Abstract
Background
Total hip arthroplasty (THA) is an established treatment for end-stage arthritis, congenital deformity, and trauma with good long-term clinical and functional outcomes. Delayed sciatic nerve injury is a rare complication after THA that requires prompt diagnosis and management.
Methods
We present a case of sciatic nerve motor and sensory deficit in a 52-year-old patient 2 years after index left THA. Electromyography (EMG) results and imaging with radiographs and CT of the affected hip demonstrated an aberrant acetabular cup screw in the posterior-inferior quadrant adjacent to the sciatic nerve.
Case Description
The patient underwent surgical exploration that revealed injury to the peroneal division of the sciatic nerve due to direct injury from screw impingement. A literature review identified 11 patients with late-onset neuropathy after THA. Ten patients underwent surgical exploration and pain often resolved after surgery with 56% of patients recovering sensory function and 25% experiencing full recovery of motor function.
Conclusions
Delayed neuropathy of the sciatic nerve is a rare complication after THA that is most often due to hardware irritation, component failure, or wear-related pseudotumor formation. Operative intervention is often pursued to explore and directly visualize the nerve with limited results in the literature showing modest relief of pain and sensory symptoms and poor restoration of motor function.
Keywords: total hip arthroplasty, delayed neuropathy, sciatic nerve, operative outcome
Introduction
Approximately 225,000 primary total hip arthroplasties (THAs) are performed in the United States per year, and projections indicate that more than 4 million THAs will be performed annually by 2030.1 Neurologic injury after THA is reported to occur in 0.09 to 3.7% of primary THAs and 0 to 7.4% of revision THAs.2 Noted causes of neurologic injury include direct intraoperative nerve injury, leg lengthening, excess retraction, cement extravasation, cement-related thermal damage, patient positioning, and postoperative hematoma.2 The majority of these injuries are symptomatic within the early postoperative period and can be managed conservatively with close follow-up. Delayed onset of neurologic injury is a rare complication with a unique differential diagnosis requiring appropriate management.
We report a case of neuropathy caused by malposition of an acetabular cup screw causing direct injury to the sciatic nerve. The patient developed progressively worsening loss of ankle dorsiflexion, resulting in complete footdrop 2 years after initial THA. The presentation, intervention, and outcome of other cases of delayed neuropathy are reviewed in the present report. Delayed neuropathies are most often caused by irritation from hardware, component failure, or wear-related pseudotumors.
Case Report
Initial Operative Intervention
The patient was a 52-year-old woman with end-stage arthritis of her bilateral hips with previous uncomplicated right THA that underwent an elective left THA. No intraoperative complications, abnormal anatomic landmarks, or events were noted at the time of surgery. Fluoroscopy confirmed equal limb lengths and appropriate hardware placement.
Re-presentation and Examination
The patient's initial orthopedic postoperative course was complicated by paresthesias of the right lower extremity, severe hypesthetic pain primarily in the lateral and anterior aspect of the right calf, and severe sciatica. During her hospital stay, the patient's sensation and pain improved; however, less than 1 year after her THA she noted gradual onset of weakness in her right lower extremity.
Two years after THA she presented to our neurosurgical clinic. At that time, she had developed a complete footdrop with loss of ankle dorsiflexion and required the use of an ankle-foot orthosis (AFO) to ambulate. She underwent an EMG at an outside facility, had a neurologic evaluation, and was undergoing physical therapy. Her only significant medical history was hypertension.
On physical examination, the patient had 0/5 dorsiflexion strength with 3/5 eversion and 5/5 inversion and plantarflexion strength. She had no Tinel sign over the fibular head. Decreased sensation was noted in the lateral aspect of the leg and the dorsum of the foot. She had no gross deformity of the lower extremity and had normal quadriceps and hamstring strength at the knee and the hip.
EMG showed severely reduced amplitude of the peroneal compound muscle action potentials and unrecordable superficial peroneal sensory response. There was also mild prolongation of bilateral tibial F-wave latency. Fibrillation potentials were seen in the peroneal division of the sciatic nerve with minimal evidence of reinnervation changes to the muscle units. This was indicative of sciatic neuropathy exclusively involving the peroneal division. This localized the lesion to proximal to the short head of the bicep femoris muscle. This led to obtaining advanced imaging consisting of a computed tomography (CT) of the pelvis, which demonstrated a malpositioned acetabular cup screw within the soft tissues adjacent to the sciatic nerve (Fig. 1).
