Abstract
[Purpose] For adult patients with late-onset idiopathic scoliosis, cosmetic concerns and pain are the main reasons for seeking treatment at a physician’s office. The purpose of this paper was to describe the mid-term effect of physical rehabilitation and part-time bracing on an adult scoliosis patient who had been suffering from chronic low back pain for fourteen years. [Subject and Methods] Case description: A 37-year-old female patient with late-onset idiopathic scoliosis presented in the office of the first author in January 2014. She reported having chronic pain (low back pain) since the age of 23 and reported daily pain at a level of 5–7 on average on a Visual Analogue Scale of 0 to 10. She received a short scoliosis-specific Schroth exercise program and was also fitted with a Gensingen brace for part-time wear. [Results] At a 16 month follow-up, the patient no longer suffered from daily low back pain (with heavy lifting only) and was fully active. Additionally, her lumbar Cobb angle and angle of trunk rotation improved. [Conclusion] Patients with late-onset idiopathic scoliosis and pain may benefit from a pattern-specific conservative treatment approach. In this population, surgical intervention should be regarded as the last resort, since there are many long-term unknowns with surgery.
Key words: Adult scoliosis, Pain, Physical rehabilitation
INTRODUCTION
Scoliosis is a three-dimensional deformity of the spine and trunk1,2,3,4). The majority of scoliosis cases (80–90%) are adolescent idiopathic scoliosis (AIS). The remaining cases are of other origin (congenital, neuromuscular, mesenchymal disorders, syndromic, etc.)5).
Progression of curvature during growth is a major concern. Currently, level-1 evidence exists that allowes to conclude that curvature progression can be halted successfully during growth6,7,8,9) in most instances.
In adulthood, cosmetic issues and pain are the most common reasons scoliosis patients consult a physician10). Typically, pain medication and/or spinal fusion surgery are suggested11). Large cohort studies have shown that there is no correlation between pain and the degree of curvature12, 13). However, in a population with scoliosis, there is slightly more pain than in controls without scoliosis1, 10).
There is some evidence that a course of intensive physical rehabilitation lasting six weeks can improve pain in a population with scoliosis. This has been found in two cohort studies utilizing a pre-/post-treatment design12, 13). However, the mid- or long-term effects of this intervention have not yet been determined.
Patients may seek advice from a spine surgeon; however, evidence that shows that pain can be prevented or improved through spinal fusion surgery in the long-term is lacking14, 15). Therefore, it stands to reason that conservative management of pain should be the first line of defense in patients with scoliosis.
Physical rehabilitation and bracing in adulthood have not yet been investigated at length. There are short- and mid-term studies available; however, a standard for bracing in adults has not yet been determined. While specific braces can improve scoliosis during growth16), bracing for adults with scoliosis and pain has not yet been investigated.
Since it is questionable that surgery is useful in the mid- and long-term17,18,19,20) and it is known that significant rates of long-term complications exist17, 21,22,23), it is necessary to study the mid- and long-term effects of current conservative treatments as well. Cases should be compiled to investigate if patients with spinal deformity and pain can achieve positive results from conservative outpatient treatment. In this study, a single case is presented; an adult woman with late-onset idiopathic scoliosis (LIS) with chronic pain.
SUBJECT AND METHODS
A 37-year-old female patient with LIS from Norway presented in the office of the first author in January 2014. She had experienced chronic pain (low back pain, LBP) since the age of 23. She refused to consider surgery. Her Cobb angles were 56° thoracic and 50° lumbar, with the curvatures rather balanced (Figs. 1, 2, and 3) and her angles of trunk rotation values (ATR) were 17° thoracic and 3° lumbar as measured with a Scoliometer™.
Fig. 1.
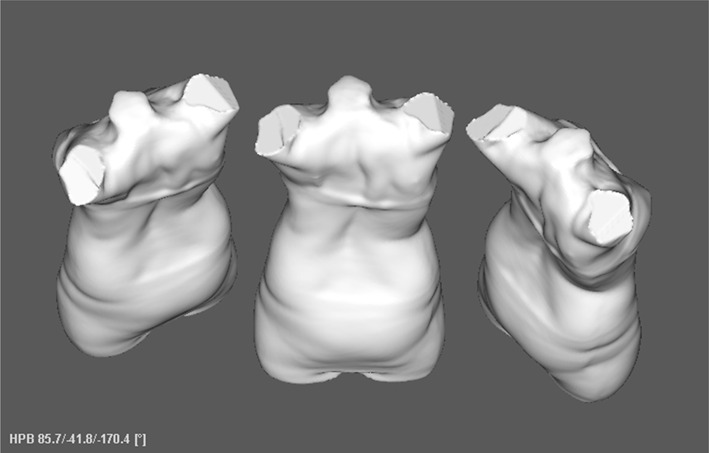
Three aspects of a scan made for the patient prior to CAD/CAM (computer-aided manufacturing) brace construction The patient had a combined curvature with a major lumbar deformity.
