlation with other scales) | Cronbach’s α = .64–.92 | 17 |
| Goold et al. (2005) | Construct (correlation with other scales) | Cronbach’s α = .95 (long version) .91 (short version) |
13 (long version) 9 (short version) |
| Hall et al. (2002) | Construct (correlation with other scales) | Cronbach’s α = .94 | 10 |
| Hall et al. (2002) | Construct (correlation with other scales) | Cronbach’s α = .89 | 11 |
| Concurrent (correlation) | |||
| Hall et al. (2006) | N/A | Cronbach’s α = .72 | 4 |
| Hillen et al. (2012) | Construct (correlation with other scales) | Cronbach’s α = .92 | 18 |
| Jones and Barry (2011) | Face (percent of who completed survey) | Cronbach’s α = .91 | 14 |
| Content (qualitative data checked) | |||
| Convergent/discriminant (correlation with other scales) | |||
| Kelly et al. (2005) | Construct (literature review, focus groups, and phone interviews) | Cronbach’s α = .88 | 18 |
| Kressin et al. (2002) | Construct (multitrait analysis) | Cronbach’s α = .72–.89 | 34 |
| LaVeist et al. (2009) | Construct (correlation with other scales) | Cronbach’s α = .76 | 7 |
| Leisen and Hyman (2001) | Content (literature review) Convergent (t-values of factor loadings) |
Cronbach’s α = .95/.89 | 51 |
| Discriminant (three antecedents were evaluated) | |||
| Criterion (correlation) | |||
| Mainous et al. (2006) | Concurrent (correlation) | Cronbach’s α = .84 | 12 |
| Moseley et al. (2005) | N/A | Cronbach’s α = .84 | 11 |
| Radwin et al. (2005) | Convergent (correlation) | Cronbach’s α = .71–.81 | 16 |
| Discriminant (standard error for correlation sets) | |||
| Radwin and Cabral (2010) | Convergent (correlation) Discriminant (standard error for correlation sets) |
Cronbach’s α = .77 | 4 |
| Construct (confirmatory factor analysis) | |||
| Rose et al. (2004) | Concurrent (correlation with other scales) | Cronbach’s α = .75 | 10 |
| Safran et al. (1998) | Convergent (correlation) | Cronbach’s α = .81–.95 | 51 |
| Discriminant (correlation with other scales) | |||
| Shea et al. (2008) | Construct (correlations with other scales) | Cronbach’s α = .73/.77 | 9 |
| Shelton et al. (2010) | Construct (correlation with other scales) | Cronbach’s α = .87 | 12 |
| Stiggelbout et al. (2004) | Construct (correlation with other scales) | Cronbach’s α = .62–.83 | 14 |
| Thom et al. (1999) | Construct (correlations) | Cronbach’s α = .89 | 11 |
| Predictive (looking at predictions of trust with other variables) | |||
| Thom et al. (2011) | Convergent (correlation) | Cronbach’s α = .93 | 12 |
| Discriminant (correlation) | |||
| Thompson et al. (2004) | Construct (regression) | Cronbach’s α = .83 | 12 |
| Convergent (correlation) | |||
| Wallston et al. (1973) | Concurrent (correlation with other scales) | N/A | 10 |
| Wallston and Wallston (1978) | Construct (correlation with other scales) Predictive (correlation with other scales) |
Cronbach’s α = .50–85 | 18 |
| Wolf et al. (1978) | Face and content validity (interviews with participants) Construct (correlations with other subscales) |
Cronbach’s α = .93 | 26 |
| Zheng et al. (2002) | Construct (correlation with other scales) | Cronbach’s α = .92 (National) .89 (Regional) |
11 |
Discussion
The purpose of this review was as follows: (1) to understand trust determinants, (2) which are the most important determinants, and (3) to determine what methodological steps need to be taken in order to develop a trust scale in an emergent care population. Based on the review, the determinants of trust that are central in understanding how trust is formed and maintained include the following: honesty (e.g. telling the truth), confidentiality (e.g. protecting private information), dependability (e.g. looking out for patient interests), communication (e.g. being open and discussing options), competency (e.g. doing what needs to be done; avoiding errors), and fiduciary responsibility, fidelity, and agency (e.g. physician responsibility to do what is best for the patient; not taking advantage of patient vulnerability). These determinants were discovered by surveying,11,15,21,31,32 communities,33 conducting a review,28,34–37 and conducting a concept analysis.38
Since trust in physicians is most frequently examined, most of the determinants come from specific physician behaviors. These behaviors can often predict the patients’ trust level (low or high). As a result, a physician’s behavior, specifically related to their communication style and interpersonal skills, is associated with the development of trust.6,10,19,26,39,40 By treating a patient with respect and dignity, as well as being warm and receptive, physicians can intentionally increase their patients trust. This is important, as most studies examine trust from the patients’ perspective only, not acknowledging how reciprocal interactions between the physician and patient can affect patient trust.24,41 In addition to physician behaviors, there is evidence that the length of social relationships with physicians is significant, with longer relationships leading to higher levels of trust.6,10,19,26,42–45 Finally, patient choice in selecting their physician (e.g. personal choice vs recommendation vs convenience) is another predictor of trust.6,10,19,26,45 Studies have found that individuals are more likely to trust their physician when they have a choice as opposed to being required to see a specific provider. Researchers have measured demographic factors such as age, race, gender, education, income, and health status,10,19,27,46–48 although these factors have not been found to be highly predictable of trust.
