Abstract
[Purpose] A simple rehabilitation device system for strengthening upper limb muscles in hemiplegic patients was developed. This system, which stimulates active exercise while accounting for intensity, time, and frequency, was examined in the present pilot study. [Subjects and Methods] Patients had shoulder pain and limited shoulder movement. Changes in range of motion (ROM) and scores of a visual analog scale (VAS) for pain were evaluated in the experimental and control groups every four weeks for twelve weeks. The modified motor assessment scale (MMAS) was used before and after experiments. [Results] Significant differences between experimental times in ROM for shoulder flexion, abduction, and adduction on the paralyzed side were observed in the experimental group at every time point. Pain VAS scores in the experimental group improved progressively and significantly with time, indicating a consistently increasing effect of exercise. There were significant differences between the MMAS scores before and after completion of the program in the experimental group. [Conclusion] Muscle strengthening is important in hemiplegic patients, and active exercise was more efficient than passive exercise in this regard. Rehabilitation with the Monkey Chair and Band system may represent an efficient and important tool in upper limb training and comprehensive modern rehabilitation therapy.
Key words: Monkey Chair and Band system, Upper extremity, Stroke
INTRODUCTION
Shoulder pain, which is experienced by 70–84% of patients with hemiplegic stroke, has become a dominant factor in delaying participation in a rehabilitation program1, 2). The pain and limited range of motion (ROM) make ambulation more difficult. In addition to affecting physical activities owing to the compromised ability to maintain balance and restricting activities of daily living (ADL), this negatively impacts the desire and ability to engage in social activities because of feelings such as fear, frustration, and disappointment3, 4). If the pain is not treated, it also causes edema, joint instability, joint contracture, and bone and soft tissue atrophy, as well as limits the ability to move the upper limbs5). The goal of rehabilitation therapy for hemiplegic patients is to allow them to regain independence in activities and make it easier to perform such activities by improving the movement on the paralyzed side6). Therefore, muscle strengthening is recommended to improve the ability to perform exercise7, 8).
Kinesitherapy is essential for preventing muscle tonicity and atrophy in hemiplegic patients. With continuous exercise, it improves muscular strength and joint flexibility, which allows performing more physical activities. Most studies on exercise effects show that exercise contributes to the recovery of physical function. Duncan et al. reported that balancing ability was increased after twelve weeks of complex exercise including bicycling9). According to Smith et al., there was a significant improvement in the strength of the hamstrings and spastic reflexes in patients who received treadmill exercise in the form of a low-intensity cardiac rehabilitation program administered three times a week for twelve weeks10). Moreover, Rimmer et al. reported that patients who had performed one-hour exercise programs three times a week for three months showed meaningful differences in oxygen uptake, muscle, hamstrings, and spine flexion, and body composition (weight, body mass index [BMI], thickness of subcutaneous fat)11). The fact that the upper limb motor ability defines the ability to perform ADL emphasizes the importance of its rehabilitation12). For hemiplegic stroke patients, passive or active exercises using machines and apparatuses are recommended to increase the ROM of the shoulder joint while simultaneously reducing shoulder pain13).
Generally, physical therapy is combined with apparatus and robotic therapy in rehabilitation of upper limb motor ability14,15,16). However, studies on the effectiveness of rehabilitation robotic systems that assist hemiplegic patients in performing exercises have been lacking. Furthermore, few comparative studies have been conducted. Finally, despite their importance, there is a deficit of studies on the impact of rehabilitation systems on the effect of exercise programs.
In this study, a simple rehabilitation device system (Monkey Chair and Band System) was developed for strengthening of upper limb muscles of hemiplegic patients. Unlike the modern complex robotic systems, which utilize only passive exercise, this system employs active exercise and accounts for factors such as exercise intensity, time, and frequency. The present pilot study comprehensively investigates the effects of this new system, focusing on the improvement of upper limbs motor ability by strengthening muscles in hemiplegic patients.