Fig. 1.
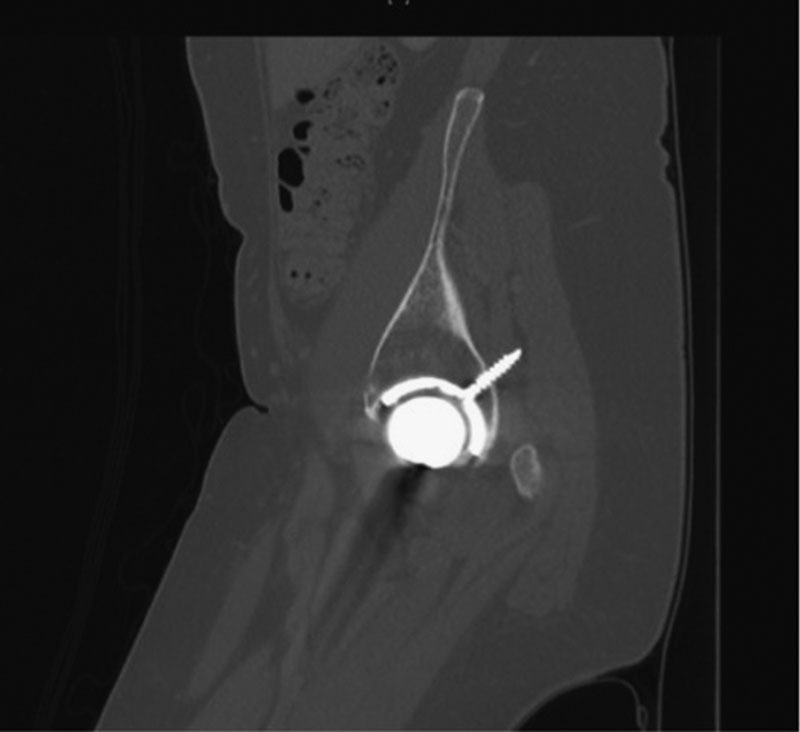
CT scan of hip showing malpositioned and long acetabular cup screw.
Operation
The patient underwent a buttock-level exploration of the sciatic nerve complex. The sciatic nerve was dissected via internal neurolysis into peroneal and tibial divisions at the level of the buttock. The division of the sciatic complex was dissected proximally to the exit of the sciatic from the pelvis. The peroneal portion of the nerve was found to be compromised by the malpositioned screw. There was no neuroma identified at the site of nerve compression, although there was evidence of nerve displacement by the protruding screw. The nerve was stimulated locally and nerve action potentials were recorded proximal and distal to the site of injury. Both peroneal and tibial portions of the nerve were tested separately to avoid false-positive conduction from the tibial division. The intraoperative recordings showed preservation of conduction across the site of nerve impingement (Fig. 2).
Fig. 2.
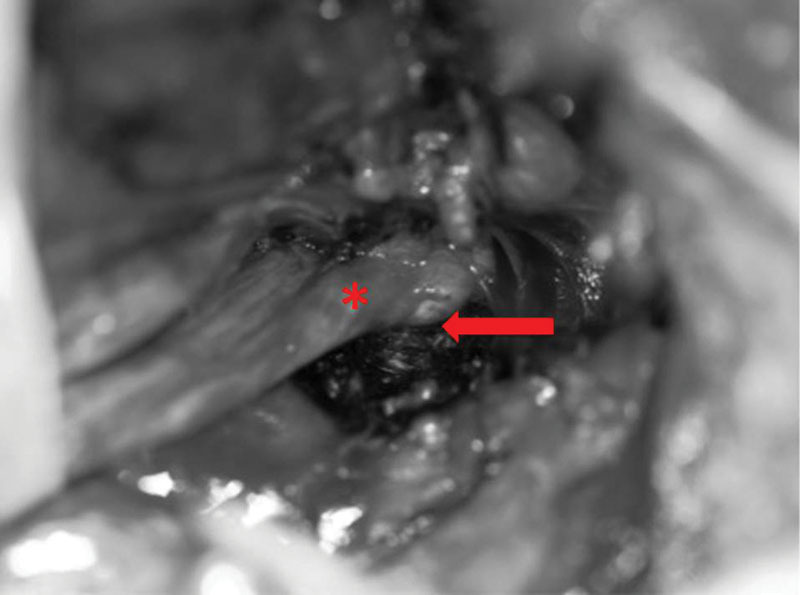
Intraoperative photo showing acetabular screw impinging on the peroneal division of the sciatic nerve. Arrow, THA screw; Asterisk, peroneal division.