Although demographic factors have not been consistently found to predict trust, it is important to note there are documented differences in individuals’ health outcomes by race. People of color, specifically African Americans, report lower levels of trust in their physicians and in medical settings.13,16,46,49,50 This lower level of trust is related to interferences in seeking medical care and adherence to medical recommendations.13,16,46,49,50 As a result of diminished care seeking, people of color are more likely to rely on EDs as their source of primary care.46 The literature has conceptualized this lack of trust as distrust,28,51 which can be described as a distinctly separate entity51 void of trust28 as well as mistrust,16 described as consistently distrusting medical institutions and persons who represent the dominant culture.16 Mistrust, as a predictor, is associated with delaying care seeking, nonadherence, and failure to keep appointments.52
Although the trust literature includes information regarding how trust is formed in primary-care and outpatient settings, a gap exists in an emergent care population. One can argue that many determinants, such as communication and competency, are important regardless of setting. Given the fact that patients do not choose their physician, do not have the time necessary to establish rapport, and are in a vulnerable state upon admission, it is essential to understand what the significant behaviors and factors that increase trust formation in an emergent care population. Understanding trust formation will allow healthcare providers to provide better care and can lead to better patient outcomes.
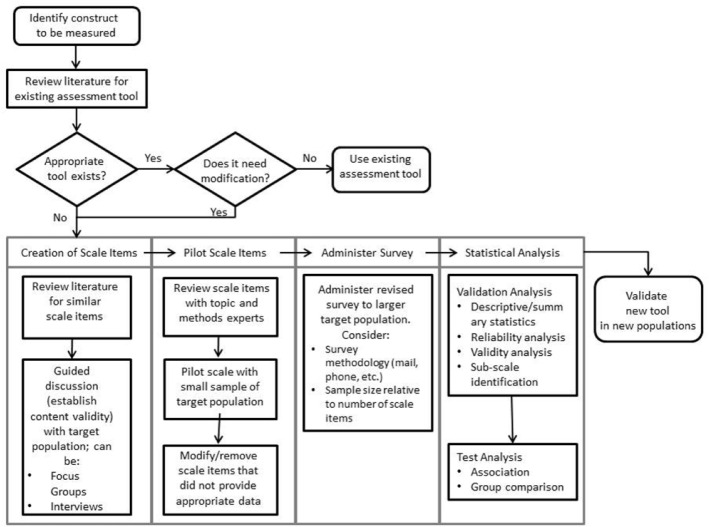
Based on the methodological literature, specific steps are needed in order to develop a scale (Figure 1). These include the following: (1) conducting a review of the literature regarding the population of interest, (2) interviewing individuals in that population in order to understand the common themes, (3) creating an initial survey based on the themes, (4) piloting to a small group (10–30) of individuals, and finally (5) surveying to a large group (350–400) in to order to generate a final number of items and as well as establish validity. See Figure 1 for a more in-depth, step-by-step guide to scale development. Readers should note that not all studies reviewed here engaged in each step. Figure 1 presents an ideal and recommended set of steps, which allows the researcher to establish validity early and arrive at complete conclusion. Often, how researchers choose to proceed with the data collection process is contingent on time and funds and may not follow the same recommended protocol.