Fig. 2.
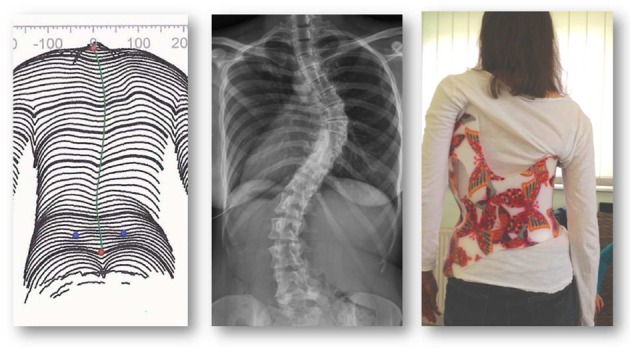
Left: Clinical appearance of the trunk at the start of treatment. Middle: X-ray at the start of treatment. Right: Gensingen brace (GBW) constructed for the patient.
Fig. 3.
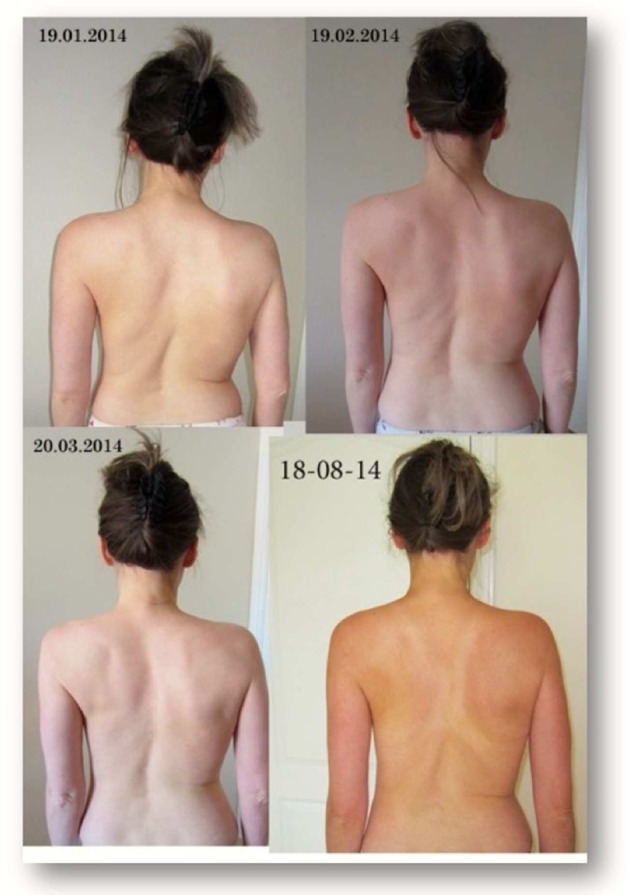
Pictures taken by the patient’s husband, which demonstrate a postural improvement over time
Other than chronic low back pain for 14 years no other severe health problems were reported during the investigation. The patient experienced daily pain at an average level of 5–7 on a Visual Analogue Scale of 0 (no pain) to 10 (extreme pain). She reported pain episodes, on the level of 8 to 9, once or twice annually. During a manual trunk recompensation maneuver simulating the brace action, pain was reduced. To simulate brace action, the right thoracic rib hump was shifted to the left manually, and the left ventral rib hump was rotated backwards at the same time in order to derotate the twisted thorax.
A CAD (computer-aided design) recompensation brace (Gensingen brace) and Schroth exercise instruction were suggested, as needed. The patient was taught a customized exercise program to be incorporated at home, which was initially provided in Germany and subsequently performed in Norway. The objective of using the Gensingen brace in an adult patient is to achieve a balanced posture in the frontal plane for the imbalanced patient and to restore a physiologic sagittal profile.
Sixteen months after her first evaluation, the patient returned to the office of the senior author for follow-up. This visit included a brace readjustment and Schroth therapy sessions according to the Schroth Best Practice® program. An updated x-ray revealed that her Cobb angles were 55° thoracic and 32° lumbar. Her ATR values were 13° thoracic and 5° lumbar, indicating a more balanced clinical situation (the main curve had reduced and the minor curve had increased little). There were no ethical considerations. Written informed consent was obtained from the patient for publishing her data, clinical pictures, and x-rays within this article.