SUBJECTS AND METHODS
Patients with post-stroke hemiparesis were treated at the Rehabilitation Medical Center in Yongin, Korea. They were enrolled in this study after they understood its purpose. Written informed consent was obtained before enrollment, and the study was approved by the Institutional Review Board (IRB) (HYI-13-046-1). The inclusion criteria were as follows: 1) presence of post-stroke hemiparesis for at least 6 months as diagnosed by a medical doctor; 2) stable vital signs (heart rate under 100/min, blood pressure under 150/80 mmHg) and ability to understand the meaning of this study; 3) ability to acquire more than twenty-five points in the Korean Mini Mental Status Examination (MMSE-K); 4) presence of shoulder pain; and 5) ability to flex and abduct the shoulder actively over 90° with limitation of shoulder ROM and ability to extend and adduct the shoulder over 20°. Twelve patients who satisfied the above criteria were assigned randomly to the experimental or control group such that selection bias in gender, age, and period was eliminated (Table 1).
Table 1. The general characteristics of participants.
| Characteristics Group | Gender (n) | Age (years) | Period (months) | Stroke type (n) | Hemiparetic side (n) | Height (cm) | Weight (kg) | BMI (kg/m2) | |||
|---|---|---|---|---|---|---|---|---|---|---|---|
| M | F | M ± SD | M ± SD | cerebral hemorrhage | ischemic stroke | right | left | M ± SD | M ± SD | M ± SD | |
| Experimental | 3 | 3 | 58.0 ± 13.6 | 15.8 ± 8.9 | 5 | 1 | 2 | 4 | 162.7 ± 12.5 | 56.5 ± 15.8 | 21.1 ± 3.7 |
| Control | 4 | 2 | 50.5 ± 8.9 | 14.9 ± 7.6 | 4 | 2 | 3 | 3 | 165.0 ± 10.5 | 63.4 ± 10.2 | 23.6 ± 1.6 |
M: male; F: female; M: mean; SD: standard deviation; BMI: body mass index
First, the general characteristics and subjective symptoms of the participants were determined via a pre-test examination, and an additional physical examination was performed for patients who reported pain. Changes in ROM and scores of the visual analog scale (VAS) for pain were then measured in the experimental and control groups of the Monkey Chair and Band program at weeks 0 (pre-test), 4 (first test), 8 (second test), and 12 (third test). Modified motor assessment scale (MMAS) scores were also evaluated before the experiment and after twelve weeks.
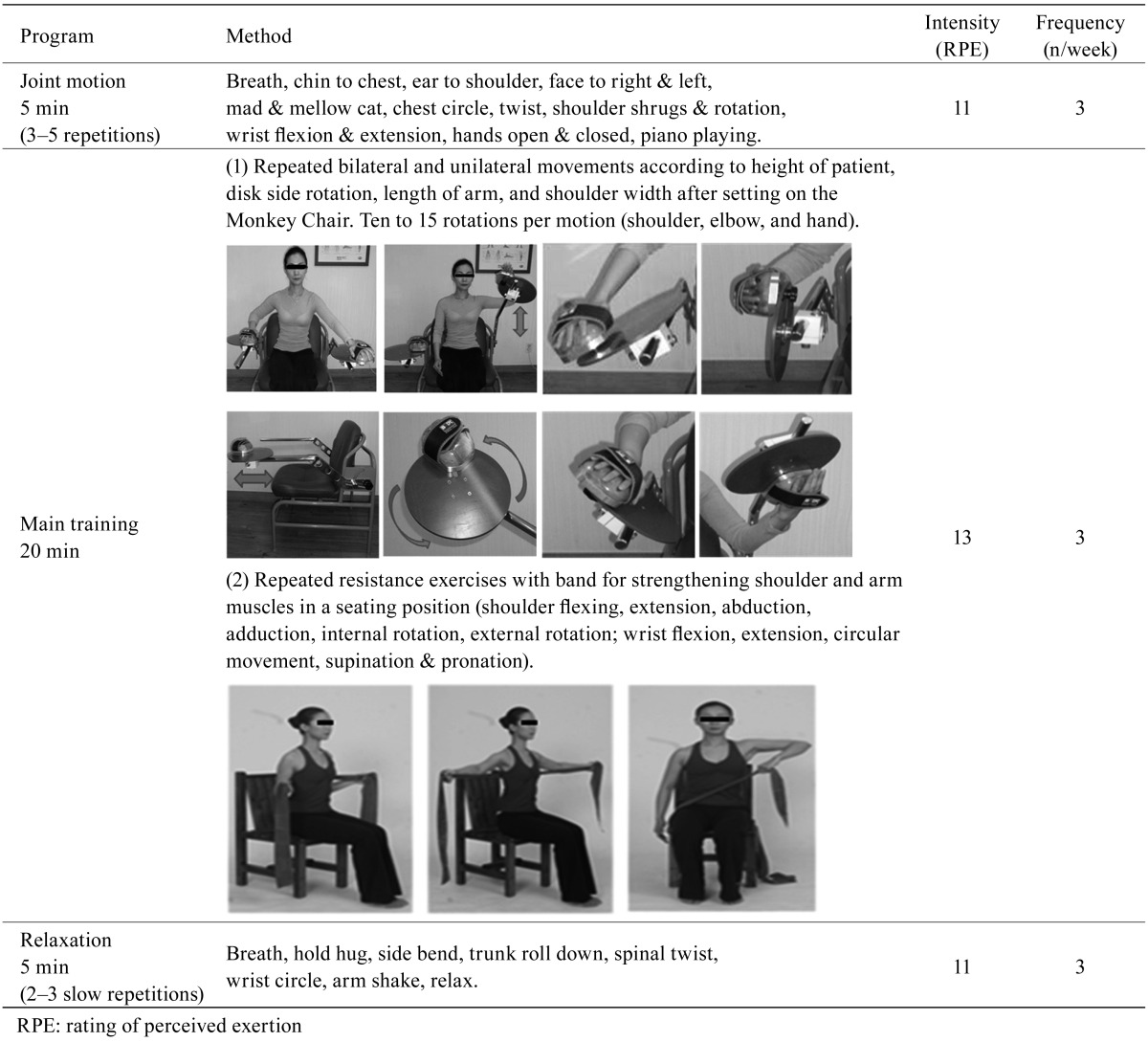
The Monkey Chair was developed to help hemiplegic patients exercise actively during upper limb rehabilitation by improving stability, accuracy, and coordination between the normal and paralyzed sides. Exercises supported by the device include flexion & extension, adduction & abduction, and internal rotation & external rotation of the shoulder, flexion & extension of the elbow, and pressing & unfolding of the palm. The device can provide all the elements of precise, active, repetitive, and