Figure 1.
Methodological process for developing a scale.
Limitations
This study is not without limitations. One limitation is reviewing English-only articles; this might have limited our ability to understand how trust is developed and measured in non-English-speaking cultures. The search was also limited to articles in PubMed® and Google Scholar™ as opposed to psychometrically based articles, such as PsycINFO®. This was purposeful, in order to keep a healthcare focus and use resources that were publicly available.
Next steps
In the first step toward the development of a psychometrically sound and valid scale to measure trust formation in an emergent care population, patient interviews with trauma and/or ED patients will be conducted at a large, tertiary level I trauma center in the Midwest. These interviews will help to understand what aspects of trust are important to emergent care patients, building the constructs and meaning of trust for this population. Questions will be based on the determinants from the literature. These include questions regarding provider communication, dependability, honesty, and fidelity/agency. In addition to providers, patient trust regarding the institution will also be gauged, to see how the hospital itself impacts patient trust. Finally, differential treatment based on demographics will be asked in order to see whether demographic differences affect care.
Once interviews are complete, qualitative analysis of the responses will begin. This analysis will include reading over statements made by the participants, to determine what aspects of the provider and hospital increase or decrease trust in an emergent care population. We can then compare these data with the extant literature in order to understand what distinguishes an emergent care population from an outpatient population and begin the third phase of scale development.
Emergent care patients enter into the physician–patient relationship vulnerable and unable to make decisions regarding initial care or choice of physician. This vulnerable state may be similar to Hillen et al.’s25 study of the cancer patient population, in that the seriousness of emergent care might lend to higher levels of trust. Understanding how trust is formed not only will help physicians comprehend trust formation and modify professional behavior to improve patient relations but also will lead to better treatment adherence and improved patient outcomes.
Acknowledgments
The authors would like to thank Dr Felecia Lee, PhD, and Ashley Hervey, Med, for their contributions to this project.
Footnotes
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Thom DH, Wong ST, Guzman D, et al. Physician trust in the patient: development and validation of a new measure. Ann Fam Med 2011; 9(2): 148–154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Kelly JJ, Njuki F, Lane PL, et al. Design of a questionnaire to measure trust in an emergency department. Acad Emerg Med 2005; 12(2): 147–151. [DOI] [PubMed] [Google Scholar]
- 3. Rempel JK, Holmes JG, Zanna MP. Trust in close relationships. J Pers Soc Psychol 1985; 49(1): 95–112. [PubMed] [Google Scholar]
- 4. Andersen R, Newman JF. Societal and individual determinants of medical care utilization in the United States. Milbank Mem Fund Q Health Soc 1973; 51(1): 95–102. [PubMed] [Google Scholar]
- 5. Russell S. Treatment-seeking behavior in urban Sri Lanka: trusting the state, trusting private providers. Soc Sci Med 2005; 61(7): 1396–1407. [DOI] [PubMed] [Google Scholar]
- 6. Safran DG, Kosinski M, Tarlov AR, et al. The Primary Care Assessment Survey: tests of data quality and measurement performance. Med Care 1998; 36(5): 728–739. [DOI] [PubMed] [Google Scholar]
- 7. Matthews AK, Sellergren SA, Manfredi C, et al. Factors influencing medical information seeking among African American cancer patients. J Health Commun 2002; 7(3): 205–219. [DOI] [PubMed] [Google Scholar]
- 8. Keating NL, Green DC, Kao AC, et al. How are patients’ specific ambulatory care experiences related to trust, satisfaction, and considering changing physicians? J Gen Intern Med 2002; 17(1): 29–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Doescher MP, Saver BG, Franks P, et al. Racial and ethnic disparities in perceptions of physician style and trust. Arch Fam Med 2000; 9(10): 1156–1163. [DOI] [PubMed] [Google Scholar]