RESULTS
The patient was interviewed one year later in January 2015. She stated that the combination of bracing and exercises resulted in a dramatic improvement in her quality of life. She reported wearing the brace during work for 3–4 hrs daily on an average of 3 days per week. Additionally, she sometimes wore an off the shelf soft thoraco-lumbao-sacral support. Initially, the patient had exercised (Schroth specific correction exercises) for one hour daily and sometimes cycled in the evening. At the time of the interview, she felt that 20 minutes of exercise every morning was enough. In general, she no longer experienced LBP, although it did occur occasionally when she engaged in heavy lifting. She reported being fully active. Her husband documented her posture and deformity by taking pictures of her back, which demonstrated improvement (Fig. 3). At the 16-month follow-up, her results showed rib hump improvement and improvement of the lumbar (painful) curve from 50° to 32° (Fig. 4).
Fig. 4.
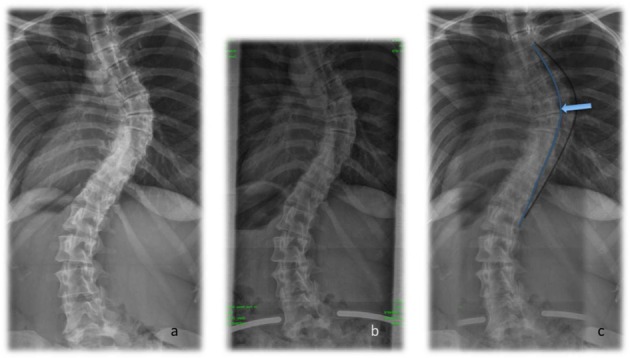
X-ray images at the beginning of treatment (a) and after 16 months of Schroth Best Practice exercise in conjunction with the Gensingen brace (GBW) (b). An overlay of the images (c) shows that recompensation was achieved via conservative treatment. The black line indicates the spinal decompensation at the beginning of treatment, and the blue line indicates the spinal decompensation after 16 months of treatment
DISCUSSION
This case reveals that daily exercise and part-time bracing can potentially reduce pain in the adult scoliosis population. The patient revealed that since her initial appointment, her quality of life improved substantially. She was instructed in Schroth exercise while in Germany, which she continued in Norway, and she subsequently transitioned to a home program.
After one year of part-time brace treatment, she remains satisfied. Additionally, she succeeded in improving her deformity clinically and on x-ray as well.
Patients with LIS do not necessarily experience chronic pain, and natural history studies have shown that they function well, even after 50 years1, 10). Therefore, only a small percentage of patients with idiopathic scoliosis may require treatment in adulthood. If, however, pain exists in adults with spinal deformities, conservative treatment is the logical first choice prior to surgical intervention.
It should be emphasized that conservative treatments can differ substantially. The treatment course in this case study consisted of pattern-specific exercises and a compatible pattern-specific brace treatment according to Schroth Best Practice updates to the Schroth Method24). General exercises and symmetric bracing would not likely have resulted in the same effect25). For the Schroth program, there is evidence in studies with large cohorts that pain can be reduced12, 13). For best results, corrective exercises should be used including training of pattern-specific self-correction during activities of daily living (ADL)24).
Nevertheless, additional information and studies are necessary in order to establish a body of evidence large enough to influence current guidelines.
In conclusion, patients with LIS and pain may benefit from a pattern-specific conservative treatment approach. In this population, surgical intervention should be regarded as a secondary treatment choice because surgery comes with long-term unknowns.
Acknowledgments
HRW provided the first draft. HRW, KM, and MM performed a literature research and wrote the second draft. Copyediting was performed by KM. All authors developed the final manuscript. All authors read and approved the final manuscript. HR Weiss is receiving financial support for attending symposia and receives royalties from Koob GmbH & Co KG. The company is held by the spouse of HR Weiss. Marc Moramarco is the principal of Scoliosis Bracing Innovations, Inc., the North American distributor of the Gensingen Brace®.
