Abstract
Obesity, diet and physical inactivity are risk factors for some cancers. Grantees of the National Comprehensive Cancer Control Program (NCCCP) in US states, tribes, and territories develop plans to coordinate funding and activities for cancer prevention and control. Including information and goals related to nutrition and physical activity (NPA) is a key opportunity for primary cancer prevention, but it is currently unclear to what extent NCCCP plans address these issues. We reviewed 69 NCCCP plans and searched for terms related to NPA. Plans were coded as (1) knowledge of NPA and cancer link; (2) goals to improve NPA behaviors; and (3) strategies to increase healthy NPA activities, environments, or systems changes. NPA content was consistently included in all cancer plans examined across all years. Only 4 (6 %) outlined only the relationship between NPA and cancer without goals or strategies. Fifty-nine plans (89 %) contained goals or strategies related to NPA, with 53 (82 %) including both. However, numbers of goals, strategies, and detail provided varied widely. All programs recognized the importance of NPA in cancer prevention. Most plans included NPA goals and strategies. Increasing the presence of NPA strategies that can be modified or adapted appropriately locally could help with more widespread implementation and measurement of NPA interventions.
Keywords: Comprehensive cancer control, Cancer prevention, Nutrition, Physical activity
Introduction
More than one in three US adults are classified as obese, and rates of obesity have remained steady since 2003 [1, 2]. Obesity has been linked to an increased risk of several cancers and is estimated to contribute to approximately 85,000 new cases of cancer each year [3–9]. Additionally, increased physical activity has been linked to a decreased risk of developing several cancers, including: breast, colorectal, ovarian, and endometrial cancers, and poor diet has been associated with increased risk of certain cancers including colorectal cancer [10–12]. Further, obesity has been linked to poorer survival outcomes in cancer survivors, and increased physical activity has been associated with increased survival [13]. Addressing issues surrounding nutrition and physical activity (NPA) are essential to the primary prevention of cancer as evidenced by recommendations from the American Institute of Cancer Research and the American Cancer Society and nutrition and physical activity guidelines from the US government [14–18].
The Centers for Disease Control and Prevention (CDC) manages the National Comprehensive Cancer Control Program (NCCCP), which funds programs in all 50 US states, the District of Columbia, Puerto Rico, 7 tribes, and 7 Pacific Island Jurisdiction territories to develop cancer plans that design and implement activities in cancer prevention and control [19]. These cancer control plans include information on the region’s cancer burden, as well as goals and potential activities to improve primary cancer prevention, cancer screening, and cancer survivorship in the community. Including information and goals related to NPA in cancer plans is a key opportunity for primary cancer prevention and for improving quality of life and survival among cancer survivors. Yet, the scope, depth, and evidence-basis for current cancer plan activities related to these issues is unknown. The objective of this study was to determine what cancer plans include on NPA information and strategies for reducing cancer risk.
Methods
Cancer plans (N = 69) from all NCCCP funded programs were downloaded from the CDC website (http://www.cdc.gov/cancer/ncccp/ccc_plans.htm). Current cancer plans spanned the years 2004–2014. Cancer plans were reviewed for terms related to NPA recommendations using Adobe Acrobat X (San Jose, CA). Search terms included: nutrition; physical activity; exercise; healthy foods, eating, or weight; obesity; walking; recreation; and physical education. All sections containing search terms were reviewed for content and detail. Cancer plans were coded as (1) knowledge of the NPA and cancer link; (2) goals to improve NPA behaviors; and/or (3) strategies to increase healthy NPA activities, environments, or systems changes. Codes were not mutually exclusive. Goals were defined as a plan to change an outcome by a quantifiable amount, such as “increase the number of adults participating in 150 min of physical activity per week.” Strategies were defined as activities outlined to meet goals for a quantifiable change in NPA behaviors, such as, “Increase the number of salad bars in schools.”
Cancer plans were also assessed for regional and overall awareness of current NPA and obesity status as well as the consistency of strategies with recommendations of The Guide to Community Preventive Services (www.thecommunityguide.org), the Institute of Medicine, CDC, the US Surgeon General and other expert bodies [17, 18, 20–25]. Recommended strategies were classified into the following categories: (1) increased awareness (any strategy designed to increase overall awareness of the NPA-cancer association), (2) community physical activity (any strategy to improve or increase access to areas in the community for physical activity), (3) school wellness (any strategy related to NPA changes in a school setting including physical education), (4) worksite wellness (any strategy related to NPA changes in a workplace setting), (5) increased healthy food access (any strategy related to the ability increase access to purchase healthy foods such as through farmer’s markets, community gardens, or retail stores), (6) increased healthy food availability (any strategy that promoted making healthy food available in settings such as schools and worksites), (7) decreased less healthy food availability (any strategy limiting access to less healthy foods at specific times or locations, such as schools or worksites), (8) community-school agreements (any strategy to increase access for the community to school resources for physical activity), and (9) decreased screen-time (any strategy to decrease television viewing or other screen-time for children). Strategies present in cancer plans were copied into a Microsoft Excel (Redmond, WA) database for analysis. Maps of region-level awareness and numbers of strategies were created with ArcGIS 10 ArcMap software (Redlands, CA).