goal-directed exercise for brain plasticity improvement. The height, length, and width of the arms of the Monkey Chair were adjusted based on the physical condition of the patients such that they were able to hold the spindle comfortably. The intensity of the rotation of the spindle was increased during the test in 4 steps (1.02 kgf, 2.75 kgf, 4.59 kgf, and 6.12 kgf). The speed and power of the spindle could be controlled. The Monkey Chair and Band system was designed to strengthen the patients’ shoulder and elbow muscles by facilitating active movements. Before starting exercise, the ability to extend a resistive band (Thera-Band, Hygenic Corporation, USA) was assessed using the formula ([extension length −stable length]/stable length) ×100. Depending on the degree of personal adaptation, the exercise intensity was adjusted every fourth week. Maximum resistance standards were determined based on the ability to pull the band ten times with the same performance. Depending on the results, the patients then performed exercise using suitable color-coded bands (yellow: 0.7–1.0 kgf, red: 0.9–1.6 kgf, green: 1.1–1.9 kgf, or blue: 1.4–2.8 kgf). For better consistency of results, shoulder flexion, extension, abduction, and adduction on the paralyzed side were measured for ROM determination using the same joint protractor (Sammons Preston®, 2003) by the same researcher. During measurements of the passive maximum angle after the active initial motion, the participants lay straight on their back while being fixed at each axis. The values at which the patients started to feel constant pain and the range of joint flexibility were measured. A VAS was used to measure shoulder pain. The MMAS, a tool with verified reliability and validity in evaluating exercise ability of hemiplegic patients, was used to assess the upper limbs and ability to walk. The MMAS includes nine elements, with eight of them designed to evaluate exercise ability and one to assess muscle tension. In this study, upper arm function, hand movement, and walking ability were measured before and after the tests. The scale consisted of seven points, from 0 to 6, with higher values indicating higher ability. The two groups also received the general physical therapy for stroke patients at the hospital. The program for the experimental group comprised joint motion (stretching gymnastics), main training, and relaxation using the Monkey Chair and Band, which were performed three times a week for 30 minutes each, for a total of thirty-six times in twelve weeks. The exercises were performed at an intensity corresponding to a Rating Perceived Exertion (RPE) scale score of 13 points (70% effort) out of 15 points (6–20). If changing the exercise level induced fatigue as determined based on the RPE score and degree of pain, the exercise was stopped (Table 2 .