REFERENCES
- 1.Asher MA, Burton DC: Adolescent idiopathic scoliosis: natural history and long term treatment effects. Scoliosis, 2006, 1: 2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Goldberg CJ, Moore DP, Fogarty EE, et al. : Adolescent idiopathic scoliosis: natural history and prognosis. Stud Health Technol Inform, 2002, 91: 59–63. [PubMed] [Google Scholar]
- 3.Weinstein SL: Adolescent idiopathic scoliosis: prevalence and natural history. Instr Course Lect, 1989, 38: 115–128. [PubMed] [Google Scholar]
- 4.Weiss HR, Moramarco M: Scoliosis—treatment indications according to current evidence. OA Musculoskelet Med, 2013, 01: 1. [Google Scholar]
- 5.Winter R: Classification and Terminology. In: Lonstein JE BD, Winter RB, Ogilvie JW (eds.), Moe’s Textbook of Scoliosis and other Spinal Deformities, 3rd ed. Philadelphia: WB Saunders, 1995. [Google Scholar]
- 6.Kuru T, Yeldan İ, Dereli EE, et al. : The efficacy of three-dimensional Schroth exercises in adolescent idiopathic scoliosis: a randomised controlled clinical trial. Clin Rehabil, 2016, 30: 181–190. [DOI] [PubMed] [Google Scholar]
- 7.Schreiber S, Parent EC, Moez EK, et al. : The effect of Schroth exercises added to the standard of care on the quality of life and muscle endurance in adolescents with idiopathic scoliosis—an assessor and statistician blinded randomized controlled trial: “SOSORT 2015 Award Winner”. Scoliosis, 2015, 10: 24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Weinstein SL, Dolan LA, Wright JG, et al. : Effects of bracing in adolescents with idiopathic scoliosis. N Engl J Med, 2013, 369: 1512–1521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Weiss HR, Weiss GM: Brace treatment during pubertal growth spurt in girls with idiopathic scoliosis (IS): a prospective trial comparing two different concepts. Pediatr Rehabil, 2005, 8: 199–206. [DOI] [PubMed] [Google Scholar]
- 10.Weinstein SL, Dolan LA, Spratt KF, et al. : Health and function of patients with untreated idiopathic scoliosis: a 50-year natural history study. JAMA, 2003, 289: 559–567. [DOI] [PubMed] [Google Scholar]
- 11.Halm H: OP-Indikationen bei Skoliose. Deutscher Kongress für Orthopädie und Unfallschirurgie (German Conference for Orthopedics and Traumatology / DKOU). Berlin, October 23rd, 2015.
- 12.Weiss HR: Scoliosis related pain in adults—treatment influences. Eur J Phys Med Rehab, 1993, 3: 91–94. [Google Scholar]
- 13.Weiss HR, Verres C, Lohschmidt K, et al. : Schmerz und Skoliose—besteht ein Zusammenhang? Orthop Prax, 1998, 34: 602–606. [Google Scholar]
- 14.Grauers A, Topalis C, Möller H, et al. : Prevalence of back problems in 1069 adults with idiopathic scoliosis and 158 adults without scoliosis. Spine, 2014, 39: 886–892. [DOI] [PubMed] [Google Scholar]
- 15.Upasani VV, Caltoum C, Petcharaporn M, et al. : Adolescent idiopathic scoliosis patients report increased pain at five years compared with two years after surgical treatment. Spine, 2008, 33: 1107–1112. [DOI] [PubMed] [Google Scholar]
- 16.Weiss HR, Moramarco M: Remodeling of trunk and backshape deformities in patients with scoliosis using standardized asymmetric CAD / CAM braces. Hard Tissue, 2013, 2: 14. [Google Scholar]
- 17.Hawes M: Impact of spine surgery on signs and symptoms of spinal deformity. Pediatr Rehabil, 2006, 9: 318–339. [DOI] [PubMed] [Google Scholar]
- 18.Weiss HR: Adolescent idiopathic scoliosis (AIS)—an indication for surgery? A systematic review of the literature. Disabil Rehabil, 2008, 30: 799–807. [DOI] [PubMed] [Google Scholar]
- 19.Westrick ER, Ward WT: Adolescent idiopathic scoliosis: 5-year to 20-year evidence-based surgical results. J Pediatr Orthop, 2011, 31: S61–S68. [DOI] [PubMed] [Google Scholar]
- 20.Ward WT, Friel N, Kenkre TS, et al. : SRS 22r Scores in Non-Operated AIS Patients with Curves 3 40°. Proceedings of the 50th Annual Meeting Minneapolis, Minnesota, US, 2015, September 30th −October 3rd. 2015.
- 21.Weiss HR, Goodall D: Rate of complications in scoliosis surgery—a systematic review of the Pub Med literature. Scoliosis, 2008, 3: 9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mueller FJ, Gluch H: Cotrel-dubousset instrumentation for the correction of adolescent idiopathic scoliosis. Long-term results with an unexpected high revision rate. Scoliosis, 2012, 7: 13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Weiss HR, Moramarco M: Indication for surgical treatment in patients with adolescent Idiopathic Scoliosis—a critical appraisal. Patient Saf Surg, 2013, 7: 17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Weiss H, Lehnert-Schroth C, Moramarco M, et al. : Schroth Therapy−Advancements in Conservative Scoliosis Treatment. Saarbrücken: Lambert Academic Publishing, 2015. [Google Scholar]
- 25.Monticone M, Ambrosini E, Cazzaniga D, et al. : Active self-correction and task-oriented exercises reduce spinal deformity and improve quality of life in subjects with mild adolescent idiopathic scoliosis. Results of a randomised controlled trial. Eur Spine J, 2014, 23: 1204–1214. [DOI] [PubMed] [Google Scholar]