Cancer survivorship or quality of life sections of cancer plans were also assessed for any mention of NPA in relation to cancer survivors. If NPA was mentioned, sections were reviewed for content and detail.
Action reports, which are a description of activities implemented and are submitted to CDC as part of the standard cooperative agreement reporting requirements for funding were also searched for the terms nutrition, physical activity, and obesity in listed action plan objectives and activities. Action reports were only available from 2013 to 2016, consistent with the most recent funding cycle. Action report objectives and activities were classified using the strategies described above. All results from the action report search were also assessed for content related to cancer survivorship.
Results
Cancer Plans
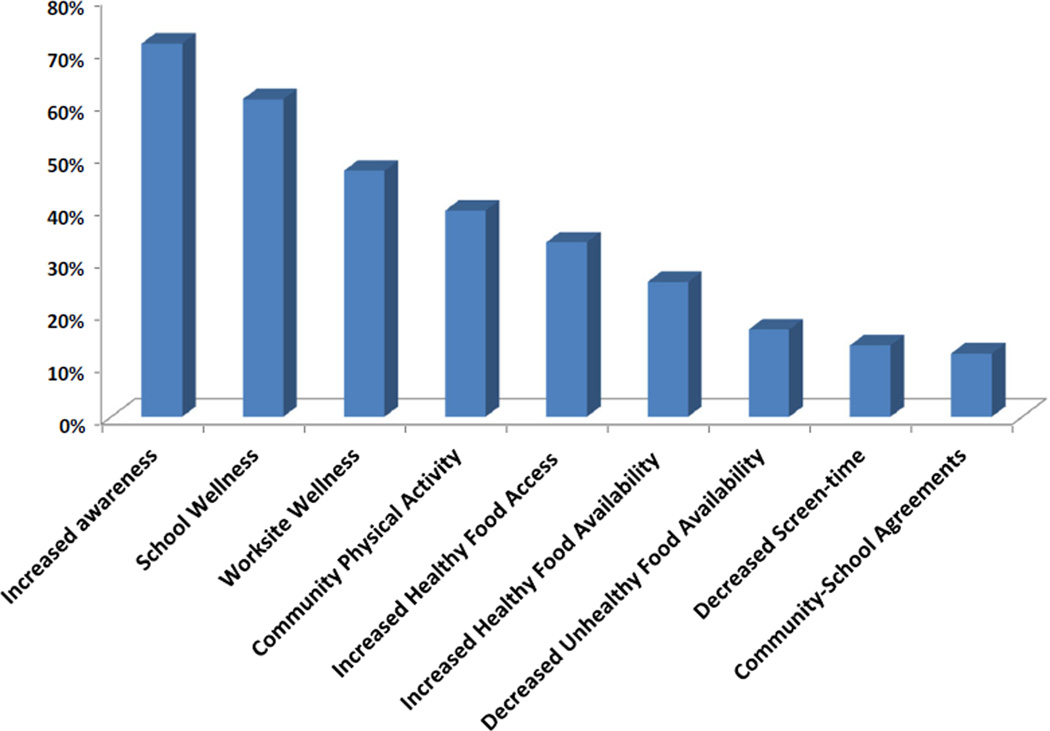
All 69 cancer plans contained the search terms “nutrition,” “physical activity,” or both for all years. Fifty-seven (86 %) included “healthy food/eating” and 51 (77 %) included “walking,” “recreation,” or “physical education” (Table 1). Fifty-nine cancer plans (89 %) were categorized as containing goals to improve healthy NPA behaviors or including strategies to address NPA, with 54 (82 %) including both (data not shown). Only 4 (6 %) included only knowledge of the relationship between NPA and cancer, indicating they acknowledged the importance of NPA in relation to cancer prevention but listed no goals or strategies to address these areas (data not shown). Examples of strategies proposed in cancer plans for each category are listed in Table 2. Seventy-one percent of cancer plans contained at least one strategy consistent with expert recommendations or scientific evidence, with the number of strategies ranging from 0 to 22 (Fig. 1). The most common strategies were to increase awareness of association of NPA with cancer risk (71 %), school wellness-based strategies (61 %), worksite-wellness based strategies (47 %), and community physical activity (39 %) (Fig. 2).
Table 1.