The nerve was reflected off the head of the screw and gently moved proximally toward the sciatic notch. An external neurolysis of the peroneal division was performed. When the nerve was free of the screw and protected, a titanium cutting drill bit was used to shorten the screw so that it was flush with the bony interface. Repeated stimulation of the nerve confirmed that action potentials were still able to propagate past the site of injury.
Postoperative Course
The patient is now 2 years out of surgery and has demonstrated some recovery of peroneal nerve function, supporting the decision to pursue external neurolysis. The patient's improvement has not been complete and the patient requires an external orthosis.
Discussion
THA is a widely used procedure for the treatment of end-stage hip arthritis that is able to restore functional ability to hundreds of thousands of patients a year in the United States. Postoperative neurologic injury is a devastating complication with significant morbidity and functional limitations. There is a known risk of immediate neuropathy from mechanisms such as intraoperative compression from retractors, hematoma, limb lengthening, and inappropriate patient positioning. However, there is also a rarer risk of delayed neuropathy after THA that has different causative pathologies. Our findings from the literature suggest that late complications from THA may be more likely due to migration of hardware over time with subsequent nerve compression or reactive mass or fluid collection. In our case, a long, malpositioned screw was found in the soft tissue compressing the peroneal branch of the sciatic nerve.
Literature Review
A search of the PubMed database was conducted using the search term “delayed neuropathy after total hip arthroplasty” covering the years 1950 through 2015. Fifteen case reports on 16 patients were selected based on involvement of a neuropathy that appeared after THA.3 4 5 6 7 8 9 10 11 12
Patients presenting prior to 1 month included those that developed postoperative hematomas, had poor patient positioning, had previously undiagnosed hereditary neuropathy with liability to pressure palsies (HNPPs), or had anesthetic-induced inflammatory neuropathy and were felt to qualify as early postoperative complications. Delayed onset was defined as those with neuropathies developing over 1 month from surgery. The initial presentations, interventions, and outcomes are outlined in Table 1.
Table 1. Summary of literature review of cases of delayed neuropathy after total hip arthroplasty.
| Case report | Time of presentation | Clinical presentation | Workup | Intervention | Identified injury | Outcome |
|---|---|---|---|---|---|---|
| Fokter et al8 | 9 y | P: Left groin and thigh pain radiation to the knee S: Hypoesthesia in anteromedial thigh M: Quadriceps weakness R: Loss of patellar reflex |
X-ray: Eccentric location of femoral head in shell showing liner wear MRI spine: Normal EMG: Lesion localized to left lumbosacral plexus with denervation in femoral distribution CT: 13-cm intrapelvic cyst |
Lower middle laparotomy and removal of pelvic cyst Revision hip arthroplasty with allograft used to repair defect |
Wear debris mass | Full recovery of function |
| May et al | 4 mo | S: Mild numbness in foot | None | None | Limb lengthening | Full recovery of function |
| May et al | 5 mo | P: Pain in foot S: Sensory deficit in big toe |
EMG | Interpositioning of fat pad between sciatic nerve and acetabular ring | Reinforcement ring implantation and scar tissue | Resolution of pain Developed foot drop 6 mo after reoperation |
| Bader et al4 | S: Numbness in anterior and medial aspect of thigh M: Weak knee extension |
EMG: 60% loss of motor conduction in femoral nerve | Nerve separation from scar tissue, removal of granuloma and acetabular ring | Loosening of acetabular implant and migration, fracture of supplemental screw, granuloma formation | Full recovery of sensory function Motor improved to 20% of function |
|
| Katsimihas et al9 | 5 mo | S: Lateral calf, foot, posterior leg R: absent ankle jerk M: Weakness in ankle dorsiflexors, evertors, and invertors |
EMG: Sciatic nerve deficit at level of the hip or proximal thigh in tibialis anterior, peroneus longus, and gastrocnemius MRI: Spine, gluteus, and pelvis unrevealing |