Table 2. The Monkey Chair and Band program.
All analyses were conducted with SPSS (Version 18.0; SPSS, Inc., Chicago, IL, USA), and means and standard deviations were calculated for all data. Repeated measures analysis of variance (RMANOVA) was used to evaluate changes in ROM of the shoulder and VAS scores for every time point and each group during the twelve weeks of exercise. The level of significance was set at p<0.05 for all differences, and the degree of freedom was 5.
RESULTS
The differences in ROM of the shoulder on the paralyzed side between the experimental and control groups and the changes at baseline and weeks 4, 8, and 12 are shown in Table 3. Significant differences were found in shoulder flexion at baseline and weeks 4, 8, and 12. Different trends of changes in flexion were revealed in the experimental and control groups (p<0.05). The experimental group showed an especially remarkable increase in ROM with time (p<0.01). The changes in shoulder abduction at baseline and weeks 4, 8, and 12 were statistically significant (p<0.001). There were also significant changes in abduction ROM between the experimental and control groups (p<0.05). The two groups differed in terms of trends of changes in abduction ROM, with a significant increase observed in the experimental group (p<0.001). Significant differences were also found in shoulder adduction at baseline and weeks 4, 8, and 12 (p<0.05). Differences in the trends of changes of adduction ROM between the two groups were observed at each time point, with the experimental group showing a noticeable increase (p<0.05). No improvements were detected in ROM for flexion, extension, abduction, and adduction in the control group during the twelve weeks. The experimental and control groups showed almost identical ROMs for flexion, abduction, and adduction at baseline (week 0, pre-test).
Table 3. The statistical comparison of shoulder ROM on the paralyzed side between the experimental and control groups at different time points.
| Variable | Experimental group (n=6) | Control group (n=6) | |
|---|---|---|---|
| M ± SD | M ± SD | ||
| Shoulder | |||
| ROM for flexion | baseline | 130.0 ± 29.5 | 127.8 ± 4.0 |
| week 4 | 150.0 ± 27.8 | 127.0 ± 4.0 | |
| week 8 | 159.2 ± 20.4 | 126.2 ± 3.8 | |
| week 12 | 165.0 ± 19.5 * | 126.2 ± 3.8 | |
| ROM for extension | baseline | 25.8 ± 10.7 | 36.3 ± 13.2 |
| week 4 | 36.7 ± 16.6 | 36.3 ± 13.2 | |
| week 8 | 40.0 ± 20.0 | 36.5 ± 13.2 | |
| week 12 | 41.7 ± 20.9 | 36.5 ± 13.2 | |
| ROM for abduction | baseline | 123.3 ± 33.7 | 117.8 ± 18.3 |
| week 4 | 143.3 ± 32.0 | 118.7 ± 18.3 | |
| week 8 | 160.0 ± 22.8 | 118.7 ± 18.3 | |
| week 12 | 166.7 ± 21.6 * | 118.7 ± 18.3 | |
| ROM for adduction | baseline | 21.7 ± 7.5 | 20.0 ± 4.9 |
| week 4 | 27.5 ± 4.2 | 20.3 ± 5.2 | |
| week 8 | 30.0 ± 6.3 | 20.8 ± 4.9 | |
| week 12 | 30.8 ± 5.9 * | 20.8 ± 4.9 | |
M: mean; SD: standard deviation; ROM: range of motion; *p<0.05 significant difference at this time point in the group
The changes and differences in the scores of the pain VAS during the twelve weeks of the program are shown in Table 4. Significant differences between the experimental group and the control group were detected at each time point. The experimental group showed a remarkable positive change at a 1% significance level and demonstrated a significant difference after each four-week period (p<0.001). Based on these results, the program was considered efficient in reducing pain. Moreover, the change in VAS scores in the experimental group was rapid, with remarkable improvements present already at week 4.