Presence of nutrition and physical activity (NPA) related search terms in cancer plans
| Search term | Number of plans (%) |
|---|---|
| Nutrition | 64 (93 %) |
| Physical activity | 64 (93 %) |
| Obesity | 62 (90 %) |
| Exercise | 43 (62 %) |
| Healthy foods/eating combined | 57 (86 %) |
| Healthy food(s) | 44 (64 %) |
| Healthy eating | 41 (59 %) |
| Healthy weight | 44 (64 %) |
| Walking/recreation/physical education combined | 51 (77 %) |
| Walking | 36 (52 %) |
| Recreation | 29 (42 %) |
| Physical education | 36 (52 %) |
NPA search terms and the percentage of plans containing each search term are listed
Table 2.
Examples of selected strategies in cancer plans
| Strategy | Example |
|---|---|
| Increased awareness | Increase public awareness of the benefits of physical activity through media campaign |
| Community physical activity | Promote building of safe sidewalks and bike paths between community schools and residential areas |
| School wellness | Promote increased time requirement for physical activity during physical education classes in school |
| Worksite wellness | Engage companies to implement evidence based worksite programs to promote physical activity |
| Increased healthy food access (farmer’s markets, gardens, etc.) | Promote policies…that provide opportunities for good nutrition in underserved communities (i.e. farmers’ markets, community gardens) |
| Increased healthy food availability | Promote an increase in schools that support healthy foods on campus by offering fruits or non-fried vegetables in vending machines and school stores, canteens, or snack bars, and during celebrations when foods and beverages are offered |
| Decreased less healthy food availability | Educate and advocate for the removal of soda vending machines from schools and replacing with water and 100 % juice products |
| Community-school agreements | Increase the proportion of schools that provide access to their physical activity…outside of normal school hours |
| Decreased screen-time | Collaborate…to encourage children to decrease time spent with video games and TV and to substitute physical activity |
Strategy categories are listed with examples from cancer plans for each category
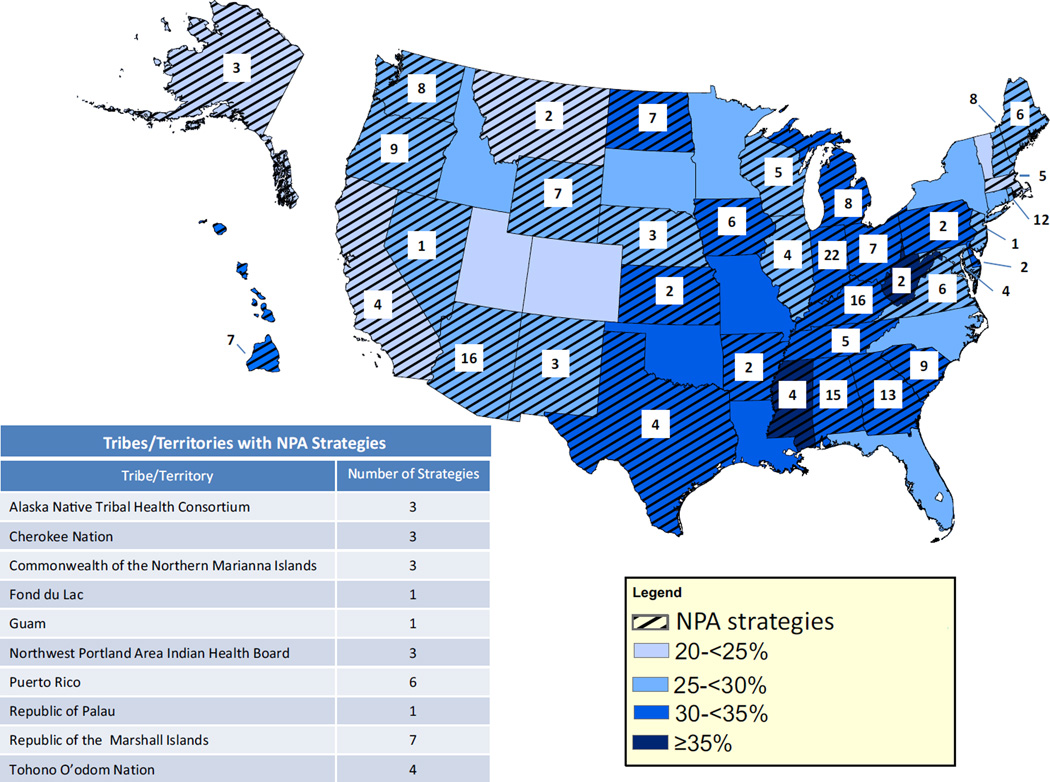
Fig. 1.
NPA strategies and nutrition, physical activity, and obesity data by region [50]. Light to dark blue shading of states corresponds to levels of obesity in states (see Legend). States cross-hatched contained evidenced-based strategies related to NPA changes in their cancer plans. The number of strategies is listed in the box in each state. Tribes and territories with NPA strategies and the number of strategies for each plan are listed in the box below the map (Color figure online)
Fig. 2.