AFO | Improvement in muscle strength and sensation, not back to baseline | |
| Fischer et al7 | 7 y | P: Lower buttock, difficulty with ambulation | EMG: Normal CT: Large fluid collection deep to abductor extending through greater sciatic notch Arthrogram: Fistula between joint and pelvic fluid collection |
L4–5 foraminotomy IR drainage of fluid collection Removal of fractured polyethylene liner and use of bone allograft, cyst resection, replacement of hardware |
Cyst formation from THA wear debris | Resolution of pain Able to ambulate unassisted |
| Stiehl and Stewart12 | 6 mo | P: Left foot S: Left foot |
Bone scan: No increased uptake EMG: Deficit in gluteus medius, tibialis anterior, flexor digitorum longus, biceps femoris, gastrocnemius |
Screw removal, dissection of nerve away from injury site | Pelvic screw migration compressing sciatic nerve | Resolution of pain Numbness persistent Motor function improved to 60% |
| Asnis et al3 | 5 y | P: Buttock and thigh S: Posterior thigh M: Hamstring weakness R: Decreased ankle jerk |
X-ray: Normal lumbosacral region; pelvis showing wire migration | Lidocaine injection Sciatic exploration showing 2 cm wire within sciatic nerve, epineurium incised and wire removed |
Migration of trochanteric wire | Full recovery of function |
| Edwards et al6 | 3 y | P: Buttock, posterior thigh to toe S: Dorsum of foot and lateral calf M: Tibialis anterior, extensor digitorum longus, extensor hallicis longus R: Absent ankle jerk |
X-ray: Normal EMG: Deficit in tibialis anterior, extensor hallicis longus, short head of biceps femoris Myelogram: Normal |
Sciatic nerve exploration; spur of methyl methacrylate found eroding through lateral side of sciatic, neurolysis and shaving down spur | Methyl methacrylate spur | Immediate pain relief Decrease in area of sensory loss No motor recover |
| Casagrande and Danahy5 | 7 mo | P: Foot pain M: Peroneal weakness |
EMG: Deficit in peroneal and tibial distribution | Sciatic nerve block and lumbar sympathetic block Sciatic exploration showing dense scar tissue, sciatic neurolysis and acrylic mass excision, osteotomy of ischial tuberosity |
Acrylic mass, scar tissue | Pain resolved No motor recovery |
| Leinung et al10 | 10 y | P: Thigh pain M: Weakness in femoral distribution |
CT: Large pelvic mass | Wide excision of tumor | Inflammatory pseudotumor of iliopsoas | |
| Xu et al | 2 y | S: Lateral leg and dorsum of foot M: Absence of dorsiflexion, weakness in ankle eversion |
MRI: Atrophy of extensor muscles EMG: Deficits in peroneal distribution of sciatic nerve CT: Displacement of screw |
Sciatic exploration with dissection of nerve off of screw; shaving down screw | Screw displacement and compression of sciatic nerve | Persistent motor and sensory loss |
Abbreviations: AFO, ankle-foot orthosis; CT, computed tomography; EMG, electromyography; IR, interventional radiology; MRI, magnetic resonance imaging; THA, total hip arthroplasty.
Eleven patients were defined as having late-onset neuropathies. Date of presentation ranged from 4 months to 9 years postoperatively. Presenting symptoms included eight patients with pain, nine with sensory deficits, eight with motor deficits, and four with loss of reflexes. Regarding patient workup, three received hip radiographs, four had CTs, two had magnetic resonance imaging (MRIs), and nine underwent EMGs. Ten patients received operative intervention, whereas one was treated conservatively with a brace and one with no intervention. Mechanisms of injury include three patients with mass formation adjacent to the construct, one patient with limb-lengthening injury, and seven patients with hardware migration and compression. Of those with mass formation next to the construct, one was felt to be inflammatory pseudotumor whereas two were felt to be wear-related cysts caused by metal debris. After intervention, four patients made a full recovery of function, whereas six out of eight patients with preintervention motor deficits had persistent motor deficits and one without preintervention motor deficits developed a foot drop postoperatively. Out of the nine patients with sensory deficits, four had persistent sensory loss after intervention.