- 10. Kao AC, Green DC, Davis NA, et al. Patients’ trust in their physicians: effects of choice, continuity, and payment method. J Gen Intern Med 1998; 13(10): 681–686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Thom DH, Kravitz RL, Bell RA, et al. Patient trust in the physician: relationship to patient requests. Fam Pract 2002; 19(5): 476–483. [DOI] [PubMed] [Google Scholar]
- 12. Mainous AG, III, Baker R, Love MM, et al. Continuity of care and trust in one’s physician: evidence from primary care in the United States and United Kingdom. Fam Med 2001; 33(1): 22–27. [PubMed] [Google Scholar]
- 13. O’Malley AS, Sheppard VB, Schwartz M, et al. The role of trust in use of preventative services among low-income African American women. Prev Med 2004; 38(6): 777–785. [DOI] [PubMed] [Google Scholar]
- 14. Egbert LD, Battit GE, Welch CE, et al. Reduction of post-operative pain by encouragement and instruction of patients. N Engl J Med 1964; 270(16): 825–827. [DOI] [PubMed] [Google Scholar]
- 15. Thom DH, Campbell B. Patient-physician trust: an exploratory study. J Fam Pract 1997; 44(2): 169–176. [PubMed] [Google Scholar]
- 16. Thompson HS, Valdimarsdottir HB, Winkel G, et al. The Group-Based Medical Mistrust Scale: psychometric properties and association with breast cancer screening. Prev Med 2004; 38(2): 209–218. [DOI] [PubMed] [Google Scholar]
- 17. Whetten K, Leserman J, Whetten R, et al. Exploring lack of trust in care providers and the government as a barrier to health service use. Am J Public Health 2006; 96(4): 716–721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Piette JD, Heisler M, Krein S, et al. The role of patient-physician trust in moderating medication nonadherence due to cost pressures. Arch Intern Med 2005; 165(15): 1749–1755. [DOI] [PubMed] [Google Scholar]
- 19. Thom DH, Ribisl KM, Stewart AL, et al. Further validation and reliability testing of the Trust in Physician Scale. The Stanford Trust Study Physicians. Med Care 1999; 37(5): 510–517. [DOI] [PubMed] [Google Scholar]
- 20. Benin AL, Wisler-Scher DJ, Colson E, et al. Qualitative analysis of mothers’ decision-making about vaccines for infants: the importance of trust. Pediatr 2006; 117(5): 1532–1541. [DOI] [PubMed] [Google Scholar]
- 21. Armstrong K, McMurphy S, Dean LT, et al. Differences in the patterns of health care system distrust between blacks and whites. J Gen Intern Med 2008; 23(6): 827–833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Hupcey JE. Establishing the burse-family relationship in the intensive care unit. West J Nurs Res 1998; 20(2): 180–194. [DOI] [PubMed] [Google Scholar]
- 23. Price PJ. Parents’ perceptions of the meaning of quality nursing care. Adv Nurs Sci 1993; 16(1): 33–41. [DOI] [PubMed] [Google Scholar]
- 24. Thorne SE, Robinson CA. Reciprocal trust in health care relationships. J Adv Nurs 1988; 13(6): 782–789. [DOI] [PubMed] [Google Scholar]
- 25. Hillen MA, Koning CCE, Wilmink JW, et al. Assessing cancer patients’ trust in their oncologist: development and validation of the Trust in Oncologist Scale (TiOS). Support Care Cancer 2012; 20(8): 1787–1795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Hall MA, Zheng B, Dugan E, et al. Measuring patients’ trust in their primary care providers. Med Care Res Rev 2002; 59(3): 293–318. [DOI] [PubMed] [Google Scholar]
- 27. Anderson LA, Dedrick RF. Development of the Trust in Physician Scale: a measure to assess interpersonal trust in patient-physician relationships. Psychol Rep 1990; 67(3 Pt 2): 1091–1100. [DOI] [PubMed] [Google Scholar]
- 28. Hall MA, Dugan E, Zheng B, et al. Trust in physicians and medical institutions: what is it, can it be measured, and does it matter? Milbank Q 2001; 79(4): 613–639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Johns JL. A concept analysis of trust. J Adv Nurs 1996; 24(1): 76–83. [DOI] [PubMed] [Google Scholar]