Percentage of strategies in cancer plans. Selected strategies found in cancer plans are listed on the x-axis. Percent of plans with each strategy are listed on the y-axis
Action Reports
A total of 47 (68 %) of action reports contained at least one of the terms “nutrition,” “physical activity,” or “obesity” (data not shown). The most commonly noted strategy included was increasing awareness, which was present in 21 action reports (30 %), followed by school based strategies (13 %), worksite wellness based strategies (12 %), and increasing food access (12 %) (Table 3). In addition, 15 action reports (22 %) mentioned collaborating with groups in the community or task forces to implement NPA strategies for cancer prevention (data not shown).
Table 3.
Strategies in action plans
| Evidence-based strategy | Action plans (%) |
Example |
|---|---|---|
| Increased awareness | 21 (30 %) | Disseminate updated scan and other available resources to educate policy makers and key stakeholders on physical activity and nutrition prevention health policy evidence base |
| Community physical activity | 4 (6 %) | Execute agreements with communities receiving a sub-award to create a bicycle and pedestrian master plan |
| School wellness | 9 (13 %) | Build school support for physical education and provide technical assistance to school to assist in development of policy |
| Worksite wellness | 8 (12 %) | [Promote] worksites to increase number of worksite wellness policies offered related to cancer prevention and nutrition and physical activity |
| Increased healthy food access (farmer’s markets, gardens, etc.) | 8 (12 %) | Increase access to healthy foods and beverages in [the] communities |
| Increased healthy food availability | 3 (4 %) | [Increase] facility and number of vendors in school compounds [in] compliance [with] the developed [nutrition] policy |
| Decreased unhealthy food availability | 1 (1 %) | [Increase] hospitals who adopt a policy to phase out the sale of sugary sweetened beverages |
| Community-school agreements | 0 (0 %) | |
| Decreased screen-time | 0 (0 %) |
Strategy categories are listed with numbers present and examples from action plans for each category
Survivorship Recommendations in Cancer Plans and Action Reports
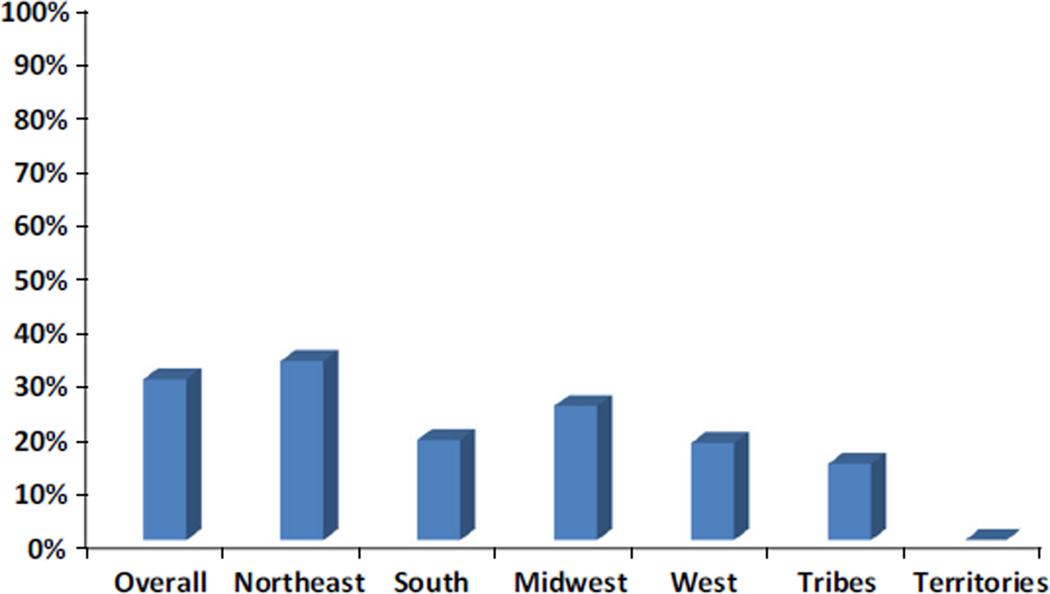
Sixty-three cancer plans contained sections related to cancer survivorship or quality of life after diagnosis. Of these cancer plans, 33 % contained any mention of NPA information in the survivorship/quality of life section (Fig. 3). The Northeast had the highest proportion of plans including NPA information, and US territories contained no NPA information for survivors (Fig. 3). Recommendations for cancer survivors ranged from general goals to specific actions. For example, one program plan included only the statement, “Improve nutrition and physical activity behaviors among cancer survivors,” while another listed, “Provide survivors access to a wellness coach…to assist them in facilitating healthy behaviors (eating better, increasing physical activity, reducing stress, losing weight, etc.) to reduce risk of recurrence and improve quality of life…” Among action reports, only four states included any information related to cancer survivors in their stated objectives or activities (data not shown).