Evaluation of Delayed Neuropathy
Patients with delayed neuropathy varied in presentation with pain, sensory, and motor symptoms. Most patients were evaluated with an EMG that can objectively quantify degree of motor compromise and aid in lesion localization.
As the causes of delayed nerve injury are largely local anatomical changes, CT and MRI can be helpful in identifying the cause of neuropathy. EMG localization of the level of deficit, combined with screw malposition, suggested that it was the cause of the patient's sensory and motor loss.
Conclusion
Delayed neuropathy is a rare complication after primary THA that can be caused by hardware irritation as in the present case. Patients can present with pain, sensory loss, motor loss, and decreased reflexes that are best worked up with EMG to localize the area of neuropathy and imaging to identify the root source. Results from the literature show that operative intervention is often pursued to explore and directly visualize the nerve with limited results in the literature showing modest relief of pain and sensory symptoms and poor restoration of motor function.
Note
Linda W. Xu and Anand Veeravagu authors contributed equally to this manuscript.
References
- 1.Kurtz S, Ong K, Lau E, Mowat F, Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am. 2007;89(4):780–785. doi: 10.2106/JBJS.F.00222. [DOI] [PubMed] [Google Scholar]
- 2.Brown G D, Swanson E A, Nercessian O A. Neurologic injuries after total hip arthroplasty. Am J Orthop. 2008;37(4):191–197. [PubMed] [Google Scholar]
- 3.Asnis S E, Hanley S, Shelton P D. Sciatic neuropathy secondary to migration of trochanteric wire following total hip arthroplasty. Clin Orthop Relat Res. 1985;(196):226–228. [PubMed] [Google Scholar]
- 4.Bader R, Mittelmeier W, Zeiler G, Tokar I, Steinhauser E, Schuh A. Pitfalls in the use of acetabular reinforcement rings in total hip revision. Arch Orthop Trauma Surg. 2005;125(8):558–563. doi: 10.1007/s00402-005-0051-z. [DOI] [PubMed] [Google Scholar]
- 5.Casagrande P A, Danahy P R. Delayed sciatic-nerve entrapment following the use of self-curing acrylic. A case report. J Bone Joint Surg Am. 1971;53(1):167–169. [PubMed] [Google Scholar]
- 6.Edwards M S, Barbaro N M, Asher S W, Murray W R. Delayed sciatic palsy after total hip replacement: case report. Neurosurgery. 1981;9(1):61–63. doi: 10.1227/00006123-198107000-00010. [DOI] [PubMed] [Google Scholar]
- 7.Fischer S R, Christ D J, Roehr B A. Sciatic neuropathy secondary to total hip arthroplasty wear debris. J Arthroplasty. 1999;14(6):771–774. doi: 10.1016/s0883-5403(99)90237-1. [DOI] [PubMed] [Google Scholar]
- 8.Fokter S K, Repse-Fokter A, Takac I. Case report: femoral neuropathy secondary to total hip arthroplasty wear debris. Clin Orthop Relat Res. 2009;467(11):3032–3035. doi: 10.1007/s11999-009-0894-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Katsimihas M, Hutchinson J, Heath P, Smith E, Travlos J. Delayed transient sciatic nerve palsy after total hip arthroplasty. J Arthroplasty. 2002;17(3):379–381. doi: 10.1054/arth.2002.30775. [DOI] [PubMed] [Google Scholar]
- 10.Leinung S, Schönfelder M, Würl P. [Inflammatory pseudotumor of the ileopsoas muscle with femoral paralysis caused by massive metal abrasion of a hip endoprosthesis] Chirurg. 2002;73(7):725–728. doi: 10.1007/s00104-002-0444-2. [DOI] [PubMed] [Google Scholar]
- 11.May O, Girard J, Hurtevent J F, Migaud H. Delayed, transient sciatic nerve palsy after primary cementless hip arthroplasty: a report of two cases. J Bone Joint Surg Br. 2008;90(5):674–676. doi: 10.1302/0301-620X.90B5.19536. [DOI] [PubMed] [Google Scholar]
- 12.Stiehl J B, Stewart W A. Late sciatic nerve entrapment following pelvic plate reconstruction in total hip arthroplasty. J Arthroplasty. 1998;13(5):586–588. doi: 10.1016/s0883-5403(98)90060-2. [DOI] [PubMed] [Google Scholar]