- 30. Dugan E, Trachtenberg F, Hall MA. Development of abbreviated measures to assess patient trust in a physician, a health insurer, and the medical profession. BMC Health Serv Res 2005; 5(1): 64–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Mechanic D, Meyer S. Concepts of trust among patients with serious illness. Soc Sci Med 2000; 51(5): 657–668. [DOI] [PubMed] [Google Scholar]
- 32. Thom DH. The Stanford Trust Study Physicians. Physician behaviors that predict patient trust. J Fam Pract 2001; 50(4): 323–328. [PubMed] [Google Scholar]
- 33. Katapodi MC, Pierce PF, Facione NC. Distrust, predisposition to use health services and breast cancer screening: results from a multicultural community-based survey. Int J Nurs Stud 2010; 47(8): 975–983. [DOI] [PubMed] [Google Scholar]
- 34. Ozawa S, Sripad P. How do you measure trust in the health system? A systematic review of the literature. Soc Sci Med 2013; 91: 10–14. [DOI] [PubMed] [Google Scholar]
- 35. Mechanic D, Schlesinger M. The impact of managed cared on patients’ trust in medical care and their physicians. JAMA 1996; 275(21): 1693–1697. [PubMed] [Google Scholar]
- 36. Thom DH, Hall MA, Pawlson G. Measuring patients’ trust in physicians when assessing quality of care. Health Aff 2004; 23(4): 124–132. [DOI] [PubMed] [Google Scholar]
- 37. Pearson SD, Raeke LH. Patients’ trust in physicians: many theories, few measures, and little data. J Gen Intern Med 2000; 15(7): 509–513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Lynn-McHale DJ, Deatrick JA. Trust between family and health care provider. J Fam Nurs 2000; 6(3): 210–230. [Google Scholar]
- 39. Cook KS. Trust in society. New York, NY: Russell Sage, 2001. [Google Scholar]
- 40. Roberts CA, Aruguete MS. Task and socioeconomic behaviors of physicians: a test of reciprocity and social interaction theories in analogue physician-patient encounters. Soc Sci Med 2000; 50(3): 309–315. [DOI] [PubMed] [Google Scholar]
- 41. Cook K, Kramer R, Thom D, et al. Trust and distrust in patient-physician relationships: perceived determinants of high and low trust relationships in managed care settings. In: Kramer R, Cook KS. (eds) Trust and distrust in organizations: dilemmas and approaches. Thousand Oaks, CA: Russell Sage, 2004, pp. 65–98. [Google Scholar]
- 42. Barber B. The logic and limits of trust. New Brunswick, NJ: Rutgers University Press, 1983. [Google Scholar]
- 43. Gambetta D. Trust: making and breaking cooperative relations. Cambridge, MA: Basil Blackwell, 1988. [Google Scholar]
- 44. Kramer RM, Tyler TR. Trust in organizations: frontiers of theory and research. Thousand Oaks, CA: SAGE, 1996. [Google Scholar]
- 45. Wholey DR, Sommers AR. The effect of preferences, choices, markets, and managed care on satisfaction with choice and trust. Working paper, 2001.
- 46. LaVeist TA, Nickerson KJ, Bowie JV. Attitudes about racism, medical mistrust, and satisfaction with care among African American and white cardiac patients. Med Care Res Rev 2000; 57(Suppl. 4): 146–161. [DOI] [PubMed] [Google Scholar]
- 47. Meit SS, Williams D, Mencken FC, et al. Gowning: effects on patient satisfaction. J Fam Pract 1997; 45(5): 397–401. [PubMed] [Google Scholar]
- 48. Pescosolido BA, Tuch ST, Martin JK. The profession of medicine and the public: examining Americans’ changing confidence in physician authority from the beginning of the “Health Care Crisis” to the era of health care reform. J Health Soc Behav 2001; 42(1): 1–16. [PubMed] [Google Scholar]
- 49. Halbert CH, Armstrong K, Gandy OH, Jr, et al. Racial differences in trust in health care providers. Arch Intern Med 2006; 166(8): 896–901. [DOI] [PubMed] [Google Scholar]
- 50. Boulware LE, Cooper LA, Ratner LE, et al. Race and trust in the health care system. Public Health Rep 2003; 118(4): 358–365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Benamati JS, Serva MA, Fuller MA. Are trust and distrust distinct constructs? An empirical study of the effects of trust and distrust among online banking users. In: Proceedings of the 39th Hawaii international conference on science systems, Kauai, HI, 4–7 January 2006, pp. 1–8. New York: ACM. [Google Scholar]
- 52. LaVeist TA, Isaac LA, Williams KP. Mistrust of healthcare organizations associated with underutilization of health services. Health Res Educ Trust 2009; 44(6): 2093–2105. [DOI] [PMC free article] [PubMed] [Google Scholar]