Fig. 3.
Percentage of cancer plans containing NPA information for survivors by region. Percent of cancer plans containing NPA information for cancer survivors is listed by geographic region. Percentage is represented on the y-axis
Discussion
This is the first assessment of NPA information in the NCCCP cancer plans, providing further insight into the current primary cancer prevention priorities undertaken by the NCCCP. Both cancer plans, which cover a 5 year period and include goals and potential activities, as well as action reports, which are reported annually and represent a snapshot in time of current program goals and activities, were assessed. All cancer plans recognized NPA changes as important for cancer prevention, and the majority included goals and strategies to address NPA changes in their regions. However, the detail and the number of goals and strategies present in cancer plans varied greatly, with some cancer plans having significantly more developed NPA sections for cancer prevention than others. Fewer states, territories, and tribes, however, contained information related to NPA strategies for cancer prevention in their action reports. The majority of cancer plans also included evidenced-informed strategies to address NPA changes and obesity reduction for cancer prevention.
Use of strategies based on scientific literature or expert judgement is important because, while a large number of potential strategies exist, not all strategies have been shown to be effective. NCCCP grantees need to make the most of their resources [26]. However, 29 % (20 of 69) of cancer plans did not include such strategies for NPA changes, which could limit their ability to reach cancer prevention goals. As the literature grows on strategies to effect changes in NPA behaviors, evidence may become available for the effectiveness of additional strategies, giving comprehensive cancer control programs even more options. By focusing on these strategies, cancer plans have the largest impact on NPA changes for cancer prevention.
Obesity rates are steady or are increasing in most states, and this will likely increase the burden of obesity-related cancers [27]. Rates of some cancers where obesity is associated with increased risk, are projected to stabilize or increase by 2020, both of which will lead to increased number of new cancer cases due to a growing population [28]. Prevention through NPA change will be paramount in reducing this increased burden from obesity-related cancers.
Physical activity, in addition to be associated with a reduced risk of some cancers, has also been linked to improved quality of life for cancer survivors and has been associated with increased survival in some studies [29]. The American College of Sports Medicine and the American Cancer Society recommend that cancer survivors participate in physical activity when able [30, 31]. However, while most cancer plans included recommendations on NPA changes for cancer prevention, only a third included any mention of NPA information for cancer survivors and even fewer contained specific recommendations for survivors (data not shown). Additionally, information included varied by geographic region, with the Northeast having the most plans with NPA information for cancer survivors and the South, where obesity is highest, having the least [32]. Addressing NPA changes in the context of cancer survivorship, particularly in areas of high obesity where this information is likely to be the most in need, is an area where cancer control programs can increase awareness of recommendations during survivorship to improve quality of life and survival for cancer survivors.
State and community based programs in addition to the NCCCP have also supported and utilized NPA strategies to promote disease prevention. CDC funded grantees through programs such as Racial and Ethnic Approaches to Community Health (REACH) program and State Public Health Actions to Prevent and Control Diabetes, Heart Disease, Obesity and Associated Risk Factors and Promote School Health have included strategies to promote healthy food access and increase physical activity as a means to improve health [33–38]. Churches and worksites have shown success in promoting changes to the nutritional environment in these settings, and increases in workplace health promotion practices were seen after introduction of evidenced-based NPA programs in rural workplaces [39, 40]. School-based programs have also shown success in promoting physical activity in students [41, 42]. Additionally, a recent review of NPA related strategies for obesity prevention in rural settings, including tribes, indicated that tailoring strategies to specific target populations and building strong local partnerships were key to successfully implementing these strategies [43]. In a survey of administrators in state health departments, most respondents agreed that the health department was supportive of evidenced-based physical activity programs [44]. Therefore, partnerships with these types of organizations may promote and support implementation of these programs in communities served by the NCCCP.
This study was subject to limitations. The most current cancer plan available for each state, tribe, or territory was reviewed for this analysis. The updating and drafting of cancer plans varies in each state and territory. Therefore, while all plans covered a range of years from 2004 to 2014, some cancer plans were more up-to-date than others. Additionally, because action reports only represent actions from a single year, they may not accurately depict past or future program goals or actions. Finally, the cancer plans were searched and categorized by one researcher only. Methods used, however, were straightforward and consistent with past cancer plan reviews, and additional review would have been unlikely to change the results of the analysis [45–47].