Table 4. The statistical comparison of pain VAS scores between the experimental and control groups at different time points.
| Variable | Experimental group (n=6) | Control group (n=6) | |
|---|---|---|---|
| M ± SD | M ± SD | ||
| VAS score | baseline | 48.3 ± 24.0 | 45.0 ± 10.5 |
| week 4 | 40.0 ± 27.6 | 43.3 ± 8.2 | |
| week 8 | 33.3 ± 26.6 | 35.0 ± 10.5 | |
| week 12 | 10.0 ± 11.0 * | 35.0 ± 12.2 | |
M: mean; SD: standard deviation; VAS: visual analogue scale; *p<0.05 significant difference at this time point in the group
The changes and differences in MMAS scores during the twelve weeks of the program are shown in Table 5. The addition of the twelve-week Monkey Chair and Band program to the traditional physical therapy resulted in a statistically significant difference between the scores before and after the program in the experimental group (p<0.05), while the control group did not show a significant difference.
Table 5. The statistical comparison of MMAS scores between the experimental and control groups.
| Variable | Experimental group (n=6) M ± SD |
Control group (n=6) M ± SD |
||
|---|---|---|---|---|
| MMAS score | 5 | Before | 2.7 ± 1.9 | 2.7 ± 2.3 |
| After | 4.3 ± 1.5 ** | 3.5 ± 2.0 | ||
| 6 | Before | 2.0 ± 2.4 | 2.0 ± 2.3 | |
| After | 3.2 ± 2.3 ** | 2.2 ± 2.4 | ||
| 8 | Before | 4.0 ± 1.1 | 3.5 ± 1.4 | |
| After | 5.3 ± 0.5 * | 3.7 ± 1.2 | ||
M: mean; SD: standard deviation; MMAS: modified motor assessment scale; 5: upper arm function; 6: hand movement; 8: walking; *p<0.05, **p<0.01 between scores before and after program
DISCUSSION
The shoulder joint is one of the most flexible joints of the body, with the greatest ROM. Hemiplegic stroke patients experience limitation in shoulder ROM and shoulder pain. This results in a vicious circle of constantly restricted activities.
The Monkey Chair and Band system described in this study seems to maintain muscle balance by continuously stimulating the flexor and extensor muscles, and it reduces muscle tone while increasing joint flexibility. In the control group, however, there were no remarkable improvements in ROM. In some cases, reduction in ROM is caused by unstable position, inactivity, and decreased muscle and joint flexibility of the affected side. Therefore, the new system should be efficient in stroke patients who feel frustrated by the long-term rehabilitation, resulting in insufficient engagement in the rehabilitation program. Similar to the studies of Bertiti as well as Brouwer et al., a positive effect of resistance exercise on ROM in hemiplegic stroke patients was detected in the present work17, 18).
Exercises improving both ROM and weigh resistance are necessary for enhancing upper limbs strength. Moreover, exercises for muscular strength of the elbow and fingers are also needed, as well as training aimed at improving hand skills and functional work ability19). According to Wolf et al., constraint-induced movement therapy led to recovery of functional exercise ability of the arms in patients three to nine months after a stroke20). The authors suggested that the improvement in motor ability was due to changes in the central nervous system. This observation further supports the results of the present study.