NPA changes are important steps toward cancer prevention, and information on NPA in cancer plans can help states, tribes, and territories address these areas as part of their overall cancer prevention strategy. Increasing the number of actionable goals and strategies for NPA changes could help improve cancer prevention and control. Cancer plans with limited NPA recommendations should consider addressing these factors using goals and strategies based on scientific literature or expert judgement, such as those in recommended by The Guide to Community Preventive Services, the CDC, the Institute of Medicine, and other expert groups. However, the appropriateness of specific interventions to each population need to be considered, and CDC’s Health Equity Resource Toolkit also offers information for state public health practitioners on how to consider health equity when planning obesity prevention activities [48, 49]. Cancer plans with more developed sections can also serve as a model for CCC programs that would like to increase NPA content in their cancer plans. Further, because nutrition, physical activity, and obesity contributes to a myriad of chronic diseases, addressing NPA for cancer prevention could reduce the burden of other diseases as well. Partnerships with organizations such as the YMCA, and local parks and recreation organizations could increase the ability of NCCCP grantees to reach more people in their communities, especially groups in need of such programs, such as cancer survivors.
Footnotes
Disclaimer The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Compliance with ethical standards
Conflict of interest The authors have no conflicts of interest to disclose. The authors have no financial relationships relevant to this article to disclose.
References
- 1.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011–2012. JAMA. 2014;311(8):806–814. doi: 10.1001/jama.2014.732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ogden CL, Carroll MD, Fryar CD, Flegal KM. Prevalence of obesity among adults and youth: United States, 2011–2014. NCHS Data Brief. 2015;219:1–8. [PubMed] [Google Scholar]
- 3.Calle EE, Rodriguez C, Walker-Thurmond K, Thun MJ. Overweight, obesity, and mortality from cancer in a prospectively studied cohort of US adults. New England Journal of Medicine. 2003;348(17):1625–1638. doi: 10.1056/NEJMoa021423. [DOI] [PubMed] [Google Scholar]
- 4.Polednak AP. Estimating the number of US incident cancers attributable to obesity and the impact on temporal trends in incidence rates for obesity-related cancers. Cancer Detection and Prevention. 2008;32(3):190–199. doi: 10.1016/j.cdp.2008.08.004. [DOI] [PubMed] [Google Scholar]
- 5.Basen-Engquist K, Chang M. Obesity and cancer risk: Recent review and evidence. Current Oncology Reports. 2011;13(1):71–76. doi: 10.1007/s11912-010-0139-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Calle EE, Thun MJ. Obesity and cancer. Oncogene. 2004;23(38):6365–6378. doi: 10.1038/sj.onc.1207751. [DOI] [PubMed] [Google Scholar]
- 7.Eheman C, Henley SJ, Ballard-Barbash R, Jacobs EJ, Schymura MJ, Noone AM, et al. Annual report to the nation on the status of cancer, 1975–2008, featuring cancers associated with excess weight and lack of sufficient physical activity. Cancer. 2012;118(9):2338–2366. doi: 10.1002/cncr.27514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.NHLBI Obesity Education Initiative Expert Panel on the Identification, Evaluation, and Treatment of Obesity in Adults (US) Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults. The evidence report. Bethesda, MD: National Heart, Lung, and Blood Institute; 1998. Available from: http://www.ncbi.nlm.nih.gov/books/NBK2003/ [Google Scholar]
- 9.World Cancer Research Fund/American Institute for Cancer Research. Food, nutrition, physical activity, and the prevention of cancer: A global perspective. Washington, DC: AICR; 2007. [Google Scholar]
- 10.Thomson CA, McCullough ML, Wertheim BC, Chlebowski RT, Martinez ME, Stefanick ML, et al. Nutrition and physical activity cancer prevention guidelines, cancer risk, and mortality in the women’s health initiative. Cancer Prevention Research. 2014;7(1):42–53. doi: 10.1158/1940-6207.CAPR-13-0258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Thune I. Assessments of physical activity and cancer risk. European Journal of Cancer Prevention. 2000;9(6):387–393. doi: 10.1097/00008469-200012000-00003. [DOI] [PubMed] [Google Scholar]
- 12.Ruiz RB, Hernández PS. Diet and cancer: Risk factors and epidemiological evidence. Maturitas. 2014;77(3):202–208. doi: 10.1016/j.maturitas.2013.11.010. [DOI] [PubMed] [Google Scholar]
- 13.Parekh N, Chandran U, Bandera EV. Obesity in cancer survival. Annual Review of Nutrition. 2012;32:311–342. doi: 10.1146/annurev-nutr-071811-150713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wiseman M. The second World Cancer Research Fund/ American Institute for Cancer Research expert report. Food, nutrition, physical activity, and the prevention of cancer: A global perspective. Proceedings of the Nutrition Society. 2008;67(3):253–256. doi: 10.1017/S002966510800712X. [DOI] [PubMed] [Google Scholar]
- 15.Kushi LH, Byers T, Doyle C, Bandera EV, McCullough M, Gansler T, et al. American Cancer Society Guidelines on Nutrition and Physical Activity for Cancer Prevention: Reducing the risk of cancer with healthy food choices and physical activity. CA: A Cancer Journal for Clinicians. 2006;56(5):254–281. doi: 10.3322/canjclin.56.5.254. [DOI] [PubMed] [Google Scholar]
- 16.Centers for Disease Control and Prevention. Winnable Battles Progress Report, 2010–2015. 2015 [Google Scholar]
- 17.U.S. Department of Health and Human Services and U.S. Department of Agriculture. 2015–2020 Dietary Guidelines for Americans. (8th) 2015 http://health.gov/dietaryguidelines/2015/guidelines/
- 18.U.S. Department of Health and Human Services. Physical activity guidelines for Americans. 2008 http://health.gov/paguidelines/guidelines/
- 19.Given LS, Hohman K, Graaf L, Rochester P, Belle-Isle L. From planning to implementation to outcomes: Comprehensive cancer control implementation building blocks. Cancer Causes & Control. 2010;21(12):1987–1994. doi: 10.1007/s10552-010-9650-2. [DOI] [PubMed] [Google Scholar]
- 20.National Heart Lung, and Blood Institute. Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults. Bethesda, MD: National Institutes of Health; 1998. [PubMed] [Google Scholar]
- 21.Institute of Medicine. Nutrition standards for foods in schools: Leading the way toward healthier youth. Washington, DC: National Academies Press; 2007. [Google Scholar]
- 22.Institute of Medicine. Accelerating progress in obesity prevention: Solving the weight of the nation. Washington, DC: National Academies Press; 2012. [PubMed] [Google Scholar]
- 23.Institute of Medicine. Early childhood obesity prevention policies. Washington, DC: National Academies Press; 2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Task Force on Community Preventive Services. Recommendations to increase physical activity in communities. American Journal of Preventive Medicine. 2002;22(4S):67–72. [Google Scholar]
- 25.CDC. School health guidelines to promote healthy eating and physical activity. MMWR 60(RR–5) 2011:1–78. http://www.cdc.gov/mmwr/pdf/rr/rr6005.pdf. [PubMed]
- 26.Briss PA, Zaza S, Pappaioanou M, Fielding J, Wright-De Aguero L, Truman BI, et al. Developing an evidence-based guide to community preventive services—Methods. American Journal of Preventive Medicine. 2000;18(1):35–43. doi: 10.1016/s0749-3797(99)00119-1. [DOI] [PubMed] [Google Scholar]
- 27.Johnson NB, Hayes LD, Brown K, Hoo EC, Ethier KA. CDC National Health Report: Leading causes of morbidity and mortality and associated behavioral risk and protective factors-United States, 2005–2013. Morbidity and Mortality Weekly Report Surveillance Summaries. 2014;63:3–27. [PubMed] [Google Scholar]
- 28.Weir HK, Thompson TD, Soman A, Moller B, Leadbetter S. The past, present, and future of cancer incidence in the United States: 1975 through 2020. Cancer. 2015;121(11):1827–1837. doi: 10.1002/cncr.29258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Schmitz KH, Holtzman J, Courneya KS, Masse LC, Duval S, Kane R. Controlled physical activity trials in cancer survivors: A systematic review and meta-analysis. Cancer Epidemiology Biomarkers. 2005;14(7):1588–1595. doi: 10.1158/1055-9965.EPI-04-0703. [DOI] [PubMed] [Google Scholar]
- 30.Schmitz KH, Courneya KS, Matthews C, Demark-Wahnefried W, Galvao DA, Pinto BM, et al. American College of Sports Medicine roundtable on exercise guidelines for cancer survivors. Medicine & Science in Sports & Exercise. 2010;42(7):1409–1426. doi: 10.1249/MSS.0b013e3181e0c112. [DOI] [PubMed] [Google Scholar]
- 31.Doyle C, Kushi LH, Byers T, Courneya KS, Demark-Wahnefried W, Grant B, et al. Nutrition and physical activity during and after cancer treatment: An American Cancer Society guide for informed choices. CA: A Cancer Journal of Clinicians. 2006;56(6):323–353. doi: 10.3322/canjclin.56.6.323. [DOI] [PubMed] [Google Scholar]
- 32.Division of Nutrition PA, and Obesity, National Center for Chronic Disease Prevention and Health Promotion. 2014 http://www.cdc.gov/obesity/data/prevalence-maps.html.