A previous study of the effects of reaching exercise in hemiplegic patients did not detect significant differences in MMAS scores for upper limb motor skills21). In contrast, according to the present results, the exercise program aimed at stabilization and strength training of the shoulder using the Monkey Chair and Band system improved the MMAS scores.
Patients in the experimental group, who had suffered from pain, experienced pain relief and increase in ROM after the completion of the Monkey Chair and Band program. No significant differences in pain intensity were observed in the control group, whereas muscular strength and movement control declined. The differences in shoulder extension ROM were less significant than the differences in ROM for other shoulder movements. This could be caused by differences in the state of patients in the experimental and control groups. Furthermore, body movement instead of joint movement was measured during the extension exercise. The use of the Monkey Chair and Band system led to especially large improvements in shoulder flexion (up to 92% compared to 72% at baseline), whereas conventional manual therapy resulted in no improvement. It can be concluded that further improvements are needed in remedial exercise equipment, including a wider range of motion. Furthermore, additional studies are necessary on automation of clinical exercise testing and frame motion.
This study has the following limitations. 1) Other treatments for shoulder pain (acupuncture, oral agents, electrotherapy, and joint cavity injections) were not controlled for because of ethical issues. 2) Physical therapy and exercises within the regular rehabilitation therapy differed for patients of the control group because each of them had an individual treatment program. 3) The results cannot be generalized owing to the insufficient sample size and study period. 4) Patients who could not flex and abduct the shoulder beyond 90° and extend and adduct the shoulder beyond 20° were not included in the study.
The use of the Monkey Chair and Band upper limbs strengthening program resulted in significant differences in both ROM improvement and pain relief compared to the general therapy, as well as in improvement of muscle strength. According to Kawahira et al., repetition of a facilitation technique promoted the functional recovery of the hemiplegic upper limb to a greater extent than the conventional rehabilitation22). The present study demonstrated the positive effect of repetitive and intensive training according to the Monkey Chair and Band program in hemiplegic stroke patients.
The rehabilitation system presented in this study is more efficient both in terms of time and cost than the use of complex apparatuses without a systemic program. Moreover, the developed program is repetitive and easy to adapt to other rehabilitation programs. Active resistant exercise yielded better results in terms of ROM, pain VAS scores, and MMAS scores than passive robot-assisted exercises while being less expensive to implement. The use of the Monkey Chair and Band system developed in this study to strengthen the upper limb muscles via simple active exercise administered according to the therapy program led to remarkable improvements in ROM and pain VAS scores of hemiplegic upper limbs compared to passive therapies. Muscle strengthening is clearly of high importance for patients with hemiplegia, and an active therapy produced a greater effect than a passive therapy. Therefore, the rehabilitation program utilizing the simple Monkey Chair and Band apparatus can be considered an important tool in efficient training of upper limbs and comprehensive modern rehabilitation therapy.