- 33.McKeever C, Faddis C, Koroloff N, Henn J. Wellness within REACH: Mind, body, and soul: A no-cost physical activity program for African Americans in Portland, Oregon, to combat cardiovascular disease. Ethnicity and Disease. 2004;14(3 Suppl 1):S93–S101. [PubMed] [Google Scholar]
- 34.Woodson JM, Braxton-Calhoun M, Benedict J. Food for health and soul: A curriculum designed to facilitate healthful recipe modifications to family favorites. Journal of Nutrition Education and Behavior. 2005;37(6):323–324. doi: 10.1016/s1499-4046(06)60164-4. [DOI] [PubMed] [Google Scholar]
- 35.Lewis LB, Galloway-Gilliam L, Flynn G, Nomachi J, Keener LC, Sloane DC. Transforming the urban food desert from the grassroots up: A model for community change. Family & Community Health. 2011;34(Suppl 1):S92–S101. doi: 10.1097/FCH.0b013e318202a87f. [DOI] [PubMed] [Google Scholar]
- 36.Lewis LB, Sloane DC, Nascimento LM, Diamant AL, Guinyard JJ, Yancey AK, et al. African Americans’ access to healthy food options in South Los Angeles restaurants. American Journal of Public Health. 2005;95(4):668–673. doi: 10.2105/AJPH.2004.050260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Yancey AK, Lewis LB, Sloane DC, Guinyard JJ, Diamant AL, Nascimento LM, et al. Leading by example: A local health department-community collaboration to incorporate physical activity into organizational practice. Journal of Public Health Management and Practice. 2004;10(2):116–123. doi: 10.1097/00124784-200403000-00005. [DOI] [PubMed] [Google Scholar]
- 38.CDC. http://www.cdc.gov/chronicdisease/about/state-public-health-actions.htm.
- 39.Honeycutt S, Carvalho M, Glanz K, Daniel SD, Kegler MC. Research to reality: A process evaluation of a minigrants program to disseminate evidence-based nutrition programs to rural churches and worksites. Journal of Public Health Management and Practice: JPHMP. 2012;18(5):431–439. doi: 10.1097/PHH.0b013e31822d4c69. [DOI] [PubMed] [Google Scholar]
- 40.Laing SS, Hannon PA, Talburt A, Kimpe S, Williams B, Harris JR. Increasing evidence-based workplace health promotion best practices in small and low-wage companies, Mason County, Washington, 2009. Preventing Chronic Disease. 2012;9:E83. [PMC free article] [PubMed] [Google Scholar]
- 41.Tucker S, Lanningham-Foster LM. Nurse-led school-based child obesity prevention. The Journal of School Nursing. 2015;31(6):450–466. doi: 10.1177/1059840515574002. [DOI] [PubMed] [Google Scholar]
- 42.Austin G, Bell T, Caperchione C, Mummery WK. Translating research to practice: Using the RE-AIM framework to examine an evidence-based physical activity intervention in primary school settings. Health Promotion Practice. 2011;12(6):932–941. doi: 10.1177/1524839910366101. [DOI] [PubMed] [Google Scholar]
- 43.Calancie L, Leeman J, Jilcott Pitts SB, Khan LK, Fleischhacker S, Evenson KR, et al. Nutrition-related policy and environmental strategies to prevent obesity in rural communities: A systematic review of the literature, 2002–2013. Preventing Chronic Disease. 2015;12:E57. doi: 10.5888/pcd12.140540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Brownson RC, Ballew P, Dieffenderfer B, Haire-Joshu D, Heath GW, Kreuter MW, et al. Evidence-based interventions to promote physical activity: what contributes to dissemination by state health departments. American Journal of Preventive Medicine. 2007;33(1 Suppl):S66–S73. doi: 10.1016/j.amepre.2007.03.011. (quiz S74-S68) [DOI] [PubMed] [Google Scholar]
- 45.Neri A, Stewart SL, Angell W. Radon control activities for lung cancer prevention in National Comprehensive Cancer Control Program Plans, 2005–2011. Preventing Chronic Diseases. 2013 doi: 10.5888/pcd10.120337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Momin B, Richardson L. An analysis of content in comprehensive cancer control plans that address chronic hepatitis B and C virus infections as major risk factors for liver cancer. Journal of Community Health. 2012;37(4):912–916. doi: 10.1007/s10900-011-9507-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Townsend JS, Richardson LC, Steele CB, White DE. Evidence-based interventions and screening recommendations for colorectal cancer in comprehensive cancer control plans: A content analysis. Preventing Chronic Diseases. 2009;6(4):A127. [PMC free article] [PubMed] [Google Scholar]
- 48.Bopp M, Fallon E. Community-based interventions to promote increased physical activity: A primer. Applied Health Economics and Health Policy. 2008;6(4):173–187. doi: 10.1007/BF03256132. [DOI] [PubMed] [Google Scholar]
- 49.Payne GH, James SD, Jr, Hawley L, Corrigan B, Kramer RE, Overton SN, et al. CDC’s Health Equity Resource Toolkit: Disseminating guidance for state practitioners to address obesity disparities. Health Promotion Practice. 2015;16(1):84–90. doi: 10.1177/1524839914538967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention (CDC), National Center for Chronic Disease Prevention and Health Promotion, Division of Nutrition, Physical Activity and Obesity; 2015. Nutrition, Physical Activity and Obesity Data, Trends and Maps web site. http://www.cdc.gov/nccdphp/DNPAO/index.html. [Google Scholar]