REFERENCES
- 1.Lee HS, Kim JU: The effect of self-directed exercise using a task board on pain and function in the upper extremities of stroke patients. J Phys Ther Sci, 2013, 25: 963–967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Griffin JW: Hemiplegic shoulder pain. Phys Ther, 1986, 66: 1884–1893. [DOI] [PubMed] [Google Scholar]
- 3.An SH, Lee GC, Kim SY: A study of the clinical utility of the BPI-12 and 23 in predicting shoulder pain in stroke patients. J Phys Ther Sci, 2012, 24: 455–460. [Google Scholar]
- 4.Roy CW: Shoulder pain in hemiplegia: a literature review. Clin Rehabil, 1988, 2: 35–44. [Google Scholar]
- 5.Tepperman PS, Greyson ND, Hilbert L, et al. : Reflex sympathetic dystrophy in hemiplegia. Arch Phys Med Rehabil, 1984, 65: 442–447. [PubMed] [Google Scholar]
- 6.Shelton FD, Volpe BT, Reding M: Motor impairment as a predictor of functional recovery and guide to rehabilitation treatment after stroke. Neurorehabil Neural Repair, 2001, 15: 229–237. [DOI] [PubMed] [Google Scholar]
- 7.Bohannon RW: Muscle strength and muscle training after stroke. J Rehabil Med, 2007, 39: 14–20. [DOI] [PubMed] [Google Scholar]
- 8.Hashidate H, Shiomi T, Sasamoto N: Effects of 6 months combined functional training on muscle strength, postural balance and gait performance in community-dwelling individuals with chronic stroke hemiplegia. J Phys Ther Sci, 2011, 23: 617–623. [Google Scholar]
- 9.Duncan P, Studenski S, Richards L, et al. : Randomized clinical trial of therapeutic exercise in subacute stroke. Stroke, 2003, 34: 2173–2180. [DOI] [PubMed] [Google Scholar]
- 10.Smith GV, Silver KH, Goldberg AP, et al. : “Task-oriented” exercise improves hamstring strength and spastic reflexes in chronic stroke patients. Stroke, 1999, 30: 2112–2118. [DOI] [PubMed] [Google Scholar]
- 11.Rimmer JH, Rauworth AE, Wang EC, et al. : A preliminary study to examine the effects of aerobic and therapeutic (nonaerobic) exercise on cardiorespiratory fitness and coronary risk reduction in stroke survivors. Arch Phys Med Rehabil, 2009, 90: 407–412. [DOI] [PubMed] [Google Scholar]
- 12.Woodson AM: Stroke. In: Trombly CA (ed.), Occupational therapy for physical dysfunction, 4th ed. Baltimore: Williams & Wilkins, 1995, pp 678–680. [Google Scholar]
- 13.Seneviratne C, Then KL, Reimer M: Post-stroke shoulder subluxation: a concern for neuroscience nurses. Axone, 2005, 27: 26–31. [PubMed] [Google Scholar]
- 14.Culmer PR, Jackson AE, Makower S, et al. : A control strategy for upper limb robotic rehabilitation with a dual robot system. IEEE/ASME Trans Mechatron, 2010, 15: 575–585. [Google Scholar]
- 15.Yoo DH, Cha YJ, Kim SK, et al. : Effect of three-dimensional robot-assisted therapy on upper limb function of patients with stroke. J Phys Ther Sci, 2013, 25: 407–409. [Google Scholar]
- 16.Huang Q, Zhou Y, Yu L, et al. : The reliability of evaluation of hip muscle strength in rehabilitation robot walking training. J Phys Ther Sci, 2015, 27: 3073–3075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bertoti DB: Effect of short leg casting on ambulation in children with cerebral palsy. Phys Ther, 1986, 66: 1522–1529. [DOI] [PubMed] [Google Scholar]
- 18.Brouwer B, Davidson LK, Olney SJ: Serial casting in idiopathic toe-walkers and children with spastic cerebral palsy. J Pediatr Orthop, 2000, 20: 221–225. [PubMed] [Google Scholar]
- 19.Pang MY, Harris JE, Eng JJ: A community-based upper-extremity group exercise program improves motor function and performance of functional activities in chronic stroke: a randomized controlled trial. Arch Phys Med Rehabil, 2006, 87: 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wolf SL, Winstein CJ, Miller JP, et al. EXCITE Investigators: Effect of constraint-induced movement therapy on upper extremity function 3 to 9 months after stroke: the EXCITE randomized clinical trial. JAMA, 2006, 296: 2095–2104. [DOI] [PubMed] [Google Scholar]
- 21.Park MC: Effect of the passive pre-positioning to proximal upper limb on reaching movement and cortical reorganization of patient with stroke (dissertation). Department of Rehabilitation Science Graduate School, Daegu University, 2009.
- 22.Kawahira K, Shimodozono M, Etoh S, et al. : Effects of intensive repetition of a new facilitation technique on motor functional recovery of the hemiplegic upper limb and hand. Brain Inj, 2010, 24: 1202–1213. [DOI] [PMC free article] [PubMed] [Google Scholar]